Post-procedure follow-up US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Post-procedure follow-up. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Post-procedure follow-up US Medical PG Question 1: An otherwise healthy 67-year-old woman comes to your clinic after being admitted to the hospital for 2 weeks after breaking her hip. She has not regularly seen a physician for the past several years because she has been working hard at her long-time job as a schoolteacher. You wonder if she has not been taking adequate preventative measures to prevent osteoporosis and order the appropriate labs. Although she is recovering from surgery well, she is visibly upset because she is worried that her hospital bill will bankrupt her. Which of the following best describes her Medicare coverage?
- A. Medicare Part C will cover the majority of drug costs during her inpatient treatment.
- B. Medicare Part A will cover the majority of her hospital fees, including inpatient drugs and lab tests. (Correct Answer)
- C. Medicare is unlikely to cover the cost of her admission because she has not been paying her premium.
- D. Medicare Part B will cover the majority of her hospital fees, including inpatient drugs and lab tests.
- E. Medicare Part D will cover the cost of drugs during her inpatient treatment.
Post-procedure follow-up Explanation: ***Medicare Part A will cover the majority of her hospital fees, including inpatient drugs and lab tests.***
* **Medicare Part A** is hospital insurance and covers **inpatient hospital stays**, skilled nursing facility care, hospice care, and some home health care. This includes services received during an inpatient stay such as drugs, lab tests, and surgery.
* Given her 2-week hospital stay for a broken hip, which resulted in surgery and ongoing recovery, Part A would be the primary payer for the majority of these costs.
*Medicare Part C will cover the majority of drug costs during her inpatient treatment.*
* **Medicare Part C**, also known as **Medicare Advantage**, is an alternative to original Medicare provided by private companies, often including Part A, B, and D benefits.
* While Part C plans can cover drug costs, **inpatient drugs** administered during a hospital stay are typically covered under **Part A**, not a separate drug plan, if the patient is using original Medicare. If she has a Part C plan, it would integrate these benefits.
*Medicare is unlikely to cover the cost of her admission because she has not been paying her premium.*
* Medicare Part A is generally **premium-free** for most individuals who have paid Medicare taxes through their employment for at least 10 years (or 40 quarters).
* Given her long career as a schoolteacher, it is highly likely she would qualify for premium-free Part A, making this statement incorrect.
*Medicare Part B will cover the majority of her hospital fees, including inpatient drugs and lab tests.*
* **Medicare Part B** is medical insurance and covers **doctor's services**, outpatient care, medical supplies, and preventive services.
* While it covers some outpatient lab tests and physician services received during an inpatient stay, it does not cover the primary costs of **inpatient hospital fees** or drugs administered during an inpatient stay, which fall under Part A.
*Medicare Part D will cover the cost of drugs during her inpatient treatment.*
* **Medicare Part D** is prescription drug coverage provided by private companies and covers **outpatient prescription drugs**.
* Medications administered to an **inpatient** during a hospital stay (i.e., when she is admitted) are typically covered under **Medicare Part A**, not Part D.
Post-procedure follow-up US Medical PG Question 2: Five days after undergoing right knee arthroplasty for osteoarthritis, a 68-year-old man has severe pain in his right knee preventing him from participating in physical therapy. On the third postoperative day when the dressing was changed, the surgical wound appeared to be intact, slightly swollen, and had a clear secretion. He has a history of diabetes, hyperlipidemia, and hypertension. Current medications include metformin, enalapril, and simvastatin. His temperature is 37.3°C (99.1°F), pulse is 94/min, and blood pressure is 130/88 mm Hg. His right knee is swollen, erythematous, and tender to palpation. There is pain on movement of the joint. The medial parapatellar skin incision appears superficially opened in its proximal and distal part with yellow-green discharge. There is blackening of the skin on both sides of the incision. Which of the following is the next best step in the management of this patient?
- A. Vacuum dressing
- B. Antiseptic dressing
- C. Nafcillin therapy
- D. Removal of prostheses
- E. Surgical debridement (Correct Answer)
Post-procedure follow-up Explanation: ***Surgical debridement***
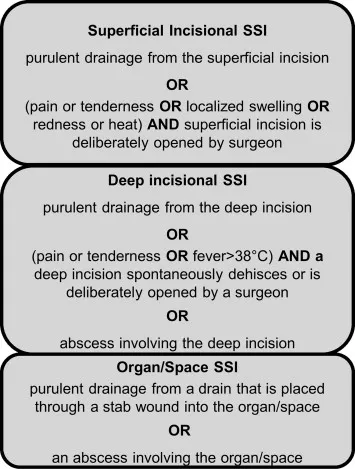
- The patient presents with classic signs of **necrotizing fasciitis** or a severe wound infection: rapidly worsening pain, erythema, swelling, **yellow-green discharge**, and crucially, **blackening of the skin** (indicating tissue necrosis).
