Retrospective cohort design US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Retrospective cohort design. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Retrospective cohort design US Medical PG Question 1: Recently, clarithromycin was found to have an increased risk of cardiac death in a Danish study. This study analyzed patients who were previously treated with clarithromycin or another antibiotic, and then they were followed over time to ascertain if cardiac death resulted. What type of study design does this represent?
- A. Cross-sectional study
- B. Randomized controlled trial
- C. Case control study
- D. Cohort study (Correct Answer)
Retrospective cohort design Explanation: ***Cohort study***
- This study design involves following a group of individuals (a **cohort**) over time to observe the incidence of specific outcomes, in this case, **cardiac death**.
- The study identifies groups based on exposure (clarithromycin treatment vs. another antibiotic) and then tracks them for future events, which is characteristic of a **prospective cohort study**.
*Cross-sectional study*
- A **cross-sectional study** assesses exposure and outcome at a **single point in time**.
- It does not involve following individuals over time, making it unsuitable for studying the temporal relationship between antibiotic use and subsequent cardiac death.
*Randomized controlled trial*
- A **randomized controlled trial (RCT)** involves randomly assigning participants to an intervention or control group to determine the effect of the intervention.
- This study did not involve random assignment of clarithromycin but rather observed groups based on **prior treatment**, ruling out an RCT.
*Case control study*
- A **case-control study** starts with individuals who have the outcome (cases) and individuals who do not (controls) and then retrospectively looks back at their exposures.
- This study started with exposed individuals (treated with clarithromycin) and then followed them forward, which is the opposite direction of a case-control study.
Retrospective cohort design US Medical PG Question 2: A study is funded by the tobacco industry to examine the association between smoking and lung cancer. They design a study with a prospective cohort of 1,000 smokers between the ages of 20-30. The length of the study is five years. After the study period ends, they conclude that there is no relationship between smoking and lung cancer. Which of the following study features is the most likely reason for the failure of the study to note an association between tobacco use and cancer?
- A. Late-look bias
- B. Latency period (Correct Answer)
- C. Confounding
- D. Effect modification
- E. Pygmalion effect
Retrospective cohort design Explanation: ***Latency period***
- **Lung cancer** typically has a **long latency period**, often **20-30+ years**, between initial exposure to tobacco carcinogens and the development of clinically detectable disease.
- A **five-year study duration** in young smokers (ages 20-30) is **far too short** to observe the development of lung cancer, which explains the false negative finding.
- This represents a **fundamental flaw in study design** rather than a bias—the biological timeline of disease development was not adequately considered.
*Late-look bias*
- **Late-look bias** occurs when a study enrolls participants who have already survived the early high-risk period of a disease, leading to **underestimation of true mortality or incidence**.
- Also called **survival bias**, it involves studying a population that has already been "selected" by survival.
- This is not applicable here, as the study simply ended before sufficient time elapsed for disease to develop.
*Confounding*
- **Confounding** occurs when a third variable is associated with both the exposure and outcome, distorting the apparent relationship between them.
- While confounding can affect study results, it would not completely eliminate the detection of a strong, well-established association like smoking and lung cancer in a properly conducted prospective cohort study.
- The issue here is temporal (insufficient follow-up time), not the presence of an unmeasured confounder.
*Effect modification*
- **Effect modification** (also called interaction) occurs when the magnitude of an association between exposure and outcome differs across levels of a third variable.
- This represents a **true biological phenomenon**, not a study design flaw or bias.
- It would not explain the complete failure to detect any association.
*Pygmalion effect*
- The **Pygmalion effect** (observer-expectancy effect) refers to a psychological phenomenon where higher expectations lead to improved performance in the observed subjects.
- This concept is relevant to **behavioral and educational research**, not to objective epidemiological studies of disease incidence.
- It has no relevance to the biological relationship between carcinogen exposure and cancer development.
Retrospective cohort design US Medical PG Question 3: A recent study attempted to analyze whether increased "patient satisfaction" driven healthcare resulted in increased hospitalization. Using this patient population, the sociodemographics, health status, and hospital use were assessed. Next year, patient satisfaction with health care providers was assessed using 5 items from the Consumer Assessment of Health Plans Survey. Which of the following best describes this study design?
- A. Retrospective case-control
- B. Cross-sectional study
- C. Prospective case-control
- D. Retrospective cohort
- E. Prospective cohort (Correct Answer)
Retrospective cohort design Explanation: ***Prospective cohort***
- This study collects baseline data (sociodemographics, health status, hospital use) on a patient population and then follows them forward in time to assess patient satisfaction the following year. This forward-looking approach with follow-up over time defines a **prospective cohort study**.
