Critical care interventions US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Critical care interventions. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Critical care interventions US Medical PG Question 1: A 28-year-old soldier is brought back to a military treatment facility 45 minutes after sustaining injuries in a building fire from a mortar attack. He was trapped inside the building for around 20 minutes. On arrival, he is confused and appears uncomfortable. He has a Glasgow Coma Score of 13. His pulse is 113/min, respirations are 18/min, and blood pressure is 108/70 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 96%. Examination shows multiple second-degree burns over the chest and bilateral upper extremities and third-degree burns over the face. There are black sediments seen within the nose and mouth. The lungs are clear to auscultation. Cardiac examination shows no abnormalities. The abdomen is soft and nontender. Intravenous fluid resuscitation is begun. Which of the following is the most appropriate next step in management?
- A. Insertion of nasogastric tube and enteral nutrition
- B. Intravenous antibiotic therapy
- C. Intubation and mechanical ventilation (Correct Answer)
- D. Immediate bronchoscopy
- E. Intravenous corticosteroid therapy
Critical care interventions Explanation: ***Intubation and mechanical ventilation***
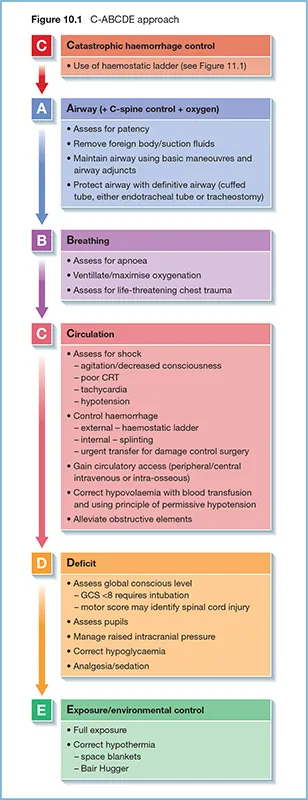
- The patient exhibits several signs of impending **airway compromise** due to **inhalation injury**, including perioral burns, black sediments in the nose and mouth, and being trapped in a fire.
- While current oxygen saturation is 96%, **airway edema** can rapidly worsen, leading to respiratory failure. **Early intubation** is crucial to secure the airway before it becomes obstructed.
*Insertion of nasogastric tube and enteral nutrition*
- A nasogastric tube is often placed in burn patients to decompress the stomach and provide nutritional support, but it is **not the immediate priority** when there is a risk of airway obstruction.
- **Enteral nutrition** is important but should be initiated only after airway control is established and the patient is stable for feeding.
*Intravenous antibiotic therapy*
- **Prophylactic antibiotics** are generally **not recommended** in the immediate management of burn patients unless there is clear evidence of infection, which is not present here.
- Unnecessary antibiotic use can lead to **antibiotic resistance** and fungal infections.
*Immediate bronchoscopy*
- While **bronchoscopy** can confirm the extent of inhalation injury, it is not the primary immediate step. **Securing the airway** through intubation takes precedence over diagnostic procedures when airway compromise is imminent.
- Bronchoscopy can be considered *after* intubation to assess the lower airway for damage and guide further management.
*Intravenous corticosteroid therapy*
- **Corticosteroids** are typically **contraindicated** in the management of inhalation injury because they can **impair immune function** and increase the risk of infection in burn patients.
- Evidence does not support the routine use of corticosteroids to reduce inflammation in inhalation injury, and they may worsen outcomes.
Critical care interventions US Medical PG Question 2: A 36-year-old male with fluctuating levels of consciousness is brought to the emergency department by ambulance due to a fire in his home. He currently opens his eyes to voice, localizes painful stimuli, responds when asked questions, but is disoriented and cannot obey commands. The patient’s temperature is 99°F (37.2°C), blood pressure is 86/52 mmHg, pulse is 88/min, and respirations are 14/min with an oxygen saturation of 97% O2 on room air. Physical exam shows evidence of soot around the patient’s nose and mouth, but no burns, airway obstruction, nor accessory muscle use. A blood lactate is 14 mmol/L. The patient is started on intravenous fluids.
