Pre-test probability assessment US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Pre-test probability assessment. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Pre-test probability assessment US Medical PG Question 1: A scientist is studying the characteristics of a newly discovered infectious disease in order to determine its features. He calculates the number of patients that develop the disease over several months and finds that on average 75 new patients become infected per month. Furthermore, he knows that the disease lasts on average 2 years before patients are either cured or die from the disease. If the population being studied consists of 7500 individuals, which of the following is the prevalence of the disease?
- A. 0.24 (Correct Answer)
- B. 0.02
- C. 0.12
- D. 0.005
- E. 0.01
Pre-test probability assessment Explanation: ***0.24***
- Prevalence is calculated as the **number of existing cases** divided by the **total population**. The number of existing cases is estimated by multiplying the **incidence rate** (75 new cases/month) by the **duration of the disease** (2 years or 24 months): 75 cases/month * 24 months = 1800 cases.
- The prevalence is then 1800 cases / 7500 individuals = **0.24**.
*0.02*
- This value might be obtained by incorrectly using only the monthly incidence or by performing **incorrect calculations** involving the duration and total population.
- It does not account for the **cumulative effect** of new cases over the entire disease duration.
*0.12*
- This answer might result from miscalculating the **duration of the disease** (e.g., using 1 year instead of 2 years), leading to an underestimation of the total existing cases.
- It suggests an error in converting the **duration from years to months** when multiplying by the monthly incidence.
*0.005*
- This value is significantly lower than the correct prevalence, suggesting a major error in calculating the total number of cases or incorrectly dividing the total cases by the entire population.
- It does not properly reflect the contribution of new cases over the **duration of the disease**.
*0.01*
- This result is likely derived from an incorrect application of the incidence rate or a misunderstanding of how the duration of the disease impacts the **total number of prevalent cases**.
- It's a calculation error that significantly underestimates the **true disease burden**.
Pre-test probability assessment US Medical PG Question 2: A researcher is trying to determine whether a newly discovered substance X can be useful in promoting wound healing after surgery. She conducts this study by enrolling the next 100 patients that will be undergoing this surgery and separating them into 2 groups. She decides which patient will be in which group by using a random number generator. Subsequently, she prepares 1 set of syringes with the novel substance X and 1 set of syringes with a saline control. Both of these sets of syringes are unlabeled and the substances inside cannot be distinguished. She gives the surgeon performing the surgery 1 of the syringes and does not inform him nor the patient which syringe was used. After the study is complete, she analyzes all the data that was collected and performs statistical analysis. This study most likely provides which level of evidence for use of substance X?
- A. Level 3
- B. Level 1 (Correct Answer)
- C. Level 4
- D. Level 5
- E. Level 2
Pre-test probability assessment Explanation: ***Level 1***
- The study design described is a **randomized controlled trial (RCT)**, which is considered the **highest level of evidence (Level 1)** in the hierarchy of medical evidence.
- Key features like **randomization**, **control group**, and **blinding (double-blind)** help minimize bias and strengthen the validity of the findings.
*Level 2*
- Level 2 evidence typically comprises **well-designed controlled trials without randomization** (non-randomized controlled trials) or **high-quality cohort studies**.
- While strong, they do not possess the same level of internal validity as randomized controlled trials.
*Level 3*
- Level 3 evidence typically includes **case-control studies** or **cohort studies**, which are observational designs and carry a higher risk of bias compared to RCTs.
- These studies generally do not involve randomization or intervention assignment by the researchers.
*Level 4*
- Level 4 evidence is usually derived from **case series** or **poor quality cohort and case-control studies**.
- These studies provide descriptive information or investigate associations without strong control for confounding factors.
*Level 5*
- Level 5 evidence is the **lowest level of evidence**, consisting of **expert opinion** or **animal research/bench research**.
- This level lacks human clinical data or systematic investigative rigor needed for higher evidence levels.
