Prioritizing interventions

On this page
🎯 The Clinical Decision Matrix: Mastering Intervention Hierarchy
Every clinical encounter demands you answer a deceptively simple question: what do I do first? You'll master the frameworks that transform overwhelming patient complexity into clear action hierarchies, learning how to weigh urgency against impact, allocate scarce resources ethically, and navigate competing priorities when multiple systems fail simultaneously. Through decision matrices, pattern recognition algorithms, and evidence-based pathways, you'll build the systematic thinking that separates reactive care from strategic intervention-ensuring your choices maximize both survival and quality of life when every second counts.
📌 Remember: ABCDE-FIRST - Airway, Breathing, Circulation, Disability, Exposure - First Identify Reversible Severe Threats
The systematic approach to intervention prioritization follows established medical principles that have evolved through decades of emergency medicine research. Primary survey protocols identify immediate threats within 60 seconds, while secondary assessment addresses non-life-threatening conditions over 15-30 minutes. This temporal framework ensures critical interventions receive priority while maintaining comprehensive patient care.
-
Immediate Priority (Red Zone)
- Airway obstruction requiring intervention within 4 minutes
- Respiratory failure with SpO2 <90% despite supplemental oxygen
- Circulatory shock with systolic BP <90 mmHg
- Hemorrhagic shock: blood loss >20% of circulating volume
- Cardiogenic shock: cardiac output <4 L/min
- Septic shock: lactate >4 mmol/L with hypotension
-
Urgent Priority (Yellow Zone)
- Chest pain with TIMI score ≥3 suggesting acute coronary syndrome
- Neurological deficits with NIHSS >4 within 4.5-hour window
- Severe pain scores ≥8/10 requiring immediate analgesia
- Renal colic with eGFR decline >25%
- Acute abdomen with peritoneal signs
| Priority Level | Time Frame | Intervention Examples | Mortality Risk | Resource Allocation |
|---|---|---|---|---|
| Immediate (P1) | 0-15 minutes | Intubation, chest tube, blood transfusion | >50% if delayed | Unlimited resources |
| Urgent (P2) | 15-60 minutes | IV antibiotics, pain control, imaging | 10-25% if delayed | High resource priority |
| Less Urgent (P3) | 1-4 hours | Wound care, medication adjustment | <5% if delayed | Standard resources |
| Non-urgent (P4) | 4-24 hours | Routine labs, discharge planning | <1% if delayed | Minimal resources |
| Expectant (P5) | Comfort only | Palliative care, family support | >95% mortality | Comfort resources |
💡 Master This: Every intervention decision requires simultaneous assessment of urgency (time-sensitive), severity (life-threatening potential), and treatability (reversibility with available resources).
Understanding intervention prioritization unlocks the systematic approach to resource allocation frameworks that guide complex multi-patient scenarios.
🎯 The Clinical Decision Matrix: Mastering Intervention Hierarchy
⚖️ Resource Allocation Architecture: The Scarcity Navigation System
📌 Remember: SMART-CARE - Severity assessment, Mortality prediction, Available resources, Reversibility potential, Time sensitivity - Cost effectiveness, Alternative options, Recovery likelihood, Ethical considerations
-
High-Priority Resource Allocation
- ICU beds: Patients with >80% survival probability and <7 days expected length of stay
- Ventilators: SOFA score <11 with reversible respiratory failure
- Blood products: Hemoglobin <7 g/dL in stable patients, <10 g/dL in cardiac patients
- Type O negative: Reserved for unknown blood type emergencies
- Platelets: <10,000/μL with bleeding or <50,000/μL pre-procedure
-
Moderate-Priority Allocation
- Specialty consultations: 48-72 hour response time for non-urgent conditions
- Advanced imaging: CT/MRI within 24 hours for diagnostic uncertainty
- Surgical scheduling: Elective procedures within 30 days of indication
- Cancer surgery: <6 weeks from diagnosis to treatment
- Cardiac procedures: <2 weeks for stable angina
| Resource Type | Allocation Criteria | Priority Score | Expected Outcome | Alternative Options |
|---|---|---|---|---|
| ICU Bed | APACHE II <25, reversible condition | 8-10 points | >70% survival | Step-down unit |
| Ventilator | P/F ratio <200, SOFA <15 | 7-9 points | >60% weaning | Non-invasive ventilation |
| OR Time | Emergency surgery, <6 hour delay | 9-10 points | >80% success | Bedside procedure |
| Blood Products | Active bleeding, Hgb <7 g/dL | 8-10 points | >90% hemostasis | Iron therapy |
| Specialist | Organ failure, <24 hour need | 6-8 points | >50% improvement | Telemedicine |
💡 Master This: Effective resource allocation requires continuous reassessment every 12-24 hours, as patient conditions and resource availability change dynamically throughout hospitalization.
