Application in different study designs US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Application in different study designs. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Application in different study designs US Medical PG Question 1: A research team develops a new monoclonal antibody checkpoint inhibitor for advanced melanoma that has shown promise in animal studies as well as high efficacy and low toxicity in early phase human clinical trials. The research team would now like to compare this drug to existing standard of care immunotherapy for advanced melanoma. The research team decides to conduct a non-randomized study where the novel drug will be offered to patients who are deemed to be at risk for toxicity with the current standard of care immunotherapy, while patients without such risk factors will receive the standard treatment. Which of the following best describes the level of evidence that this study can offer?
- A. Level 1
- B. Level 3 (Correct Answer)
- C. Level 5
- D. Level 4
- E. Level 2
Application in different study designs Explanation: ***Level 3***
- A **non-randomized controlled trial** like the one described, where patient assignment to treatment groups is based on specific characteristics (risk of toxicity), falls into Level 3 evidence.
- This level typically includes **non-randomized controlled trials** and **well-designed cohort studies** with comparison groups, which are prone to selection bias and confounding.
- The study compares two treatments but lacks randomization, making it Level 3 evidence.
*Level 1*
- Level 1 evidence is the **highest level of evidence**, derived from **systematic reviews and meta-analyses** of multiple well-designed randomized controlled trials or large, high-quality randomized controlled trials.
- The described study is explicitly stated as non-randomized, ruling out Level 1.
*Level 2*
- Level 2 evidence involves at least one **well-designed randomized controlled trial** (RCT) or **systematic reviews** of randomized trials.
- The current study is *non-randomized*, which means it cannot be classified as Level 2 evidence, as randomization is a key criterion for this level.
*Level 4*
- Level 4 evidence includes **case series**, **case-control studies**, and **poorly designed cohort or case-control studies**.
- While the study is non-randomized, it is a controlled comparative trial rather than a case series or retrospective case-control study, placing it at Level 3.
*Level 5*
- Level 5 evidence is the **lowest level of evidence**, typically consisting of **expert opinion** without explicit critical appraisal, or based on physiology, bench research, or animal studies.
- While the drug was initially tested in animal studies, the current human comparative study offers a higher level of evidence than expert opinion or preclinical data.
Application in different study designs US Medical PG Question 2: A medical research study is evaluating an investigational novel drug (medication 1) as compared with standard therapy (medication 2) in patients presenting to the emergency department with myocardial infarction (MI). The study enrolled a total of 3,000 subjects, 1,500 in each study arm. Follow-up was conducted at 45 days post-MI. The following are the results of the trial:
Endpoints Medication 1 Medication 2 P-Value
Primary: death from cardiac causes 134 210 0.03
Secondary: hyperkalemia 57 70 0.4
What is the relative risk of death from a cardiac cause, expressed as a percentage? (Round to the nearest whole number.)
- A. 64% (Correct Answer)
- B. 42%
- C. 72%
- D. 36%
- E. 57%
Application in different study designs Explanation: ***64%***
- The **relative risk (RR)** is calculated as the event rate in the exposed group divided by the event rate in the unexposed (control) group.
- For cardiac death, the event rate for Medication 1 is 134/1500 = 0.0893, and for Medication 2 is 210/1500 = 0.14. Therefore, RR = 0.0893 / 0.14 = 0.6378.
- Expressing as a percentage: 0.6378 × 100 = 63.78%, which rounds to **64%**.
- This indicates that Medication 1 has 64% of the risk of cardiac death compared to Medication 2, representing a **36% relative risk reduction**.
*42%*
- This option is incorrect as it does not reflect the accurate calculation of **relative risk** using the provided event rates.
- A calculation error or conceptual misunderstanding of the relative risk formula would lead to this value.
*72%*
- This percentage is higher than the calculated relative risk, suggesting an incorrect application of the formula or a misinterpretation of the event rates.
- It does not represent the ratio of risk between the two medication groups for cardiac death.
*36%*
- This value represents the **relative risk reduction** (100% - 64% = 36%), not the relative risk itself.
- This is a common error where students confuse relative risk with relative risk reduction.
*57%*
- While closer to the correct answer, this value is not the precise result when rounding to the nearest whole number.