Pre-test probability assessment US Medical PG Question 3: A 67-year-old woman presents with right leg pain and swelling of 5 days’ duration. She has a history of hypertension for 15 years and had a recent hospitalization for pneumonia. She had been recuperating at home but on beginning to mobilize and walk, the right leg became painful and swollen. Her temperature is 37.1°C (98.7°F), the blood pressure is 130/80 mm Hg, and the pulse is 75/min. On physical examination, the right calf is 4 cm greater in circumference than the left when measured 10 cm below the tibial tuberosity. Dilated superficial veins are present on the right foot and the right leg is slightly redder than the left. There is some tenderness on palpation in the popliteal fossa behind the knee. Which of the following is the best initial step in the management of this patient’s condition?
- A. International normalized ratio (INR)
- B. Thrombophilia screen
- C. Wells’ clinical probability tool (Correct Answer)
- D. Computerized tomography (CT) with contrast
- E. Activated partial thromboplastin time (aPTT)
Pre-test probability assessment Explanation: ***Wells' clinical probability tool***
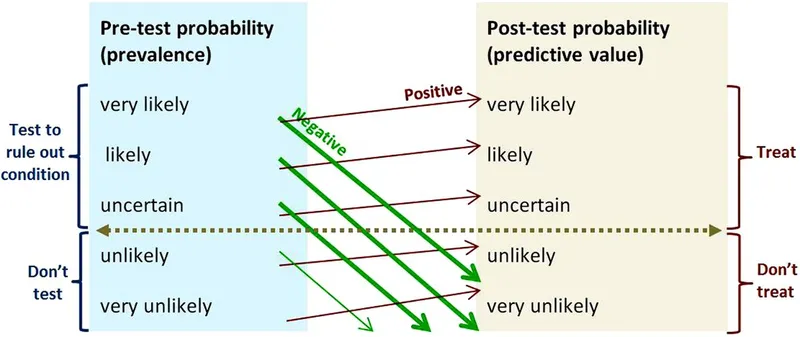
- The patient presents with classic signs and symptoms of **deep vein thrombosis (DVT)**, including unilateral leg pain and swelling, dilated superficial veins, and tenderness. The Wells' clinical probability tool helps stratify the risk of DVT, guiding further diagnostic testing.
- Using this validated clinical decision rule for risk assessment is the **best initial step** to determine the likelihood of DVT before proceeding with imaging studies (compression ultrasound) or D-dimer testing.
- Based on the Wells' score, patients are categorized as low, moderate, or high probability, which then directs appropriate diagnostic testing and potential empiric anticoagulation.
*International normalized ratio (INR)*
- **INR** is used to monitor the effectiveness of **warfarin** therapy, an anticoagulant, and to assess liver function.
- It is not an initial diagnostic tool for DVT; rather, it is used **after a DVT diagnosis** has been made and anticoagulation with warfarin has been initiated.
*Thrombophilia screen*
- A **thrombophilia screen** investigates underlying genetic or acquired clotting disorders.
- This is typically performed **after a DVT diagnosis** in younger patients, those with recurrent DVT, or those with a family history of thrombosis, not as an initial diagnostic step unless there is strong suspicion for an underlying clotting disorder.
*Computerized tomography (CT) with contrast*
- A **CT with contrast** (specifically **CT venography**) can diagnose DVT, but it is not the **first-line imaging modality** for suspected DVT because of radiation exposure and contrast risks.
- **Compression ultrasonography** is generally the preferred initial imaging study for DVT, especially after a risk assessment using the Wells' score.
*Activated partial thromboplastin time (aPTT)*
- The **aPTT** is a measure of the intrinsic and common pathways of coagulation and is used to monitor **unfractionated heparin** therapy.
- It is not an initial diagnostic test for DVT; like INR, it is used **after diagnosis** for monitoring anticoagulant treatment.
Pre-test probability assessment US Medical PG Question 4: A 43-year-old woman presents to her primary care physician with complaints of mild shortness of breath and right-sided chest pain for three days. She reports that lately she has had a nagging nonproductive cough and low-grade fevers. On examination, her vital signs are: temperature 99.1 deg F (37.3 deg C), blood pressure is 115/70 mmHg, pulse is 91/min, respirations are 17/min, and oxygen saturation 97% on room air. She is well-appearing, with normal work of breathing, and no leg swelling. She is otherwise healthy, with no prior medical or surgical history, currently taking no medications. The attending has a low suspicion for the most concerning diagnosis and would like to exclude it with a very sensitive though non-specific test. Which of the following should this physician order?
