Time advancement decision making US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Time advancement decision making. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
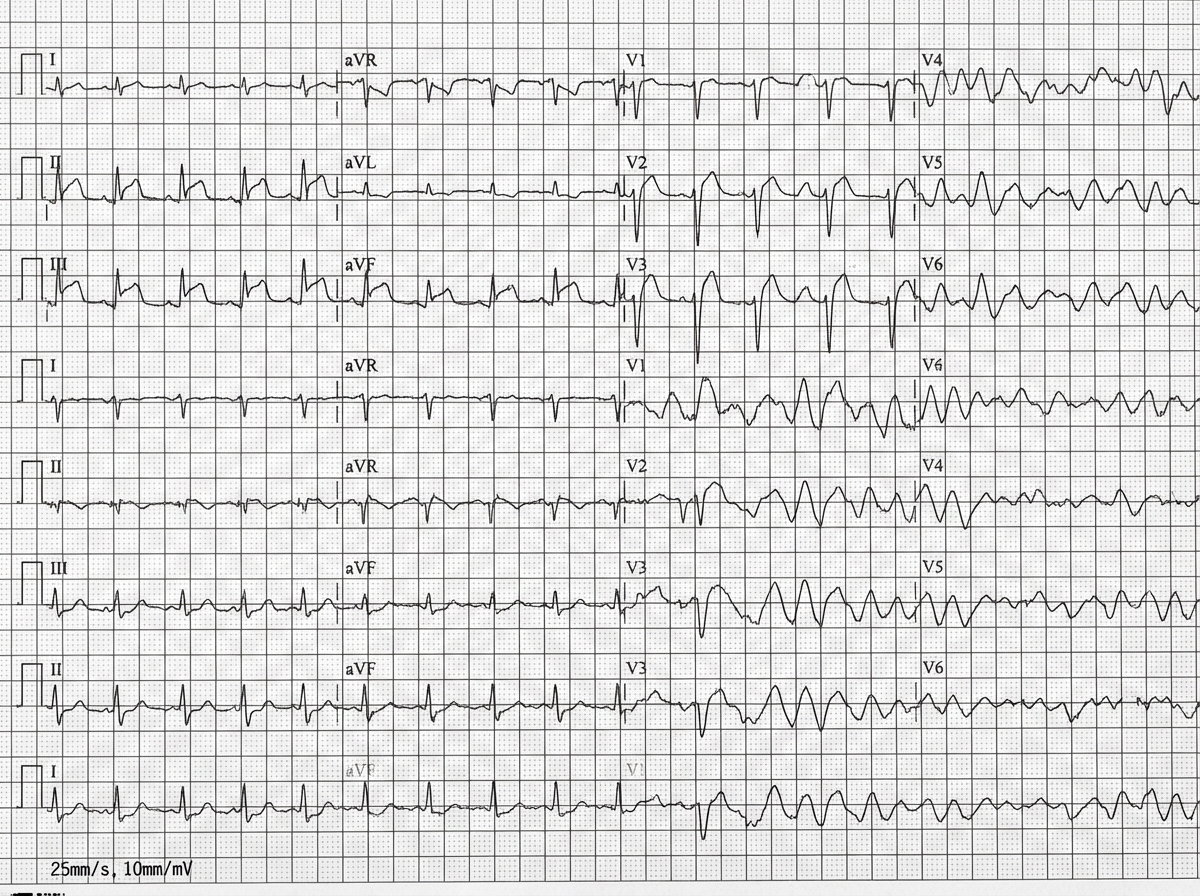
Time advancement decision making US Medical PG Question 1: A 42-year-old man is brought to the emergency department 20 minutes after the sudden onset of severe chest pain, diaphoresis, shortness of breath, and palpitations. His symptoms occurred while he was at a party with friends. He has smoked one pack of cigarettes daily for 24 years. He uses cocaine occasionally. The last use was three hours ago. He appears pale. His pulse is 110/min, blood pressure is 178/106 mm Hg, and respirations are 24/min. His pupils are dilated and react sluggishly to light. The lungs are clear to auscultation. An ECG shows tachycardia and ST segment elevation in leads II, III, and aVF. While recording the ECG, the patient loses consciousness. A photo of the ECG at that point is shown. Which of the following is the most appropriate next step in management?
