Airway, Breathing, Circulation priorities US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Airway, Breathing, Circulation priorities. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Airway, Breathing, Circulation priorities US Medical PG Question 1: A 45-year-old man was a driver in a motor vehicle collision. The patient is not able to offer a medical history during initial presentation. His temperature is 97.6°F (36.4°C), blood pressure is 104/74 mmHg, pulse is 150/min, respirations are 12/min, and oxygen saturation is 98% on room air. On exam, he does not open his eyes, he withdraws to pain, and he makes incomprehensible sounds. He has obvious signs of trauma to the chest and abdomen. His abdomen is distended and markedly tender to palpation. He also has an obvious open deformity of the left femur. What is the best initial step in management?
- A. Emergency open fracture repair
- B. Packed red blood cells
- C. Exploratory laparotomy
- D. Intubation (Correct Answer)
- E. 100% oxygen
Airway, Breathing, Circulation priorities Explanation: ***Intubation***
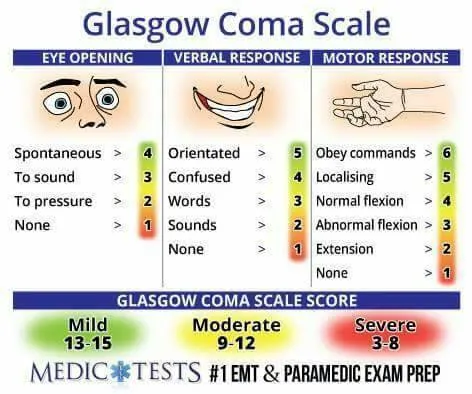
- The patient's **Glasgow Coma Scale (GCS) score is 7** (E=1, V=2, M=4), which is below 8 and indicates a severe head injury needing **airway protection** via intubation.
- A GCS ≤ 8 mandates **definitive airway management** to prevent aspiration and ensure adequate ventilation.
*Emergency open fracture repair*
- While the patient has an open femur fracture, it is not the most immediate life-threatening concern after a major trauma; **airway and breathing** take precedence.
- **Hemorrhage control** and **stabilization** often precede definitive orthopedic repair in polytrauma.
*Packed red blood cells*
- Although the patient is likely in **hemorrhagic shock** (tachycardia, hypotension, obvious trauma), administering blood products without first securing the airway is not the initial priority.
- **Circulation** management, including fluid resuscitation and blood products, follows **airway and breathing** establishment.
*Exploratory laparotomy*
- The patient's distended and tender abdomen strongly suggests intra-abdominal injury, but this is a **diagnostic and therapeutic procedure** that comes after initial resuscitation and stabilization.
- **Emergent laparotomy** for abdominal trauma is considered once the patient's airway, breathing, and circulation are secured.
*100% oxygen*
- Administering 100% oxygen is part of initial resuscitation, but it does not address the fundamental problem of an unsecured airway and the risk of **hypoventilation** or **aspiration** in a patient with a GCS of 7.
- Oxygen supplementation helps improve saturation in spontaneously breathing patients but cannot protect a compromised airway.
Airway, Breathing, Circulation priorities US Medical PG Question 2: A 47-year-old man is brought to the emergency room by his wife. She states that they were having dinner at a restaurant when the patient suddenly became out of breath. His past medical history is irrelevant but has a 20-year pack smoking history. On evaluation, the patient is alert and verbally responsive but in moderate respiratory distress. His temperature is 37°C (98.6°F), blood pressure is 85/56 mm Hg, pulse is 102/min, and respirations are 20/min. His oxygen saturation is 88% on 2L nasal cannula. An oropharyngeal examination is unremarkable. The trachea is deviated to the left. Cardiopulmonary examination reveals decreased breath sounds on the right lower lung field with nondistended neck veins. Which of the following is the next best step in the management of this patient?
