Reporting in clinical guidelines US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Reporting in clinical guidelines. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Reporting in clinical guidelines US Medical PG Question 1: You are conducting a study comparing the efficacy of two different statin medications. Two groups are placed on different statin medications, statin A and statin B. Baseline LDL levels are drawn for each group and are subsequently measured every 3 months for 1 year. Average baseline LDL levels for each group were identical. The group receiving statin A exhibited an 11 mg/dL greater reduction in LDL in comparison to the statin B group. Your statistical analysis reports a p-value of 0.052. Which of the following best describes the meaning of this p-value?
- A. There is a 95% chance that the difference in reduction of LDL observed reflects a real difference between the two groups
- B. Though A is more effective than B, there is a 5% chance the difference in reduction of LDL between the two groups is due to chance
- C. If 100 permutations of this experiment were conducted, 5 of them would show similar results to those described above
- D. This is a statistically significant result
- E. There is a 5.2% chance of observing a difference in reduction of LDL of 11 mg/dL or greater even if the two medications have identical effects (Correct Answer)
Reporting in clinical guidelines Explanation: **There is a 5.2% chance of observing a difference in reduction of LDL of 11 mg/dL or greater even if the two medications have identical effects**
- The **p-value** represents the probability of observing results as extreme as, or more extreme than, the observed data, assuming the **null hypothesis** is true (i.e., there is no true difference between the groups).
- A p-value of 0.052 means there's approximately a **5.2% chance** that the observed 11 mg/dL difference (or a more substantial difference) occurred due to **random variation**, even if both statins were equally effective.
*There is a 95% chance that the difference in reduction of LDL observed reflects a real difference between the two groups*
- This statement is an incorrect interpretation of the p-value; it confuses the p-value with the **probability that the alternative hypothesis is true**.
- A p-value does not directly tell us the probability that the observed difference is "real" or due to the intervention being studied.
*Though A is more effective than B, there is a 5% chance the difference in reduction of LDL between the two groups is due to chance*
- This statement implies that Statin A is more effective, which cannot be concluded with a p-value of 0.052 if the significance level (alpha) was set at 0.05.
- While it's true there's a chance the difference is due to chance, claiming A is "more effective" based on this p-value before statistical significance is usually declared is misleading.
*If 100 permutations of this experiment were conducted, 5 of them would show similar results to those described above*
- This is an incorrect interpretation. The p-value does not predict the outcome of repeated experiments in this manner.
- It refers to the **probability under the null hypothesis in a single experiment**, not the frequency of results across multiple hypothetical repetitions.
*This is a statistically significant result*
- A p-value of 0.052 is generally considered **not statistically significant** if the conventional alpha level (significance level) is set at 0.05 (or 5%).
- For a result to be statistically significant at alpha = 0.05, the p-value must be **less than 0.05**.
Reporting in clinical guidelines US Medical PG Question 2: A 25-year-old man with a genetic disorder presents for genetic counseling because he is concerned about the risk that any children he has will have the same disease as himself. Specifically, since childhood he has had difficulty breathing requiring bronchodilators, inhaled corticosteroids, and chest physiotherapy. He has also had diarrhea and malabsorption requiring enzyme replacement therapy. If his wife comes from a population where 1 in 10,000 people are affected by this same disorder, which of the following best represents the likelihood a child would be affected as well?
- A. 0.01%
- B. 2%
- C. 0.5%
- D. 1% (Correct Answer)
- E. 50%
Reporting in clinical guidelines Explanation: ***Correct Option: 1%***
- The patient's symptoms (difficulty breathing requiring bronchodilators, inhaled corticosteroids, and chest physiotherapy; diarrhea and malabsorption requiring enzyme replacement therapy) are classic for **cystic fibrosis (CF)**, an **autosomal recessive disorder**.
- For an autosomal recessive disorder with a prevalence of 1 in 10,000 in the general population, **q² = 1/10,000**, so **q = 1/100 = 0.01**. The carrier frequency **(2pq)** is approximately **2q = 2 × (1/100) = 1/50 = 0.02**.
- The affected man is **homozygous recessive (aa)** and will always pass on the recessive allele. His wife has a **1/50 chance of being a carrier (Aa)**. If she is a carrier, she has a **1/2 chance of passing on the recessive allele**.
- Therefore, the probability of an affected child = **(Probability wife is a carrier) × (Probability wife passes recessive allele) = 1/50 × 1/2 = 1/100 = 1%**.
*Incorrect Option: 0.01%*
- This percentage is too low and does not correctly account for the carrier frequency in the population and the probability of transmission from a carrier mother.
