Life-threatening conditions recognition US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Life-threatening conditions recognition. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
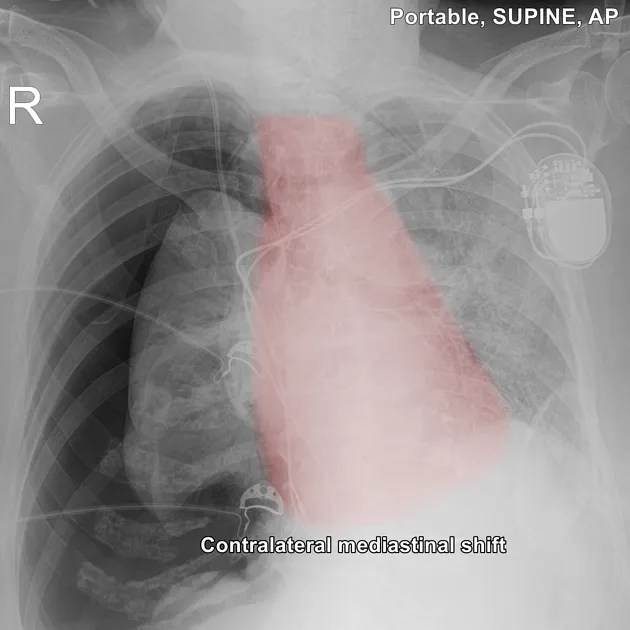
Life-threatening conditions recognition US Medical PG Question 1: A 60-year-old woman presents to the emergency department due to progressive shortness of breath and a dry cough for the past week. She notes that her symptoms are exacerbated by physical activity and relieved by rest. The woman was diagnosed with chronic kidney disease 2 years ago and was recently started on regular dialysis treatment. Her pulse rate is 105/min, blood pressure is 110/70 mm Hg, respiratory rate is 30/min, and temperature is 37.8°C (100.0°F). On examination of the respiratory system, there is dullness on percussion, decreased vocal tactile fremitus, and decreased breath sounds over the right lung base. The rest of the physical exam is within normal limits. Which of the following is the most likely cause of this patient’s symptoms?
- A. Primary spontaneous pneumothorax (PSP)
- B. Pleural effusion (Correct Answer)
- C. Acute bronchitis
- D. Pneumonia
- E. Pulmonary tuberculosis (TB)
Life-threatening conditions recognition Explanation: ***Pleural effusion***
- The patient's symptoms of **progressive shortness of breath**, **dry cough**, and physical exam findings of **dullness to percussion**, **decreased vocal tactile fremitus**, and **decreased breath sounds** over the right lung base are classic signs of a **pleural effusion**.
- Given her history of **chronic kidney disease** and recent initiation of **dialysis**, she is at high risk for fluid overload, which can lead to **transudative pleural effusions** due to **increased hydrostatic pressure**.
*Primary spontaneous pneumothorax (PSP)*
- PSP typically presents with **sudden onset of pleuritic chest pain** and **shortness of breath**, not a progressive onset over a week.
- Physical exam findings for pneumothorax include **hyperresonance to percussion** and **absent or diminished breath sounds**, but **vocal tactile fremitus would be decreased or absent**, which is similar to pleural effusion. However, the patient's presentation of gradual onset and risk factors for fluid overload point away from a PSP.
*Acute bronchitis*
- Acute bronchitis usually presents with a **productive cough**, and symptoms are often preceded by an **upper respiratory tract infection**.
- Physical exam findings typically include **wheezing** or **rhonchi**, with normal percussion and fremitus, differing from the described findings.
*Pneumonia*
- Pneumonia would typically present with a **productive cough**, **fever**, and signs of consolidation on lung exam, such as **bronchial breath sounds** and **increased vocal fremitus**, along with dullness to percussion.
- While dullness and decreased breath sounds can be present, the **decreased vocal tactile fremitus** observed here strongly suggests fluid in the pleural space rather than consolidation.
*Pulmonary tuberculosis (TB)*
- Pulmonary TB often presents with **chronic cough (often productive)**, **night sweats**, **weight loss**, and **low-grade fever**, which are not the primary symptoms described.