What is the next best step in management?
- A. Methylene blue
- B. Hyperbaric oxygen
- C. Sodium thiosulfate and sodium nitrite
- D. Intravenous epinephrine
- E. 100% oxygen, hydroxycobalamin, and sodium thiosulfate (Correct Answer)
Critical care interventions Explanation: ***100% oxygen, hydroxycobalamin, and sodium thiosulfate***
- This patient presents with signs of both **carbon monoxide poisoning** (fire exposure, disoriented, altered mental status) and **cyanide poisoning** (fire exposure, very high lactate, normal oxygen saturation despite altered mental status). This combination therapy directly addresses both.
- **100% oxygen** competes with carbon monoxide for hemoglobin binding and helps clear it, while **hydroxycobalamin** and **sodium thiosulfate** are antidotes for cyanide poisoning, converting cyanide into less toxic compounds.
*Methylene blue*
- **Methylene blue** is used to treat **methemoglobinemia**, a condition where iron in hemoglobin is oxidized, leading to impaired oxygen transport.
- The patient's symptoms (fire exposure, altered mental status, and a high lactate with normal SpO2) are not characteristic of methemoglobinemia, but rather strong indicators of carbon monoxide and cyanide poisoning.
*Hyperbaric oxygen*
- **Hyperbaric oxygen** is a treatment for severe carbon monoxide poisoning, but it is not the initial or sole treatment for a patient with suspected co-existing cyanide poisoning.
- While recommended for **severe CO poisoning**, it doesn't directly address cyanide toxicity, which is suggested by the metabolic acidosis with a high lactate level despite normal oxygen saturation.
*Sodium thiosulfate and sodium nitrite*
- This combination (the **Lilly kit**) is traditionally used to treat **cyanide poisoning**, with sodium nitrite inducing methemoglobinemia to sequester cyanide, and sodium thiosulfate aiding its excretion.
- The patient also requires treatment for **carbon monoxide poisoning**, and hydroxycobalamin is generally preferred over sodium nitrite as it does not induce methemoglobinemia, which can worsen hypoxia in CO poisoning.
*Intravenous epinephrine*
- **Epinephrine** is a powerful vasoconstrictor and bronchodilator primarily used to treat **anaphylaxis** or **cardiac arrest**.
- There is no indication of anaphylaxis or cardiac arrest in this patient, and epinephrine would not be an appropriate treatment for carbon monoxide or cyanide poisoning.
Critical care interventions US Medical PG Question 3: A 19-year-old man is rushed to the emergency department 30 minutes after diving head-first into a shallow pool of water from a cliff. He was placed on a spinal board and a rigid cervical collar was applied by the emergency medical technicians. On arrival, he is unconscious and withdraws all extremities to pain. His temperature is 36.7°C (98.1°F), pulse is 70/min, respirations are 8/min, and blood pressure is 102/70 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 96%. The pupils are equal and react sluggishly to light. There is a 3-cm (1.2-in) laceration over the forehead. The lungs are clear to auscultation. Cardiac examination shows no abnormalities. The abdomen is soft and nontender. There is a step-off palpated over the cervical spine. Which of the following is the most appropriate next step in management?
- A. Rapid sequence intubation (Correct Answer)
- B. CT scan of the spine
- C. X-ray of the cervical spine
- D. MRI of the spine
- E. Rectal tone assessment
Critical care interventions Explanation: ***Rapid sequence intubation***
- The patient has a **compromised airway** due to very shallow respirations (8/min), indicating impending respiratory failure, which is prioritized in the management of trauma patients.
