Acute vs chronic management US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Acute vs chronic management. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Acute vs chronic management US Medical PG Question 1: A 32-year-old woman comes to the office for a regular follow-up. She was diagnosed with type 2 diabetes mellitus 4 years ago. Her last blood test showed a fasting blood glucose level of 6.6 mmol/L (118.9 mg/dL) and HbA1c of 5.1%. No other significant past medical history. Current medications are metformin and a daily multivitamin. No significant family history. The physician wants to take her blood pressure measurements, but the patient states that she measures it every day in the morning and in the evening and even shows him a blood pressure diary with all the measurements being within normal limits. Which of the following statements is correct?
- A. The physician has to measure the patient’s blood pressure because it is a standard of care for any person with diabetes mellitus who presents for a check-up. (Correct Answer)
- B. Assessment of blood pressure only needs to be done at the initial visit; it is not necessary to measure blood pressure in this patient at any follow-up appointments.
- C. The physician should not measure the blood pressure in this patient and should simply make a note in a record showing the results from the patient’s diary.
- D. The physician should not measure the blood pressure in this patient because she does not have hypertension or risk factors for hypertension.
- E. The physician should not measure the blood pressure in this patient because the local standards of care in the physician's office differ from the national standards of care so measurements of this patient's blood pressure cannot be compared to diabetes care guidelines.
Acute vs chronic management Explanation: **The physician has to measure the patient’s blood pressure because it is a standard of care for any person with diabetes mellitus who presents for a check-up.**
- For individuals with **diabetes mellitus**, regular **blood pressure monitoring** by a healthcare professional is a fundamental component of their routine care, regardless of home measurements.
- This practice ensures accuracy, identifies **white coat hypertension**, and allows for early detection and management of **cardiovascular risks** inherent to diabetes.
*Assessment of blood pressure only needs to be done at the initial visit; it is not necessary to measure blood pressure in this patient at any follow-up appointments.*
- This statement is incorrect as **regular blood pressure monitoring** is essential for all follow-up visits in diabetic patients due to their elevated risk of developing **hypertension** and associated complications.
- Even if initial measurements are normal, blood pressure can change over time, necessitating continuous assessment to maintain optimal **cardiovascular health**.
*The physician should not measure the blood pressure in this patient and should simply make a note in a record showing the results from the patient’s diary.*
- Relying solely on **patient-recorded blood pressure** measurements, while valuable, does not replace the need for an **in-office measurement** by a healthcare provider.
- This is crucial for verifying the accuracy of home devices, assessing for **masked hypertension**, and ensuring compliance with **clinical guidelines**.
*The physician should not measure the blood pressure in this patient because she does not have hypertension or risk factors for hypertension.*
- This is incorrect; the patient's diagnosis of **Type 2 Diabetes Mellitus** itself is a significant **risk factor for hypertension** and cardiovascular disease.
- All individuals with diabetes require ongoing **blood pressure monitoring**, irrespective of their current blood pressure status or other obvious risk factors.
*The physician should not measure the blood pressure in this patient because the local standards of care in the physician's office differ from the national standards of care so measurements of this patient's blood pressure cannot be compared to diabetes care guidelines.*
- This statement is generally incorrect and illogical; **national guidelines** for diabetes care, including blood pressure monitoring, are established to ensure consistent and high-quality care across different settings.
- Healthcare providers are expected to adhere to these **national standards of care** or explain any deviations, making the measurement of blood pressure a critical part of a diabetic patient's visit.
Acute vs chronic management US Medical PG Question 2: A 28-year-old soldier is brought back to a military treatment facility 45 minutes after sustaining injuries in a building fire from a mortar attack. He was trapped inside the building for around 20 minutes. On arrival, he is confused and appears uncomfortable. He has a Glasgow Coma Score of 13. His pulse is 113/min, respirations are 18/min, and blood pressure is 108/70 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 96%. Examination shows multiple second-degree burns over the chest and bilateral upper extremities and third-degree burns over the face. There are black sediments seen within the nose and mouth. The lungs are clear to auscultation. Cardiac examination shows no abnormalities. The abdomen is soft and nontender. Intravenous fluid resuscitation is begun. Which of the following is the most appropriate next step in management?
