Laboratory test selection principles US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Laboratory test selection principles. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Laboratory test selection principles US Medical PG Question 1: A scientist in Chicago is studying a new blood test to detect Ab to EBV with increased sensitivity and specificity. So far, her best attempt at creating such an exam reached 82% sensitivity and 88% specificity. She is hoping to increase these numbers by at least 2 percent for each value. After several years of work, she believes that she has actually managed to reach a sensitivity and specificity much greater than what she had originally hoped for. She travels to China to begin testing her newest blood test. She finds 2,000 patients who are willing to participate in her study. Of the 2,000 patients, 1,200 of them are known to be infected with EBV. The scientist tests these 1,200 patients' blood and finds that only 120 of them tested negative with her new exam. Of the patients who are known to be EBV-free, only 20 of them tested positive. Given these results, which of the following correlates with the exam's specificity?
- A. 82%
- B. 90%
- C. 84%
- D. 86%
- E. 98% (Correct Answer)
Laboratory test selection principles Explanation: ***98%***
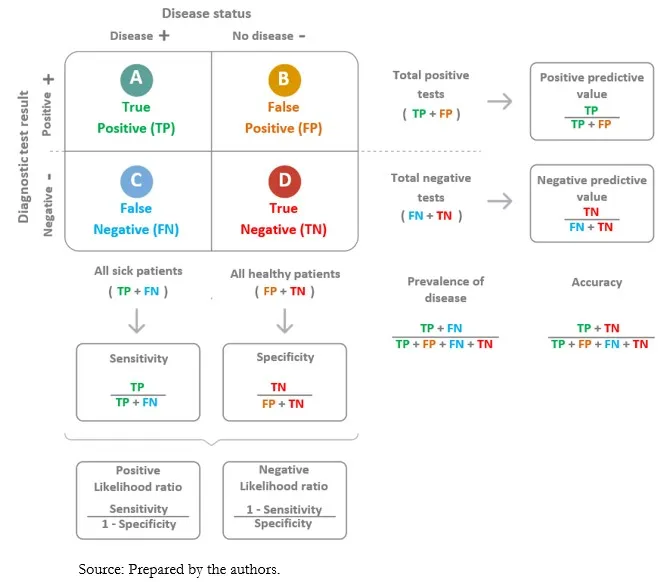
- **Specificity** measures the proportion of **true negatives** among all actual negatives.
- In this case, 800 patients are known to be EBV-free (actual negatives), and 20 of them tested positive (false positives). This means 800 - 20 = 780 tested negative (true negatives). Specificity = (780 / 800) * 100% = **98%**.
*82%*
- This value represents the *original sensitivity* before the scientist’s new attempts to improve the test.
- It does not reflect the *newly calculated specificity* based on the provided data.
*90%*
- This value represents the *newly calculated sensitivity* of the test, not the specificity.
- Out of 1200 EBV-infected patients, 120 tested negative (false negatives), meaning 1080 tested positive (true positives). Sensitivity = (1080 / 1200) * 100% = 90%.
*84%*
- This percentage is not directly derived from the information given for either sensitivity or specificity after the new test results.
- It does not correspond to any of the calculated values for the new test's performance.
*86%*
- This percentage is not directly derived from the information given for either sensitivity or specificity after the new test results.
- It does not correspond to any of the calculated values for the new test's performance.
Laboratory test selection principles US Medical PG Question 2: A mother presents to the family physician with her 16-year-old son. She explains, "There's something wrong with him doc. His grades are getting worse, he's cutting class, he's gaining weight, and his eyes are often bloodshot." Upon interviewing the patient apart from his mother, he seems withdrawn and angry at times when probed about his social history. The patient denies abuse and sexual history. What initial test should be sent to rule out the most likely culprit of this patient's behavior?
- A. Complete blood count
- B. Sexually transmitted infection (STI) testing
- C. Blood culture
- D. Urine toxicology screen (Correct Answer)
- E. Slit lamp examination
Laboratory test selection principles Explanation: ***Urine toxicology screen***
- The patient's presentation with **declining grades**, **cutting class**, **weight gain**, **bloodshot eyes**, and **irritability** are classic signs of **substance abuse** in an adolescent.