- A. Urgent needle decompression (Correct Answer)
- B. D-dimer levels
- C. Nebulization with albuterol
- D. Chest X-ray
- E. Heimlich maneuver
Airway, Breathing, Circulation priorities Explanation: ***Urgent needle decompression***
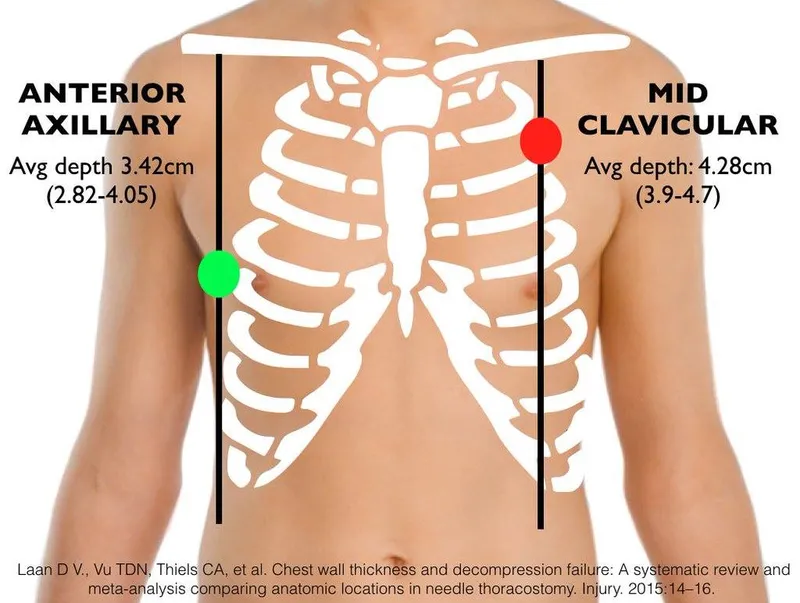
- The patient presents with sudden onset **respiratory distress**, **tracheal deviation** to the left (away from the affected right side), **decreased breath sounds** on the right, and **hypotension** with **tachycardia**. These are classic signs of a **tension pneumothorax**, which requires immediate needle decompression.
- This is a life-threatening emergency where air accumulates in the pleural space under positive pressure, collapsing the lung and shifting mediastinal structures, compromising venous return to the heart.
*D-dimer levels*
- While helpful in the workup for pulmonary embolism, **D-dimer levels** are not relevant as the immediate next step for a patient in acute respiratory distress with clear signs of tracheal deviation and decreased breath sounds, which points toward a mechanical lung issue.
- The patient's presentation with acute, severe respiratory symptoms and hemodynamic instability mandates immediate life-saving intervention.
*Nebulization with albuterol*
- **Albuterol** is used for bronchospasm, as seen in asthma or COPD exacerbations. This patient's symptoms are sudden and severe, with clear signs of a **tension pneumothorax**, which would not respond to bronchodilators.
- There is no indication of wheezing or a history of reactive airway disease to suggest this as a primary treatment.
*Chest X-ray*
- A **chest X-ray** would confirm the diagnosis of tension pneumothorax. However, given the patient's severe respiratory distress, hypotension, and classic physical findings (tracheal deviation, absent breath sounds), performing an X-ray would delay life-saving intervention.
- In a true tension pneumothorax, diagnosis is clinical, and immediate intervention takes precedence over imaging.
*Heimlich maneuver*
- The **Heimlich maneuver** is indicated for foreign body airway obstruction. The patient is verbally responsive, which indicates a patent airway, and there are no direct signs of choking on food.
- Although the patient was having dinner, the distinct clinical signs of **tracheal deviation** and unilateral decreased breath sounds do not support an airway obstruction requiring the Heimlich maneuver.