*Incorrect Option: 2%*
- This represents approximately the carrier frequency (1/50 ≈ 2%), but does not account for the additional 1/2 probability that a carrier mother would pass on the recessive allele.
*Incorrect Option: 0.5%*
- This value would be correct if the carrier frequency were 1/100 instead of 1/50, which does not match the given population prevalence.
*Incorrect Option: 50%*
- **50%** would be the risk if both parents were carriers of an autosomal recessive disorder (1/4 chance = 25% for affected, but if we know one parent passes the allele, conditional probability changes). More accurately, 50% would apply if the disorder were **autosomal dominant** with one affected parent, which is not the case here.
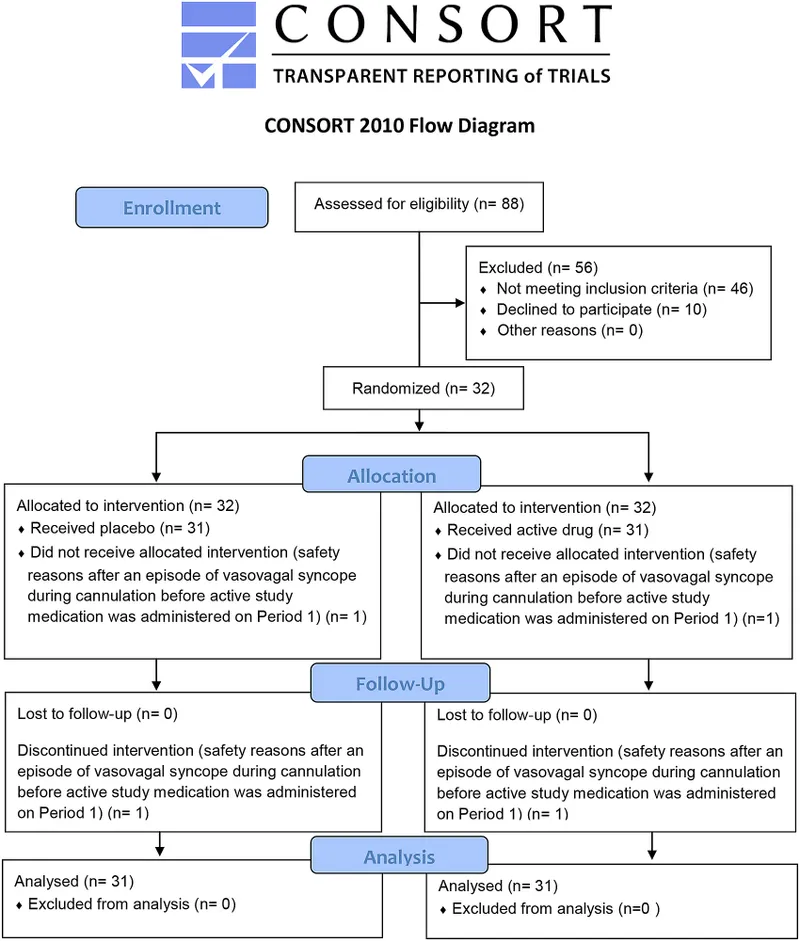
Reporting in clinical guidelines US Medical PG Question 3: A researcher is trying to determine whether a newly discovered substance X can be useful in promoting wound healing after surgery. She conducts this study by enrolling the next 100 patients that will be undergoing this surgery and separating them into 2 groups. She decides which patient will be in which group by using a random number generator. Subsequently, she prepares 1 set of syringes with the novel substance X and 1 set of syringes with a saline control. Both of these sets of syringes are unlabeled and the substances inside cannot be distinguished. She gives the surgeon performing the surgery 1 of the syringes and does not inform him nor the patient which syringe was used. After the study is complete, she analyzes all the data that was collected and performs statistical analysis. This study most likely provides which level of evidence for use of substance X?
- A. Level 3
- B. Level 1 (Correct Answer)
- C. Level 4
- D. Level 5
- E. Level 2
Reporting in clinical guidelines Explanation: ***Level 1***
- The study design described is a **randomized controlled trial (RCT)**, which is considered the **highest level of evidence (Level 1)** in the hierarchy of medical evidence.
- Key features like **randomization**, **control group**, and **blinding (double-blind)** help minimize bias and strengthen the validity of the findings.
*Level 2*
- Level 2 evidence typically comprises **well-designed controlled trials without randomization** (non-randomized controlled trials) or **high-quality cohort studies**.
- While strong, they do not possess the same level of internal validity as randomized controlled trials.
