Preventive care integration US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Preventive care integration. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Preventive care integration US Medical PG Question 1: An 11-year-old boy is brought to his pediatrician by his parents for the routine Tdap immunization booster dose that is given during adolescence. Upon reviewing the patient’s medical records, the pediatrician notes that he was immunized according to CDC recommendations, with the exception that he received a catch-up Tdap immunization at the age of 8 years. When the pediatrician asks the boy’s parents about this delay, they inform the doctor that they immigrated to this country 3 years ago from Southeast Asia, where the child had not been immunized against diphtheria, tetanus, and pertussis. Therefore, he received a catch-up series at 8 years of age, which included the first dose of the Tdap vaccine. Which of the following options should the pediatrician choose to continue the boy’s immunization schedule?
- A. A single dose of Td vaccine at 18 years of age
- B. A single dose of Td vaccine now
- C. No further vaccination needed
- D. A single dose of Tdap vaccine now
- E. A single dose of Tdap vaccine at 13 years of age (Correct Answer)
Preventive care integration Explanation: ***A single dose of Tdap vaccine at 13 years of age***
- The CDC recommends a **minimum interval of 5 years** between Tdap doses when Tdap is given as part of a catch-up series.
- Since this patient received his first Tdap at age 8, the earliest he should receive the adolescent booster is at **age 13** (5 years later).
- This timing ensures adequate spacing while still providing the recommended adolescent booster for **pertussis, tetanus, and diphtheria** protection.
- The 5-year interval prevents excessive antigen exposure and optimizes immune response.
*A single dose of Tdap vaccine now*
- Giving Tdap now would result in only a **3-year interval** from the previous Tdap dose at age 8.
- This violates the CDC recommendation of a **minimum 5-year interval** between Tdap doses.
- Shorter intervals may increase local reactogenicity without improving protection.
*A single dose of Td vaccine now*
- While this would provide tetanus and diphtheria protection, it would **not protect against pertussis**, which is a critical component of adolescent vaccination.
- The Tdap vaccine is specifically recommended for adolescents to boost waning pertussis immunity.
- Additionally, giving it now would still be earlier than the recommended 5-year interval from the previous pertussis-containing vaccine.
*A single dose of Td vaccine at 18 years of age*
- This option would result in a **10-year gap** from the last pertussis-containing vaccine, leaving the adolescent vulnerable during high-risk years.
- The adolescent Tdap booster is specifically timed for ages 11-13 to protect during peak transmission periods in middle and high school.
- Waiting until 18 would miss the critical window for pertussis protection.
*No further vaccination needed*
- While the patient completed a catch-up series, the CDC still recommends an **adolescent Tdap booster** even for those who received Tdap in a catch-up series.
- The adolescent booster is important to maintain immunity against pertussis, which wanes significantly over time.
- The booster should be given at age 13 to maintain the 5-year minimum interval.
Preventive care integration US Medical PG Question 2: A 50-year-old woman comes to the physician for a routine health maintenance examination. She has no personal or family history of serious illness. She smoked one pack of cigarettes daily for 5 years during her 20s. Her pulse is 70/min, and blood pressure is 120/78 mm Hg. Serum lipid studies and glucose concentration are within the reference ranges. Which of the following health maintenance recommendations is most appropriate at this time?
- A. Perform BRCA gene test
- B. Perform abdominal ultrasound
- C. Perform 24-hour ECG
- D. Perform DEXA scan
- E. Perform colonoscopy (Correct Answer)
Preventive care integration Explanation: ***Perform colonoscopy***
- **Colorectal cancer screening** with colonoscopy is generally recommended for individuals at average risk starting at age **45-50 years**.
- This patient is **50 years old** and has no increased risk factors, making routine colonoscopy the most appropriate screening.
*Perform BRCA gene test*
- **BRCA gene testing** is indicated for individuals with a strong **family history** of breast or ovarian cancer, or those with personal history suggesting a genetic predisposition.
- This patient has **no personal or family history** of serious illness, so BRCA testing is not warranted.
*Perform abdominal ultrasound*
- **Abdominal ultrasound** is typically used to investigate specific symptoms or screen for conditions like **abdominal aortic aneurysm** in high-risk individuals (e.g., male smokers over 65).
- This patient has **no relevant symptoms** or risk factors for which routine abdominal ultrasound screening is recommended.
*Perform 24-hour ECG*
- A **24-hour ECG (Holter monitor)** is used to detect paroxysmal **arrhythmias** or evaluate symptoms like palpitations, syncope, or dizziness.