- A. Obtain chest radiograph
- B. Obtain spiral CT chest with IV contrast
- C. Order a lower extremity ultrasound
- D. Order a D-dimer (Correct Answer)
- E. Obtain ventilation-perfusion scan
Pre-test probability assessment Explanation: ***Order a D-dimer***
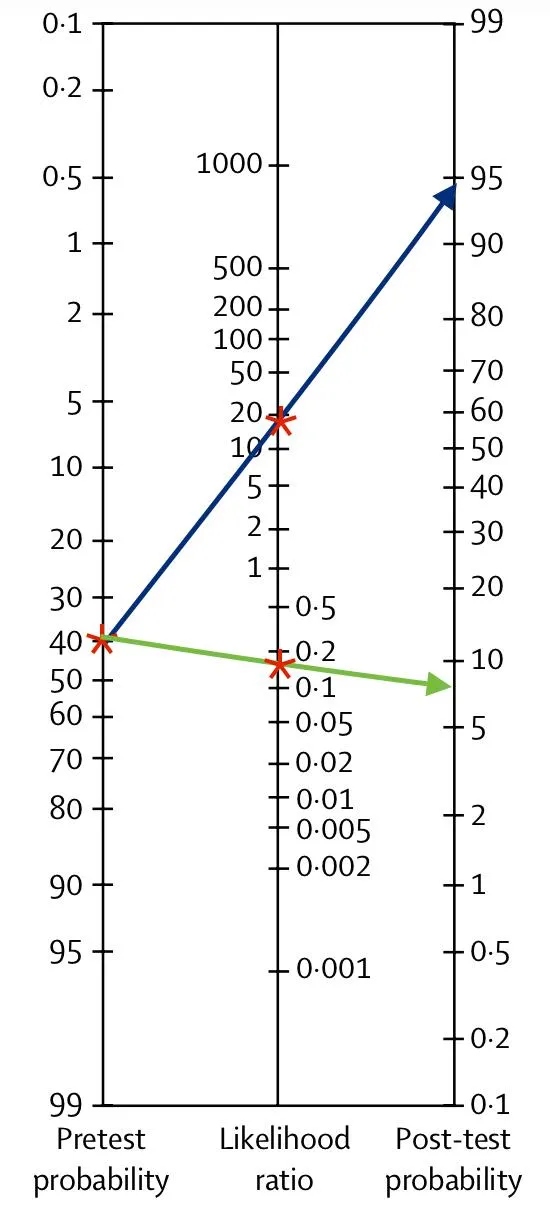
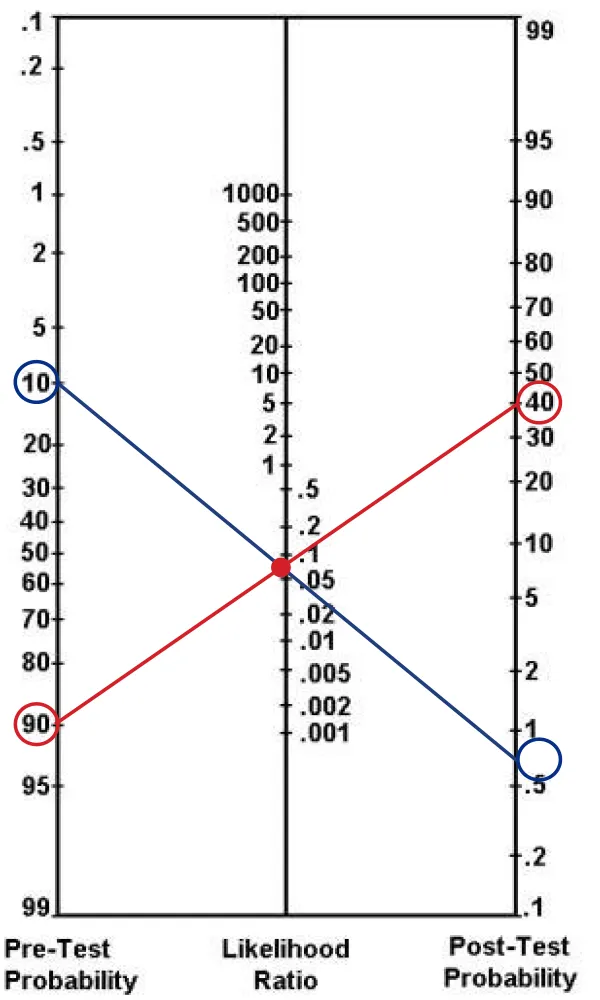
- The physician has a **low suspicion based on clinical assessment** and wants to **exclude** a concerning diagnosis (likely **pulmonary embolism** or PE) using a **sensitive test**. A negative D-dimer test can effectively rule out PE in patients with a low pre-test probability.