- Immediate **surgical debridement** is critical for source control, removal of necrotic tissue, and preventing further spread of infection, which can be life-threatening.
*Vacuum dressing*
- A vacuum-assisted closure (VAC) dressing is used for wound management after adequate debridement or for wounds without signs of aggressive infection to promote healing.
- Applying a VAC dressing to a wound with widespread necrosis and active infection, especially necrotizing fasciitis, without prior debridement would be ineffective and potentially harmful.
*Antiseptic dressing*
- While antiseptic dressings can help reduce bacterial load in some superficial wounds, they are entirely insufficient for deep-seated, rapidly spreading infections with tissue necrosis.
- This approach fails to address the underlying necrotic tissue and the extent of the infection, leading to rapid deterioration.
*Nafcillin therapy*
- **Antibiotic therapy** is essential for treating severe infections; however, it must be combined with source control, especially when necrosis is present.
- Giving antibiotics alone without **surgical debridement** in cases of necrotizing fasciitis is inadequate and will not prevent progression of the infection or improve patient outcomes.
*Removal of prostheses*
- While **prosthesis removal** may be necessary in some cases of established periprosthetic joint infection, it is a definitive and often late measure.
- The immediate priority in a rapidly progressing, necrotic wound infection is **surgical debridement** to remove devitalized tissue and control the local infection, prior to considering implant removal unless the infection is directly on the implant.
Post-procedure follow-up US Medical PG Question 3: A patient presents to the emergency department with arm pain. The patient recently experienced an open fracture of his radius when he fell from a ladder while cleaning his house. Surgical reduction took place and the patient's forearm was put in a cast. Since then, the patient has experienced worsening pain in his arm. The patient has a past medical history of hypertension and asthma. His current medications include albuterol, fluticasone, loratadine, and lisinopril. His temperature is 99.5°F (37.5°C), blood pressure is 150/95 mmHg, pulse is 90/min, respirations are 19/min, and oxygen saturation is 99% on room air. The patient's cast is removed. On physical exam, the patient's left arm is tender to palpation. Passive motion of the patient's wrist and fingers elicits severe pain. The patient's left radial and ulnar pulse are both palpable and regular. The forearm is soft and does not demonstrate any bruising but is tender to palpation. Which of the following is the next best step in management?
- A. Replace the cast with a sling
- B. Measurement of compartment pressure (Correct Answer)
- C. Ibuprofen and reassurance
- D. Emergency fasciotomy
- E. Radiography
Post-procedure follow-up Explanation: ***Measurement of compartment pressure***
- The patient exhibits classic signs of **compartment syndrome**, including severe pain out of proportion to injury, pain with passive stretching, and a history of trauma followed by casting. Measuring compartment pressure is crucial for diagnosis despite palpable pulses.
- Early measurement of compartment pressures can confirm the diagnosis and guide the decision for an **emergency fasciotomy** to prevent irreversible tissue damage.
*Replace the cast with a sling*
- This action would likely worsen the patient's condition by delaying the diagnosis and treatment of potential **compartment syndrome**.
- A sling does not address the underlying issue of increased pressure within the muscle compartments.
*Ibuprofen and reassurance*
- Administering **Ibuprofen (NSAID)** might mask the pain but will not resolve the increased pressure within the compartment, which is a surgical emergency.
- Reassurance without proper assessment of compartment syndrome could lead to irreversible muscle and nerve damage.
*Emergency fasciotomy*
- While a fasciotomy is the definitive treatment for confirmed compartment syndrome, it should only be performed **after compartment pressures have been measured** and the diagnosis confirmed, unless the clinical suspicion is extremely high and pressures cannot be obtained.
- Performing a fasciotomy without objective confirmation is generally not the immediate next step, as it is an invasive procedure with its own risks.
*Radiography*
- **Radiography** would be useful to assess the healing of the fracture or rule out new fractures, but it will not provide information about the soft tissue pressure changes characteristic of compartment syndrome.
- The patient's symptoms are more indicative of a circulatory or soft tissue issue rather than a new bony problem.