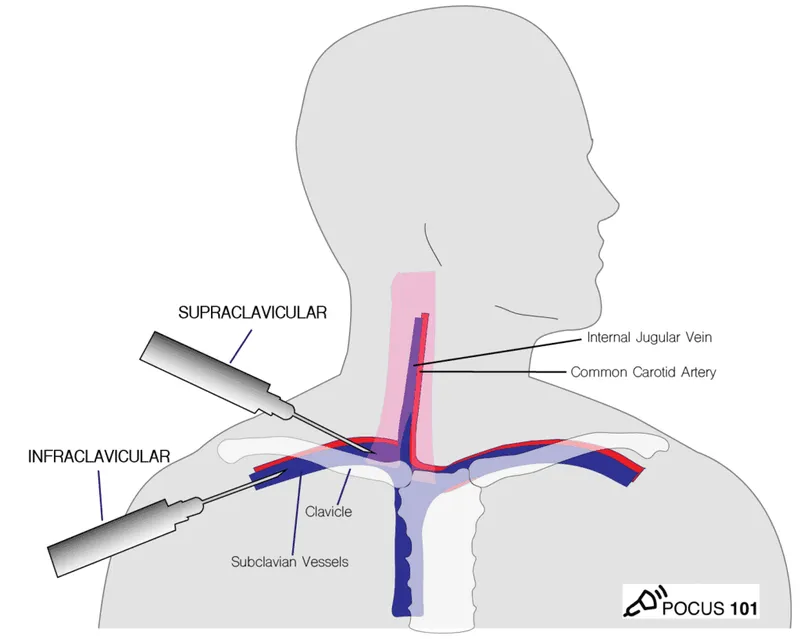
- Due to the high suspicion of a **cervical spine injury** (diving into a shallow pool, step-off palpable over the cervical spine), **rapid sequence intubation** is the safest way to secure the airway while maintaining **cervical spine immobilization**.
*CT scan of the spine*
- Imaging studies of the spine are important for diagnosis but must be performed **after securing the airway** and stabilizing vital functions.
- While a CT scan is the preferred imaging modality for evaluating bony spinal trauma, it does not address the immediate life-threatening issue of respiratory insufficiency.
*X-ray of the cervical spine*
- X-rays are less sensitive for detecting all types of cervical spine injuries, especially ligamentous damage, compared to CT or MRI.
- As with other imaging, it should be done **after airway management** is secured.
*MRI of the spine*
- MRI is excellent for evaluating **soft tissue structures** like spinal cord, ligaments, and discs, and is generally performed after initial stabilization and CT for bony injury.
- It is not an immediate diagnostic priority when the patient's airway and breathing are acutely compromised.
*Rectal tone assessment*
- This assessment is part of the neurological examination to evaluate for spinal cord injury, specifically involving the **sacral segments**.
- While important for comprehensive neurological assessment, it is not the most appropriate *next step* when the patient has critical airway and breathing compromise.
Critical care interventions US Medical PG Question 4: A 46-year-old male was found unconscious in the field and brought to the emergency department by EMS. The patient was intubated in transit and given a 2 liter bolus of normal saline. On arrival, the patient's blood pressure is 80/60 mmHg and temperature is 37.5°C. Jugular veins are flat and capillary refill time is 4 seconds.
Vascular parameters are measured and are as follows:
Cardiac index - Low
Pulmonary capillary wedge pressure (PCWP) - Low
Systemic vascular resistance - High
Which of the following is the most likely diagnosis?
