Surgical vs non-surgical management US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Surgical vs non-surgical management. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Surgical vs non-surgical management US Medical PG Question 1: A 67-year-old woman has fallen from the second story level of her home while hanging laundry. She was brought to the emergency department immediately and presented with severe abdominal pain. The patient is anxious, and her hands and feet feel very cold to the touch. There is no evidence of bone fractures, superficial skin wounds, or a foreign body penetration. Her blood pressure is 102/67 mm Hg, respirations are 19/min, pulse is 87/min, and temperature is 36.7°C (98.0°F). Her abdominal exam reveals rigidity and severe tenderness. A Foley catheter and nasogastric tube are inserted. The central venous pressure (CVP) is 5 cm H2O. The medical history is significant for hypertension. Which of the following is best indicated for the evaluation of this patient?
- A. X-Ray
- B. Ultrasound
- C. Peritoneal lavage
- D. CT scan (Correct Answer)
- E. Diagnostic laparotomy
Surgical vs non-surgical management Explanation: ***CT scan***
- A **CT scan of the abdomen and pelvis** is the most indicated imaging modality for evaluating blunt abdominal trauma due to its high sensitivity and specificity in detecting solid organ injuries, free fluid, and active bleeding.
- Given the patient's severe abdominal pain, rigidity, and tenderness after a significant fall, a CT scan will provide detailed anatomical information crucial for guiding further management.
*X-Ray*
- An **X-ray** is useful for detecting bone fractures, but it has limited utility in assessing soft tissue and organ injuries within the abdomen.
- It would not effectively visualize internal bleeding or organ damage, which are primary concerns in this patient given the mechanism of injury and symptoms.
*Ultrasound*
- An **ultrasound (FAST exam)** is effective for rapid detection of free fluid in the abdomen (indicating bleeding or fluid leakage) and can be done at the bedside.
- However, it is operator-dependent and less sensitive than CT for identifying specific organ injuries, retroperitoneal hematomas, or the source of bleeding.
*Peritoneal lavage*
- **Diagnostic peritoneal lavage (DPL)** is an invasive procedure primarily used to detect intra-abdominal bleeding in hemodynamically unstable patients, but it has largely been replaced by ultrasound and CT in stable patients.
- While it can detect blood, it is less specific for identifying the source of bleeding and does not provide anatomical detail, and carries risks of complications like bowel perforation.
*Diagnostic laparotomy*
- **Diagnostic laparotomy** is a surgical procedure to directly visualize abdominal contents and is indicated in cases of clear signs of peritonitis, hemodynamic instability with confirmed intra-abdominal bleeding, or evisceration.
- It is an invasive intervention and would not be the initial diagnostic step in a hemodynamically stable patient without clear indication for immediate surgery.
Surgical vs non-surgical management US Medical PG Question 2: A 62-year-old man presents to the emergency department with sudden onset of severe left leg pain accompanied by numbness and weakness. His medical history is remarkable for hypertension and hyperlipidemia. His vital signs include a blood pressure of 155/92 mm Hg, a temperature of 37.1°C (98.7°F), and an irregular pulse of 92/min. Physical examination reveals absent left popliteal and posterior tibial pulses. His left leg is noticeably cold and pale. There is no significant tissue compromise, nerve damage, or sensory loss. Which of the following will most likely be required for this patient's condition?
- A. Antibiotics
- B. Warfarin
- C. Fasciotomy
- D. Amputation
- E. Thromboembolectomy (Correct Answer)
Surgical vs non-surgical management Explanation: ***Thromboembolectomy***
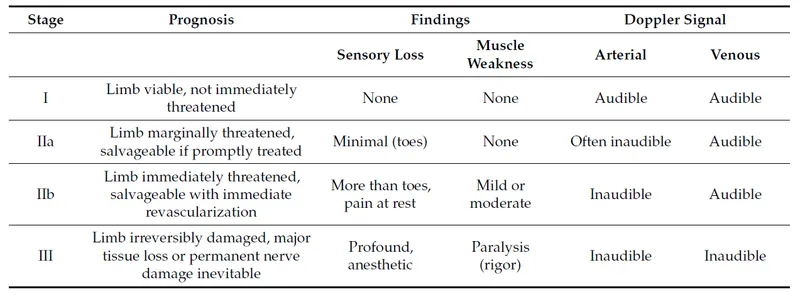
- The sudden onset of severe leg pain, numbness, and weakness with absent pulses, a cold, pale limb, and an irregular pulse suggests **acute limb ischemia** likely due to an **arterial embolus**, which requires emergent surgical removal.