*Level 3*
- Level 3 evidence typically includes **case-control studies** or **cohort studies**, which are observational designs and carry a higher risk of bias compared to RCTs.
- These studies generally do not involve randomization or intervention assignment by the researchers.
*Level 4*
- Level 4 evidence is usually derived from **case series** or **poor quality cohort and case-control studies**.
- These studies provide descriptive information or investigate associations without strong control for confounding factors.
*Level 5*
- Level 5 evidence is the **lowest level of evidence**, consisting of **expert opinion** or **animal research/bench research**.
- This level lacks human clinical data or systematic investigative rigor needed for higher evidence levels.
Reporting in clinical guidelines US Medical PG Question 4: You conduct a medical research study to determine the screening efficacy of a novel serum marker for colon cancer. The study is divided into 2 subsets. In the first, there are 500 patients with colon cancer, of which 450 are found positive for the novel serum marker. In the second arm, there are 500 patients who do not have colon cancer, and only 10 are found positive for the novel serum marker. What is the overall sensitivity of this novel test?
- A. 450 / (450 + 10)
- B. 490 / (10 + 490)
- C. 490 / (50 + 490)
- D. 450 / (450 + 50) (Correct Answer)
- E. 490 / (450 + 490)
Reporting in clinical guidelines Explanation: ***450 / (450 + 50)***
- **Sensitivity** is defined as the proportion of actual positive cases that are correctly identified by the test.
- In this study, there are **500 patients with colon cancer** (actual positives), and **450 of them tested positive** for the marker, while **50 tested negative** (500 - 450 = 50). Therefore, sensitivity = 450 / (450 + 50) = 450/500 = 0.9 or 90%.
*450 / (450 + 10)*
- This formula represents **Positive Predictive Value (PPV)**, which is the probability that a person with a positive test result actually has the disease.
- It incorrectly uses the total number of **test positives** in the denominator (450 true positives + 10 false positives) instead of the total number of diseased individuals, which is needed for sensitivity.
*490 / (10 + 490)*
- This is actually the correct formula for **specificity**, not sensitivity.
- Specificity = TN / (FP + TN) = 490 / (10 + 490) = 490/500 = 0.98 or 98%, which measures the proportion of actual negative cases correctly identified.
- The question asks for sensitivity, not specificity.
*490 / (50 + 490)*
- This formula incorrectly mixes **true negatives (490)** with **false negatives (50)** in an attempt to calculate specificity.
- The correct specificity formula should use false positives (10), not false negatives (50), in the denominator: 490 / (10 + 490).
*490 / (450 + 490)*
- This calculation incorrectly combines **true negatives (490)** and **true positives (450)** in the denominator, which does not correspond to any standard epidemiological measure.
- Neither sensitivity nor specificity uses both true positives and true negatives in the denominator.
Reporting in clinical guidelines US Medical PG Question 5: You are reading through a recent article that reports significant decreases in all-cause mortality for patients with malignant melanoma following treatment with a novel biological infusion. Which of the following choices refers to the probability that a study will find a statistically significant difference when one truly does exist?
- A. Type II error
- B. Type I error
- C. Confidence interval
- D. p-value
- E. Power (Correct Answer)
Reporting in clinical guidelines Explanation: ***Power***
- **Power** is the probability that a study will correctly reject the null hypothesis when it is, in fact, false (i.e., will find a statistically significant difference when one truly exists).
- A study with high power minimizes the risk of a **Type II error** (failing to detect a real effect).
*Type II error*
- A **Type II error** (or **beta error**) occurs when a study fails to reject a false null hypothesis, meaning it concludes there is no significant difference when one actually exists.
- This is the **opposite** of what the question describes, which asks for the probability of *finding* a difference.
*Type I error*
- A **Type I error** (or **alpha error**) occurs when a study incorrectly rejects a true null hypothesis, concluding there is a significant difference when one does not actually exist.
- This relates to the **p-value** and the level of statistical significance (e.g., p < 0.05).
*Confidence interval*
- A **confidence interval** provides a range of values within which the true population parameter is likely to lie with a certain degree of confidence (e.g., 95%).
- It does not directly represent the probability of finding a statistically significant difference when one truly exists.
*p-value*
- The **p-value** is the probability of observing data as extreme as, or more extreme than, that obtained in the study, assuming the null hypothesis is true.
- It is used to determine statistical significance, but it is not the probability of detecting a true effect.
Reporting in clinical guidelines US Medical PG Question 6: A survey was conducted in a US midwestern town in an effort to assess maternal mortality over the past year. The data from the survey are given in the table below:
Women of childbearing age 250,000
Maternal deaths 2,500
Number of live births 100, 000
Number of deaths of women of childbearing age 7,500
Maternal death is defined as the death of a woman while pregnant or within 42 days of termination of pregnancy from any cause related to or aggravated by, the pregnancy. Which of the following is the maternal mortality rate in this midwestern town?