- A **urine toxicology screen** is the most appropriate initial test to detect common illicit substances, especially given the clear signs pointing towards drug use.
*Slit lamp examination*
- This test is used to examine the **anterior segment of the eye**, including the conjunctiva, cornea, iris, and lens.
- While the patient has **bloodshot eyes**, this specific test would be more relevant for ruling out ocular infections or injuries, not for diagnosing the underlying cause of systemic behavioral changes.
*Complete blood count*
- A **complete blood count (CBC)** measures different components of the blood, such as red blood cells, white blood cells, and platelets.
- A CBC is a general health indicator and while it can detect infections or anemia, it is not specific or sensitive enough to identify the cause of the behavioral changes described.
*Sexually transmitted infection (STI) testing*
- Although the patient denies sexual history, all adolescents presenting with certain risk factors or symptoms may warrant STI testing in a broader health assessment.
- However, in this scenario, the primary cluster of symptoms (poor grades, cutting class, bloodshot eyes, irritability) points more directly to substance abuse than to an STI.
*Blood culture*
- A **blood culture** is used to detect the presence of bacteria or other microorganisms in the bloodstream, indicating a systemic infection (sepsis).
- The patient's symptoms are not indicative of an acute bacterial bloodstream infection, and a blood culture would not be the initial test for the presented behavioral changes.
Laboratory test selection principles US Medical PG Question 3: An investigator is measuring the blood calcium level in a sample of female cross country runners and a control group of sedentary females. If she would like to compare the means of the two groups, which statistical test should she use?
- A. Chi-square test
- B. Linear regression
- C. t-test (Correct Answer)
- D. ANOVA (Analysis of Variance)
- E. F-test
Laboratory test selection principles Explanation: ***t-test***
- A **t-test** is appropriate for comparing the means of two independent groups, such as the blood calcium levels between runners and sedentary females.
- It assesses whether the observed difference between the two sample means is statistically significant or occurred by chance.
*Chi-square test*
- The **chi-square test** is used to analyze categorical data to determine if there is a significant association between two variables.
- It is not suitable for comparing continuous variables like blood calcium levels.
*Linear regression*
- **Linear regression** is used to model the relationship between a dependent variable (outcome) and one or more independent variables (predictors).
- It aims to predict the value of a variable based on the value of another, rather than comparing means between groups.
*ANOVA (Analysis of Variance)*
- **ANOVA** is used to compare the means of **three or more independent groups**.
- Since there are only two groups being compared in this scenario, a t-test is more specific and appropriate.
*F-test*
- The **F-test** is primarily used to compare the variances of two populations or to assess the overall significance of a regression model.
- While it is the basis for ANOVA, it is not the direct test for comparing the means of two groups.
Laboratory test selection principles US Medical PG Question 4: During an evaluation of a new diagnostic imaging modality for detecting salivary gland tumors, 90 patients tested positive out of the 100 patients who tested positive with the gold standard test. A total of 80 individuals tested negative with the new test out of the 100 individuals who tested negative with the gold standard test. What is the positive likelihood ratio for this test?
- A. 80/90
- B. 90/100
- C. 90/20 (Correct Answer)
- D. 90/110
- E. 10/80
Laboratory test selection principles Explanation: ***90/20***
- The **positive likelihood ratio (LR+)** is calculated as **sensitivity / (1 - specificity)**. To calculate this, we first need to determine the values for true positives (TP), false positives (FP), true negatives (TN), and false negatives (FN).
- Given that 90 out of 100 actual positive patients tested positive, **TP = 90** and **FN = 100 - 90 = 10**. Also, 80 out of 100 actual negative patients tested negative, so **TN = 80** and **FP = 100 - 80 = 20**.
- **Sensitivity** is the true positive rate (TP / (TP + FN)) = 90 / (90 + 10) = 90 / 100.