- Given the symptoms and history of an irregular pulse (suggesting possible atrial fibrillation), a thromboembolectomy is the most appropriate first-line treatment to restore blood flow and prevent permanent damage.
*Antibiotics*
- Antibiotics are used to treat **bacterial infections** and are not indicated for acute limb ischemia caused by a vascular occlusion.
- There are no signs of infection present, such as fever, redness, or purulent discharge, that would warrant antibiotic therapy.
*Warfarin*
- Warfarin is an **anticoagulant** used for long-term prevention of clot formation, particularly in conditions like atrial fibrillation or deep vein thrombosis.
- While anticoagulation may eventually be part of management to prevent future events, it is insufficient as immediate therapy for an acute, established arterial embolus causing critical limb ischemia.
*Fasciotomy*
- Fasciotomy is performed to relieve **compartment syndrome**, which occurs when increased pressure within a muscle compartment compromises circulation and nerve function.
- While compartment syndrome can be a complication of reperfusion after prolonged ischemia, it is not the primary treatment for the initial arterial occlusion; the first step is to restore blood flow to prevent the need for it.
*Amputation*
- Amputation is a last resort considered when the limb is **irreversibly ischemic** and non-viable, or when revascularization attempts have failed and there is extensive tissue necrosis or infection.
- In this case, there is no significant tissue compromise or nerve damage mentioned, indicating that the limb is still salvageable with timely intervention.
Surgical vs non-surgical management US Medical PG Question 3: A 42-year-old man presents to the emergency department with abdominal pain. The patient was at home watching television when he experienced sudden and severe abdominal pain that prompted him to instantly call emergency medical services. The patient has a past medical history of obesity, smoking, alcoholism, hypertension, and osteoarthritis. His current medications include lisinopril and ibuprofen. His temperature is 98.5°F (36.9°C), blood pressure is 120/97 mmHg, pulse is 130/min, respirations are 22/min, and oxygen saturation is 97% on room air. The patient is in an antalgic position on the stretcher. His abdomen is rigid and demonstrates rebound tenderness and hypoactive bowel sounds. What is the next best step in management?
- A. CT of the abdomen
- B. Urgent laparoscopy
- C. NPO, IV fluids, and analgesics
- D. Urgent laparotomy (Correct Answer)
- E. Abdominal radiograph