Resource allocation frameworks provide the foundation for understanding quality-of-life assessment tools that guide intervention selection in complex clinical scenarios.
⚖️ Resource Allocation Architecture: The Scarcity Navigation System
🎭 Quality-of-Life Assessment Matrix: Beyond Survival Metrics

Quality-of-life (QoL) assessment represents a multidimensional evaluation encompassing physical function, emotional well-being, social relationships, and symptom burden. Modern healthcare prioritizes patient-reported outcomes alongside traditional biomarkers, recognizing that survival duration without functional capacity may not align with patient values and preferences.
-
Physical Function Assessment
- Activities of Daily Living (ADL): Barthel Index score >60 indicates functional independence
- Instrumental ADL: Lawton Scale >14 suggests community living capability
- Mobility measures: 6-minute walk test >300 meters predicts cardiovascular fitness
- Gait speed >0.8 m/s: Associated with reduced mortality risk
- Grip strength >16 kg (women), >27 kg (men): Functional muscle mass indicator
-
Symptom Burden Evaluation
- Pain assessment: Numeric Rating Scale >7/10 requires immediate intervention
- Fatigue scales: FACIT-Fatigue <30 indicates severe functional impairment
- Dyspnea measurement: Modified Medical Research Council >3 suggests severe limitation
- Nausea/vomiting: >3 episodes/day significantly impacts nutrition
- Sleep disturbance: <4 hours continuous sleep affects cognitive function
📌 Remember: HOPE-SCALE - Health perception, Optimism level, Pain control, Energy level - Social support, Cognitive function, Activity tolerance, Life satisfaction, Emotional stability
| QoL Domain | Assessment Tool | Normal Range | Intervention Threshold | Clinical Significance |
|---|---|---|---|---|
| Physical Function | SF-36 Physical | >80 points | <50 points | Predicts hospitalization risk |
| Mental Health | PHQ-9 Depression | <5 points | >10 points | Affects treatment compliance |
| Social Function | Social Support Scale | >70 points | <40 points | Impacts recovery outcomes |
| Symptom Burden | ESAS Total Score | <30 points | >50 points | Reduces treatment tolerance |
| Global QoL | EORTC QLQ-C30 | >70 points | <50 points | Predicts survival outcomes |
💡 Master This: Baseline QoL assessment should occur within 48 hours of admission, with weekly reassessment during active treatment to guide intervention modifications and goals-of-care discussions.
Quality-of-life frameworks establish the foundation for pattern recognition systems that identify intervention priorities across diverse clinical presentations.