- This patient is asymptomatic with a normal pulse and blood pressure; therefore, **routine 24-hour ECG** is not indicated.
*Perform DEXA scan*
- A **DEXA scan** is recommended for **osteoporosis screening** in women typically starting at age **65**, or earlier if they have significant risk factors like a history of fragility fractures or certain medical conditions.
- At **50 years old** and with no apparent risk factors for osteoporosis, a DEXA scan is not yet routinely indicated according to general guidelines.
Preventive care integration US Medical PG Question 3: A 58-year-old woman presents to the physician for a routine gynecological visit. She denies any acute issues and remarks that she has not been sexually active for the past year. Her last Pap test was negative for any abnormal cytology. A pelvic examination and Pap test is performed at the current visit with no remarkable findings. Which of the following approaches to cervical cancer screening is most appropriate for this patient?
- A. Colposcopy in 3 years
- B. Pap test and HPV test in 5 years (Correct Answer)
- C. Pap test only in 5 years
- D. Discontinue screening until the patient becomes sexually active
- E. Colposcopy at the current visit to verify Pap test results
Preventive care integration Explanation: ***Pap test and HPV test in 5 years***
- For women aged 30-65, **co-testing with both a Pap test and HPV test every 5 years** is the preferred screening interval if both results are normal.
- This patient, at 58 years old, falls within this age range, and her prior normal Pap tests along with a normal current one, support a 5-year interval for co-testing.
*Colposcopy in 3 years*
- **Colposcopy** is a diagnostic procedure performed to further evaluate abnormal Pap test results, not a routine screening method.
- Doing a colposcopy in 3 years would be an overly aggressive approach given her history of normal screenings.
*Pap test only in 5 years*
- While a Pap test alone every 3 years is an acceptable screening option, **co-testing with HPV every 5 years** is generally preferred due to its higher sensitivity for detecting precancerous lesions.
- Omitting the HPV test would reduce the effectiveness of the screening strategy in detecting cervical cancer early.
*Discontinue screening until the patient becomes sexually active*
- **Sexual activity** is a risk factor for HPV infection, but cervical cancer screening guidelines do not link its discontinuation to a lack of sexual activity.
- Women over 65 years old with a history of adequate negative screenings may discontinue screening, but this patient is 58 and does not meet that criterion yet.
*Colposcopy at the current visit to verify Pap test results*
- A **colposcopy** is indicated for **abnormal Pap test results**, which this patient does not have.
- Performing a colposcopy in the absence of abnormal findings is unnecessary and not part of routine screening.
Preventive care integration US Medical PG Question 4: A 61-year-old man presents to the family medicine clinic with a worsening cough for the last week. He denies hemoptysis, sputum production, shortness of breath, or upper respiratory tract symptoms. He does endorse nausea and heartburn after he eats large meals, as well as an occasional metallic taste in his mouth throughout the day. He has been diagnosed with hypertension and osteoarthritis, for which he takes lisinopril and aspirin. He has smoked half a pack of cigarettes per day since he was 20 years old. Three years ago, he had his second colonoscopy performed with normal results. His heart rate is 76/min, respiratory rate is 16/min, temperature is 37.3°C (99.2°F), and blood pressure is 148/92 mm Hg. He exhibits signs of truncal obesity. Heart auscultation reveals wide splitting of S2. Auscultation of the lungs is clear, but wheezing is noted on forced expiration. Which of the following is recommended for the patient at this time?
- A. Meningococcal vaccine
- B. Intra-articular steroid injection
- C. Hepatitis B vaccine
- D. Zoster vaccine
- E. Low-dose chest CT (Correct Answer)
Preventive care integration Explanation: ***Low-dose chest CT***
- This patient is a 61-year-old male with a significant **smoking history** (half a pack/day since age 20 is 41 pack-years), placing him at high risk for **lung cancer**.
- **Low-dose chest CT (LDCT) screening** is recommended annually for individuals aged 50-80 with at least a **20 pack-year smoking history** who currently smoke or have quit within the past 15 years.