Surgical vs non-surgical management Explanation: ***Urgent laparotomy***
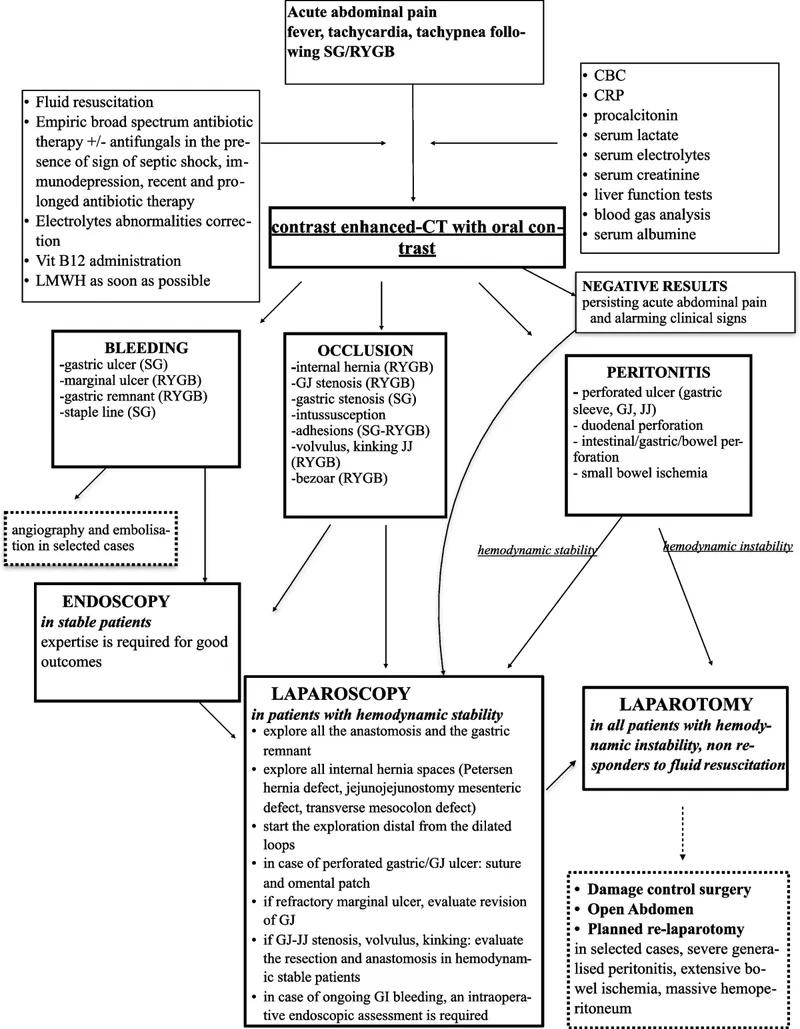
- The patient's presentation with **sudden, severe abdominal pain**, a **rigid abdomen**, **rebound tenderness**, and **hypoactive bowel sounds** indicates **acute peritonitis**, most likely from a **perforated viscus**.
- In a patient with **frank peritonitis** and clinical signs of perforation, the diagnosis is **made clinically** based on physical examination findings.
- **Urgent laparotomy** (exploratory surgery) is the definitive management and should not be delayed for imaging when peritonitis is obvious.
- The patient's risk factors (NSAID use, alcoholism) further support peptic ulcer perforation as the likely etiology.
*CT of the abdomen*
- While CT scan is highly sensitive for identifying perforation and can provide anatomic detail, it is **not necessary when the diagnosis of peritonitis is clinically evident**.
- In a patient with **obvious peritonitis**, obtaining a CT scan would **delay definitive surgical treatment** without changing management.
- CT is more appropriate for stable patients with **uncertain diagnosis** or equivocal physical findings, not for those with frank peritonitis.
*Urgent laparoscopy*
- **Laparoscopy** can be used diagnostically and therapeutically in selected cases of abdominal emergencies.
- However, in a patient with diffuse peritonitis and suspected perforation, **laparotomy** is generally preferred over laparoscopy as it provides better exposure, faster source control, and easier peritoneal lavage.
- Laparoscopy may be considered in stable patients with localized findings, but this patient has signs of diffuse peritonitis.
*NPO, IV fluids, and analgesics*
- These are **essential supportive measures** and should be initiated immediately as part of resuscitation.
- However, they are **adjunctive** to definitive surgical management and do not constitute the "next best step" in a patient requiring emergency surgery.
- These measures should be initiated concurrently while preparing for urgent laparotomy.
*Abdominal radiograph*
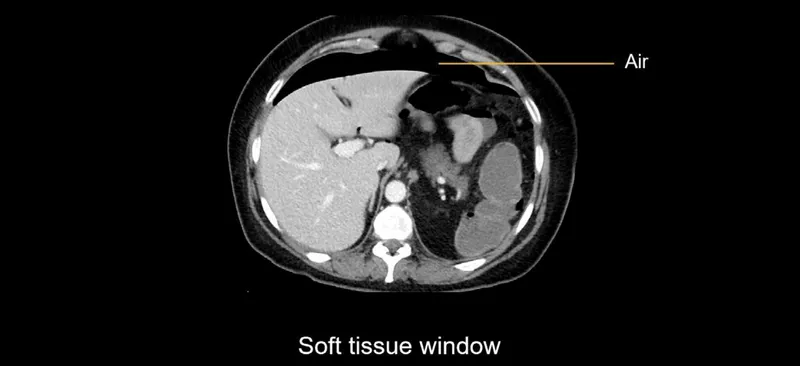
- An **upright chest X-ray** or **abdominal radiograph** can show **free air under the diaphragm** (pneumoperitoneum) in cases of perforation.
- However, it is **only 50-70% sensitive**, meaning it misses many perforations.
- In a patient with **clinical peritonitis**, the absence of free air on X-ray does **not rule out perforation** and should not delay surgery.
- Imaging should not delay surgical intervention when peritonitis is clinically evident.