- A. 1,000 per 100,000 live births
- B. 33 per 100,000 live births
- C. 3,000 per 100,000 live births
- D. 33,300 per 100,000 live births
- E. 2,500 per 100,000 live births (Correct Answer)
Reporting in clinical guidelines Explanation: ***2,500 per 100,000 live births***
- The maternal mortality rate is calculated as the number of **maternal deaths** per 100,000 **live births**. The given data directly provide these values.
- Calculation: (2,500 maternal deaths / 100,000 live births) × 100,000 = **2,500 per 100,000 live births**.
*1,000 per 100,000 live births*
- This value is incorrect as it does not align with the provided numbers for maternal deaths and live births in the calculation.
- It might result from a miscalculation or using incorrect numerator/denominator values from the dataset.
*33 per 100,000 live births*
- This value is significantly lower than the correct rate and suggests a substantial error in calculation or an incorrect understanding of how the maternal mortality rate is derived.
- It could potentially result from dividing the number of live births by maternal deaths, which is the inverse of the correct formula.
*3,000 per 100,000 live births*
- This option is close to the correct answer but slightly higher, indicating a possible calculation error, for instance, including non-maternal deaths or other causes of deaths in the numerator.
- The definition of maternal death is specific to pregnancy-related or aggravated causes, so extraneous deaths would inflate the rate.
*33,300 per 100,000 live births*
- This figure results from incorrectly calculating the proportion of maternal deaths among all deaths of women of childbearing age: (2,500 / 7,500) × 100,000 = 33,333.
- This is a conceptual error as the maternal mortality rate should use live births as the denominator, not total deaths of women of childbearing age.
Reporting in clinical guidelines US Medical PG Question 7: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Reporting in clinical guidelines Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Reporting in clinical guidelines US Medical PG Question 8: You are interested in studying the etiology of heart failure reduced ejection fraction (HFrEF) and attempt to construct an appropriate design study. Specifically, you wish to look for potential causality between dietary glucose consumption and HFrEF. Which of the following study designs would allow you to assess for and determine this causality?
- A. Cross-sectional study
- B. Case series
- C. Cohort study (Correct Answer)
- D. Case-control study
- E. Randomized controlled trial
Reporting in clinical guidelines Explanation: ***Cohort study***
- A **cohort study** observes a group of individuals over time to identify risk factors and outcomes, allowing for the assessment of **temporal relationships** between exposure (dietary glucose) and outcome (HFrEF).
- This design is suitable for establishing a potential **causal link** as it tracks participants from exposure to outcome, enabling the calculation of incidence rates and relative risks.
*Cross-sectional study*
- A **cross-sectional study** measures exposure and outcome simultaneously at a single point in time, making it impossible to determine the **temporal sequence** of events.
- This design can only identify **associations** or correlations, not causation, as it cannot establish whether high glucose consumption preceded HFrEF.
*Case series*
- A **case series** describes characteristics of a group of patients with a particular disease or exposure, often to highlight unusual clinical features, but it lacks a **comparison group**.
- It cannot assess causality because it does not provide information on the frequency of exposure in healthy individuals or the incidence of the disease in unexposed individuals.
*Case-control study*
- A **case-control study** compares individuals with the outcome (cases) to those without the outcome (controls) to determine past exposures, which makes it prone to **recall bias**.
- While it can suggest associations, it cannot definitively establish a temporal relationship or causation as the outcome is already known when exposure is assessed.
*Randomized controlled trial*
- A **randomized controlled trial (RCT)** is the gold standard for establishing causation by randomly assigning participants to an intervention or control group, but it may not be ethical or feasible for studying long-term dietary exposures and chronic diseases like HFrEF due to the long follow-up period and complexity of diet.
- While ideal for causality, directly controlling and randomizing dietary glucose intake over decades to observe HFrEF development might be practically challenging or unethical.
Reporting in clinical guidelines US Medical PG Question 9: You are reviewing raw data from a research study performed at your medical center examining the effectiveness of a novel AIDS screening examination. The study enrolled 250 patients with confirmed AIDS, and 240 of these patients demonstrated a positive screening examination. The control arm of the study enrolled 250 patients who do not have AIDS, and only 5 of these patients tested positive on the novel screening examination. What is the NPV of this novel test?