- Small calculation discrepancies or rounding at intermediate steps could lead to this slightly different percentage.
Application in different study designs US Medical PG Question 3: A recent study attempted to analyze whether increased "patient satisfaction" driven healthcare resulted in increased hospitalization. In this hospital, several of the wards adopted new aspects of "patient satisfaction" driven healthcare, whereas the remainder of the hospital continued to use existing protocols. Baseline population characteristics and demographics were collected at the start of the study. At the end of the following year, hospital use was assessed and compared between the two groups. Which of the following best describes this type of study?
- A. Prospective cohort (Correct Answer)
- B. Cross-sectional study
- C. Retrospective case-control
- D. Prospective case-control
- E. Retrospective cohort
Application in different study designs Explanation: ***Prospective cohort***
- This study design involves following a group of **exposed individuals (patient satisfaction-driven healthcare)** and a group of **unexposed individuals (existing protocols)** forward in time to observe the development of an outcome (**hospitalization**).
- The exposure status is determined at the **start of the study (baseline)**, and outcomes are measured prospectively over a period, which aligns with observing hospital use over the following year.
*Cross-sectional study*
- A **cross-sectional study** assesses both exposure and outcome simultaneously at a single point in time, providing a snapshot.
- This study design involves follow-up over a year, making it unsuitable for a cross-sectional classification.
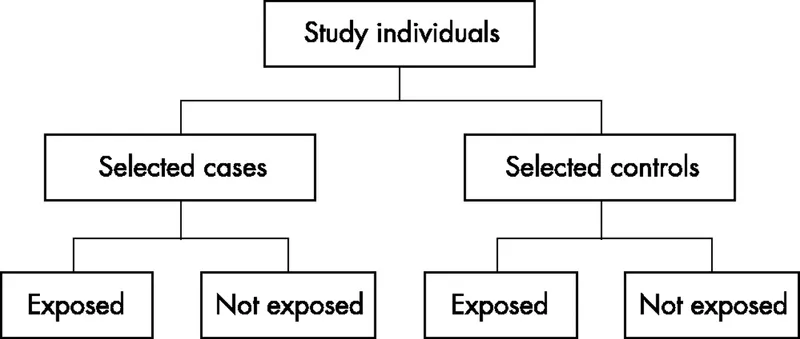
*Retrospective case-control*
- A **retrospective case-control study** begins with identifying individuals based on their outcome status (cases with the outcome and controls without the outcome) and then looks back in time to determine past exposures.
- This study starts by defining exposure groups and then follows them to observe future outcomes, which is the opposite of a case-control design.
*Prospective case-control*
- A **prospective case-control study** is a less common and often refers to a nested case-control study within a cohort, where cases and controls are selected from a larger cohort that has been followed prospectively.
- The described study directly follows entire exposed and unexposed groups without specifically selecting cases and controls from a pre-defined cohort.
*Retrospective cohort*
- A **retrospective cohort study** defines cohorts based on past exposures using existing data and then looks back in time to determine outcomes that have already occurred.
- The study explicitly states that hospital use was assessed at the "end of the following year," indicating a forward-looking collection of outcome data, not a retrospective assessment of already recorded outcomes.
Application in different study designs US Medical PG Question 4: A researcher is trying to determine whether a newly discovered substance X can be useful in promoting wound healing after surgery. She conducts this study by enrolling the next 100 patients that will be undergoing this surgery and separating them into 2 groups. She decides which patient will be in which group by using a random number generator. Subsequently, she prepares 1 set of syringes with the novel substance X and 1 set of syringes with a saline control. Both of these sets of syringes are unlabeled and the substances inside cannot be distinguished. She gives the surgeon performing the surgery 1 of the syringes and does not inform him nor the patient which syringe was used. After the study is complete, she analyzes all the data that was collected and performs statistical analysis. This study most likely provides which level of evidence for use of substance X?
- A. Level 3
- B. Level 1 (Correct Answer)
- C. Level 4
- D. Level 5
- E. Level 2
Application in different study designs Explanation: ***Level 1***
- The study design described is a **randomized controlled trial (RCT)**, which is considered the **highest level of evidence (Level 1)** in the hierarchy of medical evidence.
