Sensitivity/Specificity

On this page
🎯 The Diagnostic Accuracy Arsenal: Sensitivity & Specificity Mastery
Diagnostic tests promise answers, but how do you know when to trust them? You'll master sensitivity and specificity-the twin pillars that reveal whether a test catches disease when present and stays silent when absent. By understanding their trade-offs, interpreting test characteristics across clinical contexts, and integrating multiple diagnostics strategically, you'll transform from passive test-orderer to confident clinical decision-maker who knows exactly what each result truly means for your patient.
Understanding sensitivity and specificity unlocks the logic behind every screening protocol, diagnostic algorithm, and clinical decision rule. These twin pillars of diagnostic accuracy determine whether a test excels at catching disease (sensitivity) or avoiding false alarms (specificity), fundamentally shaping how we approach patient care from emergency departments to specialized clinics.
📌 Remember: SNOUT & SPIN - Sensitive tests rule OUT disease when negative; SPecific tests rule IN disease when positive. High sensitivity (>95%) means negative results confidently exclude disease, while high specificity (>95%) means positive results reliably confirm disease presence.
The mathematical precision of these metrics enables clinicians to quantify diagnostic confidence with remarkable accuracy. A test with 99% sensitivity misses only 1 in 100 diseased patients, while 99% specificity generates false positives in just 1 in 100 healthy individuals. This quantitative framework transforms subjective clinical impressions into objective probability assessments.
| Test Characteristic | Sensitivity | Specificity | Clinical Application | Threshold | Example Test |
|---|---|---|---|---|---|
| Screening Excellence | >95% | >80% | Rule out disease | High sensitivity priority | Mammography (85% sens) |
| Confirmatory Power | >80% | >95% | Rule in disease | High specificity priority | Biopsy (99% spec) |
| Balanced Accuracy | 85-95% | 85-95% | General diagnosis | Moderate both | CT angiography |
| Emergency Screening | >98% | >70% | Cannot miss disease | Maximum sensitivity | D-dimer (98% sens) |
| Specialized Confirmation | >70% | >99% | Avoid false positives | Maximum specificity | Genetic testing |
-
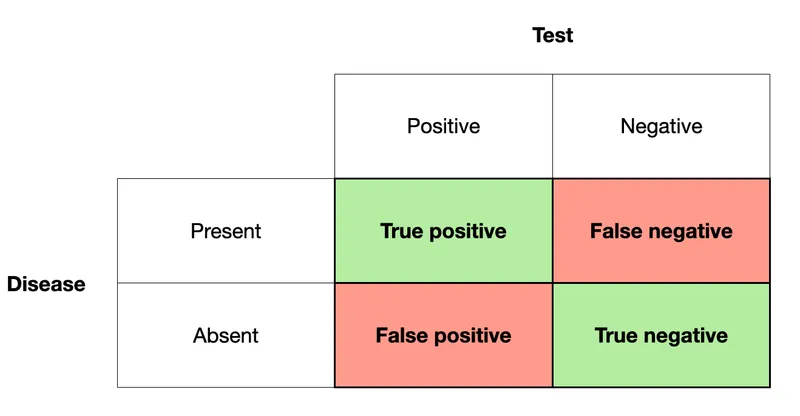
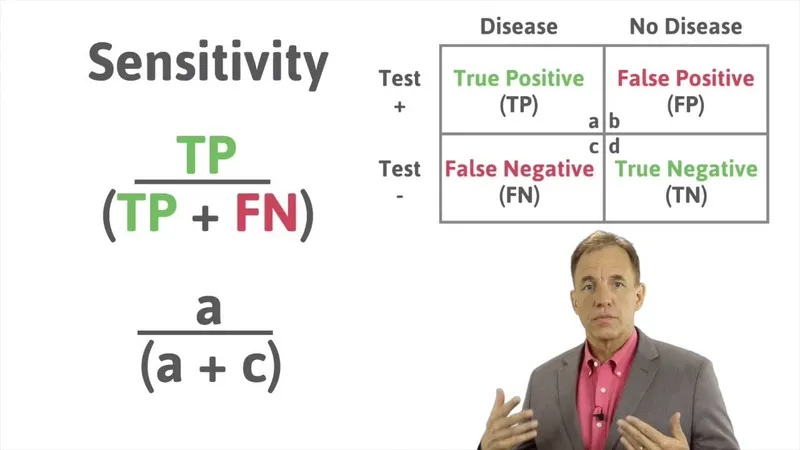
Sensitivity Architecture
- True positive rate: TP/(TP+FN)
- Disease detection capability: 85-99% range for most clinical tests
- False negative rate: (100% - Sensitivity)
- High sensitivity (>95%): False negative rate <5%
- Moderate sensitivity (85%): False negative rate 15%
- Low sensitivity (<80%): False negative rate >20%
-
Specificity Framework
- True negative rate: TN/(TN+FP)
- Healthy population accuracy: 80-99% for diagnostic tests
- False positive rate: (100% - Specificity)
- High specificity (>95%): False positive rate <5%
- Moderate specificity (85%): False positive rate 15%
- Low specificity (<80%): False positive rate >20%