- **Specificity** is the true negative rate (TN / (TN + FP)) = 80 / (80 + 20) = 80 / 100.
- Therefore, LR+ = (90/100) / (1 - 80/100) = (90/100) / (20/100) = **90/20**.
*80/90*
- This option incorrectly represents the components for the likelihood ratio. It seems to misinterpret the **true negative** count and the **true positive** count.
- It does not follow the formula for LR+ which is **sensitivity / (1 - specificity)**.
*90/100*
- This value represents the **sensitivity** of the test, which is the proportion of true positives among all actual positives.
- It does not incorporate the **false positive rate** (1 - specificity) in the denominator required for the positive likelihood ratio.
*90/110*
- This option incorrectly combines different values, possibly by confusing the denominator for sensitivity or specificity calculations.
- It does not correspond to the formula for the **positive likelihood ratio**.
*10/80*
- This value seems to relate to the inverse of the **false negative rate** (10/100) or misrepresents the relationship between false negatives and true negatives.
- It is not correctly structured to represent the **positive likelihood ratio (LR+)**.
Laboratory test selection principles US Medical PG Question 5: A 21-year-old U.S. born first year medical student with no prior hospital or healthcare work presents to the physician for a routine physical exam. The patient is HIV negative, denies drug use, and denies sick contacts. The physician places a purified protein tuberculin test in the patient's right forearm intradermally. What is the proper time to read the test and induration diameter that would indicate a positive test result?
- A. 36 hours and 7mm diameter
- B. 48 hours and 11mm diameter
- C. 72 hours and 16mm diameter (Correct Answer)
- D. 96 hours and 14mm diameter
- E. 24 hours and 18mm diameter
Laboratory test selection principles Explanation: ***72 hours and 16mm diameter***
- The **purified protein derivative (PPD) test** should ideally be read between 48 and 72 hours after administration to allow for the **Type IV hypersensitivity reaction** to fully develop.
- For individuals with no known risk factors for tuberculosis and no prior exposure, an induration of **≥15 mm** is considered a positive result. A 16mm diameter falls within this range.
*36 hours and 7mm diameter*
- **36 hours** is too early to accurately read a PPD test, as the delayed-type hypersensitivity reaction may not have fully manifested.
- A **7mm induration** would generally be considered negative in a low-risk individual, as the threshold for positivity in this group is higher.
*48 hours and 11mm diameter*
- While **48 hours** is within the acceptable window for reading a PPD test, an **11mm induration** is not considered positive for a young, low-risk individual without any predisposing conditions like HIV or organ transplant.
- The threshold for a positive result in this demographic is typically **≥15 mm**.
*96 hours and 14mm diameter*
- **96 hours** (4 days) is generally too late to accurately read a PPD test, as the reaction may begin to fade, leading to a potentially false negative.
- A **14mm induration** is still below the positive threshold of ≥15mm for a low-risk individual.
*24 hours and 18mm diameter*
- **24 hours** is significantly too early to read a PPD test, as the immune response will not have fully developed, leading to unreliable results.
- While **18mm induration** would be a positive result, the timing makes the reading invalid.
Laboratory test selection principles US Medical PG Question 6: You are reviewing raw data from a research study performed at your medical center examining the effectiveness of a novel AIDS screening examination. The study enrolled 250 patients with confirmed AIDS, and 240 of these patients demonstrated a positive screening examination. The control arm of the study enrolled 250 patients who do not have AIDS, and only 5 of these patients tested positive on the novel screening examination. What is the NPV of this novel test?
- A. 240 / (240 + 15)
- B. 240 / (240 + 5)
- C. 240 / (240 + 10)
- D. 245 / (245 + 10) (Correct Answer)
- E. 245 / (245 + 5)
Laboratory test selection principles Explanation: ***245 / (245 + 10)***
- The **negative predictive value (NPV)** is calculated as **true negatives (TN)** divided by the sum of **true negatives (TN)** and **false negatives (FN)**.