- The study establishes a cohort at baseline, measures initial characteristics and hospital use, then prospectively assesses patient satisfaction and subsequent healthcare utilization, allowing analysis of associations between satisfaction and hospitalization patterns.
*Retrospective case-control*
- A **case-control study** identifies individuals with an outcome (cases) and without the outcome (controls) and then looks backward in time to determine past exposures.
- This study does not select participants based on outcome status; instead, it defines a cohort and follows them forward, which is characteristic of cohort design, not case-control.
*Cross-sectional study*
- A **cross-sectional study** measures both exposure and outcome at a single point in time, providing a snapshot of the population.
- This study involves follow-up over time, as patient satisfaction is assessed "next year" after baseline data collection, making it longitudinal rather than cross-sectional.
*Prospective case-control*
- **Case-control studies** inherently select participants based on their outcome status (cases vs. controls), whether prospective or retrospective.
- This study starts with a defined patient population before outcomes occur and follows them forward without outcome-based selection, which is characteristic of a cohort study, not a case-control design.
*Retrospective cohort*
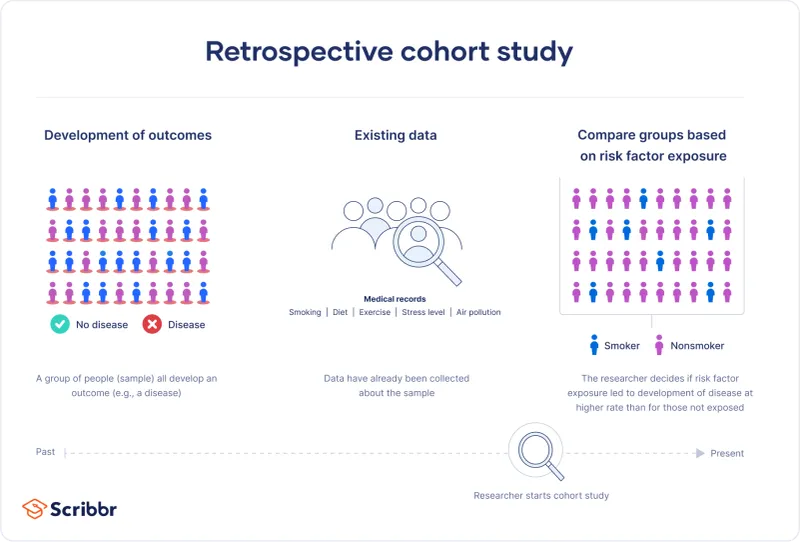
- A **retrospective cohort study** uses existing data to define a cohort and then looks back in time to identify exposures and outcomes that have already occurred.
- This study involves collecting new data prospectively and following participants forward ("next year"), rather than analyzing past records, making it prospective rather than retrospective.
Retrospective cohort design US Medical PG Question 4: A researcher is trying to determine whether a newly discovered substance X can be useful in promoting wound healing after surgery. She conducts this study by enrolling the next 100 patients that will be undergoing this surgery and separating them into 2 groups. She decides which patient will be in which group by using a random number generator. Subsequently, she prepares 1 set of syringes with the novel substance X and 1 set of syringes with a saline control. Both of these sets of syringes are unlabeled and the substances inside cannot be distinguished. She gives the surgeon performing the surgery 1 of the syringes and does not inform him nor the patient which syringe was used. After the study is complete, she analyzes all the data that was collected and performs statistical analysis. This study most likely provides which level of evidence for use of substance X?
- A. Level 3
- B. Level 1 (Correct Answer)
- C. Level 4
- D. Level 5
- E. Level 2
Retrospective cohort design Explanation: ***Level 1***
- The study design described is a **randomized controlled trial (RCT)**, which is considered the **highest level of evidence (Level 1)** in the hierarchy of medical evidence.
- Key features like **randomization**, **control group**, and **blinding (double-blind)** help minimize bias and strengthen the validity of the findings.
*Level 2*
- Level 2 evidence typically comprises **well-designed controlled trials without randomization** (non-randomized controlled trials) or **high-quality cohort studies**.
- While strong, they do not possess the same level of internal validity as randomized controlled trials.
*Level 3*
- Level 3 evidence typically includes **case-control studies** or **cohort studies**, which are observational designs and carry a higher risk of bias compared to RCTs.
- These studies generally do not involve randomization or intervention assignment by the researchers.
*Level 4*
- Level 4 evidence is usually derived from **case series** or **poor quality cohort and case-control studies**.
- These studies provide descriptive information or investigate associations without strong control for confounding factors.