- While CXR findings can vary, the acute presentation with clear signs of fluid accumulation in a patient with kidney disease makes TB less likely without other predisposing factors or prolonged symptomatology.
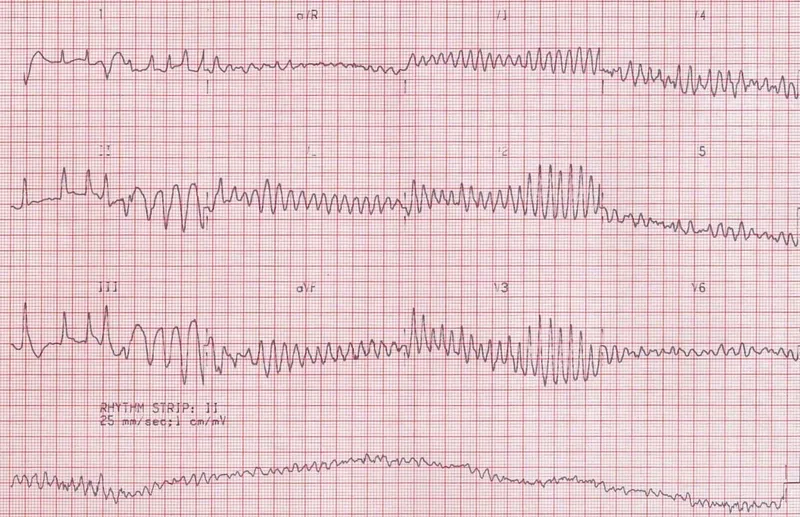
Life-threatening conditions recognition US Medical PG Question 2: One hour after being admitted to the hospital for sharp, acute chest pain and diaphoresis, a 55-year-old woman with type 2 diabetes mellitus loses consciousness in the emergency department. There are no palpable pulses. Chest compressions are started. The patient has a history of breast cancer that was surgically treated 4 years ago. Prior to admission, the patient was on a long bus ride to visit her sister. Her medications include tamoxifen, atorvastatin, metoprolol, metformin, and insulin. Serum troponin levels are elevated. The cardiac rhythm is shown. Which of the following is the most appropriate next step in management?
- A. Defibrillation (Correct Answer)
- B. Coronary angiography
- C. Intravenous dextrose therapy
- D. Intravenous epinephrine therapy
- E. Intravenous glucagon therapy
Life-threatening conditions recognition Explanation: ***Defibrillation***
- The ECG shows **ventricular fibrillation (VF)**, characterized by chaotic, disorganized electrical activity with no identifiable QRS complexes and no palpable pulse. VF is a **shockable rhythm**.
- According to ACLS guidelines, the immediate management for VF is **unsynchronized defibrillation** along with high-quality chest compressions.
- Defibrillation depolarizes the myocardium simultaneously, allowing the sinoatrial node to potentially resume normal electrical activity and restore organized cardiac rhythm.
- For refractory VF after initial shocks, epinephrine and antiarrhythmics (amiodarone or lidocaine) are added.
*Intravenous epinephrine therapy*
- Epinephrine is a vasopressor used in cardiac arrest to increase coronary and cerebral perfusion pressure.
- While epinephrine is given during VF arrest, it is administered **after** the initial defibrillation attempts, not as the immediate first step.
- Epinephrine is the primary drug for **non-shockable rhythms** (PEA and asystole), but defibrillation takes priority in shockable rhythms like VF.
*Intravenous glucagon therapy*
- Glucagon is used for severe **hypoglycemia** or **beta-blocker/calcium channel blocker overdose**.
- While the patient takes metoprolol (a beta-blocker), the clinical presentation with elevated troponin, chest pain, and VF rhythm clearly indicates an acute cardiac event, not beta-blocker toxicity.
- Glucagon has no role in the immediate management of cardiac arrest from VF.
*Coronary angiography*
- Coronary angiography is indicated for **post-cardiac arrest care** after return of spontaneous circulation (ROSC), especially in patients with suspected acute coronary syndrome.