- Key features like **randomization**, **control group**, and **blinding (double-blind)** help minimize bias and strengthen the validity of the findings.
*Level 2*
- Level 2 evidence typically comprises **well-designed controlled trials without randomization** (non-randomized controlled trials) or **high-quality cohort studies**.
- While strong, they do not possess the same level of internal validity as randomized controlled trials.
*Level 3*
- Level 3 evidence typically includes **case-control studies** or **cohort studies**, which are observational designs and carry a higher risk of bias compared to RCTs.
- These studies generally do not involve randomization or intervention assignment by the researchers.
*Level 4*
- Level 4 evidence is usually derived from **case series** or **poor quality cohort and case-control studies**.
- These studies provide descriptive information or investigate associations without strong control for confounding factors.
*Level 5*
- Level 5 evidence is the **lowest level of evidence**, consisting of **expert opinion** or **animal research/bench research**.
- This level lacks human clinical data or systematic investigative rigor needed for higher evidence levels.
Application in different study designs US Medical PG Question 5: A 6-month-old male presents for a routine visit to his pediatrician. Two months ago, the patient was seen for tachypnea and wheezing, and diagnosed with severe respiratory syncytial virus (RSV) bronchiolitis. After admission to the hospital and supportive care, the patient recovered and currently is not experiencing any trouble breathing. Regarding the possibility of future reactive airway disease, which of the following statements is most accurate?
- A. “There is no clear relationship between RSV and the development of asthma.”
- B. “Your child has a greater than 20% chance of developing asthma” (Correct Answer)
- C. “Your child’s risk of asthma is less than the general population.”
- D. “Your child has a less than 5% chance of developing asthma”
- E. “Your child’s risk of asthma is the same as the general population.”
Application in different study designs Explanation: ***“Your child has a greater than 20% chance of developing asthma”***
- Severe **RSV bronchiolitis** in infancy is a significant risk factor for the development of **recurrent wheezing** and **childhood asthma**.
- Studies estimate that a substantial proportion, often greater than 20%, of infants with severe RSV bronchiolitis will go on to develop **asthma** later in childhood.
*“There is no clear relationship between RSV and the development of asthma.”*
- This statement is incorrect as there is a **well-established link** between severe RSV infection in early life and an increased risk of developing **asthma**.
- Numerous epidemiological and longitudinal studies have documented this association.
*“Your child’s risk of asthma is less than the general population.”*
- This is incorrect, as severe RSV infection **increases** the risk of asthma, not decreases it.
- Children with a history of severe RSV have a **higher incidence** of asthma compared to the general pediatric population.
*“Your child has a less than 5% chance of developing asthma”*
- This percentage is **too low** given the known association between severe RSV bronchiolitis and subsequent asthma.
- The actual risk is considerably higher, typically falling into the range of 20-50% for those with severe RSV.
*“Your child’s risk of asthma is the same as the general population.”*
- This statement is inaccurate because severe RSV infection in infancy is a recognized independent **risk factor** for **asthma development**.
- Therefore, the child's risk is elevated above that of the general population.
Application in different study designs US Medical PG Question 6: A research group wants to assess the safety and toxicity profile of a new drug. A clinical trial is conducted with 20 volunteers to estimate the maximum tolerated dose and monitor the apparent toxicity of the drug. The study design is best described as which of the following phases of a clinical trial?
- A. Phase 0
- B. Phase III
- C. Phase V
- D. Phase II
- E. Phase I (Correct Answer)
Application in different study designs Explanation: ***Phase I***
- **Phase I clinical trials** involve a small group of healthy volunteers (typically 20-100) to primarily assess **drug safety**, determine a safe dosage range, and identify side effects.
- The main goal is to establish the **maximum tolerated dose (MTD)** and evaluate the drug's pharmacokinetic and pharmacodynamic profiles.
*Phase 0*
- **Phase 0 trials** are exploratory studies conducted in a very small number of subjects (10-15) to gather preliminary data on a drug's **pharmacodynamics and pharmacokinetics** in humans.
- They involve microdoses, not intended to have therapeutic effects, and thus cannot determine toxicity or MTD.