🎭 Quality-of-Life Assessment Matrix: Beyond Survival Metrics
🔍 Pattern Recognition Command Center: Clinical Decision Algorithms
-
Cardiovascular Pattern Recognition
- Chest pain + ST elevation: Primary PCI within 90 minutes (door-to-balloon)
- Hypotension + JVD + muffled heart sounds: Pericardial tamponade requiring immediate pericardiocentesis
- Tearing chest pain + pulse differential: Aortic dissection needing blood pressure control <140 mmHg
- Type A dissection: Emergency surgery within 6 hours
- Type B dissection: Medical management unless complications develop
-
Neurological Pattern Recognition
- Sudden onset weakness + speech difficulty: Stroke protocol within 4.5-hour window
- Headache + neck stiffness + photophobia: Meningitis workup with antibiotics <1 hour
- Altered mental status + focal signs: Mass effect requiring neurosurgical evaluation
- Pupil asymmetry >2mm: Herniation risk needing osmotic therapy
- GCS decline >2 points: ICP monitoring consideration
📌 Remember: RAPID-SCAN - Respiratory distress, Altered consciousness, Pain severe, Infection signs, Deformity visible - Shock signs, Cardiac symptoms, Acute abdomen, Neurological deficits
| Clinical Pattern | Recognition Triggers | Time Window | First Intervention | Success Rate |
|---|---|---|---|---|
| STEMI | ST elevation >1mm, chest pain >20 min | <90 minutes | Primary PCI | >95% vessel opening |
| Sepsis | qSOFA ≥2, lactate >2 mmol/L | <1 hour | Antibiotics + fluids | >80% survival |
| Stroke | FAST positive, <4.5 hours | <60 minutes | tPA administration | >70% improvement |
| Trauma | Mechanism + vitals, <1 hour | <10 minutes | Primary survey | >90% stabilization |
| Anaphylaxis | Urticaria + hypotension, <30 min | <5 minutes | Epinephrine IM | >95% response |
💡 Master This: High-frequency patterns (chest pain, dyspnea, altered mental status) account for 60% of emergency presentations, making pattern mastery essential for efficient triage and resource utilization.
Pattern recognition systems provide the framework for systematic comparison tools that differentiate between similar clinical presentations requiring different intervention priorities.
🔍 Pattern Recognition Command Center: Clinical Decision Algorithms
⚖️ Differential Priority Matrix: Systematic Clinical Discrimination
Systematic clinical discrimination requires evidence-based frameworks that differentiate between similar presentations with vastly different intervention priorities. Expert clinicians utilize discriminating features with known sensitivity and specificity values to rapidly distinguish life-threatening conditions from benign mimics, ensuring appropriate resource allocation and timely intervention.
-
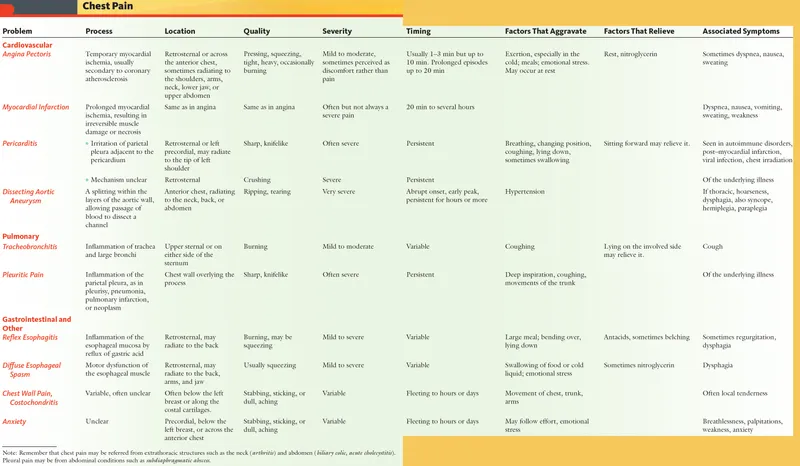
Chest Pain Discrimination Framework
- Cardiac vs. Non-cardiac: HEART score >3 indicates cardiac evaluation priority
- STEMI vs. NSTEMI: ST elevation >1mm in ≥2 contiguous leads requires immediate catheterization
- Aortic dissection vs. MI: Pulse differential >20 mmHg suggests dissection priority
- D-dimer >500 ng/mL: 90% sensitivity for aortic dissection
- Troponin elevation: 95% sensitivity for myocardial injury within 6 hours
-
Dyspnea Discrimination Framework
- Heart failure vs. COPD: BNP >400 pg/mL indicates cardiac etiology
- Pulmonary embolism vs. pneumonia: Wells score >4 prioritizes PE workup
- Pneumothorax vs. asthma: Unilateral breath sounds require immediate chest imaging
- Peak flow <50% predicted: Severe asthma exacerbation
- Oxygen saturation <90%: Respiratory failure regardless of etiology
📌 Remember: RISK-SORT - Red flags present, Immediate threats, Severity markers, Key discriminators - Sensitivity values, Outcome predictors, Resource needs, Time sensitivity
| Presentation | High-Risk Discriminators | Moderate-Risk Features | Low-Risk Indicators | Intervention Priority |
|---|---|---|---|---|
| Chest Pain | ST elevation, hypotension | Troponin positive, age >65 | Reproducible, normal ECG | Immediate vs. Urgent vs. Standard |
| Dyspnea | Hypoxemia, altered mental status | Elevated BNP, fever | Exertional only, normal vitals | Immediate vs. Urgent vs. Standard |
| Headache | Neck stiffness, focal deficits | Sudden onset, age >50 | Gradual onset, typical pattern | Immediate vs. Urgent vs. Standard |
| Abdominal Pain | Peritoneal signs, hypotension | Elevated WBC, fever | Cramping, normal exam | Immediate vs. Urgent vs. Standard |
| Altered Mental Status | Focal signs, hypoglycemia | Fever, medication changes | Chronic baseline, stable vitals | Immediate vs. Urgent vs. Standard |
💡 Master This: High-risk discriminators have >90% sensitivity for life-threatening conditions, while low-risk indicators have >95% negative predictive value for serious pathology.