- A. Septic shock
- B. Anaphylactic shock
- C. Cardiogenic shock
- D. Hypovolemic shock (Correct Answer)
- E. Neurogenic shock
Critical care interventions Explanation: ***Hypovolemic shock***
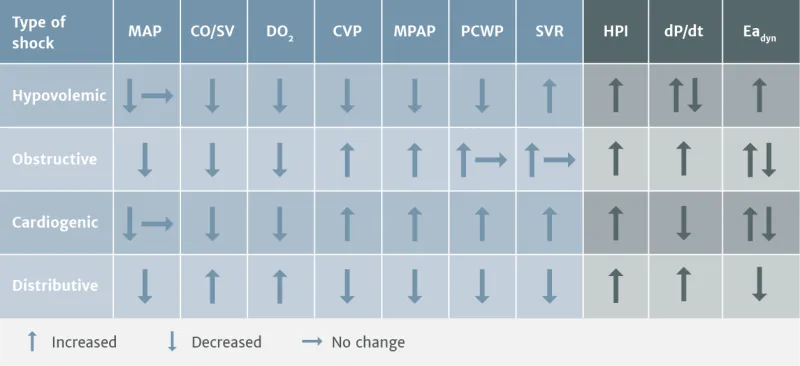
- The patient presents with **hypotension**, **flat jugular veins**, **prolonged capillary refill**, and a **low cardiac index** and **low pulmonary capillary wedge pressure (PCWP)**, all indicative of inadequate intravascular volume.
- The **high systemic vascular resistance** is a compensatory mechanism to maintain blood pressure in the setting of decreased circulating volume.
*Septic shock*
- Septic shock typically presents with **vasodilation**, leading to a **low systemic vascular resistance**, which contradicts the findings in this patient.
- While patients can be hypotensive, the vascular parameters, especially SVR, do not align with septic shock.
*Anaphylactic shock*
- This type of shock is characterized by widespread **vasodilation** and increased capillary permeability, leading to a **low systemic vascular resistance** and often significant **edema** or **urticaria**, none of which are suggested here.
- While it can cause hypotension and low PCWP due to fluid shifts, the high SVR makes it less likely.
*Cardiogenic shock*
- Cardiogenic shock is characterized by **pump failure**, leading to a **low cardiac index** but a **high PCWP** due to fluid backup in the pulmonary circulation.
- This directly contrasts the patient's low PCWP.
*Neurogenic shock*
- Neurogenic shock involves a loss of **sympathetic tone**, resulting in widespread **vasodilation** and a **low systemic vascular resistance**, often accompanied by **bradycardia**.
- The high SVR in this patient rules out neurogenic shock.
Critical care interventions US Medical PG Question 5: A 35-year-old man is brought to the emergency department from a kitchen fire. The patient was cooking when boiling oil splashed on his exposed skin. His temperature is 99.7°F (37.6°C), blood pressure is 127/82 mmHg, pulse is 120/min, respirations are 12/min, and oxygen saturation is 98% on room air. He has dry, nontender, and circumferential burns over his arms bilaterally, burns over the anterior portion of his chest and abdomen, and tender spot burns with blisters on his shins. A 1L bolus of normal saline is administered and the patient is given morphine and his pulse is subsequently 80/min. A Foley catheter is placed which drains 10 mL of urine. What is the best next step in management?
- A. Additional fluids and escharotomy (Correct Answer)
- B. Escharotomy
- C. Continuous observation
- D. Moist dressings and discharge
- E. Additional fluids and admission to the ICU
Critical care interventions Explanation: ***Additional fluids and escharotomy***
- The patient has **circumferential full-thickness burns** on both arms (dry, nontender), which require **escharotomy** to prevent compartment syndrome and vascular compromise to the limbs.
- The **oliguria** (10 mL urine output) despite a 1L fluid bolus indicates **inadequate fluid resuscitation** from burn shock. With approximately 40% TBSA burns, the patient requires aggressive fluid resuscitation per the Parkland formula (4 mL/kg/% TBSA), which would be approximately 11 liters in the first 24 hours. Adequate resuscitation targets urine output of 0.5-1 mL/kg/hr (35-70 mL/hr for this patient).
- Both interventions are immediately necessary: fluids for burn shock and escharotomy for circumferential burns.
*Escharotomy*
- While **escharotomy** is essential for the circumferential full-thickness burns to prevent compartment syndrome, it alone will not address the **severe fluid deficit** causing oliguria and hypoperfusion.
- The low urine output reflects systemic hypovolemia from burn shock, not just local compartment issues, requiring aggressive fluid resuscitation.