- The D-dimer is a product of **fibrin degradation** and its elevation indicates recent or ongoing **thrombus formation** and lysis. It is highly sensitive for PE but has low specificity.
*Obtain chest radiograph*
- A chest radiograph is often **normal in pulmonary embolism** or may show non-specific findings, making it unsuitable for ruling out PE.
- While useful for diagnosing other conditions like pneumonia or pleural effusions, it is **not sensitive enough to exclude PE**.
*Obtain spiral CT chest with IV contrast*
- A **spiral CT chest with IV contrast (CT pulmonary angiography)** is the gold standard for diagnosing PE, but it is **not a sensitive rule-out test** for low-probability cases.
- It involves **radiation exposure** and **contrast administration**, which are generally avoided if a less invasive, equally effective rule-out test is available for low-risk patients.
*Order a lower extremity ultrasound*
- Lower extremity ultrasound is used to diagnose **deep vein thrombosis (DVT)**, which is a common source of PE.
- While DVT can lead to PE, a negative lower extremity ultrasound **does not rule out PE** itself, as the clot may have already embolized or originated from elsewhere.
*Obtain ventilation-perfusion scan*
- A **ventilation-perfusion (V/Q) scan** is an alternative to CT angiography for diagnosing PE, particularly in patients with contraindications to contrast.
- However, it is **less definitive than CTPA** and is typically used when suspicion for PE is moderate or higher, rather than as a primary rule-out test for low-probability patients.
Pre-test probability assessment US Medical PG Question 5: A pharmaceutical corporation is developing a research study to evaluate a novel blood test to screen for breast cancer. They enrolled 800 patients in the study, half of which have breast cancer. The remaining enrolled patients are age-matched controls who do not have the disease. Of those in the diseased arm, 330 are found positive for the test. Of the patients in the control arm, only 30 are found positive. What is this test’s sensitivity?
- A. 330 / (330 + 30)
- B. 330 / (330 + 70) (Correct Answer)
- C. 370 / (30 + 370)
- D. 370 / (70 + 370)
- E. 330 / (400 + 400)
Pre-test probability assessment Explanation: ***330 / (330 + 70)***
- **Sensitivity** measures the proportion of actual **positives** that are correctly identified as such.
- In this study, there are **400 diseased patients** (half of 800). Of these, 330 tested positive (true positives), meaning 70 tested negative (false negatives). So sensitivity is **330 / (330 + 70)**.
*330 / (330 + 30)*
- This calculation represents the **positive predictive value**, which is the probability that subjects with a positive screening test truly have the disease. It uses **true positives / (true positives + false positives)**.
- It does not correctly calculate **sensitivity**, which requires knowing the total number of diseased individuals.
*370 / (30 + 370)*
- This expression is attempting to calculate **specificity**, which is the proportion of actual negatives that are correctly identified. It would be **true negatives / (true negatives + false positives)**.
- However, the numbers used are incorrect for specificity in this context given the data provided.
*370 / (70 + 370)*
- This formula is an incorrect combination of values and does not represent any standard epidemiological measure like **sensitivity** or **specificity**.
- It is attempting to combine false negatives (70) and true negatives (370 from control arm) in a non-standard way.
*330 / (400 + 400)*
- This calculation attempts to divide true positives by the total study population (800 patients).
- This metric represents the **prevalence of true positives within the entire study cohort**, not the test's **sensitivity**.
Pre-test probability assessment US Medical PG Question 6: A 65-year-old non-smoking woman with no symptoms comes to your clinic to establish care with a primary care provider. She hasn’t seen a doctor in 12 years and states that she feels very healthy. You realize that guidelines by the national cancer organization suggest that she is due for some cancer screening tests, including a mammogram for breast cancer, a colonoscopy for colon cancer, and a pap smear for cervical cancer. These three screening tests are most likely to be considered which of the following?