Surgical vs non-surgical management US Medical PG Question 4: A 24-year-old woman is brought to the emergency department after being assaulted. The paramedics report that the patient was found conscious and reported being kicked many times in the torso. She is alert and able to respond to questions. She denies any head trauma. She has a past medical history of endometriosis and a tubo-ovarian abscess that was removed surgically two years ago. Her only home medication is oral contraceptive pills. Her temperature is 98.5°F (36.9°C), blood pressure is 82/51 mmHg, pulse is 136/min, respirations are 24/min, and SpO2 is 94%. She has superficial lacerations to the face and severe bruising over her chest and abdomen. Her lungs are clear to auscultation bilaterally and her abdomen is soft, distended, and diffusely tender to palpation. Her skin is cool and clammy. Her FAST exam reveals fluid in the perisplenic space.
Which of the following is the next best step in management?
- A. Emergency laparotomy (Correct Answer)
- B. Abdominal radiograph
- C. Abdominal CT
- D. Fluid resuscitation
- E. Diagnostic peritoneal lavage
Surgical vs non-surgical management Explanation: ***Emergency laparotomy***
- The patient presents with **hemodynamic instability** (BP 82/51 mmHg, HR 136/min) and a **positive FAST exam** showing fluid in the perisplenic space, indicating intra-abdominal hemorrhage.
- According to **ATLS guidelines**, a hemodynamically unstable patient with a positive FAST exam requires **immediate operative intervention** to control bleeding. This is the definitive management for ongoing hemorrhage.
- While fluid resuscitation is initiated simultaneously (en route to OR), **surgical control of the bleeding source** is the priority and should not be delayed.
*Fluid resuscitation*
- Fluid resuscitation with IV crystalloids is essential and should be started immediately in this patient with hypovolemic shock.
- However, in a patient with **uncontrolled intra-abdominal hemorrhage** (positive FAST, hemodynamic instability), fluids alone will not stop the bleeding. Continued fluid resuscitation without surgical intervention can lead to dilutional coagulopathy and worsening outcomes.
- Fluid resuscitation occurs **concurrently with preparation for surgery**, not as a separate step that delays definitive management.
*Diagnostic peritoneal lavage*
- DPL is an invasive diagnostic procedure that has largely been replaced by FAST exam in modern trauma care.
- Given that the **FAST is already positive**, DPL would provide no additional useful information and would only **delay definitive surgical management**.
- In hemodynamically unstable patients with positive FAST, proceeding directly to laparotomy is indicated.
*Abdominal radiograph*
- Plain radiographs have **limited sensitivity** for detecting intra-abdominal bleeding or solid organ injury.
- They may show free air (indicating hollow viscus perforation) but cannot assess for fluid or characterize solid organ injuries.
- This would **delay necessary operative intervention** without providing actionable information.
*Abdominal CT*
- CT abdomen is the imaging modality of choice for **hemodynamically stable** trauma patients to characterize injuries and guide management.
- For **unstable patients**, CT is **contraindicated** as it delays definitive treatment and removes the patient from a resuscitation environment where deterioration can be immediately addressed.
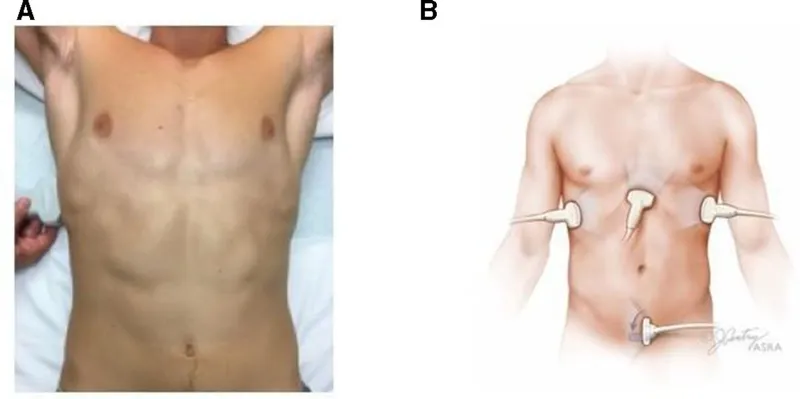
Surgical vs non-surgical management US Medical PG Question 5: A 72-year-old man comes to the emergency department because of severe, acute, right leg pain for 2 hours. The patient's symptoms started suddenly while he was doing household chores. He has no history of leg pain at rest or with exertion. Yesterday, he returned home after a 6-hour bus ride from his grandson's home. He has hypertension treated with ramipril. He appears uncomfortable. His temperature is 37.4°C (99.3°F), pulse is 105/min and irregular, and blood pressure is 146/92 mm Hg. The right lower extremity is cool and tender to touch. A photograph of the limb is shown. Femoral pulses are palpable bilaterally; popliteal and pedal pulses are decreased on the right side. Sensation to pinprick and light touch and muscle strength are decreased in the right lower extremity. Which of the following is most likely to confirm the underlying source of this patient's condition?