- A. Insertion of nasogastric tube and enteral nutrition
- B. Intravenous antibiotic therapy
- C. Intubation and mechanical ventilation (Correct Answer)
- D. Immediate bronchoscopy
- E. Intravenous corticosteroid therapy
Acute vs chronic management Explanation: ***Intubation and mechanical ventilation***
- The patient exhibits several signs of impending **airway compromise** due to **inhalation injury**, including perioral burns, black sediments in the nose and mouth, and being trapped in a fire.
- While current oxygen saturation is 96%, **airway edema** can rapidly worsen, leading to respiratory failure. **Early intubation** is crucial to secure the airway before it becomes obstructed.
*Insertion of nasogastric tube and enteral nutrition*
- A nasogastric tube is often placed in burn patients to decompress the stomach and provide nutritional support, but it is **not the immediate priority** when there is a risk of airway obstruction.
- **Enteral nutrition** is important but should be initiated only after airway control is established and the patient is stable for feeding.
*Intravenous antibiotic therapy*
- **Prophylactic antibiotics** are generally **not recommended** in the immediate management of burn patients unless there is clear evidence of infection, which is not present here.
- Unnecessary antibiotic use can lead to **antibiotic resistance** and fungal infections.
*Immediate bronchoscopy*
- While **bronchoscopy** can confirm the extent of inhalation injury, it is not the primary immediate step. **Securing the airway** through intubation takes precedence over diagnostic procedures when airway compromise is imminent.
- Bronchoscopy can be considered *after* intubation to assess the lower airway for damage and guide further management.
*Intravenous corticosteroid therapy*
- **Corticosteroids** are typically **contraindicated** in the management of inhalation injury because they can **impair immune function** and increase the risk of infection in burn patients.
- Evidence does not support the routine use of corticosteroids to reduce inflammation in inhalation injury, and they may worsen outcomes.
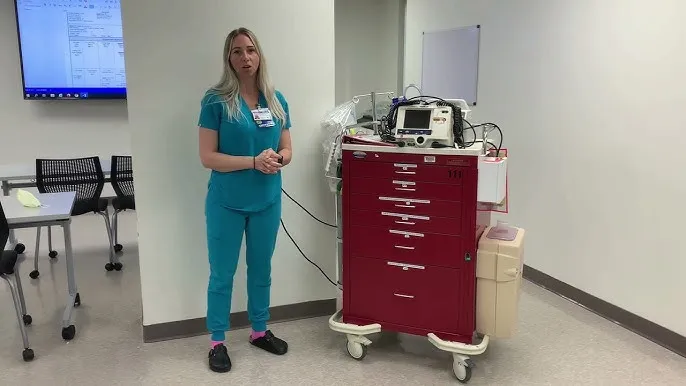
Acute vs chronic management US Medical PG Question 3: One hour after being admitted to the hospital for sharp, acute chest pain and diaphoresis, a 55-year-old woman with type 2 diabetes mellitus loses consciousness in the emergency department. There are no palpable pulses. Chest compressions are started. The patient has a history of breast cancer that was surgically treated 4 years ago. Prior to admission, the patient was on a long bus ride to visit her sister. Her medications include tamoxifen, atorvastatin, metoprolol, metformin, and insulin. Serum troponin levels are elevated. The cardiac rhythm is shown. Which of the following is the most appropriate next step in management?
- A. Defibrillation (Correct Answer)
- B. Coronary angiography
- C. Intravenous dextrose therapy
- D. Intravenous epinephrine therapy
- E. Intravenous glucagon therapy
Acute vs chronic management Explanation: ***Defibrillation***
- The ECG shows **ventricular fibrillation (VF)**, characterized by chaotic, disorganized electrical activity with no identifiable QRS complexes and no palpable pulse. VF is a **shockable rhythm**.
- According to ACLS guidelines, the immediate management for VF is **unsynchronized defibrillation** along with high-quality chest compressions.
- Defibrillation depolarizes the myocardium simultaneously, allowing the sinoatrial node to potentially resume normal electrical activity and restore organized cardiac rhythm.
- For refractory VF after initial shocks, epinephrine and antiarrhythmics (amiodarone or lidocaine) are added.