- A. Administer lidocaine
- B. Unsynchronized cardioversion (Correct Answer)
- C. Administer epinephrine
- D. Coronary angiography
- E. Synchronized cardioversion
Time advancement decision making Explanation: ***Unsynchronized cardioversion***
- The ECG shows **ventricular fibrillation (VF)**, characterized by chaotic, irregular electrical activity without distinct QRS complexes, indicating a life-threatening arrhythmia.
- In a patient who has lost consciousness due to VF, immediate **defibrillation (unsynchronized cardioversion)** is crucial to restore normal sinus rhythm and prevent sudden cardiac death.
- Note: Unsynchronized cardioversion and defibrillation are **synonymous terms** for delivering an unsynchronized shock, with "defibrillation" being the preferred ACLS terminology for VF/pulseless VT.
*Administer lidocaine*
- While lidocaine is an **antiarrhythmic** used in some ventricular arrhythmias, it is typically administered after initial defibrillation attempts have failed or as an adjunct therapy.
- It is not the primary treatment for **unstable ventricular fibrillation**, which requires immediate electrical therapy.
*Administer epinephrine*
- Epinephrine is a **vasopressor** used during cardiac arrest to improve coronary and cerebral perfusion.
- It is administered during **cardiopulmonary resuscitation (CPR)** intervals, usually after initial defibrillation attempts, but not as the first line treatment for VF.
*Coronary angiography*
- Coronary angiography is an **invasive diagnostic procedure** to visualize coronary arteries and identify blockages, suggested by the patient's symptoms and ST elevation in the initial ECG leads.
- However, in the context of **cardiac arrest due to VF**, immediate life-saving interventions take precedence over diagnostic procedures.
*Synchronized cardioversion*
- **Synchronized cardioversion** delivers an electrical shock timed to the R-wave of the QRS complex to treat **tachyarrhythmias with a pulse** (e.g., ventricular tachycardia, atrial fibrillation with rapid ventricular response).
- It is **contraindicated in ventricular fibrillation** because there are no organized QRS complexes to synchronize with, and attempting synchronization can delay life-saving defibrillation.
Time advancement decision making US Medical PG Question 2: A 75-year-old man presents to the emergency department after an episode of syncope while walking outside with his wife. His wife states that he suddenly appeared pale and collapsed to the ground. She says he remained unconscious for 1 minute. He says he noticed a fluttering in his chest and excessive sweating before the episode. He has type 2 diabetes mellitus, essential hypertension, and chronic stable angina. He has not started any new medications in the past few months. Vital signs reveal: temperature 37.0°C (98.6°F), blood pressure 135/72 mm Hg, and pulse 72/min. Physical examination is unremarkable. ECG shows an old bifascicular block. Echocardiogram and 24-hour Holter monitoring are normal. Which of the following is the best next step in the evaluation of this patient's condition?
- A. Cardiac enzymes
- B. Continuous loop recorder (Correct Answer)
- C. Valsalva maneuver
- D. Electroencephalography (EEG)
- E. Tilt-table test
Time advancement decision making Explanation: ***Continuous loop recorder***
- This patient's syncope is preceded by **palpitations (fluttering in chest)** and **sweating**, suggesting a cardiac etiology, specifically a **transient arrhythmia** not captured on a standard ECG or 24-hour Holter.
- A continuous loop recorder provides prolonged monitoring (months to years), increasing the likelihood of detecting intermittent arrhythmias responsible for syncopal episodes.
*Cardiac enzymes*
- While cardiac enzymes (e.g., troponin) are crucial for evaluating **acute myocardial ischemia** or infarction, the patient presents with syncope and no new chest pain, and his stable angina suggests chronic disease rather than an acute event leading to syncope in this specific instance.
- An **ECG showing an old bifascicular block** and an **unremarkable physical exam** make an acute cardiac event less likely as the primary cause of syncope when an arrhythmia is suspected.