Airway, Breathing, Circulation priorities US Medical PG Question 3: A 27-year-old man is brought to the emergency department 45 minutes after being involved in a motor vehicle collision. He is agitated. He has pain in his upper right arm, which he is cradling in his left arm. His temperature is 36.7°C (98°F), pulse is 135/min, respirations are 25/min, and blood pressure is 145/90 mm Hg. His breathing is shallow. Pulse oximetry on 100% oxygen via a non-rebreather face mask shows an oxygen saturation of 83%. He is confused and oriented only to person. Examination shows multiple bruises on the right anterior thoracic wall. The pupils are equal and reactive to light. On inspiration, his right chest wall demonstrates paradoxical inward movement while his left chest wall is expanding. There is pain to palpation and crepitus over his right anterior ribs. The remainder of the examination shows no abnormalities. An x-ray of the chest is shown. Two large-bore IVs are placed. After fluid resuscitation and analgesia, which of the following is the most appropriate next step in management?
- A. Bedside thoracotomy
- B. Surgical fixation of right third to sixth ribs
- C. Intubation with positive pressure ventilation (Correct Answer)
- D. Placement of a chest tube
- E. CT scan of the chest
Airway, Breathing, Circulation priorities Explanation: ***Intubation with positive pressure ventilation***
- The patient presents with **flail chest** (paradoxical chest wall movement with pain and crepitus), respiratory distress (tachypnea, shallow breathing), and **hypoxemia** (SpO2 83% on 100% oxygen) despite initial fluid resuscitation and analgesia. These are clear indications for **endotracheal intubation** and mechanical ventilation to stabilize the chest wall, improve oxygenation, and reduce the work of breathing.
- **Positive pressure ventilation** helps to internally splint the flail segment, enabling more effective gas exchange and preventing further atelectasis.
*Bedside thoracotomy*
- **Bedside thoracotomy** is typically reserved for patients in traumatic cardiac arrest who have witnessed signs of life on arrival or are in profound shock unresponsive to other resuscitative measures, making it inappropriate here.
- This patient is **hemodynamically stable** (BP 145/90 mmHg) and does not show signs of massive hemorrhage or cardiac tamponade requiring immediate thoracotomy.
*Surgical fixation of right third to sixth ribs*
- **Surgical fixation of rib fractures** is a more definitive treatment for flail chest but is not an immediate life-saving intervention in the setting of acute respiratory failure and hypoxemia.
- While it can be considered later to reduce pain and improve pulmonary mechanics, the priority is to stabilize the patient's respiratory status through **ventilation**.
*Placement of a chest tube*
- **Placement of a chest tube** is indicated for pneumothorax, hemothorax, or empyema. While a pneumothorax or hemothorax could be present given the trauma and rib fractures, the primary issue driving this patient's acute respiratory failure is the **flail chest leading to inadequate ventilation and oxygenation**.
- There is no mention of diminished breath sounds or hyperresonance/dullness to percussion, which would suggest pneumothorax or hemothorax as the primary and immediate problem after initial resuscitation.
*CT scan of the chest*
- A **CT scan of the chest** is an important diagnostic tool to assess the extent of injuries, but it is not an immediate therapeutic intervention for a patient in acute respiratory failure and severe hypoxemia.
- Delaying definitive airway management for a diagnostic test in an unstable patient is **inappropriate** and could worsen the patient's condition.
Airway, Breathing, Circulation priorities US Medical PG Question 4: A 28-year-old soldier is brought back to a military treatment facility 45 minutes after sustaining injuries in a building fire from a mortar attack. He was trapped inside the building for around 20 minutes. On arrival, he is confused and appears uncomfortable. He has a Glasgow Coma Score of 13. His pulse is 113/min, respirations are 18/min, and blood pressure is 108/70 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 96%. Examination shows multiple second-degree burns over the chest and bilateral upper extremities and third-degree burns over the face. There are black sediments seen within the nose and mouth. The lungs are clear to auscultation. Cardiac examination shows no abnormalities. The abdomen is soft and nontender. Intravenous fluid resuscitation is begun. Which of the following is the most appropriate next step in management?
- A. Insertion of nasogastric tube and enteral nutrition
- B. Intravenous antibiotic therapy
- C. Intubation and mechanical ventilation (Correct Answer)
- D. Immediate bronchoscopy
- E. Intravenous corticosteroid therapy
Airway, Breathing, Circulation priorities Explanation: ***Intubation and mechanical ventilation***
- The patient exhibits several signs of impending **airway compromise** due to **inhalation injury**, including perioral burns, black sediments in the nose and mouth, and being trapped in a fire.