*Intravenous epinephrine therapy*
- Epinephrine is a vasopressor used in cardiac arrest to increase coronary and cerebral perfusion pressure.
- While epinephrine is given during VF arrest, it is administered **after** the initial defibrillation attempts, not as the immediate first step.
- Epinephrine is the primary drug for **non-shockable rhythms** (PEA and asystole), but defibrillation takes priority in shockable rhythms like VF.
*Intravenous glucagon therapy*
- Glucagon is used for severe **hypoglycemia** or **beta-blocker/calcium channel blocker overdose**.
- While the patient takes metoprolol (a beta-blocker), the clinical presentation with elevated troponin, chest pain, and VF rhythm clearly indicates an acute cardiac event, not beta-blocker toxicity.
- Glucagon has no role in the immediate management of cardiac arrest from VF.
*Coronary angiography*
- Coronary angiography is indicated for **post-cardiac arrest care** after return of spontaneous circulation (ROSC), especially in patients with suspected acute coronary syndrome.
- The patient has elevated troponin suggesting acute MI, making early angiography important **after** successful resuscitation.
- However, angiography cannot be performed during active cardiac arrest; immediate defibrillation and CPR are required first.
*Intravenous dextrose therapy*
- Dextrose is used to treat **hypoglycemia**.
- While the patient has diabetes and takes insulin (hypoglycemia risk), the presentation with chest pain, elevated troponin, and VF rhythm indicates acute coronary syndrome with cardiac arrest.
- Hypoglycemia does not cause VF; the rhythm is consistent with ischemic cardiac arrest requiring immediate defibrillation.
Acute vs chronic management US Medical PG Question 4: A 55-year-old man presents to his primary care physician for a wellness checkup. He states that he generally feels well and has no complaints at this time. The patient consumes alcohol frequently, eats a high sodium diet, and is sedentary. His temperature is 97.5°F (36.4°C), blood pressure is 167/108 mmHg, pulse is 90/min, respirations are 15/min, and oxygen saturation is 99% on room air. The patient is 5'10" tall and weighs 220 lbs (BMI 31.5 kg/m²). The patient's blood pressure at his last 2 appointments were 159/100 mmHg and 162/99 mmHg, respectively. His physician wants to intervene to manage his blood pressure. Which of the following is the most effective lifestyle intervention for this patient's hypertension?
- A. Exercise
- B. DASH diet (Correct Answer)
- C. Reduce alcohol consumption
- D. Sodium restriction
- E. Weight loss
Acute vs chronic management Explanation: ***DASH diet***
- The **DASH (Dietary Approaches to Stop Hypertension) diet** is a comprehensive dietary plan rich in fruits, vegetables, and low-fat dairy, and reduced in saturated and total fats. It is the most effective single lifestyle intervention for reducing **blood pressure (BP)**.
- This patient has **stage 2 hypertension** and multiple risk factors including obesity, frequent alcohol consumption, and a high-sodium diet, making a holistic dietary approach crucial for significant BP reduction.
*Exercise*
- While **regular exercise** is beneficial for overall cardiovascular health and can help manage hypertension, it is generally less effective than the DASH diet for initial, significant **blood pressure reduction** in a patient with stage 2 hypertension.
- The patient's **sedentary lifestyle** contributes to his hypertension, but exercise alone may not achieve the desired BP control as effectively as a comprehensive dietary change.
*Reduce alcohol consumption*
- **Excessive alcohol intake** is a risk factor for hypertension, and reducing consumption can lower blood pressure. However, its effect is typically less pronounced compared to the **DASH diet** in achieving major BP reductions.
- The patient's "frequent" alcohol consumption suggests this is an important area for intervention, but it's part of a broader lifestyle modification rather than the single most effective treatment.
*Sodium restriction*
- A **high sodium diet** is a significant contributor to hypertension, and **sodium restriction** is a key component of managing blood pressure. However, the DASH diet inherently incorporates sodium restriction along with other beneficial dietary changes.
- While important, focusing solely on sodium restriction often yields less comprehensive and sustained BP reduction compared to the **multi-faceted approach** of the DASH diet.
*Weight loss*
- Given the patient's **obesity (BMI 31.5 kg/m²)**, **weight loss** is a critical intervention for blood pressure control and overall health.