- A. Biopsy of a superficial vein
- B. Doppler ultrasonography of the legs
- C. Digital subtraction angiography
- D. Manometry
- E. Echocardiography (Correct Answer)
Surgical vs non-surgical management Explanation: ***Echocardiography***
- The patient's presentation with acute, severe leg pain, coolness, decreased pulses, and neurological deficits in the right lower extremity, along with an **irregular pulse** (suggesting **atrial fibrillation**), points to an **arterial embolism**.
- An **echocardiogram** is crucial to identify the source of the embolus, most commonly a **left atrial thrombus** due to atrial fibrillation, which would then confirm the underlying cause.
*Biopsy of a superficial vein*
- A biopsy of a superficial vein would be indicated for conditions like **vasculitis** or **thrombophlebitis**, which are not consistent with the acute, severe arterial occlusion observed.
- This test would not help in identifying the source of an arterial embolus causing acute limb ischemia.
*Doppler ultrasonography of the legs*
- While **Doppler ultrasonography** can confirm the presence of **arterial occlusion** and assess flow, it does not identify the **source** of an embolus.
- It is more useful for diagnosing deep vein thrombosis or chronic arterial insufficiency, which are not the primary concern here.
*Digital subtraction angiography*
- **Digital subtraction angiography** is an invasive procedure that can precisely map the arterial tree and identify the location of the **occlusion**.
- However, it primarily pinpoints the site of the blockage and doesn't reveal the **etiology** or the source of an embolus in the heart.
*Manometry*
- **Manometry** is used to measure pressures, typically in the gastrointestinal tract or for compartment syndrome, and is not relevant for diagnosing the source of an arterial embolus.
- This diagnostic tool has no role in the investigation of acute limb ischemia or its cardiac origin.
Surgical vs non-surgical management US Medical PG Question 6: A 32-year-old man is brought to the emergency department after a skiing accident. The patient had been skiing down the mountain when he collided with another skier who had stopped suddenly in front of him. He is alert but complaining of pain in his chest and abdomen. He has a past medical history of intravenous drug use and peptic ulcer disease. He is a current smoker. His temperature is 97.4°F (36.3°C), blood pressure is 77/53 mmHg, pulse is 127/min, and respirations are 13/min. He has a GCS of 15 and bilateral shallow breath sounds. His abdomen is soft and distended with bruising over the epigastrium. He is moving all four extremities and has scattered lacerations on his face. His skin is cool and delayed capillary refill is present. Two large-bore IVs are placed in his antecubital fossa, and he is given 2L of normal saline. His FAST exam reveals fluid in Morison's pouch. Following the 2L normal saline, his temperature is 97.5°F (36.4°C), blood pressure is 97/62 mmHg, pulse is 115/min, and respirations are 12/min.
Which of the following is the best next step in management?
- A. Diagnostic peritoneal lavage
- B. Emergency laparotomy (Correct Answer)
- C. Upper gastrointestinal endoscopy
- D. Close observation
- E. Diagnostic laparoscopy
Surgical vs non-surgical management Explanation: ***Emergency laparotomy***
- The patient remains **hemodynamically unstable** (BP 97/62 mmHg, HR 115/min after 2L IV fluids) with evidence of **intra-abdominal fluid on FAST exam** (fluid in Morison's pouch).
- This clinical picture indicates active intra-abdominal hemorrhage requiring **immediate surgical intervention** to identify and control the source of bleeding.
*Diagnostic peritoneal lavage*
- **Diagnostic peritoneal lavage (DPL)** has largely been replaced by the focused abdominal sonography for trauma (FAST) exam and CT scans.