💡 Master This: Sensitivity answers "Of all patients WITH disease, what percentage tests positive?" while specificity answers "Of all patients WITHOUT disease, what percentage tests negative?" These complementary metrics create the foundation for evidence-based diagnostic strategies across all medical specialties.
The mathematical relationship between these metrics reveals why perfect tests remain elusive - improving sensitivity often decreases specificity and vice versa. This trade-off relationship drives the strategic selection of different tests for screening versus confirmation, creating the diagnostic cascade that optimizes patient outcomes while minimizing unnecessary procedures.
🎯 The Diagnostic Accuracy Arsenal: Sensitivity & Specificity Mastery
⚡ The Detection Engine: Sensitivity's Disease-Hunting Power
📌 Remember: SENSITIVE = SCREENING - High sensitivity tests (>95%) excel at screening because they catch nearly all disease cases. Think Sensitive Screening: mammography (85% sensitivity), Pap smears (80% sensitivity), and colonoscopy (95% sensitivity) prioritize disease detection over specificity.
The mathematical foundation reveals sensitivity's clinical power through quantitative thresholds that guide test selection. Tests with >95% sensitivity miss fewer than 5 in 100 diseased patients, making them ideal for conditions where missing disease carries severe consequences. Emergency medicine leverages this principle extensively, accepting higher false-positive rates to ensure life-threatening conditions aren't overlooked.
| Clinical Context | Sensitivity Threshold | False Negative Rate | Example Application | Clinical Consequence |
|---|---|---|---|---|
| Cancer Screening | >90% | <10% | Mammography (85%) | Early detection saves lives |
| Emergency Medicine | >95% | <5% | D-dimer (98%) | Cannot miss PE/DVT |
| Infectious Disease | >85% | <15% | Rapid strep (85%) | Prevent complications |
| Cardiac Events | >90% | <10% | Troponin (95%) | Identify MI quickly |
| Neurological | >80% | <20% | CT stroke (85%) | Time-critical intervention |
-
Sensitivity Calculation Mastery
- Formula: Sensitivity = TP/(TP + FN) × 100%
- True Positives: Diseased patients correctly identified
- False Negatives: Diseased patients incorrectly missed
- High sensitivity (95%): Misses 5% of disease cases
- Moderate sensitivity (85%): Misses 15% of disease cases
- Low sensitivity (70%): Misses 30% of disease cases
-
Clinical Interpretation Framework
- >95% sensitivity: Excellent screening test, negative results rule out disease
- 85-95% sensitivity: Good screening capability, consider confirmatory testing
- <85% sensitivity: Poor screening performance, high miss rate unacceptable
- Exception: When combined with high specificity for confirmation
- Acceptable for non-critical conditions with treatment options
💡 Master This: Sensitivity determines a test's negative predictive power - highly sensitive tests generate confidence in negative results. When mammography shows no abnormalities with 85% sensitivity, the probability of missing early-stage cancer drops to <5% in average-risk populations, justifying annual screening intervals.