*Phase III*
- **Phase III trials** are large-scale studies involving hundreds to thousands of patients to confirm the drug's **efficacy**, monitor side effects, compare it to standard treatments, and collect information that will allow the drug to be used safely.
- These trials are conducted after safety and initial efficacy have been established in earlier phases.
*Phase V*
- "Phase V" is not a standard, recognized phase in the traditional clinical trial classification (Phase 0, I, II, III, IV).
- This term might be used in some non-standard research contexts or for post-marketing studies that go beyond Phase IV surveillance, but it is not a formal phase for initial drug development.
*Phase II*
- **Phase II trials** involve several hundred patients with the condition the drug is intended to treat, focusing on **drug efficacy** and further evaluating safety.
- While safety is still monitored, the primary objective shifts to determining if the drug works for its intended purpose and at what dose.
Application in different study designs US Medical PG Question 7: A physician attempts to study cirrhosis in his state. Using a registry of admitted patients over the last 10 years at the local hospital, he isolates all patients who have been diagnosed with cirrhosis. Subsequently, he contacts this group of patients, asking them to complete a survey assessing their prior exposure to alcohol use, intravenous drug abuse, blood transfusions, personal history of cancer, and other medical comorbidities. An identical survey is given to an equal number of patients in the registry who do not carry a prior diagnosis of cirrhosis. Which of the following is the study design utilized by this physician?
- A. Randomized controlled trial
- B. Case-control study (Correct Answer)
- C. Cross-sectional study
- D. Cohort study
- E. Meta-analysis
Application in different study designs Explanation: ***Case-control study***
- This study design **identifies subjects based on their outcome (cases with cirrhosis, controls without cirrhosis)** and then retrospectively investigates their past exposures.
- The physician selected patients with cirrhosis (cases) and patients without cirrhosis (controls), then assessed their prior exposures to risk factors like alcohol use and intravenous drug abuse.
*Randomized controlled trial*
- This design involves randomly assigning participants to an **intervention group** or a **control group** to assess the effect of an intervention.
- There is no intervention being tested or randomization occurring in this study; it is observational.
*Cross-sectional study*
- A cross-sectional study measures the **prevalence of disease and exposure at a single point in time** in a defined population.
- This study collects retrospective exposure data and compares two distinct groups (cases and controls), rather than assessing prevalence at one time point.
*Cohort study*
- A cohort study **follows a group of individuals over time** to see if their exposure to a risk factor is associated with the development of a disease.
- This study starts with the outcome (cirrhosis) and looks backward at exposures, which is the opposite direction of a cohort study.
*Meta-analysis*
- A meta-analysis is a statistical method that **combines the results of multiple independent studies** to produce a single, more powerful estimate of treatment effect or association.
- This is an original research study collecting new data, not a systematic review or synthesis of existing studies.
Application in different study designs US Medical PG Question 8: A medical research study is beginning to evaluate the positive predictive value of a novel blood test for non-Hodgkin’s lymphoma. The diagnostic arm contains 700 patients with NHL, of which 400 tested positive for the novel blood test. In the control arm, 700 age-matched control patients are enrolled and 0 are found positive for the novel test. What is the PPV of this test?
- A. 400 / (400 + 0) (Correct Answer)
- B. 700 / (700 + 300)
- C. 400 / (400 + 300)
- D. 700 / (700 + 0)
- E. 700 / (400 + 400)
Application in different study designs Explanation: ***400 / (400 + 0) = 1.0 or 100%***
- The **positive predictive value (PPV)** is calculated as **True Positives / (True Positives + False Positives)**.
- In this scenario, **True Positives (TP)** are the 400 patients with NHL who tested positive, and **False Positives (FP)** are 0, as no control patients tested positive.
- This gives a PPV of 400/400 = **1.0 or 100%**, indicating that all patients who tested positive actually had the disease.
*700 / (700 + 300)*
- This calculation does not align with the formula for PPV based on the given data.
- The denominator `(700+300)` suggests an incorrect combination of various patient groups.
*400 / (400 + 300)*
- The denominator `(400+300)` incorrectly includes 300, which is the number of **False Negatives** (patients with NHL who tested negative), not False Positives.
- PPV focuses on the proportion of true positives among all positive tests, not all diseased individuals.