- While it can detect intra-abdominal bleeding, it is **invasive** and would delay definitive treatment in a hemodynamically unstable patient with positive FAST.
*Upper gastrointestinal endoscopy*
- This procedure is primarily for diagnosing and treating **upper gastrointestinal bleeding** or mucosal abnormalities.
- It is **not indicated** for evaluating traumatic intra-abdominal hemorrhage or hemodynamic instability following blunt abdominal trauma.
*Close observation*
- Close observation is appropriate for **hemodynamically stable patients** with blunt abdominal trauma and minor injuries or equivocal findings.
- This patient's persistent hypotension, tachycardia, and positive FAST findings rule out observation as a safe or appropriate next step.
*Diagnostic laparoscopy*
- **Diagnostic laparoscopy** is a minimally invasive surgical procedure used to evaluate the abdominal cavity.
- While it can be diagnostic, it is generally **contraindicated in hemodynamically unstable patients** as it can prolong the time to definitive hemorrhage control if a major injury is found.
Surgical vs non-surgical management US Medical PG Question 7: A trauma 'huddle' is called. Morphine is administered for pain. Low-flow oxygen is begun. A traumatic diaphragmatic rupture is suspected. Infusion of 0.9% saline is begun. Which of the following is the most appropriate next step in management?
- A. Chest fluoroscopy
- B. Barium study
- C. CT of the chest, abdomen, and pelvis (Correct Answer)
- D. MRI chest and abdomen
- E. ICU admission and observation
Surgical vs non-surgical management Explanation: ***CT of the chest, abdomen, and pelvis***
- A suspected **traumatic diaphragmatic rupture** requires a comprehensive imaging study to assess the diaphragm, surrounding organs, and potential associated injuries.
- **CT scan** of the chest, abdomen, and pelvis provides detailed anatomical information, can identify herniated abdominal contents, and is essential for surgical planning in trauma settings.
*Chest fluoroscopy*
- While fluoroscopy can detect diaphragmatic motion, it is **less sensitive** for identifying tears or herniated contents in the **acute trauma setting**.
- It does not provide the comprehensive view of surrounding organs and associated injuries often needed in trauma.
*Barium study*
- A barium study is primarily used to evaluate the **gastrointestinal tract**, but it is generally **not the initial imaging modality** for diaphragmatic rupture due to its limited ability to visualize the diaphragm itself or other solid organ injuries.
- It would be performed after suspicion is increased or for very specific indications, not as a primary diagnostic tool.
*MRI chest and abdomen*
- While MRI offers excellent soft tissue contrast, its use in **acute trauma** is limited by **longer acquisition times**, potential contraindications with metallic implants (though less common in acute trauma), and lower availability compared to CT.
- CT remains the **gold standard** for rapid, comprehensive imaging in unstable trauma patients.
*ICU admission and observation*
- While observation in the ICU is important for monitoring and supportive care, it is **not the next step for diagnosis** of a suspected diaphragmatic rupture.
- Definitive diagnosis through imaging (CT) is crucial before determining specific management strategies, including potential surgical intervention.
Surgical vs non-surgical management US Medical PG Question 8: A 25-year-old man is brought to the emergency department because of a 6-day history of fever and chills. During this period, he has had generalized weakness, chest pain, and night sweats. He has a bicuspid aortic valve and recurrent migraine attacks. He has smoked one pack of cigarettes daily for 5 years. He does not drink alcohol. He has experimented with intravenous drugs in the past but has not used any illicit drugs in the last two months. Current medications include propranolol and a multivitamin. He appears ill. His temperature is 39°C (102.2°F), pulse is 108/min, respirations are 14/min, and blood pressure is 150/50 mm Hg. Diffuse crackles are heard. A grade 3/6 high-pitched, early diastolic, decrescendo murmur is best heard along the left sternal border. An S3 gallop is heard. The remainder of the physical examination shows no abnormalities. Laboratory studies show:
Hemoglobin 13.1 g/dL
Leukocyte count 13,300/mm3
Platelet count 270,000/mm3
Serum
Glucose 92 mg/dL
Creatinine 0.9 mg/dL
Total bilirubin 0.4 mg/dL
AST 25 U/L
ALT 28 U/L
Three sets of blood cultures are sent to the laboratory. Transthoracic echocardiography confirms the diagnosis. In addition to antibiotic therapy, which of the following is the most appropriate next step in management?