- A. Tertiary prevention
- B. Primary prevention
- C. Secondary prevention (Correct Answer)
- D. Cancer screening does not fit into these categories
- E. Quaternary prevention
Pre-test probability assessment Explanation: ***Secondary prevention***
- **Secondary prevention** aims to detect and treat a disease early, before symptoms appear, to prevent its progression or recurrence.
- **Cancer screening tests** such as mammograms, colonoscopies, and Pap smears fit this category perfectly as they are performed in asymptomatic individuals to identify early-stage cancer or pre-cancerous lesions.
*Tertiary prevention*
- **Tertiary prevention** focuses on minimizing the impact of an established disease and improving quality of life through treatment and rehabilitation.
- This would involve managing existing cancer, not screening for it.
*Primary prevention*
- **Primary prevention** aims to prevent a disease from occurring in the first place, often through health promotion and risk reduction.
- Examples include vaccination, lifestyle modifications (e.g., healthy diet, exercise), or avoiding smoking.
*Cancer screening does not fit into these categories*
- This statement is incorrect as cancer screening is a well-established component of preventive healthcare.
- It clearly falls within the defined categories of prevention, specifically secondary prevention.
*Quaternary prevention*
- **Quaternary prevention** aims to protect patients from medical interventions that are likely to cause more harm than good, or to avoid over-medicalization.
- This concept is distinct from screening for diseases and focuses on ethical considerations in medical care.
Pre-test probability assessment US Medical PG Question 7: A 16-year-old presents to the primary care physician because he has noticed an increase in the size of his breast tissue over the past 3 years. He states that he is significantly taller than his entire class at school although he feels increasingly weak and uncoordinated. He performs at the bottom of his grade level academically. On physical exam the patient has marked gynecomastia with small firm testes. The physician decides to perform a karyotype on the patient. What is the most likely outcome of this test?
- A. 47, XYY
- B. 45, XO
- C. 47, XXY (Correct Answer)
- D. 47, XXX
- E. 46, XY
Pre-test probability assessment Explanation: ***47, XXY***
The constellation of **gynecomastia, tall stature, learning difficulties, and small testes** is classic for **Klinefelter syndrome**, which is characterized by a **47, XXY** karyotype.
The presence of an extra X chromosome leads to **hypogonadism** and **endocrine imbalances**, explaining the physical and developmental findings.
*47, XYY*
- Individuals with **47, XYY syndrome** are typically tall but do not usually present with breast enlargement or other features of hypogonadism.
- They may have an increased risk of learning difficulties and behavioral problems.
*45, XO*
- This karyotype, also known as **Turner syndrome**, is characterized by the absence of an X chromosome and typically affects **females**.
- Common features include **short stature, webbed neck, and ovarian dysfunction**, which are inconsistent with the patient's presentation.
*47, XXX*
- This karyotype, known as **Triple X syndrome**, affects **females** and is characterized by the presence of an extra X chromosome.
- While some individuals may experience learning difficulties or developmental delays, it does not cause gynecomastia or small testes in males.
*46, XY*
- This is the **normal male karyotype** and would not explain the patient's symptoms of gynecomastia, small testes, tall stature, or learning difficulties.
- These symptoms suggest an underlying chromosomal abnormality.
Pre-test probability assessment US Medical PG Question 8: A 60-year-old-man presents to his physician with worsening myalgias and new symptoms of early fatigue, muscle weakness, and drooping eyelids. His wife presents with him and states that he never used to have such symptoms. His medical history is significant for gout, hypertension, hypercholesterolemia, diabetes mellitus type II, and pilocytic astrocytoma as a teenager. He denies smoking, drinks a 6-pack of beer per day, and endorses a past history of cocaine use but currently denies any illicit drug use. His vital signs include temperature 36.7°C (98.0°F), blood pressure 126/74 mm Hg, heart rate 87/min, and respiratory rate 15/min. Physical examination shows minimal bibasilar rales, but otherwise clear lungs on auscultation, grade 2/6 holosystolic murmur, 3/5 strength in all extremities, and benign abdominal findings. The Tensilon test result is positive. Which of the following options explains why a chest CT should be ordered for this patient?