*Meningococcal vaccine*
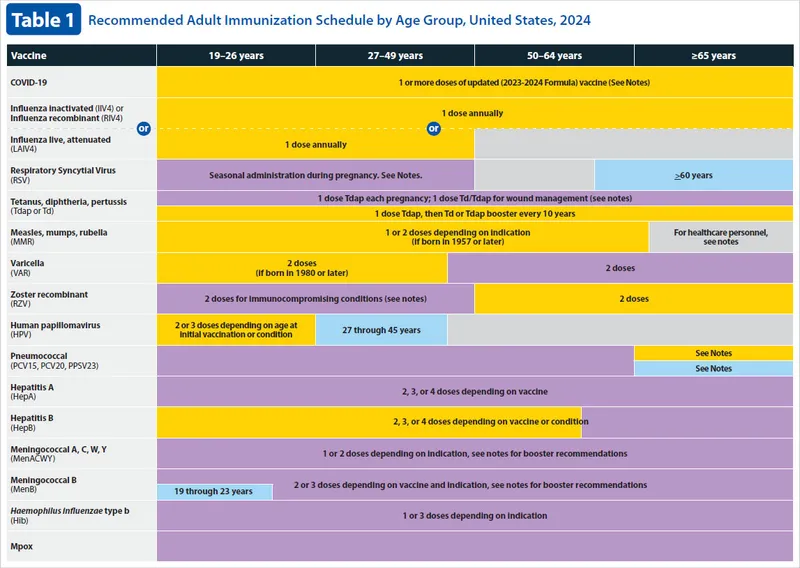
- The **meningococcal vaccine** is routinely recommended for adolescents and young adults, or for specific higher-risk groups such as those with asplenia or complement deficiencies.
- This patient does not fall into a general adult population category for routine meningococcal vaccination at age 61.
*Intra-articular steroid injection*
- The patient has osteoarthritis, but his primary concern is a **worsening cough** and he has not reported increased joint pain or inflammation necessitating this treatment.
- While intra-articular steroid injections are used for osteoarthritis, they do not address the acute cough or the more pressing cancer screening need.
*Hepatitis B vaccine*
- The **Hepatitis B vaccine** is generally recommended for individuals at risk of exposure to the virus, such as healthcare workers, or those with chronic liver disease, diabetes, or HIV.
- There is no information in the patient's presentation to suggest any specific risk factors for Hepatitis B infection that would warrant vaccination at this time.
*Zoster vaccine*
- The **zoster vaccine** is recommended for adults 50 years and older to prevent shingles.
- While this patient is 61 and technically eligible for the zoster vaccine, addressing the more immediate and higher-risk concern of lung cancer screening due to his smoking history takes precedence, and the question asks for *what is recommended at this time*, implying the most urgent or relevant intervention given the clinical picture.
Preventive care integration US Medical PG Question 5: An 18-year-old woman presents for a routine check-up. She is a college student with no complaints. She has a 2 pack-year history of smoking and consumes alcohol occasionally. Her sexual debut was at 15 years of age and has had 2 sexual partners. She takes oral contraceptives and uses barrier contraception. Her family history is significant for cervical cancer in her aunt. Which of the following statements regarding cervical cancer screening in this patient is correct?
- A. The patient requires annual Pap testing due to her family history of cervical cancer.
- B. HPV testing is more preferable than Pap testing in sexually active women under 21 years of age.
- C. It is reasonable to start Pap-test screening at the current visit and repeat it every 3 years.
- D. The patient should undergo screening every 3 years after she turns 21 years of age. (Correct Answer)
- E. The patient does not require Pap testing as long as she uses barrier contraception.
Preventive care integration Explanation: **The patient should undergo screening every 3 years after she turns 21 years of age.**
- Current guidelines recommend initiating cervical cancer screening at **age 21**, regardless of sexual activity.
- The recommended interval for cytology-only screening is **every 3 years** for women aged 21-29.
*The patient requires annual Pap testing due to her family history of cervical cancer.*
- **Family history of cervical cancer** is generally not considered a reason for earlier or more frequent screening in individuals under 21 years of age, unless specific genetic syndromes are suspected, which is not mentioned here.
- The primary risk factor for cervical cancer is **HPV infection**, not direct family history.
*HPV testing is more preferable than Pap testing in sexually active women under 21 years of age.*
- **HPV testing** as a primary screening method is **not recommended for women younger than 25** due to the high prevalence of transient HPV infections that resolve spontaneously in this age group.
- Over-screening and subsequent interventions could lead to unnecessary anxiety and procedures for conditions that would likely resolve on their own.
*It is reasonable to start Pap-test screening at the current visit and repeat it every 3 years.*
- Starting screening at the current age of **18 years is not recommended** according to current guidelines, as screening typically begins at age 21.
- Early screening in this age group often leads to the detection of **transient HPV infections** that would otherwise resolve without intervention, causing undue stress and follow-up.