- However, achieving significant weight loss often requires a combination of dietary changes and increased physical activity, making the **DASH diet** a more direct and often more achievable initial step for BP reduction.
Acute vs chronic management US Medical PG Question 5: A 64-year-old woman is brought to the emergency department 1 hour after the onset of acute shortness of breath and chest pain. The chest pain is retrosternal in nature and does not radiate. She feels nauseated but has not vomited. She has type 2 diabetes mellitus, hypertension, and chronic kidney disease. Current medications include insulin, aspirin, metoprolol, and hydrochlorothiazide. She is pale and diaphoretic. Her temperature is 37°C (98°F), pulse is 136/min, and blood pressure is 80/60 mm Hg. Examination shows jugular venous distention and absence of a radial pulse during inspiration. Crackles are heard at the lung bases bilaterally. Cardiac examination shows distant heart sounds. Laboratory studies show:
Hemoglobin 8.3 g/dL
Serum
Glucose 313 mg/dL
Urea nitrogen 130 mg/dL
Creatinine 6.0 mg/dL
Which of the following is the most appropriate next step in management?
- A. Furosemide therapy
- B. Pericardiocentesis (Correct Answer)
- C. Aspirin therapy
- D. Hemodialysis
- E. Norepinephrine infusion
Acute vs chronic management Explanation: ***Pericardiocentesis***
* The patient presents with classic signs of **cardiac tamponade**, including **Beck's triad** (hypotension, jugular venous distension, distant heart sounds), **pulsus paradoxus** (absence of radial pulse during inspiration), and acute onset of shortness of breath and chest pain.
* Given her history of **chronic kidney disease** and elevated urea/creatinine levels, uremic pericarditis is a likely cause, leading to significant pericardial effusion and tamponade. **Pericardiocentesis** is the definitive treatment to relieve pressure on the heart.
*Furosemide therapy*
* While **crackles** suggest pulmonary congestion, this patient is severely hypotensive with signs of cardiogenic shock due to tamponade. Administering a diuretic like **furosemide** would further reduce preload, worsening her already compromised cardiac output and hypotension.
* The primary issue is extrinsic compression of the heart by pericardial fluid, not left ventricular failure responsive to diuresis.
*Aspirin therapy*
* The patient's chest pain and other symptoms could potentially point to an acute coronary syndrome, which would warrant **aspirin**. However, her profound hypotension and clear signs of cardiac tamponade (Beck's triad, pulsus paradoxus) make **cardiac tamponade** the more immediate and life-threatening concern.
* Addressing the tamponade takes priority as its hemodynamic compromise is more acute and direct.
*Hemodialysis*
* The patient has severe **acute-on-chronic kidney disease** and likely **uremic pericarditis**. While **hemodialysis** is indicated for uremia, it is not the immediate life-saving intervention for **cardiac tamponade**.
* **Pericardiocentesis** is required first to stabilize her hemodynamics; hemodialysis can be performed afterward to address the underlying uremia.
*Norepinephrine infusion*
* **Norepinephrine** is a powerful vasopressor that would increase systemic vascular resistance and blood pressure. While the patient is hypotensive, the underlying cause is **cardiac tamponade**, which mechanically obstructs cardiac filling and output.
* **Vasopressors** alone will not resolve the mechanical obstruction and may even increase myocardial oxygen demand without increasing cardiac output, potentially worsening the situation. The tamponade must be relieved first.
Acute vs chronic management US Medical PG Question 6: A 57-year-old woman with type 2 diabetes mellitus comes to the physician for a follow-up examination. She previously had been compliant with her diet and medication but has had a 5-kg (11-lb) weight gain since the last visit 6 months ago. She reports that she often misses doses of her metformin. Her hemoglobin A1c is 9.8%. Which of the following is the most appropriate course of action?
- A. Add glyburide to the medication regimen
- B. Stop metformin and begin an insulin regimen
- C. Schedule more frequent follow-up visits
- D. Refer the patient to an endocrinologist
- E. Refer the patient to a dietician (Correct Answer)
Acute vs chronic management Explanation: ***Refer the patient to a dietician***
- The patient has **non-compliance with both diet and medication**, along with significant weight gain (5 kg) and severely uncontrolled diabetes (HbA1c 9.8%). A dietician can provide structured education on **nutrition management**, help address barriers to lifestyle adherence, and support weight management.