*Valsalva maneuver*
- The Valsalva maneuver is a diagnostic tool often used to differentiate between certain types of **tachyarrhythmias** or to evaluate for **autonomic dysfunction**, but it is not an evaluative step for a patient presenting with unexplained syncope where an arrhythmia has not yet been documented.
- It would not help in identifying the cause of intermittent syncope in a patient whose standard workup has been unremarkable, as it's a test for immediate physiological response, not prolonged cardiac rhythm monitoring.
*Electroencephalography (EEG)*
- EEG is indicated when **seizure disorder** is suspected as the cause of loss of consciousness, often characterized by tonic-clonic movements, post-ictal confusion, or focal neurologic signs, which are absent in this patient's presentation.
- The patient's pre-syncopal symptoms of **palpitations and sweating** point away from a seizure and towards a cardiac cause.
*Tilt-table test*
- A tilt-table test is used to evaluate for **vasovagal syncope** or **postural orthostatic tachycardia syndrome (POTS)**, often considered when other cardiac causes are ruled out or when syncope is typically triggered by prolonged standing.
- Given the patient's pre-syncopal **palpitations**, a **cardiac arrhythmia** remains a higher suspicion than vasovagal syncope at this stage, especially after normal echocardiogram and Holter monitoring, necessitating further arrhythmia investigation.
Time advancement decision making US Medical PG Question 3: A 22-year-old man is brought to the emergency department by his friends 30 minutes after falling down a flight of stairs. His friends report that they were at a college party, where he drank large amounts of alcohol. He is aggressive and restless. Examination shows tenderness to palpation and swelling of his right lower leg. An x-ray of the right leg shows a lower tibial shaft fracture. The physician recommends overnight observation and surgery the following morning. The patient refuses the suggested treatment and requests immediate discharge. Otherwise, he says, he will call his lawyer and sue the entire medical staff involved in his care. Which of the following is the most appropriate response by the physician?
- A. You can leave the hospital after signing a self-discharge against medical advice form.
- B. If you don't consent to treatment, I'll be forced to obtain consent from your parents.
- C. I understand that you want to go home, but I'll have to keep you here as long as you are intoxicated. (Correct Answer)
- D. Have you ever felt you should cut down on your drinking?
- E. I can't force you to stay here, but I'll have to inform your dean of this incident.
Time advancement decision making Explanation: ***I understand that you want to go home, but I'll have to keep you here as long as you are intoxicated.***
- An **intoxicated patient may lack decision-making capacity** to refuse medically necessary treatment for a serious injury.
- Before accepting a refusal of treatment or allowing AMA discharge, physicians must **assess the patient's capacity** to make informed decisions.
- Signs of impaired capacity include **acute intoxication, aggressive behavior, and restlessness**, all present in this patient.
- Temporarily holding a patient who lacks capacity and has a serious medical condition requiring urgent care is **legally and ethically justified** to prevent harm—this is NOT false imprisonment.
- Once the patient regains capacity (i.e., sobers up), his decision-making ability can be reassessed, and if he still refuses, AMA discharge can be offered.
*You can leave the hospital after signing a self-discharge against medical advice form.*
- While competent adults have the right to refuse treatment and leave AMA, this option is **premature** because it fails to address the patient's **impaired decision-making capacity** due to acute intoxication.
- A valid refusal requires **capacity to understand the risks and consequences** of leaving—offering AMA discharge without capacity assessment is inappropriate and potentially negligent.
*I can't force you to stay here, but I'll have to inform your dean of this incident.*
- Threatening to inform the patient's dean is a **breach of confidentiality** and an unprofessional response.
- Healthcare providers are bound by **patient confidentiality (HIPAA)**, and sharing this information without consent is unethical and illegal.
*If you don't consent to treatment, I'll be forced to obtain consent from your parents.*
- Since the patient is a **competent adult (age 22)**, his parents cannot give or withhold consent for his medical treatment.
- Parental consent is only required for **minors** or adults who have been legally declared **incompetent** through a court process.
*Have you ever felt you should cut down on your drinking?*
- While addressing alcohol use disorder is important, asking a **CAGE screening question** in this acute, high-stress situation is **inappropriate timing** and poor prioritization.
- The immediate priority is addressing the patient's **acute medical needs and impaired capacity**, not initiating a substance abuse screening.