*Level 5*
- Level 5 evidence is the **lowest level of evidence**, consisting of **expert opinion** or **animal research/bench research**.
- This level lacks human clinical data or systematic investigative rigor needed for higher evidence levels.
Retrospective cohort design US Medical PG Question 5: A 15-year-old female presents to her family physician for an annual school physical exam and check-up. She is accompanied by her mother to the visit and is present in the exam room. The patient has no complaints, and she does not have any past medical problems. She takes no medications. The patient reports that she remains active, exercising 5 times a week, and eats a healthy and varied diet. Which of the following would be the best way for the physician to obtain a more in-depth social history, including sexual history and use of alcohol, tobacco, or recreational drugs?
- A. Disallow the mother to be present in the examination room throughout the entirety of the visit
- B. Give the patient a social history questionnaire to fill out in the exam room
- C. Ask the mother to step outside into the hall for a portion of the visit (Correct Answer)
- D. Ask the patient the questions directly, with her mother still in the exam room
- E. Speak softly to the patient so that the mother does not hear and the patient is not embarrassed
Retrospective cohort design Explanation: ***Ask the mother to step outside into the hall for a portion of the visit***
- This approach allows the physician to speak with the adolescent **privately and confidentially**, which is crucial for obtaining sensitive information such as sexual history, drug use, and mental health concerns.
- Adolescents are more likely to disclose personal information when their parents are not present, fostering trust and ensuring **comprehensive history-taking** vital for their well-being.
*Disallow the mother to be present in the examination room throughout the entirety of the visit*
- This is an **overly restrictive** approach that might create tension or distrust between the physician, patient, and parent, especially at the start of the visit.
- While privacy is essential for sensitive topics, parental presence can be valuable for discussing general health, family history, and **treatment plans**, especially for younger adolescents.
*Give the patient a social history questionnaire to fill out in the exam room*
- While questionnaires can be useful for gathering basic information, they often **lack the nuance** of a direct conversation and may not prompt the patient to elaborate on sensitive issues.
- Furthermore, having the mother present while the patient fills out a questionnaire on sensitive topics still **compromises confidentiality** and may lead to incomplete or dishonest answers.
*Ask the patient the questions directly, with her mother still in the exam room*
- Asking sensitive questions with a parent present is **unlikely to yield truthful and complete answers**, as adolescents may feel embarrassed, judged, or fear parental disapproval.
- This approach compromises the **confidentiality** that is fundamental to building trust with adolescent patients.
*Speak softly to the patient so that the mother does not hear and the patient is not embarrassed*
- Speaking softly is **unprofessional** and still does not guarantee privacy, as the mother might still overhear parts of the conversation.
- This method also **fails to establish true confidentiality**, which is central to building rapport and encouraging open communication with adolescent patients about sensitive topics.
Retrospective cohort design US Medical PG Question 6: Study X examined the relationship between coffee consumption and lung cancer. The authors of Study X retrospectively reviewed patients' reported coffee consumption and found that drinking greater than 6 cups of coffee per day was associated with an increased risk of developing lung cancer. However, Study X was criticized by the authors of Study Y. Study Y showed that increased coffee consumption was associated with smoking. What type of bias affected Study X, and what study design is geared to reduce the chance of that bias?
- A. Observer bias; double blind analysis
- B. Selection bias; randomization
- C. Lead time bias; placebo
- D. Measurement bias; blinding
- E. Confounding; randomization (Correct Answer)
Retrospective cohort design Explanation: ***Confounding; randomization***
- Study Y suggests that **smoking** is a **confounding variable** because it is associated with both increased coffee consumption (exposure) and increased risk of lung cancer (outcome), distorting the apparent relationship between coffee and lung cancer.
- **Randomization** in experimental studies (such as randomized controlled trials) helps reduce confounding by ensuring that known and unknown confounding factors are evenly distributed among study groups.
- In observational studies where randomization is not possible, confounding can be addressed through **stratification**, **matching**, or **multivariable adjustment** during analysis.
*Observer bias; double blind analysis*
- **Observer bias** occurs when researchers' beliefs or expectations influence the study outcome, which is not the primary issue described here regarding the relationship between coffee, smoking, and lung cancer.
- **Double-blind analysis** is a method to mitigate observer bias by ensuring neither participants nor researchers know who is in the control or experimental groups.
*Selection bias; randomization*
- **Selection bias** happens when the study population is not representative of the target population, leading to inaccurate results, which is not directly indicated by the interaction between coffee and smoking.
- While **randomization** is used to reduce selection bias by creating comparable groups, the core problem identified in Study X is confounding, not flawed participant selection.