- Dietician referral is a **concrete, actionable intervention** that directly addresses multiple issues: the stated diet non-compliance, weight gain, and provides diabetes self-management education that can improve overall medication adherence.
- This intervention provides **professional support** beyond what can be achieved in brief physician visits and is appropriate before escalating to more complex medication regimens.
*Schedule more frequent follow-up visits*
- While increased monitoring may seem reasonable, this is a **passive approach** that doesn't provide the patient with concrete tools or resources to address her diet non-compliance and weight gain.
- With an HbA1c of 9.8%, simply watching and waiting with more frequent visits is insufficient; **active intervention** is needed to address the underlying behavioral and lifestyle issues.
- More frequent visits alone don't provide the structured education and support this patient needs.
*Add glyburide to the medication regimen*
- Adding a **sulfonylurea** like glyburide would likely worsen the patient's weight gain, as these drugs stimulate insulin release and commonly cause weight gain of 2-3 kg.
- Before adding medications, addressing the **underlying adherence issues** with current therapy is more appropriate, as medication intensification in a non-adherent patient is unlikely to be effective.
- Glyburide also carries a higher risk of **hypoglycemia** compared to metformin.
*Stop metformin and begin an insulin regimen*
- Starting insulin without first addressing **medication adherence** and lifestyle factors is premature, especially when the patient is already struggling with a simpler oral medication regimen.
- Insulin initiation requires intensive patient education, frequent glucose monitoring, and excellent self-management skills, making it particularly challenging for a patient with documented **adherence difficulties**.
- Before escalating to insulin, interventions targeting diet, lifestyle, and adherence should be attempted.
*Refer the patient to an endocrinologist*
- Endocrinology referral is typically reserved for **complex diabetes cases** with multiple complications, failure of optimal primary care management, or need for advanced therapies.
- The primary issue here is **non-compliance with basic management**, which can and should be addressed in primary care with appropriate support services (dietician, diabetes educator).
- Referral to an endocrinologist doesn't address the fundamental adherence and lifestyle issues this patient faces.
Acute vs chronic management US Medical PG Question 7: A 72-year-old man presents to the emergency department after a fall. The patient was found lying down on the floor in his room in his retirement community. The patient has a past medical history of Alzheimer dementia and a prosthetic valve. His current medications include donepezil and warfarin. His temperature is 97.7°F (36.5°C), blood pressure is 85/50 mmHg, pulse is 160/min, respirations are 13/min, and oxygen saturation is 97% on room air. The patient is started on IV fluids and a type and screen is performed. Laboratory values are ordered as seen below.
Hemoglobin: 13 g/dL
Hematocrit: 39%
Leukocyte count: 5,500 cells/mm^3 with normal differential
Platelet count: 225,000/mm^3
INR: 2.5
AST: 10 U/L
ALT: 12 U/L
A chest radiograph and EKG are performed and are within normal limits. A full physical exam is within normal limits. The patient's vitals are repeated. His temperature is 99.5°F (37.5°C), blood pressure is 110/70 mmHg, pulse is 90/min, respirations are 10/min, and oxygen saturation is 98% on room air. Which of the following is the best next step in management?
- A. CT scan (Correct Answer)
- B. Urgent blood transfusion
- C. Fresh frozen plasma
- D. Exploratory laparoscopy
- E. Exploratory laparotomy
Acute vs chronic management Explanation: ***CT scan***
- A patient with a **prosthetic valve** on **warfarin** and a fall is at high risk for **intracranial hemorrhage**, even without focal neurological deficits.
- While initial vitals improved after IV fluids, the mechanism of injury (fall) and medication profile warrant a **CT scan** of the head to rule out serious internal injury, especially given the history of dementia which might mask symptoms.
*Urgent blood transfusion*
- The patient's **hemoglobin (13 g/dL)** and **hematocrit (39%)** are within normal limits, indicating no acute need for blood transfusion due to hemorrhage.