Time advancement decision making US Medical PG Question 4: A 57-year-old man presents to his oncologist to discuss management of small cell lung cancer. The patient is a lifelong smoker and was diagnosed with cancer 1 week ago. The patient states that the cancer was his fault for smoking and that there is "no hope now." He seems disinterested in discussing the treatment options and making a plan for treatment and followup. The patient says "he does not want any treatment" for his condition. Which of the following is the most appropriate response from the physician?
- A. "You seem upset at the news of this diagnosis. I want you to go home and discuss this with your loved ones and come back when you feel ready to make a plan together for your care."
- B. "It must be tough having received this diagnosis; however, new cancer therapies show increased efficacy and excellent outcomes."
- C. "It must be very challenging having received this diagnosis. I want to work with you to create a plan." (Correct Answer)
- D. "We are going to need to treat your lung cancer. I am here to help you throughout the process."
- E. "I respect your decision and we will not administer any treatment. Let me know if I can help in any way."
Time advancement decision making Explanation: ***"It must be very challenging having received this diagnosis. I want to work with you to create a plan."***
- This response **acknowledges the patient's emotional distress** and feelings of guilt and hopelessness, which is crucial for building rapport and trust.
- It also gently **re-engages the patient** by offering a collaborative approach to treatment, demonstrating the physician's commitment to supporting him through the process.
*"You seem upset at the news of this diagnosis. I want you to go home and discuss this with your loved ones and come back when you feel ready to make a plan together for your care."*
- While acknowledging distress, sending the patient home without further engagement **delays urgent care** for small cell lung cancer, which is aggressive.
- This response might be perceived as dismissive of his immediate feelings and can **exacerbate his sense of hopelessness** and isolation.
*"It must be tough having received this diagnosis; however, new cancer therapies show increased efficacy and excellent outcomes."*
- This statement moves too quickly to treatment efficacy without adequately addressing the patient's current **emotional state and fatalism**.
- While factual, it **lacks empathy** for his personal feelings of blame and hopelessness, potentially making him feel unheard.
*"We are going to need to treat your lung cancer. I am here to help you throughout the process."*
- This response is **too directive and authoritarian**, which can alienate a patient who is already feeling guilty and resistant to treatment.
- It fails to acknowledge his stated feelings of "no hope now" or his disinterest in treatment, which are critical to address before discussing the necessity of treatment.
*"I respect your decision and we will not administer any treatment. Let me know if I can help in any way."*
- While respecting patient autonomy is vital, immediately accepting a patient's decision to refuse treatment without exploring the underlying reasons (e.g., guilt, hopelessness, lack of information) is **premature and potentially harmful**.
- The physician has a responsibility to ensure the patient is making an informed decision, especially for a rapidly progressing condition like small cell lung cancer.
Time advancement decision making US Medical PG Question 5: A 73-year-old man is brought to the emergency department by ambulance after being found to be non-communicative by his family during dinner. On presentation he appears to be alert, though he is confused and cannot follow instructions. When he tries to speak, he vocalizes a string of fluent but unintelligible syllables. Given this presentation, his physician decides to administer tissue plasminogen activator to this patient. This intervention best represents which of the following principles?
- A. Tertiary prevention
- B. Primary prevention
- C. This does not represent prevention (Correct Answer)
- D. Quaternary prevention
- E. Secondary prevention
Time advancement decision making Explanation: ***This does not represent prevention***
- The administration of **tissue plasminogen activator (tPA)** during an **acute stroke** is a **therapeutic intervention**, not a form of prevention.
- **Prevention** refers to actions taken to prevent disease occurrence, detect it early, or prevent complications after recovery. Treating an acute, symptomatic event is **acute treatment**, not prevention.
- This is an active medical intervention to treat an ongoing, symptomatic disease process (acute ischemic stroke), which falls under **therapeutic management** rather than any category of prevention.
*Secondary prevention*
- **Secondary prevention** involves **early detection** and treatment of asymptomatic or minimally symptomatic disease to prevent progression (e.g., screening mammography, colonoscopy).