*Lead time bias; placebo*
- **Lead time bias** occurs in screening programs when early detection without improved outcomes makes survival appear longer, an issue unrelated to the described association between coffee, smoking, and lung cancer.
- A **placebo** is an inactive treatment used in clinical trials to control for psychological effects, and its relevance here is limited to treatment intervention studies.
*Measurement bias; blinding*
- **Measurement bias** arises from systematic errors in data collection, such as inaccurate patient reporting of coffee consumption, but the main criticism from Study Y points to a third variable (smoking) affecting the association, not just flawed measurement.
- **Blinding** helps reduce measurement bias by preventing participants or researchers from knowing group assignments, thus minimizing conscious or unconscious influences on data collection.
Retrospective cohort design US Medical PG Question 7: A scientist is designing a study to determine whether eating a new diet is able to lower blood pressure in a group of patients. In particular, he believes that starting the diet may help decrease peak blood pressures throughout the day. Therefore, he will equip study participants with blood pressure monitors and follow pressure trends over a 24-hour period. He decides that after recruiting subjects, he will start them on either the new diet or a control diet and follow them for 1 month. After this time, he will switch patients onto the other diet and follow them for an additional month. He will analyze the results from the first month against the results from the second month for each patient. This type of study design is best at controlling for which of the following problems with studies?
- A. Hawthorne effect
- B. Recall bias
- C. Confounding (Correct Answer)
- D. Selection bias
- E. Pygmalion effect
Retrospective cohort design Explanation: ***Confounding***
- This **crossover design** (switching patients to the other diet) effectively controls for **confounding variables** by making each patient their own control, ensuring that inherent patient characteristics do not bias the comparison between diets.
- By comparing the effects of both diets within the same individual, individual variability in factors such as genetics, lifestyle, and other co-morbidities are accounted for, reducing their potential as confounders.
*Hawthorne effect*
- The **Hawthorne effect** refers to subjects modifying their behavior in response to being observed, which this study design does not specifically address or eliminate.
- While patients are being monitored, the design aims to compare the diets' effects, not to prevent behavioral changes due to observation itself.
*Recall bias*
- **Recall bias** occurs when participants' memories of past events are inaccurate, often influenced by their current health status or beliefs.
- This study measures **real-time blood pressure** data, not relying on recollection of past exposures or outcomes, thereby mitigating recall bias.
*Selection bias*
- **Selection bias** arises from non-random selection of participants into study groups, leading to systematic differences between groups.
- While patient recruitment could introduce selection bias into the overall study population, the **crossover design** itself helps control for differences between treatment arms because all participants eventually receive both treatments.
*Pygmalion effect*
- The **Pygmalion effect** (or observer-expectancy effect) describes phenomena where higher expectations lead to increased performance, usually from a researcher influencing a subject.
- This effect is not directly addressed by the crossover design; the design focuses on controlling for patient-specific confounders rather than investigator bias in expectations.
Retrospective cohort design US Medical PG Question 8: In recent years, psoriasis has been identified as a risk factor for cardiovascular disease. A researcher conducted a study in which he identified 200 patients with psoriasis and 200 patients without psoriasis. The patients were followed for 10 years. At the end of this period, participants' charts were reviewed for myocardial infarction during this time interval.
Myocardial infarction No myocardial infarction Total
Psoriasis 12 188 200
No psoriasis 4 196 200
Total 16 384 400
What is the 10-year risk of myocardial infarction in participants with psoriasis?
- A. 0.75
- B. 0.04
- C. 0.5
- D. 0.06 (Correct Answer)
- E. 0.02
Retrospective cohort design Explanation: ***0.06***
- The **risk of myocardial infarction** in participants with psoriasis is calculated by dividing the number of psoriasis patients who had a myocardial infarction by the total number of psoriasis patients.
- This calculation is 12 (myocardial infarctions in psoriasis group) / 200 (total psoriasis patients) = **0.06 or 6%**.
- This represents the **cumulative incidence** or **absolute risk** in the exposed cohort over 10 years.
*0.75*
- This value represents the **proportion of all MI cases that occurred in the psoriasis group**: 12/16 = 0.75.
- This is not the same as risk, which requires the denominator to be the total at-risk population (all psoriasis patients), not just those with the outcome.
*0.04*
- This value represents the **risk of myocardial infarction in the control group** (no psoriasis): 4/200 = 0.02, not 0.04.
- However, 0.04 could represent 2 × 0.02, which has no meaningful epidemiological interpretation for this study.
*0.5*
- This value does not correspond to any standard epidemiological measure from the given data.
- It might represent a miscalculation or confusion with other statistical concepts.