- Transfusions are typically reserved for patients with significant blood loss or severe symptomatic anemia.
*Fresh frozen plasma*
- The patient's **INR of 2.5** is within the therapeutic range for a patient with a prosthetic valve on warfarin.
- There is no evidence of active bleeding or supratherapeutic anticoagulation that would necessitate the administration of **fresh frozen plasma (FFP)** to reverse anticoagulation.
*Exploratory laparoscopy*
- There are no clinical signs or symptoms, such as abdominal pain, distension, or evidence of intra-abdominal bleeding (e.g., declining hemoglobin, peritoneal signs), to suggest an indication for an **exploratory laparoscopy**.
- The patient's physical exam was described as normal.
*Exploratory laparotomy*
- Similar to laparoscopy, there is no clinical evidence of acute abdominal injury or hemorrhage, which would necessitate an **exploratory laparotomy**.
- This invasive procedure is reserved for cases with strong suspicion of significant intra-abdominal pathology or trauma.
Acute vs chronic management US Medical PG Question 8: A 55-year-old man presents to the emergency department with hematemesis that started 1 hour ago but has subsided. His past medical history is significant for cirrhosis with known esophageal varices which have been previously banded. His temperature is 97.5°F (36.4°C), blood pressure is 114/64 mmHg, pulse is 130/min, respirations are 12/min, and oxygen saturation is 98% on room air. During the patient's physical exam, he begins vomiting again and his heart rate increases with a worsening blood pressure. He develops mental status changes and on exam he opens his eyes and flexes his arms only to sternal rub and is muttering incoherent words. Which of the following is the most appropriate next step in management?
- A. Transfuse blood products
- B. Intubation (Correct Answer)
- C. Emergency surgery
- D. IV fluids and fresh frozen plasma
- E. Emergency variceal banding
Acute vs chronic management Explanation: ***Intubation***
- The patient exhibits signs of **airway compromise** and hypoxemic respiratory failure due to continuous vomiting and worsening mental status, indicated by a GCS score consistent with severe neurological impairment (GCS < 8).
- **Securing the airway via intubation** is the priority to prevent aspiration and ensure adequate ventilation and oxygenation in a patient with active hematemesis and altered mental status.
*Transfuse blood products*
- While transfusion is often necessary for significant bleeding in variceal hemorrhage, the immediate priority in this deteriorating patient is **airway protection and stabilization**.
- Transfusion alone will not address the immediate risk of **aspiration** or progressive respiratory compromise.
*Emergency surgery*
- Emergency surgery (e.g., portosystemic shunt) for variceal bleeding is typically considered only after **endoscopic and pharmacological therapies have failed** to control hemorrhage.
- It is a **more invasive** and higher-risk procedure that is not the immediate first-line intervention for acute variceal bleeding.
*IV fluids and fresh frozen plasma*
- **IV fluids** are crucial for initial resuscitation in hypovolemic shock, and **fresh frozen plasma (FFP)** can help correct coagulopathy in cirrhotic patients.
- However, these interventions do not address the immediate and critical need for **airway protection** in a patient with active vomiting and declining mental status.
*Emergency variceal banding*
- **Endoscopic variceal banding** is a primary treatment for acute variceal bleeding but requires a **secured airway** and patient cooperation.
- Given the patient's deteriorating mental status and ongoing hematemesis, performing endoscopy immediately without prior intubation carries a high risk of **aspiration**.
Acute vs chronic management US Medical PG Question 9: A 52-year-old woman presents to the clinic with several days of vomiting and diarrhea. She also complains of headaches, muscle aches, and fever, but denies tenesmus, urgency, and bloody diarrhea. Past medical history is insignificant. When asked about any recent travel she says that she just came back from a cruise ship vacation. Her temperature is 37°C (98.6° F), respiratory rate is 15/min, pulse is 67/min, and blood pressure is 122/98 mm Hg. Physical examination is non-contributory. Microscopic examination of the stool is negative for ova or parasites. What is the most likely diagnosis?