- The patient has elevated troponin suggesting acute MI, making early angiography important **after** successful resuscitation.
- However, angiography cannot be performed during active cardiac arrest; immediate defibrillation and CPR are required first.
*Intravenous dextrose therapy*
- Dextrose is used to treat **hypoglycemia**.
- While the patient has diabetes and takes insulin (hypoglycemia risk), the presentation with chest pain, elevated troponin, and VF rhythm indicates acute coronary syndrome with cardiac arrest.
- Hypoglycemia does not cause VF; the rhythm is consistent with ischemic cardiac arrest requiring immediate defibrillation.
Life-threatening conditions recognition US Medical PG Question 3: A 65-year-old man presents to the emergency department for sudden weakness. He was doing mechanical work on his car where he acutely developed right-leg weakness and fell to the ground. He is accompanied by his wife, who said that this has never happened before. He was last seen neurologically normal approximately 2 hours prior to presentation. His past medical history is significant for hypertension and type II diabetes. His temperature is 98.8°F (37.1°C), blood pressure is 177/108 mmHg, pulse is 90/min, respirations are 15/min, and oxygen saturation is 99% on room air. Neurological exam reveals that he is having trouble speaking and has profound weakness of his right upper and lower extremity. Which of the following is the best next step in management?
- A. Thrombolytics
- B. Noncontrast head CT (Correct Answer)
- C. CT angiogram
- D. MRI of the head
- E. Aspirin
Life-threatening conditions recognition Explanation: ***Noncontrast head CT***
- A **noncontrast head CT** is the most crucial initial step in managing acute stroke symptoms because it can rapidly rule out an **intracranial hemorrhage**.
- Distinguishing between ischemic stroke and hemorrhagic stroke is critical, as the management strategies are vastly different and administering thrombolytics in the presence of hemorrhage can be fatal.
*Thrombolytics*
- **Thrombolytics** can only be administered after an **intracranial hemorrhage** has been excluded via noncontrast head CT.
- Administering thrombolytics without imaging could worsen a hemorrhagic stroke, causing significant harm or death.
*CT angiogram*
- A **CT angiogram** is used to identify large vessel occlusions in ischemic stroke and is typically performed after a noncontrast CT rules out hemorrhage.
- This imaging is crucial for determining eligibility for **endovascular thrombectomy** but is not the very first diagnostic step.
*MRI of the head*
- An **MRI of the head** is more sensitive for detecting acute ischemic changes but takes longer to perform and is often not readily available in the acute emergency setting.
- It is not the initial imaging of choice for ruling out hemorrhage due to its longer acquisition time compared to CT.
*Aspirin*
- **Aspirin** is indicated for acute ischemic stroke but should only be given after an **intracranial hemorrhage** has been ruled out.
- Like thrombolytics, aspirin could exacerbate a hemorrhagic stroke and is thus deferred until initial imaging is complete.
Life-threatening conditions recognition US Medical PG Question 4: A 25-year-old woman presents to the emergency department with fatigue and weakness. She states over the past 24 hours she has not felt like herself and has felt like she has no strength. The patient has no significant past medical history other than a single episode of blood-tinged diarrhea 1 week ago which resolved on its own. Her temperature is 99.4°F (37.4°C), blood pressure is 124/62 mmHg, pulse is 95/min, respirations are 29/min, and oxygen saturation is 95% on room air. Physical exam is notable for 2/5 strength of the lower extremities and decreased sensation in the lower extremities and finger tips. Which of the following is the best initial step in management?
- A. IV immunoglobulin
- B. Dexamethasone
- C. Spirometry (Correct Answer)
- D. Intubation
- E. Pyridostigmine
Life-threatening conditions recognition Explanation: ***Spirometry***
- The patient's symptoms (fatigue, weakness, decreased strength, and sensation in extremities) following a gastrointestinal infection are highly suggestive of **Guillain-Barré Syndrome (GBS)**.
- **Spirometry** is the most critical initial step to assess respiratory function, as **respiratory muscle weakness** is the primary cause of morbidity and mortality in GBS.