The clinical application of sensitivity extends beyond individual test interpretation to shape entire diagnostic algorithms. Sequential testing strategies often begin with highly sensitive screening tests, followed by more specific confirmatory procedures. This approach maximizes disease detection while controlling healthcare costs and patient burden through strategic test selection.
⚡ The Detection Engine: Sensitivity's Disease-Hunting Power
🔍 The Precision Filter: Specificity's False-Alarm Defense System
📌 Remember: SPECIFIC = CONFIRMATION - High specificity tests (>95%) excel at confirmation because positive results reliably indicate disease. Think SPecific Positive IN: tissue biopsy (99% specificity), genetic testing (>99% specificity), and specialized imaging (90-95% specificity) confirm diagnoses with minimal false positives.
The mathematical precision of specificity drives clinical decision-making through quantitative thresholds that minimize healthcare waste and patient harm. Tests with >95% specificity generate false positives in fewer than 5 in 100 healthy patients, making positive results highly reliable for treatment decisions and specialist referrals.
| Test Category | Specificity Range | False Positive Rate | Clinical Application | Cost Implication |
|---|---|---|---|---|
| Tissue Biopsy | >99% | <1% | Definitive diagnosis | High cost, justified accuracy |
| Genetic Testing | >99% | <1% | Hereditary conditions | Expensive, family implications |
| Specialized Imaging | 90-95% | 5-10% | Structural abnormalities | Moderate cost, good accuracy |
| Biomarker Panels | 85-90% | 10-15% | Disease monitoring | Variable cost, trending |
| Point-of-Care Tests | 80-85% | 15-20% | Rapid screening | Low cost, convenience |
-
Specificity Calculation Architecture
- Formula: Specificity = TN/(TN + FP) × 100%
- True Negatives: Healthy patients correctly identified
- False Positives: Healthy patients incorrectly flagged
- High specificity (95%): 5% false positive rate
- Moderate specificity (85%): 15% false positive rate
- Low specificity (70%): 30% false positive rate
-
Clinical Decision Framework
- >95% specificity: Excellent confirmation, positive results reliable
- 85-95% specificity: Good confirmatory capability, consider additional testing
- <85% specificity: Poor confirmation performance, high false-alarm rate
- Acceptable for screening when combined with high sensitivity
- Requires confirmatory testing for positive results
💡 Master This: Specificity determines a test's positive predictive power - highly specific tests generate confidence in positive results. When cardiac catheterization reveals significant stenosis with 95% specificity, the probability of false-positive coronary disease drops to <5%, justifying immediate intervention without additional confirmation.
The economic impact of specificity extends throughout healthcare systems, where false-positive results cascade into unnecessary procedures, specialist consultations, and patient anxiety. High-specificity confirmatory tests serve as gatekeepers, ensuring that expensive or risky interventions target truly diseased patients while protecting healthy individuals from medical overtreatment.
🔍 The Precision Filter: Specificity's False-Alarm Defense System
🎲 The Clinical Decision Matrix: Pattern Recognition Through Diagnostic Accuracy
📌 Remember: RULE-OUT vs RULE-IN - High sensitivity rules OUT disease when negative (SNOUT); High specificity rules IN disease when positive (SPIN). Emergency medicine uses sensitive tests (>95%) to exclude dangerous conditions, while specialists use specific tests (>95%) to confirm diagnoses before treatment.