- A. Traveler’s diarrhea due to ETEC
- B. Irritable bowel syndrome
- C. Norovirus infection (Correct Answer)
- D. Giardiasis
- E. C. difficile colitis
Acute vs chronic management Explanation: ***Norovirus infection***
- The combination of **vomiting** and **diarrhea** along with a history of **cruise ship travel** is highly suggestive of norovirus. Norovirus is a common cause of gastroenteritis outbreaks in crowded settings like cruise ships, schools, and nursing homes.
- While fever, headaches, and muscle aches can be present, the absence of **bloody diarrhea** and **tenesmus** points away from bacterial dysentery.
*Traveler’s diarrhea due to ETEC*
- **Enterotoxigenic *E. coli* (ETEC)** is a common cause of traveler's diarrhea, but the primary symptom is typically **watery diarrhea** often without significant vomiting.
- While travel is a risk factor, **cruise ship outbreaks** are more characteristic of norovirus due to its highly contagious nature and short incubation period.
*Irritable bowel syndrome*
- **Irritable bowel syndrome (IBS)** is a chronic functional gastrointestinal disorder characterized by recurrent abdominal pain associated with altered bowel habits.
- It does not typically present with an acute onset of **vomiting, diarrhea, fever, and muscle aches** following a specific exposure like a cruise.
*Giardiasis*
- **Giardiasis** is caused by the parasite *Giardia lamblia* and typically presents with **prolonged watery diarrhea**, abdominal cramps, bloating, and malabsorption.
- The acute, self-limiting nature and prominent **vomiting** in this case are less typical for giardiasis, and stool microscopy was negative for ova or parasites.
*C. difficile colitis*
- ***C. difficile* colitis** is primarily associated with **recent antibiotic use** and symptoms include **severe watery diarrhea**, abdominal pain, and fever.
- There is no history of antibiotic use, and the cruise travel context and prominent vomiting are not typical for *C. difficile* infection.
Acute vs chronic management US Medical PG Question 10: A 55-year-old man comes to the physician because of a 4-month history of episodic, pressure-like chest pain. The chest pain occurs when he is walking up stairs and improves with rest. He has hypertension and type 2 diabetes mellitus. His father died from a myocardial infarction at the age of 50 years. Current medications include hydrochlorothiazide and metformin. His pulse is 85/min, respirations are 12/min, and blood pressure is 140/90 mm Hg. Cardiac examination shows normal heart sounds without any murmurs, rubs, or gallops. An ECG shows high amplitude of the S wave in lead V3. An exercise stress test is performed but stopped after 4 minutes because the patient experiences chest pain. An ECG obtained during the stress test shows sinus tachycardia and ST-segment depressions in leads V1–V4. Which of the following is the most appropriate long-term pharmacotherapy to reduce the frequency of symptoms in this patient?
- A. Metoprolol (Correct Answer)
- B. Clopidogrel
- C. Aspirin
- D. Nitroglycerin
- E. Isosorbide mononitrate
Acute vs chronic management Explanation: ***Metoprolol***
- **Beta-blockers** like metoprolol are first-line agents for **symptom relief** in stable angina by reducing myocardial oxygen demand.
- They decrease **heart rate**, **blood pressure**, and **myocardial contractility**, thereby reducing the frequency and severity of anginal episodes.
*Clopidogrel*
- **Clopidogrel** is an antiplatelet agent used primarily to prevent **thrombotic events** in patients with established cardiovascular disease or acute coronary syndromes.
- It does not directly reduce the frequency of anginal symptoms, but rather prevents progression to **myocardial infarction** or **stroke**.
*Aspirin*
- **Aspirin** is an antiplatelet medication used for **secondary prevention** of cardiovascular events by inhibiting platelet aggregation.
- While crucial for reducing cardiovascular risk, it does not directly alleviate the **frequency of anginal symptoms** themselves.
*Nitroglycerin*
- **Nitroglycerin** is a short-acting nitrate used to provide **immediate relief** of anginal pain during an acute episode.
- It is not a long-term pharmacotherapy for reducing the *frequency* of symptoms.
*Isosorbide mononitrate*
- **Isosorbide mononitrate** is a long-acting nitrate used to *prevent* angina, but it is typically a **second-line agent** after beta-blockers due to potential for **tolerance** and side effects.
- While it can reduce symptom frequency, beta-blockers are generally preferred as initial long-term therapy for symptom control.
More Acute vs chronic management US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.