- A. Transcatheter aortic valve implantation (TAVI)
- B. Repeat echocardiography in 4 weeks
- C. Cardiac MRI
- D. Mechanical valve replacement of the aortic valve
- E. Porcine valve replacement of the aortic valve (Correct Answer)
Surgical vs non-surgical management Explanation: ***Porcine valve replacement of the aortic valve***
- The patient presents with **infective endocarditis** (fever, history of IV drug use, bicuspid aortic valve) complicated by **severe aortic regurgitation** with **hemodynamic compromise** (wide pulse pressure 150/50 mmHg, diffuse crackles, S3 gallop indicating heart failure). The presence of heart failure, severe regurgitation, and hemodynamic instability are **class I indications for urgent surgical valve replacement** in infective endocarditis.
- For this **25-year-old with a history of IV drug use**, a **bioprosthetic (porcine) valve** is preferred over mechanical valve because it **avoids the need for lifelong anticoagulation**. In patients with **history of substance abuse**, there are significant concerns about **compliance with warfarin therapy** and the associated bleeding risks. Additionally, the risk of **recurrent endocarditis** from future IV drug use makes avoiding anticoagulation particularly important, as warfarin increases bleeding complications.
- The **new diastolic murmur**, **S3 gallop**, and **low diastolic blood pressure (50 mmHg)** indicate critical hemodynamic compromise requiring prompt surgical intervention once antibiotic therapy is initiated.
*Mechanical valve replacement of the aortic valve*
- While mechanical valves offer **greater durability** and are often considered for young patients due to longevity (avoiding repeat surgery), they require **lifelong anticoagulation with warfarin**.
- In this patient with **recent IV drug use history** (stopped only 2 months ago), there are significant concerns about **medication compliance** and the **high risk of bleeding complications** with anticoagulation. The risk of **recurrent IV drug use** and potential for trauma also makes anticoagulation particularly hazardous.
- Though mechanical valve is a viable option, the **patient's social history** makes bioprosthetic valve the safer choice despite his young age.
*Transcatheter aortic valve implantation (TAVI)*
- **TAVI** is primarily indicated for **aortic stenosis** in elderly or high-surgical-risk patients, not for **aortic regurgitation** in young patients.
- The presence of **active infection** is a **relative contraindication** to TAVI due to risk of seeding the new prosthetic valve and technical challenges with valve seating in an inflamed annulus.
*Repeat echocardiography in 4 weeks*
- Delayed follow-up would be appropriate for **stable, medically managed endocarditis** or mild valve dysfunction.
- This patient has **acute, severe heart failure** with hemodynamic instability requiring **urgent surgical intervention**, not watchful waiting.
*Cardiac MRI*
- While cardiac MRI provides detailed anatomical and functional information, it is **not indicated** when the diagnosis has already been **confirmed by echocardiography** and the patient requires **urgent surgical management**.
- Further imaging would only delay necessary treatment in a hemodynamically unstable patient.
Surgical vs non-surgical management US Medical PG Question 9: An 8-month-old boy is brought to the emergency department by his mother. She is concerned that her son has had intermittent periods of severe abdominal pain over the past several days that has been associated with emesis and "currant jelly" stool. Of note, the family lives in a rural part of the state, requiring a 2 hour drive to the nearest hospital. He currently appears to be in significant pain and has vomited twice in the past hour. On physical examination, a sausage-shaped mass is noted on palpation of the right upper quadrant of the abdomen. Ultrasound of the abdomen was consistent with a diagnosis of intussusception. An air-contrast barium enema was performed, which confirmed the diagnosis and also successfully reduced the intussusception. Which of the following is the next best step in the management of this patient?
- A. Keep patient NPO and initiate work-up to identify lead-point
- B. Admit to hospital for 24 hour observation for complications and/or recurrence (Correct Answer)
- C. Pursue urgent surgical reduction with resection of necrotic segments of bowel
- D. Repeat barium enema q6 hrs to monitor for recurrence
- E. Discharge to home with follow-up in 3 weeks in an outpatient pediatric gastroenterology clinic
Surgical vs non-surgical management Explanation: ***Admit to hospital for 24 hour observation for complications and/or recurrence***
- Following successful non-operative reduction of intussusception, there is a risk of **recurrence** (approximately 5-10%) and potential for **perforation** or other delayed complications, necessitating close hospital observation.