- A. Evaluation for mediastinal botulinum abscess
- B. Evaluation of congenital vascular anomaly
- C. Exclusion of underlying lung cancer
- D. Assessment for motor neuron disease
- E. Exclusion of a thymoma (Correct Answer)
Pre-test probability assessment Explanation: ***Exclusion of a thymoma***
- The positive **Tensilon test** strongly indicates **myasthenia gravis**, a condition frequently associated with **thymoma**, a tumor of the thymus gland.
- A **chest CT** is crucial for identifying or excluding a **thymoma** in patients with myasthenia gravis, as its resection can improve symptoms.
*Evaluation for mediastinal botulinum abscess*
- **Botulism** would present with descending paralysis and autonomic dysfunction, and an abscess is not a typical manifestation or diagnostic consideration in this context.
- While mediastinal abscesses can occur, they are usually associated with infection, trauma, or surgery and not directly linked to the patient's symptoms or positive Tensilon test.
*Evaluation of congenital vascular anomaly*
- Congenital vascular anomalies are typically diagnosed earlier in life and are not directly associated with the new onset of myalgias, fatigue, muscle weakness, and ptosis in a 60-year-old.
- There are no clinical signs or symptoms presented that would suggest a vascular anomaly as a cause for his current presentation.
*Exclusion of underlying lung cancer*
- Although lung cancer can cause **paraneoplastic syndromes** such as Lambert-Eaton myasthenic syndrome, the symptoms of myalgias, muscle weakness, and ptosis improving with Tensilon strongly point to **myasthenia gravis**, not a paraneoplastic process.
- The specific combination of symptoms and a positive Tensilon test makes myasthenia gravis and its association with thymoma a more direct concern requiring evaluation.
*Assessment for motor neuron disease*
- **Motor neuron diseases** (e.g., ALS) typically present with progressive muscle weakness, spasticity, and fasciculations, but they do not show improvement with a **Tensilon test**.
- The positive Tensilon test specifically rules against motor neuron disease as the primary cause for the reported symptoms.
Pre-test probability assessment US Medical PG Question 9: A 71-year old man is brought to the emergency department because of progressively worsening shortness of breath and fatigue for 3 days. During the last month, he has also noticed dark colored urine. He had an upper respiratory infection 6 weeks ago. He underwent a cholecystectomy at the age of 30 years. He has hypertension, hyperlipidemia, and type 2 diabetes mellitus. He immigrated to the US from Italy 50 years ago. Current medications include simvastatin, lisinopril, and metformin. He appears pale. His temperature is 37.1°C (98.8°F), pulse is 96/min, respirations are 21/min, and blood pressure is 150/80 mm Hg. Auscultation of the heart shows a grade 4/6 systolic murmur over the right second intercostal space that radiates to the carotids. Laboratory studies show:
Leukocyte count 9,000/mm3
Hemoglobin 8.3 g/dL
Hematocrit 24%
Platelet count 180,000/mm3
LDH 212 U/L
Haptoglobin 15 mg/dL (N=41–165)
Serum
Na+ 138 mEq/L
K+ 4.5 mEq/L
CL- 102 mEq/L
HCO3- 24 mEq/L
Urea nitrogen 20 mg/dL
Creatinine 1.2 mg/dL
Total bilirubin 1.8 mg/dL
Stool testing for occult blood is negative. Direct Coombs test is negative. Echocardiography shows an aortic jet velocity of 4.2 m/s and a mean pressure gradient of 46 mm Hg. Which of the following is the most appropriate next step in management to treat this patient's anemia?
- A. Aortic valve replacement (Correct Answer)
- B. Administration of corticosteroids
- C. Discontinuation of medication
- D. Administration of hydroxyurea
- E. Supplementation with iron
Pre-test probability assessment Explanation: ***Aortic valve replacement***
- The patient's **severe aortic stenosis** (aortic jet velocity >4.0 m/s and mean pressure gradient >40 mmHg) is causing **shear stress** on red blood cells, leading to **microangiopathic hemolytic anemia**. This is characterized by low hemoglobin, high LDH, low haptoglobin, and negative Coombs test.