*Continuous observation*
- **Continuous observation** is inappropriate given the patient's critical findings: circumferential full-thickness burns requiring urgent escharotomy and oliguria indicating inadequate resuscitation.
- Delaying escharotomy can lead to irreversible ischemic damage to the limbs, and inadequate fluid resuscitation can progress to multiorgan failure.
*Moist dressings and discharge*
- This option is completely inappropriate for a patient with **extensive deep burns** (approximately 40% TBSA) including full-thickness injuries requiring hospitalization and specialized burn care.
- Discharge would lead to severe complications including infection, inadequate fluid resuscitation, compartment syndrome, and potential limb loss.
*Additional fluids and admission to the ICU*
- While ICU admission and additional fluids are necessary components of care, this option is **incomplete** because it omits **escharotomy**, which is urgently needed for the circumferential full-thickness burns.
- Escharotomy is a time-sensitive procedure that must be performed promptly to prevent ischemic injury to the limbs from vascular compromise.
Critical care interventions US Medical PG Question 6: A 70-year-old man is brought to the emergency room with complaints of severe substernal chest pain for the last hour. The pain started suddenly, and the patient describes the pain as “going into the shoulder”. The patient took aspirin at home and has been given multiple doses of sublingual nitroglycerin, but the pain has not subsided. He has a blood pressure of 112/84 mm Hg, the pulse is 63/min, the respiratory rate is 18/min, and the temperature is 36.9°C (98.0°F). Cardiac auscultation reveals normal S1 and S2 sounds, however, an additional S4 sound is heard. The patient is sweating profusely, and the lungs are clear to auscultation. No jugular venous distension or pedal edema is observed. His initial ECG shows ST elevation in leads II, III, and aVF. Which of the following will likely have the most benefit in this patient?
- A. Antiarrhythmics
- B. Percutaneous coronary intervention (Correct Answer)
- C. Thrombolytics
- D. Beta blockers
- E. Clopidogrel
Critical care interventions Explanation: ***Percutaneous coronary intervention***
- This patient is experiencing a **ST-elevation myocardial infarction (STEMI)**, indicated by severe chest pain radiating to the shoulder, no relief with nitroglycerin, and ST elevation in leads II, III, and aVF.
- **Reperfusion therapy** is crucial for STEMI, and PCI is the preferred method when available within the recommended timeframe (typically <90-120 minutes from first medical contact) as it directly opens the occluded coronary artery.
*Antiarrhythmics*
- While **arrhythmias** can occur during an MI, there is no indication that the patient is currently experiencing a life-threatening arrhythmia requiring immediate antiarrhythmic drug administration.
- The primary goal in STEMI is **reperfusion**, not immediate arrhythmia suppression unless the arrhythmia is hemodynamically unstable.
*Thrombolytics*
- **Thrombolytics (fibrinolytics)** are an alternative reperfusion strategy for STEMI if PCI is not available or cannot be performed within the recommended timeframe.
- Given that the question asks for the "most benefit," and PCI is generally superior to thrombolytics in terms of complete reperfusion and clinical outcomes when available promptly, thrombolytics would not be the first choice.
*Beta blockers*
- **Beta blockers** are important for managing MI by reducing myocardial oxygen demand and preventing arrhythmias; however, they are often initiated after reperfusion and careful patient evaluation, especially in the acute phase of STEMI where immediate reperfusion is paramount.
- They should be used with caution if there are signs of **heart failure** or **cardiogenic shock**, which are not present here but still highlight that it's not the immediate, most beneficial intervention.
*Clopidogrel*
- **Clopidogrel** is an antiplatelet agent that would be part of the medical management for STEMI, along with aspirin and anticoagulants, to prevent further clot formation.
- While important, it is an adjunctive therapy and does not directly address the need for **rapid reperfusion** to restore blood flow to the ischemic myocardium, which is the most critical intervention in STEMI.
More Critical care interventions US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.