- In this study, there are 250 patients with AIDS; 240 tested positive (true positives, TP), meaning 10 tested negative (false negatives, FN = 250 - 240). There are 250 patients without AIDS; 5 tested positive (false positives, FP), meaning 245 tested negative (true negatives, TN = 250 - 5). Therefore, NPV = 245 / (245 + 10).
*240 / (240 + 15)*
- This calculation incorrectly uses the number of **true positives** (240) in the numerator and denominator, which is relevant for **positive predictive value (PPV)**, not NPV.
- The denominator `(240 + 15)` does not correspond to a valid sum for calculating NPV from the given data.
*240 / (240 + 5)*
- This calculation incorrectly uses **true positives** (240) in the numerator, which is not part of the NPV formula.
- The denominator `(240 + 5)` mixes true positives and false positives, which is incorrect for NPV.
*240 / (240 + 10)*
- This incorrectly places **true positives** (240) in the numerator instead of **true negatives**.
- The denominator `(240+10)` represents **true positives + false negatives**, which is related to sensitivity, not NPV.
*245 / (245 + 5)*
- This calculation correctly identifies **true negatives** (245) in the numerator but incorrectly uses **false positives** (5) in the denominator instead of **false negatives**.
- The denominator for NPV should be **true negatives + false negatives**, which is 245 + 10.
Laboratory test selection principles US Medical PG Question 7: A 23-year-old female college basketball player presents in Sports Clinic after she felt a "pop" in her knee after coming down with a rebound. To examine the patient, you have her lie down on the table with her knees flexed 90 degrees. With your hand around her knee you are able to draw the tibia toward you from underneath the femur. The torn structure implicated by this physical exam maneuver has which of the following attachments?
- A. The posterior intercondylar area of tibia and the posteromedial aspect of the lateral femur
- B. The anterior intercondylar area of tibia and the posteromedial aspect of the lateral femur (Correct Answer)
- C. The patella and tibial tuberosity
- D. The lateral epicondyle of the femur and the head of fibula
- E. The medial condyle of the femur and the medial condyle of the tibia
Laboratory test selection principles Explanation: ***The anterior intercondylar area of tibia and the posteromedial aspect of the lateral femur***
- The patient's presentation with a "pop" in the knee after a basketball maneuver and a positive **anterior drawer test** (drawing the tibia forward) is classic for an **anterior cruciate ligament (ACL) tear**.
- The **ACL originates from the anterior intercondylar area of the tibia** and **inserts into the posteromedial aspect of the lateral femoral condyle**.
*The posterior intercondylar area of tibia and the posteromedial aspect of the lateral femur*
- This describes the attachments of the **posterior cruciate ligament (PCL)**.
- A PCL tear would typically be indicated by a **posterior drawer test** (pushing the tibia backward), which is not described.
*The patella and tibial tuberosity*
- These are the attachment points for the **patellar ligament** (or patellar tendon).
- Injury to the patellar ligament would cause pain and difficulty with knee extension, but not primarily instability evident with an anterior drawer test.
*The lateral epicondyle of the femur and the head of fibula*
- These are the attachment points for the **fibular collateral ligament (LCL)**.
- An LCL injury would present with pain on the lateral side of the knee and instability to **varus stress**, not an anterior drawer.
*The medial condyle of the femur and the medial condyle of the tibia*
- These are general areas involved with the **medial collateral ligament (MCL)**.
- An MCL injury would cause pain on the medial side of the knee and instability to **valgus stress**, not an anterior drawer.
Laboratory test selection principles US Medical PG Question 8: A 60-year-old-man presents to his physician with worsening myalgias and new symptoms of early fatigue, muscle weakness, and drooping eyelids. His wife presents with him and states that he never used to have such symptoms. His medical history is significant for gout, hypertension, hypercholesterolemia, diabetes mellitus type II, and pilocytic astrocytoma as a teenager. He denies smoking, drinks a 6-pack of beer per day, and endorses a past history of cocaine use but currently denies any illicit drug use. His vital signs include temperature 36.7°C (98.0°F), blood pressure 126/74 mm Hg, heart rate 87/min, and respiratory rate 15/min. Physical examination shows minimal bibasilar rales, but otherwise clear lungs on auscultation, grade 2/6 holosystolic murmur, 3/5 strength in all extremities, and benign abdominal findings. The Tensilon test result is positive. Which of the following options explains why a chest CT should be ordered for this patient?