- A. 240 / (240 + 15)
- B. 240 / (240 + 5)
- C. 240 / (240 + 10)
- D. 245 / (245 + 10) (Correct Answer)
- E. 245 / (245 + 5)
Reporting in clinical guidelines Explanation: ***245 / (245 + 10)***
- The **negative predictive value (NPV)** is calculated as **true negatives (TN)** divided by the sum of **true negatives (TN)** and **false negatives (FN)**.
- In this study, there are 250 patients with AIDS; 240 tested positive (true positives, TP), meaning 10 tested negative (false negatives, FN = 250 - 240). There are 250 patients without AIDS; 5 tested positive (false positives, FP), meaning 245 tested negative (true negatives, TN = 250 - 5). Therefore, NPV = 245 / (245 + 10).
*240 / (240 + 15)*
- This calculation incorrectly uses the number of **true positives** (240) in the numerator and denominator, which is relevant for **positive predictive value (PPV)**, not NPV.
- The denominator `(240 + 15)` does not correspond to a valid sum for calculating NPV from the given data.
*240 / (240 + 5)*
- This calculation incorrectly uses **true positives** (240) in the numerator, which is not part of the NPV formula.
- The denominator `(240 + 5)` mixes true positives and false positives, which is incorrect for NPV.
*240 / (240 + 10)*
- This incorrectly places **true positives** (240) in the numerator instead of **true negatives**.
- The denominator `(240+10)` represents **true positives + false negatives**, which is related to sensitivity, not NPV.
*245 / (245 + 5)*
- This calculation correctly identifies **true negatives** (245) in the numerator but incorrectly uses **false positives** (5) in the denominator instead of **false negatives**.
- The denominator for NPV should be **true negatives + false negatives**, which is 245 + 10.
Reporting in clinical guidelines US Medical PG Question 10: A pharmaceutical company reports a new antihypertensive drug reduces cardiovascular events with an NNT of 50 over 5 years based on a trial of 10,000 patients. An independent analysis reveals the benefit was driven entirely by a subgroup with resistant hypertension (20% of participants, NNT=15), while the remaining 80% showed no benefit over standard therapy (NNT approaching infinity). Evaluate the ethical and regulatory implications of reporting the overall NNT.
- A. Conduct a new trial in the general hypertensive population to validate efficacy before broader approval
- B. The subgroup analysis represents data dredging; only the overall NNT should be used for clinical decisions
- C. The overall NNT of 50 is statistically valid and appropriate for regulatory approval and marketing
- D. Report both overall and subgroup NNTs; allow clinicians to determine appropriate use based on patient characteristics
- E. The overall NNT is misleading; approval should be restricted to resistant hypertension population where benefit is demonstrated (Correct Answer)
Reporting in clinical guidelines Explanation: ***The overall NNT is misleading; approval should be restricted to resistant hypertension population where benefit is demonstrated***
- Reporting an **aggregate NNT** when the clinical benefit is confined to a specific **subgroup** obscures the fact that the drug is ineffective for 80% of the study population.
- Regulatory and ethical standards dictate that **indication for use** must be limited to populations where a **favorable benefit-risk ratio** has been proven, preventing unnecessary exposure to side effects in non-responders.
*The overall NNT of 50 is statistically valid and appropriate for regulatory approval and marketing*
- While the math is accurate for the trial population as a whole, it ignores **heterogeneity of treatment effect**, which is critical for making safe **clinical recommendations**.
- Marketing a drug based on an **averaged NNT** when the majority of patients derive zero benefit is considered **clinically misleading** and ethically questionable.
*Report both overall and subgroup NNTs; allow clinicians to determine appropriate use based on patient characteristics*
- This approach puts the burden of identifying the correct population on the clinician rather than setting **clear regulatory boundaries** through specific labelling.
- Merely reporting the **overall NNT** may lead to **off-label use** in populations where the NNT is effectively **infinity**, representing a failure in evidence-based guidance.
*Conduct a new trial in the general hypertensive population to validate efficacy before broader approval*
- The existing data already demonstrates that the **general population** (the 80% non-resistant group) showed no benefit over standard therapy.
- Conducting a new trial for the general population would be **unethical and redundant**, as the lack of efficacy in that specific group has already been established by the **independent analysis**.
*The subgroup analysis represents data dredging; only the overall NNT should be used for clinical decisions*
- **Data dredging** refers to finding random patterns; however, identifying a lack of benefit in 80% of a population is a critical **safety and efficacy finding** that cannot be ignored.
- Dismissing the **subgroup effect** would result in potentially treating millions of patients with an **ineffective medication**, violating the principle of **non-maleficence**.
More Reporting in clinical guidelines US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.