Differential priority matrices establish the foundation for evidence-based treatment algorithms that guide intervention selection and resource allocation.
⚖️ Differential Priority Matrix: Systematic Clinical Discrimination
🎯 Treatment Algorithm Architecture: Evidence-Based Intervention Pathways
-
Sepsis Treatment Algorithm
- Hour 1: Blood cultures + broad-spectrum antibiotics + 30 mL/kg crystalloid
- Hour 3: Lactate reassessment + vasopressors if MAP <65 mmHg
- Hour 6: Source control evaluation + antibiotic de-escalation consideration
- Norepinephrine: First-line vasopressor starting 0.1 mcg/kg/min
- Procalcitonin <0.25: 85% negative predictive value for bacterial infection
-
Acute Coronary Syndrome Algorithm
- STEMI: Primary PCI within 90 minutes or fibrinolysis within 30 minutes
- NSTEMI: Risk stratification with TIMI score + troponin trending
- Unstable angina: Antiplatelet therapy + anticoagulation + ischemia evaluation
- Dual antiplatelet therapy: Aspirin 325 mg + clopidogrel 600 mg loading
- Heparin dosing: 60 units/kg bolus + 12 units/kg/hour infusion
📌 Remember: TREAT-FAST - Time-sensitive protocols, Response monitoring, Escalation criteria, Alternative pathways, Target endpoints - Failure recognition, Adjustment triggers, Safety parameters, Termination criteria
| Condition | First-Line Treatment | Response Timeline | Escalation Criteria | Success Rate |
|---|---|---|---|---|
| Septic Shock | Antibiotics + fluids + vasopressors | 1-6 hours | Lactate >4 mmol/L | >70% survival |
| STEMI | Primary PCI | 90 minutes | Failed reperfusion | >95% vessel opening |
| Status Epilepticus | Lorazepam 4 mg IV | 5-10 minutes | Continued seizures | >80% termination |
| Anaphylaxis | Epinephrine 0.3 mg IM | 5-15 minutes | Persistent hypotension | >95% response |
| Acute Asthma | Albuterol + corticosteroids | 1-4 hours | Peak flow <50% | >85% improvement |
💡 Master This: Treatment algorithms require continuous updating based on emerging evidence, with major revisions occurring every 3-5 years as new randomized controlled trials modify standard-of-care recommendations.
Treatment algorithms provide the systematic foundation for multi-system integration approaches that address complex patients with multiple competing priorities.