Post-procedure follow-up US Medical PG Question 4: An 86-year-old man is admitted to the hospital for management of pneumonia. His hospital course has been relatively uneventful, and he is progressing well. On morning rounds nearing the end of the patient's hospital stay, the patient's cousin finally arrives to the hospital for the first time after not being present for most of the patient's hospitalization. He asks about the patient's prognosis and potential future discharge date as he is the primary caretaker of the patient and needs to plan for his arrival home. The patient is doing well and can likely be discharged in the next few days. Which of the following is the most appropriate course of action?
- A. Bring the cousin to the room and explain the plan to both the patient and cousin
- B. Explain the plan to discharge the patient in the next few days
- C. Explain that you cannot discuss the patient's care at this time
- D. Tell the cousin that you do not know the patient's course well
- E. Bring the cousin to the room and ask the patient if it is acceptable to disclose his course (Correct Answer)
Post-procedure follow-up Explanation: ***Bring the cousin to the room and ask the patient if it is acceptable to disclose his course***
- This option prioritizes **patient autonomy** and privacy by allowing the patient to decide if their medical information can be shared with the cousin.
- Even if the cousin is the primary caretaker, explicit permission from the patient is required under **HIPAA** rules before disclosing protected health information.
- This approach balances **confidentiality protection** with practical discharge planning needs.
*Bring the cousin to the room and explain the plan to both the patient and cousin*
- This option prematurely assumes the patient's consent to share information with the cousin, which may violate **patient privacy**.
- While it facilitates communication, it bypasses the critical step of confirming the patient's willingness to disclose their medical details.
- This constitutes a **HIPAA violation** by disclosing information before obtaining consent.
*Explain the plan to discharge the patient in the next few days*
- Disclosing this information solely to the cousin without the patient's explicit permission constitutes a **breach of confidentiality**.
- This action violates **HIPAA regulations**, even if the cousin is identified as the primary caretaker.
- Protected health information (PHI) cannot be shared with family members without patient authorization.
*Explain that you cannot discuss the patient's care at this time*
- While protecting patient privacy, this response is overly abrupt and unhelpful, potentially creating **frustration** and hindering discharge planning.
- It does not offer a constructive path toward obtaining consent or addressing the cousin's legitimate concerns as a caretaker.
- A better approach involves facilitating consent rather than simply refusing communication.
*Tell the cousin that you do not know the patient's course well*
- This statement is **untruthful** and unprofessional, as the physician on rounds is expected to be knowledgeable about their patient's condition.
- It undermines trust and misrepresents the physician's duty to provide accurate information when appropriate.
- Dishonesty is never an acceptable approach to navigating privacy concerns.
Post-procedure follow-up US Medical PG Question 5: Four days after undergoing a craniotomy and evacuation of a subdural hematoma, a 56-year-old man has severe pain and swelling of his right leg. He has chills and nausea. He has type 2 diabetes mellitus and chronic kidney disease, and was started on hemodialysis 2 years ago. Prior to admission, his medications were insulin, enalapril, atorvastatin, and sevelamer. His temperature is 38.3°C (101°F), pulse is 110/min, and blood pressure is 130/80 mm Hg. Examination shows a swollen, warm, and erythematous right calf. Dorsiflexion of the right foot causes severe pain in the right calf. The peripheral pulses are palpated bilaterally. Cardiopulmonary examination shows no abnormalities. Laboratory studies show:
Hemoglobin 10.1 g/dL
Leukocyte count 11,800/mm3
Platelet count 230,000/mm3
Serum
Glucose 87 mg/dL
Creatinine 1.9 mg/dL
Which of the following is the most appropriate next step in treatment?
- A. Urokinase therapy
- B. Iliac stenting
- C. Warfarin therapy
- D. Unfractionated heparin therapy (Correct Answer)
- E. Inferior vena cava filter
Post-procedure follow-up Explanation: ***Unfractionated heparin therapy***
- The patient presents with classic symptoms of **deep vein thrombosis (DVT)**, including unilateral leg pain, swelling, warmth, erythema, and a positive Homan's sign (pain on dorsiflexion). The recent craniotomy places him at high risk for DVT.
- **Unfractionated heparin is the anticoagulant of choice** for this patient due to TWO critical factors:
1. **Recent craniotomy (4 days ago)**: Requires a rapidly reversible anticoagulant in case of intracranial bleeding; UFH can be reversed with protamine sulfate
2. **Chronic kidney disease on hemodialysis**: Low molecular weight heparin (LMWH) is contraindicated in severe renal failure (CrCl <30 mL/min) as it is renally eliminated and increases bleeding risk. UFH is not renally cleared and can be monitored with aPTT.
*Urokinase therapy*
- **Urokinase is a thrombolytic agent** used to dissolve existing clots, primarily in cases of massive pulmonary embolism or severe DVT with limb-threatening ischemia (phlegmasia cerulea dolens).