- A. Evaluation for mediastinal botulinum abscess
- B. Evaluation of congenital vascular anomaly
- C. Exclusion of underlying lung cancer
- D. Assessment for motor neuron disease
- E. Exclusion of a thymoma (Correct Answer)
Laboratory test selection principles Explanation: ***Exclusion of a thymoma***
- The positive **Tensilon test** strongly indicates **myasthenia gravis**, a condition frequently associated with **thymoma**, a tumor of the thymus gland.
- A **chest CT** is crucial for identifying or excluding a **thymoma** in patients with myasthenia gravis, as its resection can improve symptoms.
*Evaluation for mediastinal botulinum abscess*
- **Botulism** would present with descending paralysis and autonomic dysfunction, and an abscess is not a typical manifestation or diagnostic consideration in this context.
- While mediastinal abscesses can occur, they are usually associated with infection, trauma, or surgery and not directly linked to the patient's symptoms or positive Tensilon test.
*Evaluation of congenital vascular anomaly*
- Congenital vascular anomalies are typically diagnosed earlier in life and are not directly associated with the new onset of myalgias, fatigue, muscle weakness, and ptosis in a 60-year-old.
- There are no clinical signs or symptoms presented that would suggest a vascular anomaly as a cause for his current presentation.
*Exclusion of underlying lung cancer*
- Although lung cancer can cause **paraneoplastic syndromes** such as Lambert-Eaton myasthenic syndrome, the symptoms of myalgias, muscle weakness, and ptosis improving with Tensilon strongly point to **myasthenia gravis**, not a paraneoplastic process.
- The specific combination of symptoms and a positive Tensilon test makes myasthenia gravis and its association with thymoma a more direct concern requiring evaluation.
*Assessment for motor neuron disease*
- **Motor neuron diseases** (e.g., ALS) typically present with progressive muscle weakness, spasticity, and fasciculations, but they do not show improvement with a **Tensilon test**.
- The positive Tensilon test specifically rules against motor neuron disease as the primary cause for the reported symptoms.
Laboratory test selection principles US Medical PG Question 9: A 28-year-old woman comes to the emergency department for a rash that began 3 days ago. She has low-grade fever and muscle aches. She has no history of serious illness and takes no medications. She has had 5 male sexual partners over the past year and uses condoms inconsistently. Her temperature is 38.1°C (100.6° F), pulse is 85/min, and blood pressure is 126/89 mm Hg. Examination shows a diffuse maculopapular rash that includes the palms and soles. The remainder of the examination shows no abnormalities. A venereal disease research laboratory (VDRL) test is positive. Which of the following is the next appropriate step in management?
- A. Intravenous penicillin G
- B. Dark field microscopy
- C. Treponemal culture
- D. Oral doxycycline
- E. Fluorescent treponemal antibody absorption test (Correct Answer)
Laboratory test selection principles Explanation: ***Fluorescent treponemal antibody absorption test***
- A positive **VDRL** (a non-treponemal test) should be confirmed with a **treponemal-specific test** like the **fluorescent treponemal antibody absorption (FTA-ABS)** test or **Treponema pallidum particle agglutination (TPPA)** assay to definitively diagnose syphilis.
- This confirmatory step helps differentiate true syphilis from false-positive VDRL results, which can occur in autoimmune diseases (SLE, antiphospholipid syndrome), other infections (malaria, mononucleosis), pregnancy, or recent vaccination.
- While this patient's presentation is highly suggestive of **secondary syphilis** (diffuse maculopapular rash involving palms and soles, fever, myalgias, positive VDRL), confirmatory testing is the standard next step before initiating treatment.