- **Aortic valve replacement** is the definitive treatment to reduce the shear stress, resolve the hemolysis, and improve the patient's symptoms of anemia and heart failure.
*Administration of corticosteroids*
- Corticosteroids are primarily used in **autoimmune hemolytic anemia** (positive Coombs test), which is not the case here as the direct Coombs test is negative.
- They would not address the underlying **mechanical destruction of red blood cells** due to aortic stenosis.
*Discontinuation of medication*
- The patient's current medications (simvastatin, lisinopril, metformin) are for managing his chronic conditions and are **not associated with hemolytic anemia**. Discontinuing them would be inappropriate and potentially harmful.
- There is no evidence to suggest a **drug-induced hemolytic anemia** in this case.
*Administration of hydroxyurea*
- Hydroxyurea is used in conditions like **sickle cell anemia** or **polycythemia vera** to modify red blood cell production or reduce cell counts, respectively.
- It has no role in treating **mechanical hemolytic anemia** caused by valvular heart disease.
*Supplementation with iron*
- While the patient has anemia, it is a **hemolytic anemia**, not an iron deficiency anemia, as indicated by the low haptoglobin and elevated LDH.
- Iron supplementation would **not stop the destruction of red blood cells** caused by the turbulent flow across the aortic valve.
Pre-test probability assessment US Medical PG Question 10: A 5-year-old boy is brought to the physician because of behavioral problems. His mother says that he has frequent angry outbursts and gets into fights with his classmates. He constantly complains of feeling hungry, even after eating a full meal. He has no siblings, and both of his parents are healthy. He is at the 25th percentile for height and is above the 95th percentile for weight. Physical examination shows central obesity, undescended testes, almond-shaped eyes, and a thin upper lip. Which of the following genetic changes is most likely associated with this patient's condition?
- A. Mitotic nondisjunction of chromosome 21
- B. Mutation of FBN-1 gene on chromosome 15
- C. Microdeletion of long arm of chromosome 7
- D. Loss of paternal gene expression on chromosome 15 (Correct Answer)
- E. Deletion of Phe508 on chromosome 7
Pre-test probability assessment Explanation: ***Loss of paternal gene expression on chromosome 15***
- The patient's symptoms, including **hyperphagia**, **obesity**, behavioral issues, short stature, and **hypogonadism** (undescended testes), are characteristic of **Prader-Willi syndrome**.
- Prader-Willi syndrome is most commonly caused by the **loss of paternal gene expression** from the **q11-q13 region of chromosome 15**, either due to a paternal deletion, maternal uniparental disomy, or a defect in the imprinting center.
*Microdeletion of long arm of chromosome 7*
- A microdeletion on the long arm of chromosome 7 (7q11.23) is associated with **Williams syndrome**, characterized by an **elfin facial appearance**, supravalvular aortic stenosis, and intellectual disability.
- This does not match the patient's symptoms of obesity, hyperphagia, or hypogonadism.
*Deletion of Phe508 on chromosome 7*
- A deletion of phenylalanine at position 508 (**ΔF508**) on chromosome 7 is the most common mutation in the **cystic fibrosis transmembrane conductance regulator (CFTR)** gene, causing **cystic fibrosis**.
- Cystic fibrosis is an **autosomal recessive disorder** requiring mutations in both alleles (inherited from both parents), and primarily affects the exocrine glands, leading to lung disease, pancreatic insufficiency, and infertility, which are unrelated to the patient's presentation.
*Mutation of FBN-1 gene on chromosome 15*
- A mutation in the **FBN1 gene** on chromosome 15 (15q21.1) causes **Marfan syndrome**, which is a connective tissue disorder.
- Marfan syndrome presents with tall stature, long limbs (**arachnodactyly**), lens dislocation, and aortic root dilation, none of which are described in this patient.
*Mitotic nondisjunction of chromosome 21*
- Mitotic nondisjunction of chromosome 21 can lead to **mosaic Down syndrome**, but **trisomy 21** (due to meiotic nondisjunction) is the most common cause of Down syndrome.
- Down syndrome is associated with characteristic facial features, intellectual disability, and congenital heart defects, which are distinct from the symptoms presented.
More Pre-test probability assessment US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.