The diagnostic decision matrix integrates test characteristics with clinical probability to optimize patient outcomes while minimizing unnecessary procedures. This systematic approach prevents both missed diagnoses (through adequate sensitivity) and overtreatment (through adequate specificity), creating cost-effective diagnostic pathways.
| Clinical Scenario | Test Strategy | Sensitivity Priority | Specificity Priority | Decision Logic |
|---|---|---|---|---|
| Chest Pain (ED) | Rule-out MI | >95% | >80% | Cannot miss cardiac event |
| Breast Mass | Screen → Confirm | >90% → >95% | >80% → >95% | Detect early, confirm accurately |
| Cognitive Decline | Exclude reversible | >85% | >90% | Rule out treatable causes |
| Fever in Child | Bacterial vs viral | >90% | >85% | Avoid unnecessary antibiotics |
| Abdominal Pain | Surgical emergency | >95% | >85% | Cannot miss appendicitis |
- High-sensitivity screening: D-dimer (98%), troponin (95%), CT head (95%)
- Decision rule: Negative high-sensitivity test = safe discharge
- Risk tolerance: Accept 10-15% false positives to avoid missing <5% of serious disease
- Pulmonary embolism: Wells score + D-dimer strategy
- Acute coronary syndrome: HEART score + troponin protocol
- Stroke: NIHSS + CT imaging algorithm
- Specialist Confirmation Patterns
- High-specificity confirmation: Biopsy (>99%), angiography (>95%), genetic testing (>99%)
- Decision rule: Positive high-specificity test = proceed with treatment
- Risk tolerance: Accept 5-10% false negatives to avoid >95% false positives
- Cancer diagnosis: Imaging → biopsy → molecular markers
- Coronary disease: Stress test → catheterization → intervention
- Autoimmune disease: Clinical criteria → specific antibodies → treatment
⭐ Clinical Pearl: The "rule-out" strategy uses tests with sensitivity >95% to safely exclude disease. Emergency physicians rely on negative D-dimer (98% sensitivity) to rule out pulmonary embolism in >80% of patients, avoiding unnecessary CT angiography while missing <2% of cases.
💡 Master This: Sequential testing optimizes both sensitivity and specificity through strategic combinations. Mammography (85% sensitivity, 90% specificity) followed by biopsy (80% sensitivity, 99% specificity) achieves >95% overall accuracy while minimizing false positives and unnecessary procedures in breast cancer screening.
The pattern recognition framework extends to test interpretation confidence levels, where clinicians adjust diagnostic certainty based on test characteristics and clinical context. Understanding these mathematical relationships enables precise communication of diagnostic probability to patients and colleagues, improving shared decision-making and treatment adherence.
🎲 The Clinical Decision Matrix: Pattern Recognition Through Diagnostic Accuracy
⚖️ The Diagnostic Balance: Optimizing Sensitivity-Specificity Trade-offs
📌 Remember: THRESHOLD EFFECTS - Lower thresholds increase sensitivity but decrease specificity; Higher thresholds increase specificity but decrease sensitivity. Troponin cutoffs demonstrate this: 0.04 ng/mL achieves 98% sensitivity with 85% specificity, while 0.1 ng/mL achieves 90% sensitivity with 95% specificity.
The mathematical optimization of diagnostic thresholds requires understanding the clinical consequences of false positives versus false negatives. Emergency medicine tolerates higher false-positive rates to avoid missing life-threatening conditions, while specialized diagnostics prioritize specificity to prevent unnecessary interventions.