- While current oxygen saturation is 96%, **airway edema** can rapidly worsen, leading to respiratory failure. **Early intubation** is crucial to secure the airway before it becomes obstructed.
*Insertion of nasogastric tube and enteral nutrition*
- A nasogastric tube is often placed in burn patients to decompress the stomach and provide nutritional support, but it is **not the immediate priority** when there is a risk of airway obstruction.
- **Enteral nutrition** is important but should be initiated only after airway control is established and the patient is stable for feeding.
*Intravenous antibiotic therapy*
- **Prophylactic antibiotics** are generally **not recommended** in the immediate management of burn patients unless there is clear evidence of infection, which is not present here.
- Unnecessary antibiotic use can lead to **antibiotic resistance** and fungal infections.
*Immediate bronchoscopy*
- While **bronchoscopy** can confirm the extent of inhalation injury, it is not the primary immediate step. **Securing the airway** through intubation takes precedence over diagnostic procedures when airway compromise is imminent.
- Bronchoscopy can be considered *after* intubation to assess the lower airway for damage and guide further management.
*Intravenous corticosteroid therapy*
- **Corticosteroids** are typically **contraindicated** in the management of inhalation injury because they can **impair immune function** and increase the risk of infection in burn patients.
- Evidence does not support the routine use of corticosteroids to reduce inflammation in inhalation injury, and they may worsen outcomes.
Airway, Breathing, Circulation priorities US Medical PG Question 5: A 15-year-old boy is brought to the emergency department one hour after sustaining an injury during football practice. He collided head-on into another player while wearing a mouthguard and helmet. Immediately after the collision he was confused but able to use appropriate words. He opened his eyes spontaneously and followed commands. There was no loss of consciousness. He also had a headache with dizziness and nausea. He is no longer confused upon arrival. He feels well. Vital signs are within normal limits. He is fully alert and oriented. His speech is organized and he is able to perform tasks demonstrating full attention, memory, and balance. Neurological examination shows no abnormalities. There is mild tenderness to palpation over the crown of his head but no signs of skin break or fracture. Which of the following is the most appropriate next step?
- A. Discharge without activity restrictions
- B. Discharge and refrain from all physical activity for one week
- C. Observe for 6 hours in the ED and refrain from contact sports for one week (Correct Answer)
- D. Administer prophylactic levetiracetam and observe for 24 hours
- E. Administer prophylactic phenytoin and observe for 24 hours
Airway, Breathing, Circulation priorities Explanation: ***Observe for 6 hours in the ED and refrain from contact sports for one week***
- This patient experienced a brief period of **confusion, headache, dizziness**, and **nausea** immediately after a head injury, which are symptoms consistent with a **mild traumatic brain injury (mTBI)** or **concussion**.
- Although his symptoms have resolved at presentation, observation in the ED for a few hours is prudent to ensure no delayed onset of more severe symptoms, and he should **refrain from contact sports** for at least one week as part of concussion management.
*Discharge without activity restrictions*
- Discharging without activity restrictions is unsafe given the initial symptoms of **confusion** and the potential for delayed symptom presentation or complications from a concussion.
- Concussion management requires a period of **physical and cognitive rest** to allow the brain to heal and prevent **second impact syndrome**.
*Discharge and refrain from all physical activity for one week*
- While refraining from all physical activity for one week is part of concussion management, discharging immediately without any observation period after initial neurological symptoms could be risky.
- An observation period allows for monitoring of any **worsening neurological signs** or symptoms that might indicate a more serious injury.
*Administer prophylactic levetiracetam and observe for 24 hours*
- **Prophylactic anticonvulsants** like levetiracetam are typically not recommended for routine management of **mild traumatic brain injury** or concussion.
- Their use is generally reserved for patients with more severe injuries, evolving conditions, or those who have had **seizures post-trauma**.