🎯 Treatment Algorithm Architecture: Evidence-Based Intervention Pathways
🔗 Multi-System Integration Hub: Complex Patient Navigation
-
Cardiovascular-Renal Integration
- Heart failure + CKD: ACE inhibitor titration balancing cardiac benefit vs. renal function
- Target eGFR decline: <30% from baseline acceptable for cardiac protection
- Diuretic management: Loop diuretics with potassium monitoring every 48-72 hours
- Furosemide dosing: 40-80 mg daily with creatinine monitoring
- Spironolactone: 25 mg daily if potassium <5.0 mEq/L
-
Diabetes-Cardiovascular Integration
- Glycemic targets: HbA1c <7% in stable patients, <8% in complex comorbidities
- SGLT2 inhibitors: Cardiovascular benefit independent of glucose lowering
- Metformin continuation: Safe until eGFR <30 mL/min/1.73m²
- Insulin adjustment: 20% reduction during acute illness
- Hypoglycemia risk: Increased 3-fold with multiple comorbidities
📌 Remember: SYSTEM-SYNC - Severity ranking, Yield optimization, Specialist coordination, Timing priorities, Evidence integration, Monitoring protocols - Safety parameters, Yield assessment, Need reassessment, Care coordination
| System Combination | Primary Priority | Secondary Considerations | Monitoring Parameters | Integration Challenges |
|---|---|---|---|---|
| Cardiac-Renal | Hemodynamic stability | Fluid balance, electrolytes | Daily weights, BUN/Cr | Medication dosing |
| Diabetes-Cardiac | Glycemic control | Cardiovascular protection | HbA1c, lipids | Hypoglycemia risk |
| Pulmonary-Cardiac | Oxygenation | Right heart function | ABG, echo | Fluid management |
| Neuro-Cardiac | Cerebral perfusion | Blood pressure control | Neuro checks, BP | Medication interactions |
| GI-Hepatic | Nutritional status | Liver function | Albumin, LFTs | Drug metabolism |
💡 Master This: System prioritization changes dynamically during hospitalization, requiring daily reassessment of competing priorities and adjustment of intervention hierarchies based on clinical response and emerging complications.
Multi-system integration frameworks establish the foundation for rapid mastery tools that enable efficient clinical decision-making in complex scenarios.
🔗 Multi-System Integration Hub: Complex Patient Navigation
🎯 Clinical Mastery Arsenal: Rapid Decision Tools
-
Rapid Assessment Arsenal
- ABCDE Primary Survey: 60-second systematic evaluation for life threats
- SBAR Communication: Situation-Background-Assessment-Recommendation for handoffs
- ISBAR Protocol: Identity added for patient safety during transitions
- Situation: Chief complaint + current status in <30 seconds
- Background: Relevant history + medications in <60 seconds
- Assessment: Clinical findings + vital signs in <30 seconds
- Recommendation: Specific requests + timeline in <30 seconds
-
Priority Scoring Systems
- qSOFA Score: ≥2 points indicates sepsis risk requiring immediate evaluation
- HEART Score: >3 points suggests cardiac evaluation within 6 hours
- NIHSS Score: >4 points indicates stroke severity requiring specialist consultation
- Glasgow Coma Scale: <13 requires neurological monitoring
- APACHE II Score: >25 predicts >50% mortality in ICU patients
| Decision Tool | Time to Complete | Clinical Application | Sensitivity | Specificity |
|---|---|---|---|---|
| qSOFA | <2 minutes | Sepsis screening | >85% | >70% |
| HEART Score | <3 minutes | Chest pain risk | >90% | >75% |
| NIHSS | <5 minutes | Stroke severity | >95% | >80% |
| Wells Score | <3 minutes | PE probability | >80% | >85% |
| CURB-65 | <2 minutes | Pneumonia severity | >75% | >90% |
⭐ Clinical Pearl: Standardized decision tools reduce diagnostic errors by 35% and improve consistency across different providers by 50%, particularly during high-stress situations.
💡 Master This: Tool selection depends on clinical context - screening tools for broad populations, diagnostic tools for specific conditions, and prognostic tools for outcome prediction and resource allocation.
🎯 Clinical Mastery Arsenal: Rapid Decision Tools
Practice Questions: Prioritizing interventions
Test your understanding with these related questions
A research team develops a new monoclonal antibody checkpoint inhibitor for advanced melanoma that has shown promise in animal studies as well as high efficacy and low toxicity in early phase human clinical trials. The research team would now like to compare this drug to existing standard of care immunotherapy for advanced melanoma. The research team decides to conduct a non-randomized study where the novel drug will be offered to patients who are deemed to be at risk for toxicity with the current standard of care immunotherapy, while patients without such risk factors will receive the standard treatment. Which of the following best describes the level of evidence that this study can offer?