| Clinical Priority | Threshold Strategy | Sensitivity Target | Specificity Target | Example Application |
|---|---|---|---|---|
| Cannot Miss Disease | Lower threshold | >95% | >80% | PE screening (D-dimer <500) |
| Avoid False Alarms | Higher threshold | >80% | >95% | Cancer confirmation (PSA >10) |
| Balanced Accuracy | Optimal threshold | 85-90% | 85-90% | Diabetes screening (HbA1c 6.5%) |
| Cost Minimization | Economic threshold | >90% | >85% | Cholesterol screening (LDL >130) |
| Population Screening | Epidemiologic threshold | >85% | >90% | Hypertension (BP >140/90) |
-
Threshold Optimization Strategies
- Clinical consequence weighting: False negatives vs false positives
- Population prevalence adjustment: Higher prevalence tolerates lower specificity
- Resource availability consideration: Limited confirmatory testing capacity
- Emergency settings: Prioritize sensitivity (>95%) over specificity (>80%)
- Specialist settings: Prioritize specificity (>95%) over sensitivity (>80%)
- Screening programs: Balance both metrics (>85% each)
-
Economic Impact Assessment
- False positive costs: Unnecessary procedures, anxiety, follow-up testing
- False negative costs: Delayed diagnosis, disease progression, litigation
- Optimal economic threshold: Minimizes total healthcare costs
- Mammography: $50,000 per false positive vs $200,000 per missed cancer
- Colonoscopy: $1,500 per false positive vs $150,000 per missed cancer
- Cardiac catheterization: $15,000 per false positive vs $100,000 per missed MI
💡 Master This: Context-dependent optimization requires different thresholds for the same test in different populations. Troponin cutoffs vary by age, gender, and clinical presentation: 0.04 ng/mL for emergency screening, 0.1 ng/mL for confirmatory diagnosis, and 0.014 ng/mL for high-sensitivity assays in women.
The strategic application of sensitivity-specificity trade-offs extends to test combinations, where sequential or parallel testing strategies can achieve superior overall performance compared to single tests. Understanding these mathematical relationships enables clinicians to design optimal diagnostic pathways that maximize accuracy while minimizing costs and patient burden.
⚖️ The Diagnostic Balance: Optimizing Sensitivity-Specificity Trade-offs
🔗 The Diagnostic Ecosystem: Multi-Test Integration and Advanced Applications
📌 Remember: SERIAL vs PARALLEL - Serial testing (sequence) increases overall specificity but decreases sensitivity; Parallel testing (simultaneous) increases overall sensitivity but decreases specificity. Cancer screening uses serial approach: mammography → ultrasound → biopsy, while emergency medicine uses parallel approach: ECG + troponin + chest X-ray simultaneously.
The mathematical integration of multiple test results creates diagnostic algorithms that achieve >95% accuracy through strategic combinations. These approaches recognize that real-world diagnostic challenges often require multiple data points to reach definitive conclusions, particularly in complex medical conditions with overlapping presentations.
| Integration Strategy | Sensitivity Effect | Specificity Effect | Clinical Application | Example Protocol |
|---|---|---|---|---|
| Serial Testing | Decreases | Increases | Confirmation pathway | Mammography → Biopsy |
| Parallel Testing | Increases | Decreases | Emergency screening | ECG + Troponin + CXR |
| Conditional Testing | Optimized | Optimized | Risk-stratified approach | Wells + D-dimer |
| Bayesian Integration | Dynamic | Dynamic | Probability updating | Clinical + Lab + Imaging |
| Machine Learning | Adaptive | Adaptive | Pattern recognition | AI-assisted diagnosis |
-
Serial Testing Mathematics
- Combined sensitivity: Sens₁ × Sens₂ (multiplicative effect)
- Combined specificity: 1 - [(1-Spec₁) × (1-Spec₂)] (additive effect)
- Clinical example: Mammography (85% sens, 90% spec) → Biopsy (80% sens, 99% spec)
- Overall sensitivity: 0.85 × 0.80 = 68% (decreased)
- Overall specificity: 1 - [(1-0.90) × (1-0.99)] = 99.9% (increased)
-
Parallel Testing Mathematics
- Combined sensitivity: 1 - [(1-Sens₁) × (1-Sens₂)] (additive effect)
- Combined specificity: Spec₁ × Spec₂ (multiplicative effect)
- Clinical example: ECG (85% sens, 90% spec) + Troponin (95% sens, 85% spec)
- Overall sensitivity: 1 - [(1-0.85) × (1-0.95)] = 99.25% (increased)
- Overall specificity: 0.90 × 0.85 = 76.5% (decreased)
⭐ Clinical Pearl: Conditional testing strategies optimize both sensitivity and specificity through risk stratification. The Wells score + D-dimer protocol achieves >98% sensitivity for pulmonary embolism while maintaining >85% specificity by using clinical probability to guide test interpretation and subsequent imaging decisions.