- Given the patient's **recent craniotomy and subdural hematoma evacuation**, thrombolytic therapy is **absolutely contraindicated** due to very high risk of intracranial hemorrhage. Recent neurosurgery is a contraindication for at least 2-4 weeks.
*Iliac stenting*
- **Iliac vein stenting** is a procedure typically used to treat chronic **iliac vein compression** (e.g., May-Thurner syndrome) or chronic post-thrombotic obstruction.
- This is an **acute DVT presentation** (4 days post-op) with no indication of chronic iliac vein compression or obstruction. Stenting has no role in acute DVT management.
*Warfarin therapy*
- **Warfarin is an oral anticoagulant** used for long-term DVT treatment but has a **delayed onset of action** (requires 5-7 days to reach therapeutic INR).
- It is **not suitable for acute initial treatment** of DVT, especially in a patient requiring rapid anticoagulation. Warfarin must be overlapped with parenteral anticoagulation (heparin) initially.
- Additionally, warfarin dosing is complex in dialysis patients due to altered vitamin K metabolism.
*Inferior vena cava filter*
- An **IVC filter** is indicated for patients with DVT who have an **absolute contraindication to anticoagulation** (e.g., active bleeding, recent hemorrhagic stroke) or who develop recurrent thromboembolism despite adequate anticoagulation.
- This patient **does not have a contraindication to anticoagulation**. While he had recent neurosurgery, unfractionated heparin is safe to use with careful monitoring and is rapidly reversible if needed.
- IVC filters have significant complications (thrombosis, filter migration, IVC perforation) and should be avoided when anticoagulation is feasible.
Post-procedure follow-up US Medical PG Question 6: Three hours after undergoing open proctocolectomy for ulcerative colitis, a 42-year-old male complains of abdominal pain. The pain is localized to the periumbilical and hypogastric regions. A total of 20 mL of urine has drained from his urinary catheter since the end of the procedure. Temperature is 37.2°C (98.9°F), pulse is 92/min, respirations are 12/min, and blood pressure is 110/72 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 99%. Physical examination shows a 20 cm vertical midline incision and an ileostomy in the right lower quadrant. There is no fluid drainage from the surgical wounds. The urinary catheter flushes easily and is without obstruction. Cardiopulmonary examination shows no abnormalities. Serum studies show a blood urea nitrogen of 30 mg/dL and a creatinine of 1.3 mg/dL. Which of the following is the most appropriate next step in management?
- A. Administer tamsulosin
- B. Administer intravenous furosemide
- C. Obtain an abdominal CT
- D. Start ciprofloxacin
- E. Administer intravenous fluids (Correct Answer)
Post-procedure follow-up Explanation: ***Administer intravenous fluids***
- The patient's **oliguria** (20 mL urine over 3 hours, ~7 mL/hour) post-surgery, elevated **BUN (30 mg/dL)**, and **creatinine (1.3 mg/dL)** with a **BUN:Cr ratio >20:1** suggest **prerenal acute kidney injury** due to **hypovolemia**.
- Post-operative fluid losses from **third-spacing**, blood loss, and insensible losses commonly cause hypovolemia after major abdominal surgery.
- **Intravenous fluids** are the most appropriate initial step to restore intravascular volume and improve renal perfusion.
*Administer tamsulosin*
- **Tamsulosin** is an alpha-blocker used to relax smooth muscle in the prostate and bladder neck, primarily for **urinary retention** due to benign prostatic hyperplasia.
- This patient's oliguria is due to **prerenal azotemia** from hypovolemia, not prostatic obstruction, and the catheter flushes easily without obstruction.
*Administer intravenous furosemide*
- **Furosemide** is a loop diuretic that increases urine output, but administering it in the context of **prerenal acute kidney injury** can worsen hypovolemia and further compromise renal function.
- Diuretics are generally contraindicated in oliguria due to hypovolemia and should only be considered after volume resuscitation.
*Obtain an abdominal CT*
- While an abdominal CT can diagnose surgical complications, there are no immediate signs of a surgical emergency like **anastomotic leak** or **bowel obstruction**.
- Addressing the likely **hypovolemia** is more urgent and should precede further imaging in this scenario.
*Start ciprofloxacin*
- The patient does not show signs of infection, such as fever or localized signs of bacterial peritonitis, making **antibiotics** like ciprofloxacin inappropriate as the initial management step.
- The elevated BUN and creatinine are more indicative of volume depletion than infection.
More Post-procedure follow-up US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.