*IV immunoglobulin*
- While **intravenous immunoglobulin (IVIG)** is a treatment for GBS, it is not the *initial* management step.
- The immediate priority in suspected GBS is to assess and stabilize the patient's respiratory status, not to initiate definitive treatment.
*Dexamethasone*
- **Corticosteroids** like dexamethasone have **not been shown to be effective** in treating GBS and may even prolong recovery in some cases.
- Their use is generally avoided in the management of GBS.
*Intubation*
- **Intubation** is indicated if spirometry reveals rapidly declining or severely compromised respiratory function, but it is not the *initial* step.
- An assessment of respiratory capacity via spirometry should precede intubation unless acute respiratory failure is immediately apparent.
*Pyridostigmine*
- **Pyridostigmine** is an anticholinesterase inhibitor used primarily for the symptomatic treatment of **myasthenia gravis**.
- It is not indicated for the management of GBS, which involves a different pathophysiological mechanism.
Life-threatening conditions recognition US Medical PG Question 5: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Life-threatening conditions recognition Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Life-threatening conditions recognition US Medical PG Question 6: A 28-year-old man is admitted to the emergency department with a gunshot wound to the abdomen. He complains of weakness and diffuse abdominal pain. Morphine is administered and IV fluids are started by paramedics at the scene. On admission, the patient’s blood pressure is 90/60 mm Hg, heart rate is 103/min, respiratory rate is 17/min, the temperature is 36.2℃ (97.1℉), and oxygen saturation is 94% on room air. The patient is responsive but lethargic. The patient is diaphoretic and extremities are pale and cool. Lungs are clear to auscultation. Cardiac sounds are diminished. Abdominal examination shows a visible bullet entry wound in the left upper quadrant (LUQ) with no corresponding exit wound on the flanks or back. The abdomen is distended and diffusely tender with a rebound. Aspiration of the nasogastric tube reveals bloody contents. Rectal examination shows no blood. Stool guaiac is negative. Which of the following is the next best step in management?
- A. Focused assessment with sonography for trauma (FAST)
- B. Abdominal CT
- C. Exploratory laparotomy (Correct Answer)
- D. Abdominal X-ray
- E. Diagnostic peritoneal lavage
Life-threatening conditions recognition Explanation: ***Exploratory laparotomy***
- The patient presents with clear signs of **hemodynamic instability** (BP 90/60 mmHg, HR 103/min, lethargy, cool extremities, diminished cardiac sounds) following a **gunshot wound to the abdomen**.
- In hemodynamically unstable trauma patients with penetrating abdominal injuries, immediate **exploratory laparotomy** is indicated to identify and control hemorrhage and repair organ damage.
*Focused assessment with sonography for trauma (FAST)*
- While FAST can detect free fluid (e.g., blood) in the abdomen, it is **not sufficient to rule out significant injury** in a hemodynamically unstable patient with a penetrating abdominal wound.
- A positive FAST in a stable patient might prompt further imaging, but in this unstable case, it would delay definitive surgical intervention.
*Abdominal CT*
- Abdominal CT is useful for evaluating intra-abdominal injuries in **hemodynamically stable** patients.
- Performing a CT on this unstable patient would delay critical surgical intervention and could lead to rapid deterioration in the scanner.
*Abdominal X-ray*
- An abdominal X-ray can sometimes identify the **location of a bullet** or **free air** under the diaphragm, but it has limited utility in assessing or quantifying intra-abdominal hemorrhage or solid organ injury.
- It is not the definitive diagnostic or therapeutic step for an unstable patient with a penetrating abdominal injury.
*Diagnostic peritoneal lavage*
- DPL is an invasive procedure that can detect intra-abdominal bleeding or perforation, but it has largely been **replaced by FAST and CT scans** in hemodynamically stable patients.
- For a hemodynamically unstable patient with a clear indication for surgery (penetrating trauma and instability), DPL would delay definitive surgical management and provides less information than direct visualization via laparotomy.
More Life-threatening conditions recognition US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.