- Note: In some clinical settings with classic secondary syphilis, immediate treatment may be initiated, but confirmatory testing remains the most appropriate next diagnostic step.
*Intravenous penicillin G*
- IV aqueous penicillin G is the treatment for **neurosyphilis**, not uncomplicated secondary syphilis.
- **Secondary syphilis** is treated with **intramuscular benzathine penicillin G 2.4 million units** as a single dose.
- Treatment should follow confirmed diagnosis with treponemal-specific testing.
*Dark field microscopy*
- This technique visualizes spirochetes directly from **primary lesions** (chancres) or moist secondary lesions (condyloma lata, mucous patches).
- It is not practical for this patient who has a diffuse maculopapular rash without obvious mucosal or genital lesions.
- Dark-field microscopy requires specialized equipment and expertise not readily available in most emergency departments.
*Treponemal culture*
- **Treponema pallidum** cannot be cultured on artificial media because it is an **obligate pathogen** that requires living host cells.
- Culture is not a diagnostic option for syphilis.
*Oral doxycycline*
- **Doxycycline 100 mg twice daily for 14 days** is an alternative treatment for early syphilis in **penicillin-allergic patients**.
- Treatment should only be initiated after diagnosis is confirmed with treponemal-specific testing.
- This is not the next appropriate step; confirmatory testing comes first.
Laboratory test selection principles US Medical PG Question 10: A 28-year-old man presents with one week of redness and discharge in his eyes, pain and swelling in his left second and third toes, and rash on the soles of his feet. He is sexually active with multiple partners and uses condoms occasionally. He denies any recent travel or illness and does not take any medications. Review of systems is otherwise unremarkable. On physical exam, he has bilateral conjunctivitis, dactylitis of the left second and third toes, and crusty yellow-brown vesicles on his plantar feet. Complete blood count and chemistries are within normal limits. Erythrocyte sedimentation rate (ESR) is 40 mm/h. Toe radiographs demonstrate soft tissue swelling but no fractures. Which diagnostic test should be performed next?
- A. Rheumatoid factor
- B. Anti-cyclic citrullinated peptide antibody assay
- C. HLA-B27
- D. Nucleic acid amplification testing for Chlamydia trachomatis (Correct Answer)
- E. Antinuclear antibody assay
Laboratory test selection principles Explanation: ***Nucleic acid amplification testing for Chlamydia trachomatis***
- The patient's symptoms (conjunctivitis, dactylitis, and plantar rash) with a history of unprotected sexual activity are highly suggestive of **reactive arthritis**, often triggered by **Chlamydia trachomatis infection**.
- **NAAT** is the most sensitive and specific test for detecting *Chlamydia trachomatis* in urethral or urine samples, even in asymptomatic infections.
*Rheumatoid factor*
- This test is primarily used for **rheumatoid arthritis**, which typically presents with symmetric polyarthritis, not the asymmetric dactylitis and conjunctivitis seen here.
- The patient’s acute presentation and specific rash are inconsistent with classic rheumatoid arthritis.
*Anti-cyclic citrullinated peptide antibody assay*
- Like rheumatoid factor, this assay is a specific marker for **rheumatoid arthritis** and would not be the most appropriate first step in diagnosing reactive arthritis.
- Its utility in this clinical context is minimal given the patient's symptoms point away from rheumatoid arthritis.
*HLA-B27*
- While **HLA-B27** is associated with reactive arthritis (and other spondyloarthropathies), it is a **genetic predisposition factor**, not a diagnostic test for acute infection.
- A positive result would confirm susceptibility but would not identify the underlying *Chlamydia* infection that needs treatment.
*Antinuclear antibody assay*
- This assay is used to screen for **systemic lupus erythematosus** and other autoimmune connective tissue diseases.
- The patient's acute presentation of conjunctivitis, dactylitis, and plantar rash is not typical for lupus or similar conditions.
More Laboratory test selection principles US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.