*The patient does not require Pap testing as long as she uses barrier contraception.*
- While **barrier contraception** (condoms) reduces the risk of HPV transmission, it does not eliminate it entirely and therefore **does not negate the need for cervical cancer screening.**
- Regular screening is still recommended to detect any persistent HPV infections and associated cervical changes early.
Preventive care integration US Medical PG Question 6: A 19-year-old male arrives to student health for an annual check up. He is up to date on his infant and childhood vaccinations up to age 10. At age 12, he received a single dose of the tetanus, diphtheria, and acellular pertussis vaccine, and a quadrivalent meningococcal conjugate vaccine. A month ago, he received the influenza vaccine. The patient has no significant medical history. He takes over the counter ibuprofen for occasional headaches. He has a father with hypertension and hyperlipidemia, and his brother has asthma. He is sexually active with his current girlfriend. He denies tobacco use, illicit drug use, and recent or future travel. The patient’s temperature is 98°F (36.7°C), blood pressure is 118/78 mmHg, pulse is 70/min, and respirations are 14/min with an oxygen saturation of 99% O2 on room air. A physical examination is normal. What of the following is the best recommendation for vaccination?
- A. Human papillomavirus vaccine (Correct Answer)
- B. Hepatitis A vaccine
- C. Herpes zoster vaccine
- D. Pneumococcal vaccine
- E. Tetanus and reduced diphtheria toxoid booster
Preventive care integration Explanation: ***Human papilloma virus***
- This patient, being 19 years old and **sexually active**, is a prime candidate for the **HPV vaccine** to prevent infections that can lead to various cancers.
- The CDC recommends routine HPV vaccination at age 11-12, but catch-up vaccination is recommended for individuals up to age 26 if not adequately vaccinated previously.
*Hepatitis A vaccine*
- The Hepatitis A vaccine is generally recommended for individuals at **increased risk** of infection, such as travelers to endemic areas, men who have sex with men, or those with chronic liver disease, none of which apply to this patient.
- There is no indication for routine vaccination without specific risk factors in this otherwise healthy young male.
*Herpes zoster vaccine*
- The herpes zoster (shingles) vaccine is recommended for adults **age 50 years and older** to prevent shingles.
- This patient is only 19 years old, making him too young for this vaccine recommendation.
*Pneumococcal vaccine*
- Pneumococcal vaccines (PCV13 and PPSV23) are typically recommended for **young children**, adults **65 years and older**, or individuals with **certain underlying medical conditions** (e.g., chronic heart, lung, or kidney disease, or immunocompromised states).
- This 19-year-old patient has no such risk factors for pneumococcal disease.
*Tetanus and reduced diphtheria toxoid booster*
- The patient received a Tdap vaccine at age 12. A Td booster is recommended **every 10 years** for adults.
- Since it has been only 7 years since his last Tdap vaccine, he is not due for a Td booster at this time.
Preventive care integration US Medical PG Question 7: A 65-year-old non-smoking woman with no symptoms comes to your clinic to establish care with a primary care provider. She hasn’t seen a doctor in 12 years and states that she feels very healthy. You realize that guidelines by the national cancer organization suggest that she is due for some cancer screening tests, including a mammogram for breast cancer, a colonoscopy for colon cancer, and a pap smear for cervical cancer. These three screening tests are most likely to be considered which of the following?
- A. Tertiary prevention
- B. Primary prevention
- C. Secondary prevention (Correct Answer)
- D. Cancer screening does not fit into these categories
- E. Quaternary prevention
Preventive care integration Explanation: ***Secondary prevention***
- **Secondary prevention** aims to detect and treat a disease early, before symptoms appear, to prevent its progression or recurrence.
- **Cancer screening tests** such as mammograms, colonoscopies, and Pap smears fit this category perfectly as they are performed in asymptomatic individuals to identify early-stage cancer or pre-cancerous lesions.
*Tertiary prevention*
- **Tertiary prevention** focuses on minimizing the impact of an established disease and improving quality of life through treatment and rehabilitation.
- This would involve managing existing cancer, not screening for it.
*Primary prevention*
- **Primary prevention** aims to prevent a disease from occurring in the first place, often through health promotion and risk reduction.
- Examples include vaccination, lifestyle modifications (e.g., healthy diet, exercise), or avoiding smoking.
*Cancer screening does not fit into these categories*
- This statement is incorrect as cancer screening is a well-established component of preventive healthcare.
- It clearly falls within the defined categories of prevention, specifically secondary prevention.
*Quaternary prevention*
- **Quaternary prevention** aims to protect patients from medical interventions that are likely to cause more harm than good, or to avoid over-medicalization.