*700 / (700 + 0)*
- This calculation incorrectly uses the total number of patients with NHL (700) as the numerator, rather than the number of positive test results in that group.
- The numerator should be the **True Positives** (400), not the total number of diseased individuals.
*700 / (400 + 400)*
- This calculation uses incorrect values for both the numerator and denominator, not corresponding to the PPV formula.
- The numerator 700 represents the total number of patients with the disease, not those who tested positive, and the denominator incorrectly sums up values that don't represent the proper PPV calculation.
Application in different study designs US Medical PG Question 9: In a randomized controlled trial studying a new treatment, the primary endpoint (mortality) occurred in 14.4% of the treatment group and 16.7% of the control group. Which of the following represents the number of patients needed to treat to save one life, based on the primary endpoint?
- A. 1/(0.144 - 0.167)
- B. 1/(0.167 - 0.144) (Correct Answer)
- C. 1/(0.300 - 0.267)
- D. 1/(0.267 - 0.300)
- E. 1/(0.136 - 0.118)
Application in different study designs Explanation: ***1/(0.167 - 0.144)***
- The **Number Needed to Treat (NNT)** is calculated as **1 / Absolute Risk Reduction (ARR)**.
- The **Absolute Risk Reduction (ARR)** is the difference between the event rate in the control group (16.7%) and the event rate in the treatment group (14.4%), which is **0.167 - 0.144**.
*1/(0.144 - 0.167)*
- This calculation represents 1 divided by the **Absolute Risk Increase**, which would be relevant if the treatment increased mortality.
- The **NNT should always be a positive value**, indicating the number of patients to treat to prevent one adverse event.
*1/(0.300 - 0.267)*
- This option uses arbitrary numbers (0.300 and 0.267) that do not correspond to the given **mortality rates** in the problem.
- It does not reflect the correct calculation for **absolute risk reduction** based on the provided data.
*1/(0.267 - 0.300)*
- This option also uses arbitrary numbers not derived from the problem's data, and it would result in a **negative value** for the denominator.
- The difference between event rates of 0.267 and 0.300 is not present in the given information for this study.
*1/(0.136 - 0.118)*
- This calculation uses arbitrary numbers (0.136 and 0.118) that are not consistent with the reported **mortality rates** of 14.4% and 16.7%.
- These values do not represent the **Absolute Risk Reduction** required for calculating NNT in this specific scenario.
Application in different study designs US Medical PG Question 10: A prospective cohort study was conducted to assess the relationship between LDL and the incidence of heart disease. The patients were selected at random. Results showed a 10-year relative risk of 2.3 for people with elevated LDL levels compared to individuals with normal LDL levels. The 95% confidence interval was 1.05-3.50. This study is most likely to have which of the following p values?
- A. 0.20
- B. 0.06
- C. 0.08
- D. 0.04 (Correct Answer)
- E. 0.10
Application in different study designs Explanation: ***0.04***
- A 95% confidence interval that **does not include 1 (one)** suggests a **statistically significant** association, meaning the p-value is likely to be **less than 0.05**.
- The given CI of 1.05-3.50 for the relative risk (RR) is entirely above 1, indicating a significant positive association, and therefore, a p-value less than 0.05.
*0.20*
- A p-value of 0.20 is **greater than 0.05**, which would imply the finding is **not statistically significant**.
- If the p-value were 0.20, the 95% confidence interval would likely **include 1**, suggesting no significant difference in risk.
*0.06*
- A p-value of 0.06 is **greater than 0.05**, indicating that the association is **not statistically significant at the conventional alpha level**.
- If the p-value were 0.06, the 95% confidence interval would likely **include 1**, or be very close to including it, contradicting the given CI of 1.05-3.50.
*0.08*
- A p-value of 0.08 is **greater than 0.05**, indicating that the finding is **not statistically significant**.
- If the p-value were 0.08, the 95% confidence interval would almost certainly **include 1**, which is inconsistent with the provided interval.
*0.10*
- A p-value of 0.10 is **greater than 0.05**, which signifies that the finding is **not statistically significant**.
- If the p-value were 0.10, the 95% confidence interval for the relative risk would typically **include 1**, contradicting the given confidence interval.
More Application in different study designs US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.