*Administer prophylactic phenytoin and observe for 24 hours*
- Similar to levetiracetam, **phenytoin** is an anticonvulsant and its prophylactic use is not indicated for **mild head injuries** or concussions.
- Anticonvulsant prophylaxis is associated with potential side effects and is reserved for specific high-risk scenarios, such as **severe TBI** or **penetrating head trauma**.
Airway, Breathing, Circulation priorities US Medical PG Question 6: A 27-year-old soldier stationed in Libya sustains a shrapnel injury during an attack, causing a traumatic above-elbow amputation. The resulting arterial bleed is managed with a tourniquet prior to transport to the military treatment facility. On arrival, he is alert and oriented to person, place, and time. His armor and clothing are removed. His pulse is 145/min, respirations are 28/min, and blood pressure is 95/52 mm Hg. Pulmonary examination shows symmetric chest rise. The lungs are clear to auscultation. Abdominal examination shows no abnormalities. There are multiple shrapnel wounds over the upper and lower extremities. A tourniquet is in place around the right upper extremity; the right proximal forearm has been amputated. One large-bore intravenous catheter is placed in the left antecubital fossa. Despite multiple attempts, medical staff is unable to establish additional intravenous access. Which of the following is the most appropriate next step in management?
- A. Irrigate the shrapnel wounds
- B. Perform endotracheal intubation
- C. Establish intraosseous access (Correct Answer)
- D. Establish central venous access
- E. Replace the tourniquet with a pressure dressing
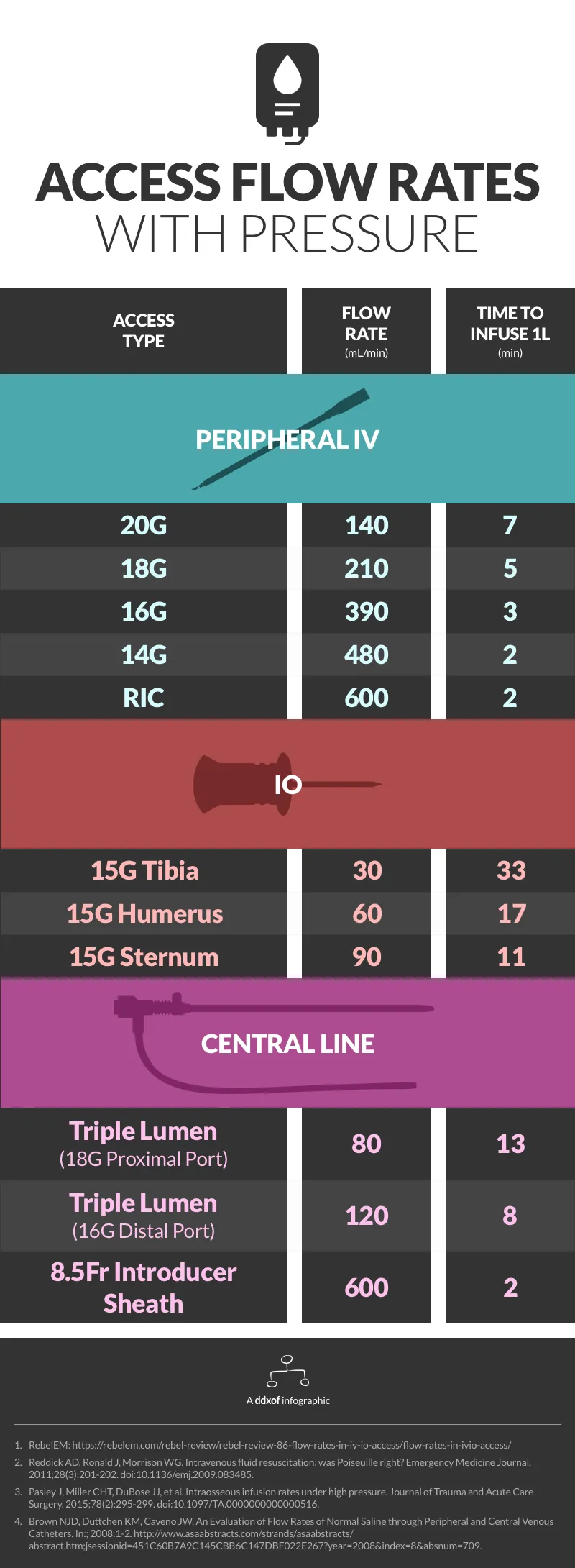
Airway, Breathing, Circulation priorities Explanation: ***Establish intraosseous access***
- The patient is in **hemorrhagic shock** (tachycardia, hypotension) and requires rapid fluid resuscitation, but peripheral intravenous access is difficult to obtain. **Intraosseous (IO) access** provides a rapid and reliable route for fluids and medications, especially in emergencies when IV access is challenging.