Advanced diagnostic integration incorporates artificial intelligence and machine learning algorithms that continuously optimize sensitivity-specificity trade-offs based on population data and individual patient characteristics. These systems achieve >95% diagnostic accuracy in specialized applications like radiology interpretation and pathology analysis.
- Cutting-Edge Applications
- AI-enhanced mammography: 94% sensitivity, 87% specificity (vs 85%, 90% traditional)
- Machine learning ECG: >95% sensitivity for acute MI detection
- Deep learning pathology: >98% accuracy in cancer diagnosis
- Reduces false positives by 30-40% compared to human interpretation
- Identifies subtle patterns missed by traditional analysis
- Integrates multiple data sources for comprehensive assessment
💡 Master This: Bayesian diagnostic integration continuously updates disease probability as new test results become available. Starting with pre-test probability based on clinical presentation, each additional test result modifies the post-test probability using likelihood ratios derived from sensitivity and specificity values, creating dynamic diagnostic confidence that guides clinical decisions.
The future of diagnostic medicine lies in personalized test selection based on individual patient characteristics, genetic profiles, and risk factors. This precision approach optimizes sensitivity-specificity trade-offs for specific populations, achieving superior diagnostic accuracy while minimizing unnecessary testing and healthcare costs.
🔗 The Diagnostic Ecosystem: Multi-Test Integration and Advanced Applications
🎯 The Clinical Mastery Toolkit: Rapid-Fire Diagnostic Excellence
📌 Remember: The DIAGNOSTIC COMMANDMENTS - SNOUT (Sensitive tests rule OUT), SPIN (Specific tests rule IN), Serial CONFIRMS (↑specificity), Parallel SCREENS (↑sensitivity). Master these four principles, and you possess the foundation for evidence-based diagnostic excellence across all medical specialties.
| Essential Arsenal | Sensitivity | Specificity | Clinical Application | Decision Rule |
|---|---|---|---|---|
| D-dimer | 98% | 40% | PE/DVT screening | Negative = rule out |
| Troponin | 95% | 90% | MI diagnosis | Positive = likely MI |
| Mammography | 85% | 90% | Breast cancer screen | Abnormal → biopsy |
| Colonoscopy | 95% | 95% | Colorectal cancer | Gold standard |
| CT angiography | 90% | 95% | PE confirmation | Positive = treat |
- Rapid Pattern Recognition Drills
- High sensitivity + negative result = Disease ruled out with confidence
- High specificity + positive result = Disease confirmed with confidence
- Low sensitivity + negative result = Cannot exclude disease, need more testing
- Low specificity + positive result = Cannot confirm disease, need confirmation
💡 Master This: The 95% Rule - Tests with >95% sensitivity reliably rule out disease when negative; tests with >95% specificity reliably rule in disease when positive. This threshold represents the clinical confidence level where single-test decisions become defensible in most practice settings.
Clinical Decision Framework: Sensitivity and specificity transform diagnostic uncertainty into quantified probability, enabling evidence-based patient care that optimizes outcomes while minimizing unnecessary procedures and healthcare costs across all medical specialties.
🎯 The Clinical Mastery Toolkit: Rapid-Fire Diagnostic Excellence
Practice Questions: Sensitivity/Specificity
Test your understanding with these related questions
A group of investigators who are studying individuals infected with Trypanosoma cruzi is evaluating the ELISA absorbance cutoff value of serum samples for diagnosis of infection. The previous cutoff point is found to be too high, and the researchers decide to lower the threshold by 15%. Which of the following outcomes is most likely to result from this decision?