*0.02*
- This value represents the **risk of myocardial infarction in the unexposed group** (no psoriasis): 4/200 = 0.02 or 2%.
- The question specifically asks for the risk in the psoriasis group, not the control group.
Retrospective cohort design US Medical PG Question 9: A population is studied for risk factors associated with testicular cancer. Alcohol exposure, smoking, dietary factors, social support, and environmental exposure are all assessed. The researchers are interested in the incidence and prevalence of the disease in addition to other outcomes. Which pair of studies would best assess the 1. incidence and 2. prevalence?
- A. 1. Prospective cohort study 2. Cross sectional study (Correct Answer)
- B. 1. Prospective cohort study 2. Retrospective cohort study
- C. 1. Cross sectional study 2. Retrospective cohort study
- D. 1. Case-control study 2. Prospective cohort study
- E. 1. Clinical trial 2. Cross sectional study
Retrospective cohort design Explanation: ***1. Prospective cohort study 2. Cross sectional study***
- A **prospective cohort study** is ideal for measuring **incidence** (new cases over time) because it follows a group of individuals forward in time to observe who develops the disease.
- A **cross-sectional study** is suitable for measuring **prevalence** (existing cases at a specific point in time) as it surveys a population at one moment to determine the proportion with the disease.
*1. Prospective cohort study 2. Retrospective cohort study*
- A **retrospective cohort study** assesses past exposures and outcomes and can measure incidence, but it is not the primary choice for prevalence.
- While a prospective cohort study is appropriate for incidence, a retrospective cohort study is less suited for determining current prevalence.
*1. Cross sectional study 2. Retrospective cohort study*
- A **cross-sectional study** measures prevalence, not incidence, as it captures disease status at a single point in time.
- A **retrospective cohort study** looks back in time to identify past exposures and subsequent outcomes, which is not the best method for current prevalence.
*1. Case-control study 2. Prospective cohort study*
- A **case-control study** compares exposures between individuals with a disease (cases) and those without (controls) and is best for studying rare diseases and estimating odds ratios, not incidence or prevalence directly.
- A **prospective cohort study** is suitable for incidence, but a case-control study is not for incidence or prevalence.
*1. Clinical trial 2. Cross sectional study*
- A **clinical trial** is an experimental study designed to test the efficacy of interventions and is not primarily used to measure disease incidence or prevalence in a general population.
- While a cross-sectional study is appropriate for prevalence, a clinical trial is not designed for incidence measurement.
Retrospective cohort design US Medical PG Question 10: A researcher wants to determine whether there is an association between CRP values and the risk of MI or cancer. Four relative risk (RR) values were plotted $(0.5,1.5,1.7,1.8)$ with respect to CRP levels. What conclusion can be drawn?
- A. CRP has no relationship
- B. CRP decreases & disease decreases
- C. CRP increases disease/cancer risk (Correct Answer)
- D. No association in first interval
- E. CRP shows protective effect in first interval
Retrospective cohort design Explanation: ***CRP increases disease/cancer risk***
- A **relative risk (RR)** greater than 1 indicates an increased risk of the outcome (MI or cancer) in the exposed group (higher CRP levels) compared to the unexposed group.
- The plots show RRs of 1.5, 1.7, and 1.8, all of which are greater than 1, consistently indicating that higher CRP levels are associated with an elevated risk for MI or cancer.
- The overall trend across the four intervals demonstrates a positive association between CRP and disease risk.
*CRP has no relationship*
- This conclusion is incorrect because three of the four plotted RR values (1.5, 1.7, 1.8) are above 1, indicating a positive association or increased risk.
- An RR of 1 signifies no relationship, but the majority of values clearly deviate from 1, showing a definite association.
*CRP decreases & disease decreases*
- While one RR value (0.5) suggests a decreased risk, the majority of the given RRs (1.5, 1.7, 1.8) are greater than 1, indicating an increased risk.
- This option would only be true if all or most RR values were less than 1, implying a protective effect, which is not the overall trend here.
*No association in first interval*
- The first interval shows an RR of 0.5. An RR of 1 indicates no association, while an RR of 0.5 actually indicates a **decreased risk or protective effect**, rather than no association.
- Therefore, stating "no association" for the first interval is inaccurate given the definition of relative risk.
*CRP shows protective effect in first interval*
- While the first interval RR of 0.5 does suggest a protective effect in isolation, this option fails to capture the **overall conclusion** from all four data points.
- When interpreting multiple RR values together, the predominant pattern (three values >1) indicates an overall increased risk, making this a misleading conclusion for the study as a whole.
More Retrospective cohort design US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.