- IO access is a **bridge to definitive venous access** and is crucial for immediate life-saving interventions in trauma.
*Irrigate the shrapnel wounds*
- While wound irrigation is important for preventing infection, it is **not the immediate priority** when the patient is in hemorrhagic shock.
- Addressing the circulatory compromise takes precedence over local wound care.
*Perform endotracheal intubation*
- The patient is **alert and oriented** with symmetric chest rise and clear lungs, indicating he does not currently have an airway crisis requiring intubation.
- Intubation is an invasive procedure that carries risks and should only be performed when indicated for airway protection or respiratory failure.
*Establish central venous access*
- While central venous access is useful for long-term fluid management and monitoring, it is generally **more time-consuming and technically challenging** to establish than IO access, especially in an emergent, unstable patient.
- Given the urgency of rapid fluid administration, IO access is preferred as the immediate next step.
*Replace the tourniquet with a pressure dressing*
- The patient has an above-elbow amputation, suggesting significant injury, and the tourniquet is currently controlling the bleed. Removing the tourniquet prematurely without proximal surgical control can lead to **recurrent catastrophic hemorrhage**.
- A definitive surgical approach is needed to manage the amputation, not simply replacing the tourniquet with a pressure dressing, which may be insufficient to control arterial bleeding.
Airway, Breathing, Circulation priorities US Medical PG Question 7: A 17-year-old boy is brought to the emergency department by his parents 6 hours after he suddenly began to experience dyspnea and pleuritic chest pain at home. He has a remote history of asthma in childhood but has not required any treatment since the age of four. His temperature is 98.4°F (36.9°C), blood pressure is 100/76 mmHg, pulse is 125/min, respirations are 24/min. On exam, he has decreased lung sounds and hyperresonance in the left upper lung field. A chest radiograph shows a slight tracheal shift to the right. What is the best next step in management?
- A. Needle decompression
- B. CT scan for apical blebs
- C. Observe for another six hours for resolution
- D. Chest tube placement (Correct Answer)
- E. Pleurodesis
Airway, Breathing, Circulation priorities Explanation: ***Chest tube placement***
- The patient's presentation with **sudden dyspnea**, **pleuritic chest pain**, **decreased lung sounds**, **hyperresonance**, **tachycardia**, and **tracheal shift** indicates a **tension pneumothorax**, which requires immediate **chest tube insertion** for definitive management.
- While the tracheal shift might suggest tension pneumothorax, the patient's relative **hemodynamic stability** (BP 100/76, pulse 125/min) and the fact that he was stable for 6 hours implies it's a large **primary spontaneous pneumothorax** rather than an emergent tension pneumothorax. A chest tube is the appropriate next step for symptomatic patients with a large pneumothorax.
*Needle decompression*
- This procedure is reserved for true **tension pneumothorax** where there is imminent **hemodynamic compromise** (e.g., hypotension, severe tachycardia, hypoxemia) due to severe intrathoracic pressure buildup.
- The patient's blood pressure is stable, indicating that while there is a significant pneumothorax, it's not immediately life-threatening enough to warrant needle decompression before chest tube placement.