- The patient's presentation with significant pain and vomiting, coupled with the long travel time to the hospital, further supports the need for **hospital admission** to monitor for stability and potential early recurrence.
*Keep patient NPO and initiate work-up to identify lead-point*
- While keeping the patient NPO (nil per os) might be appropriate initially, a work-up for a **lead point** is generally performed if there are multiple recurrences or in older children, as most intussusceptions in infants are idiopathic.
- Doing this immediately without observation can delay identification of recurrence and prompt intervention.
*Pursue urgent surgical reduction with resection of necrotic segments of bowel*
- Surgical reduction is indicated if **non-operative reduction fails**, if there are signs of **perforation**, diffuse peritonitis, or if there is clinical evidence of **bowel necrosis**.
- Since the intussusception was successfully reduced by air-contrast enema and there are no signs of perforation or necrosis currently, urgent surgery is not the immediate next step.
*Repeat barium enema q6 hrs to monitor for recurrence*
- Repeated enemas carry risks such as **radiation exposure** and potential for perforation, and are not a standard monitoring strategy for recurrence.
- Clinical observation and physical examination are generally sufficient for monitoring during the initial 24-hour period.
*Discharge to home with follow-up in 3 weeks in an outpatient pediatric gastroenterology clinic*
- Discharging the patient home so soon after reduction is unsafe due to the significant risk of **early recurrence** (especially within the first 24-48 hours) or development of complications.
- A follow-up in 3 weeks is too delayed for immediate post-reduction concerns.
Surgical vs non-surgical management US Medical PG Question 10: A 43-year-old woman comes to the physician because of a 3-month history of a painless ulcer on the sole of her right foot. There is no history of trauma. She has been dressing the ulcer once daily at home with gauze. She has a 15-year history of poorly-controlled type 1 diabetes mellitus and hypertension. Current medications include insulin and lisinopril. Vital signs are within normal limits. Examination shows a 2 x 2-cm ulcer on the plantar aspect of the base of the great toe with whitish, loose tissue on the floor of the ulcer and a calloused margin. A blunt metal probe reaches the deep plantar space. Sensation to vibration and light touch is decreased over both feet. Pedal pulses are intact. An x-ray of the right foot shows no abnormalities. Which of the following is the most appropriate initial step in management?
- A. Surgical revascularization of the right foot
- B. Amputation of the right forefoot
- C. Total contact casting of right foot
- D. Intravenous antibiotic therapy
- E. Sharp surgical debridement of the ulcer (Correct Answer)
Surgical vs non-surgical management Explanation: ***Sharp surgical debridement of the ulcer***
- The presence of a **painless ulcer**, decreased sensation (neuropathy), and a calloused margin with loose tissue indicates a **neuropathic ulcer** common in diabetic patients. **Sharp surgical debridement** is crucial to remove non-viable tissue and promote healing.
- The probe reaching the deep plantar space suggests a potential deep infection or osteomyelitis, which needs aggressive debridement to remove all infected and necrotic tissue. However, since the X-ray is normal, it is less likely to have osteomyelitis, but it needs to be ruled out by further investigations.
*Surgical revascularization of the right foot*
- This is primarily indicated for **ischemic ulcers** where blood supply is compromised.
- The patient has **intact pedal pulses**, meaning good distal blood flow, making revascularization unnecessary at this stage.
*Amputation of the right forefoot*
- Amputation is a measure of last resort for **severe, non-healing ulcers** with extensive infection or gangrene that fail to respond to conservative and surgical debridement.
- The current presentation does not warrant such an extreme intervention as a first step.
*Total contact casting of right foot*
- **Total contact casting** is used for **off-loading pressure** from a neuropathic ulcer to facilitate healing.
- While it's an important step in management, it should generally follow **debridement** to ensure a clean wound bed.
*Intravenous antibiotic therapy*
- This is indicated if there are definitive signs of **spreading infection** (e.g., cellulitis, fever, purulence).
- While debridement helps prevent infection by removing necrotic tissue, there is no mention of systemic signs of infection or severe local infection requiring immediate IV antibiotics.
More Surgical vs non-surgical management US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.