- For stroke specifically, secondary prevention would include interventions **after** the acute event to **prevent recurrence**, such as starting antiplatelet therapy (aspirin, clopidogrel), anticoagulation for atrial fibrillation, statin therapy, or carotid endarterectomy after TIA.
- tPA is given during the acute symptomatic phase, making it treatment rather than secondary prevention.
*Tertiary prevention*
- **Tertiary prevention** focuses on **rehabilitation** and managing established disease to prevent complications and improve quality of life.
- Examples after stroke include physical therapy, occupational therapy, speech therapy, and managing post-stroke complications like depression or spasticity.
- This occurs in the recovery phase, not during acute treatment.
*Primary prevention*
- **Primary prevention** aims to prevent disease before it occurs in healthy individuals.
- Examples include controlling hypertension, managing diabetes, smoking cessation, exercise, and healthy diet - all interventions that reduce stroke risk **before** any event occurs.
*Quaternary prevention*
- **Quaternary prevention** protects patients from **overmedicalization** and excessive or harmful medical interventions.
- It involves avoiding unnecessary testing or treatment that may cause more harm than benefit.
- Administering tPA for acute stroke (when indicated) is evidence-based treatment, not overtreatment.
Time advancement decision making US Medical PG Question 6: An orthopaedic surgeon at a local community hospital has noticed that turnover times in the operating room have been unnecessarily long. She believes that the long wait times may be due to inefficient communication between the surgical nursing staff, the staff in the pre-operative area, and the staff in the post-operative receiving area. She believes a secure communication mobile phone app would help to streamline communication between providers and improve efficiency in turnover times. Which of the following methods is most appropriate to evaluate the impact of this intervention in the clinical setting?
- A. Plan-Do-Study-Act cycle (Correct Answer)
- B. Failure modes and effects analysis
- C. Standardization
- D. Forcing function
- E. Root cause analysis
Time advancement decision making Explanation: ***Plan-Do-Study-Act cycle***
- The **Plan-Do-Study-Act (PDSA) cycle** is a structured, iterative model used for continuous improvement in quality and efficiency, making it ideal for evaluating the impact of a new intervention like a communication app.
- This cycle allows for small-scale testing of changes, observation of results, learning from the observations, and refinement of the intervention before full implementation.
*Failure modes and effects analysis*
- **Failure modes and effects analysis (FMEA)** is a prospective method to identify potential failures in a process, predict their effects, and prioritize actions to prevent them.
- While useful for process improvement, FMEA is typically performed *before* implementing a change to identify risks, rather than to evaluate the impact of an already implemented intervention.
*Standardization*
- **Standardization** involves creating and implementing consistent processes or protocols to reduce variability and improve reliability.
- While the communication app might contribute to standardization, standardization itself is a *method of improvement* rather than a method for *evaluating the impact* of an intervention.
*Forcing function*
- A **forcing function** is a design feature that physically prevents an error from occurring, making it impossible to complete a task incorrectly.
- An app that streamlines communication does not act as a forcing function, as it facilitates a process rather than physically preventing an incorrect action.
*Root cause analysis*
- **Root cause analysis (RCA)** is a retrospective method used to investigate an event that has already occurred (e.g., an adverse event) to identify its underlying causes.
- This method is used *after* a problem has manifested to understand *why* it happened, not to evaluate the *impact* of a new intervention designed to prevent future problems.
Time advancement decision making US Medical PG Question 7: You are currently employed as a clinical researcher working on clinical trials of a new drug to be used for the treatment of Parkinson's disease. Currently, you have already determined the safe clinical dose of the drug in a healthy patient. You are in the phase of drug development where the drug is studied in patients with the target disease to determine its efficacy. Which of the following phases is this new drug currently in?
- A. Phase 4
- B. Phase 1
- C. Phase 2 (Correct Answer)
- D. Phase 0
- E. Phase 3
Time advancement decision making Explanation: ***Phase 2***
- **Phase 2 trials** involve studying the drug in patients with the target disease to assess its **efficacy** and further evaluate safety, typically involving a few hundred patients.
- The question describes a stage after safe dosing in healthy patients (Phase 1) and before large-scale efficacy confirmation (Phase 3), focusing on efficacy in the target population.