*CT scan for apical blebs*
- A **CT scan** might be useful for identifying the cause of the pneumothorax, such as **apical blebs**, but it's not an immediate management step for an acute, symptomatic pneumothorax.
- Prioritizing definitive treatment to reinflate the lung and relieve symptoms is crucial before investigating the underlying cause.
*Observe for another six hours for resolution*
- Observation is only appropriate for **small, asymptomatic pneumothoraces**.
- This patient is symptomatic with significant findings (dyspnea, chest pain, decreased lung sounds, hyperresonance, slight tracheal shift), making observation an unsafe option.
*Pleurodesis*
- **Pleurodesis** is a procedure used to prevent recurrent pneumothoraces and is typically performed after the acute event has been resolved, or for patients with **recurrent pneumothoraces**.
- It is not an acute management step for a new, symptomatic pneumothorax.
Airway, Breathing, Circulation priorities US Medical PG Question 8: A 57-year-old man was brought into the emergency department unconscious 2 days ago. His friends who were with him at that time say he collapsed on the street. Upon arrival to the ED, he had a generalized tonic seizure. At that time, he was intubated and is being treated with diazepam and phenytoin. A noncontrast head CT revealed hemorrhages within the pons and cerebellum with a mass effect and tonsillar herniation. Today, his blood pressure is 110/65 mm Hg, heart rate is 65/min, respiratory rate is 12/min (intubated, ventilator settings: tidal volume (TV) 600 ml, positive end-expiratory pressure (PEEP) 5 cm H2O, and FiO2 40%), and temperature is 37.0°C (98.6°F). On physical examination, the patient is in a comatose state. Pupils are 4 mm bilaterally and unresponsive to light. Cornea reflexes are absent. Gag reflex and cough reflex are also absent. Which of the following is the next best step in the management of this patient?
- A. Second opinion from a neurologist
- B. Withdraw ventilation support and mark time of death
- C. Electroencephalogram
- D. Repeat examination in several hours
- E. Apnea test (Correct Answer)
Airway, Breathing, Circulation priorities Explanation: ***Apnea test***
- The patient exhibits classic signs of **brain death**, including a **coma**, fixed and dilated pupils, and absent brainstem reflexes (corneal, gag, cough). The next step is to perform an apnea test to confirm the absence of spontaneous respiratory drive.
- An apnea test confirms brain death by demonstrating the **absence of respiratory effort** despite a rising pCO2, provided that spinal cord reflexes are not mistaken for respiratory efforts.
*Second opinion from a neurologist*
- While consulting a neurologist is often helpful in complex neurological cases, the current clinical picture presents such clear signs of brain death that **further confirmatory testing** for brain death (like the apnea test) is more immediately indicated before seeking additional opinions on diagnosis.
- A second opinion would typically be sought to confirm the diagnosis or guide management, but establishing brain death requires a specific protocol which is incomplete without the apnea test.
*Withdraw ventilation support and mark time of death*
- It is **premature to withdraw ventilation** before brain death is unequivocally confirmed by all necessary clinical and confirmatory tests, including the apnea test.
- Withdrawing support without full confirmation could lead to ethical and legal issues, as the patient might still have residual brainstem function, however minimal.
*Electroencephalogram*
- An **EEG** can show absent electrical activity, supporting brain death, but it is **not a mandatory part of the core brain death criteria** in many protocols, especially when clinical signs are clear and an apnea test can be performed.
- The primary diagnostic criteria for brain death usually prioritize clinical examination and the apnea test for proving irreversible cessation of all brain functions.
*Repeat examination in several hours*
- Repeating the examination in several hours is typically done if there are **confounding factors** (e.g., severe hypothermia, drug intoxication) that might mimic brain death, or if the initial assessment is incomplete.
- In this case, there are no mentioned confounding factors, and the immediate priority is to complete the brain death protocol with an apnea test, given the current clear clinical picture.
More Airway, Breathing, Circulation priorities US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.
 insertion in emergency)
insertion in emergency)