- This concept is distinct from screening for diseases and focuses on ethical considerations in medical care.
Preventive care integration US Medical PG Question 8: A 46-year-old woman presents to her primary care physician for her annual examination. At her prior exam one year earlier, she had a Pap smear which was within normal limits. Which of the following health screenings is recommended for this patient?
- A. Colorectal screening (Correct Answer)
- B. Blood glucose and/or HbA1c screening
- C. Blood pressure at least once every 3 years
- D. Yearly Pap smear
- E. Bone mineral density screening
Preventive care integration Explanation: ***Colorectal screening***
- **Colorectal cancer screening** is generally recommended to start at age **45 years** for individuals at average risk.
- This patient is 46 years old, making immediate colorectal screening appropriate based on current guidelines.
*Blood glucose and/or HbA1c screening*
- **Blood glucose or HbA1c screening** for diabetes is recommended starting at age **35 for all adults** or earlier if there are risk factors such as obesity or a family history of diabetes.
- While this patient is 46, this screening should have already been initiated, and it is not the *most* uniquely recommended screening for this specific age that might have been overlooked.
*Blood pressure at least once every 3 years*
- **Blood pressure screening** should be performed **at least annually** for adults aged 40 and older, or more frequently if there are risk factors.
- Screening only every 3 years is insufficient for a 46-year-old patient.
*Yearly Pap smear*
- **Pap smear frequency** has changed; for women aged 30-65 with normal results, screening is recommended every **3 years** with cytology alone, or every 5 years with high-risk HPV testing alone or co-testing.
- A yearly Pap smear is no longer typical practice for a woman with normal prior results and no specific risk factors.
*Bone mineral density screening*
- **Bone mineral density (BMD) screening** for osteoporosis is typically recommended for women starting at age **65 years** or earlier if they have significant risk factors.
- This patient is 46 years old and has no mentioned risk factors, so BMD screening is not routinely indicated at this age.
Preventive care integration US Medical PG Question 9: A 16-year-old girl comes to her primary care physician for an annual check-up. She has no specific complaints. Her medical history is significant for asthma. She uses an albuterol inhaler as needed. She has no notable surgical history. Her mom had breast cancer and her grandfather died of colon cancer. She received all her childhood scheduled vaccinations up to age 8. She reports that she is doing well in school but hates math. She is sexually active with her boyfriend. They use condoms consistently, and they both tested negative recently for gonorrhea, chlamydia, syphilis and human immunodeficiency virus. She asks about birth control. In addition to educating the patient on her options for contraception, which of the following is the best next step in management?
- A. Cytology and human papilloma virus (HPV) testing now and then every 3 years
- B. No HPV-related screening as the patient is low risk
- C. No HPV-related screening and administer HPV vaccine (Correct Answer)
- D. Cytology and HPV testing now and then every 5 years
- E. Cytology now and then every 3 years
Preventive care integration Explanation: ***No HPV-related screening and administer HPV vaccine***
- Current guidelines from organizations like the **American College of Obstetricians and Gynecologists (ACOG)** recommend **HPV vaccination** for individuals aged 9 to 26 years, regardless of sexual activity.
- **Cervical cancer screening (Pap smears and HPV testing)** is not recommended for individuals under 21 years old, as HPV infections in this age group are highly likely to clear spontaneously.
*Cytology and human papilloma virus (HPV) testing now and then every 3 years*
- **Cervical cancer screening** with cytology and HPV testing is not recommended for individuals under **21 years old**, even if sexually active.
- Initiating screening now at age 16 would be **over-screening** and could lead to unnecessary procedures and anxiety given the high rate of spontaneous HPV clearance in adolescents.
*No HPV-related screening as the patient is low risk*
- While the patient is not yet indicated for cervical cancer screening, stating "no HPV-related screening as the patient is low risk" is incomplete. The patient is sexually active, putting her at risk for future HPV infection.
- The most appropriate action is to **offer the HPV vaccine** to prevent future infections, regardless of current screening guidelines.
*Cytology and HPV testing now and then every 5 years*
- This screening frequency (every 5 years) for co-testing is typically recommended for women **over 30 years old** with negative results, not for a 16-year-old.
- As with other screening options, initiating any cervical cancer screening at this age is **not recommended** by current guidelines.
*Cytology now and then every 3 years*
- This option refers to **cytology-only screening**, which is recommended every 3 years for individuals aged 21-29.
- Again, initiating any form of cervical cancer screening at **age 16 is not appropriate** according to current guidelines.
More Preventive care integration US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.