*Phase 4*
- **Phase 4 trials** occur **after a drug has been approved** and marketed, monitoring long-term effects, optimal use, and rare side effects in a diverse patient population.
- This phase is conducted post-market approval, whereas the question describes a drug still in development prior to approval.
*Phase 1*
- **Phase 1 trials** primarily focus on determining the **safety and dosage** of a new drug in a **small group of healthy volunteers** (or sometimes patients with advanced disease if the drug is highly toxic).
- The question states that the safe clinical dose in a healthy patient has already been determined, indicating that Phase 1 has been completed.
*Phase 0*
- **Phase 0 trials** are exploratory, very early-stage studies designed to confirm that the drug reaches the target and acts as intended, typically involving a very small number of doses and participants.
- These trials are conducted much earlier in the development process, preceding the determination of safe clinical doses and large-scale efficacy studies.
*Phase 3*
- **Phase 3 trials** are large-scale studies involving hundreds to thousands of patients to confirm **efficacy**, monitor side effects, compare it to commonly used treatments, and collect information that will allow the drug to be used safely.
- While Phase 3 does assess efficacy, it follows Phase 2 and is typically conducted on a much larger scale before submitting for regulatory approval.
Time advancement decision making US Medical PG Question 8: A 59-year-old woman comes to the physician because of left leg swelling that started after a transcontinental flight. A duplex ultrasound of the left leg shows a noncompressible popliteal vein. A drug is prescribed that inhibits the coagulation cascade. Two weeks later, laboratory studies show:
Platelet count 210,000/mm3
Partial thromboplastin time 28 seconds (normal: 25-35)
Prothrombin time 12 seconds (normal: 11-13)
Thrombin time 15 seconds (control: 15 seconds)
Which of the following drugs was most likely prescribed?
- A. Unfractionated heparin
- B. Apixaban
- C. Aspirin
- D. Warfarin
- E. Low molecular weight heparin (Correct Answer)
Time advancement decision making Explanation: ***Low molecular weight heparin***
- **LMWH (e.g., enoxaparin) is the first-line treatment for acute DVT** in ambulatory patients and is the most likely drug prescribed in this outpatient scenario
- LMWH enhances **antithrombin activity primarily against Factor Xa** (more than Factor IIa/thrombin), which is why it has **minimal effect on routine coagulation tests** (PT, PTT, TT)
- **Monitoring of LMWH is done via anti-Xa levels**, not PTT, PT, or TT, explaining why all these values remain normal two weeks after initiation
- The normal coagulation studies are **expected and consistent** with therapeutic LMWH use
*Unfractionated heparin*
- Unfractionated heparin (UFH) acts by enhancing **antithrombin activity against both Factor Xa and Factor IIa (thrombin)**, which significantly **prolongs PTT** (typically 1.5-2x control when therapeutic)
- UFH requires **IV administration and hospital monitoring**, making it unlikely for this ambulatory post-flight DVT patient
- If the patient were currently on UFH, the **PTT would be prolonged** (not normal as shown); if discontinued, this wouldn't be "the drug prescribed" for ongoing DVT treatment
*Apixaban*
- Apixaban is a **direct Factor Xa inhibitor** that would cause **mild prolongation of PT** and possibly PTT at therapeutic levels
- While it's a reasonable outpatient DVT treatment, the completely normal PT argues against current apixaban use
- Apixaban doesn't require routine monitoring, but when measured, coagulation times would typically show some abnormality
*Warfarin*
- Warfarin is a **vitamin K antagonist** that inhibits synthesis of factors II, VII, IX, and X, causing **significant PT/INR prolongation** (target INR 2-3 for DVT)
- The **normal PT (12 seconds) excludes warfarin** as the current medication
- Warfarin requires regular INR monitoring and would not show normal values at therapeutic doses
*Aspirin*
- Aspirin is an **antiplatelet agent** (COX-1 inhibitor) that affects platelet aggregation, **not the coagulation cascade**
- It has **no effect on PT, PTT, or TT** and is **inadequate monotherapy for DVT treatment**
- While it may have a role in extended VTE prevention, it would not be the primary drug prescribed for acute DVT
More Time advancement decision making US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.