Vitamin cofactor functions in metabolism US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Vitamin cofactor functions in metabolism. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Vitamin cofactor functions in metabolism US Medical PG Question 1: A 68-year-old man with type 2 diabetes mellitus comes to the physician because of a 5-month history of episodic palpitations, dizziness, and fatigue. His pulse is 134/min and irregularly irregular, and his blood pressure is 165/92 mm Hg. An ECG shows a narrow complex tachycardia with absent P waves. He is prescribed a drug that decreases the long-term risk of thromboembolic complications by inhibiting the extrinsic pathway of the coagulation cascade. The expected beneficial effect of this drug is most likely due to which of the following actions?
- A. Inhibit the reduction of vitamin K (Correct Answer)
- B. Activate gamma-glutamyl carboxylase
- C. Inhibit the phosphorylation of glutamate on the factor II precursor
- D. Activate factor VII calcium-binding sites
- E. Inhibit the absorption of vitamin K
Vitamin cofactor functions in metabolism Explanation: ***Inhibit the reduction of vitamin K***
- The patient's symptoms and ECG findings (irregularly irregular pulse, absent P waves, narrow complex tachycardia) are consistent with **atrial fibrillation**, which carries a high risk of **thromboembolic complications**.
- The drug described, acting on the **extrinsic pathway** and reducing thromboembolic risk, is most likely **warfarin**, a **vitamin K antagonist** that inhibits the reduction (regeneration) of vitamin K, thus impairing the synthesis of coagulation factors II, VII, IX, and X.
*Activate gamma-glutamyl carboxylase*
- **Gamma-glutamyl carboxylase** is an enzyme that requires reduced vitamin K as a cofactor.
- Warfarin's action is to **inhibit** the enzyme that *reduces* vitamin K, thereby *reducing* the activity of gamma-glutamyl carboxylase, not activating it.
*Inhibit the phosphorylation of glutamate on the factor II precursor*
- The modification of glutamate residues on coagulation factors is through **gamma-carboxylation**, not phosphorylation.
- Warfarin inhibits the **gamma-carboxylation** of factors II, VII, IX, and X, not their phosphorylation.
*Activate factor VII calcium-binding sites*
- Factor VII, like other vitamin K-dependent factors, requires **gamma-carboxylation** for calcium binding, which is essential for its activation and function.
- Warfarin **inhibits** this carboxylation, thereby impairing calcium binding and the activation of these factors, rather than activating their calcium-binding sites.
*Inhibit the absorption of vitamin K*
- While vitamin K absorption can be affected by certain conditions or drugs (e.g., malabsorption syndromes, broad-spectrum antibiotics), warfarin's primary mechanism of action is **post-absorption**, targeting the **epoxide reductase enzyme** involved in vitamin K recycling, not its intestinal absorption.
Vitamin cofactor functions in metabolism US Medical PG Question 2: An investigator is studying nutritional deficiencies in humans. A group of healthy volunteers are started on a diet deficient in pantothenic acid. After 4 weeks, several of the volunteers develop irritability, abdominal cramps, and burning paresthesias of their feet. These symptoms are fully reversed after reintroduction of pantothenic acid to their diet. The function of which of the following enzymes was most likely impaired in the volunteers during the study?
- A. Gamma-glutamyl carboxylase
- B. Alpha-ketoglutarate dehydrogenase (Correct Answer)
- C. Dopamine beta-hydroxylase
- D. Methionine synthase
- E. Glutathione reductase
Vitamin cofactor functions in metabolism Explanation: ***Alpha-ketoglutarate dehydrogenase***
- **Pantothenic acid** (vitamin B5) is a precursor of **coenzyme A (CoA)**, which is essential for the function of alpha-ketoglutarate dehydrogenase in the **Krebs cycle**.
- Impairment of this enzyme, critical for energy production, can lead to widespread metabolic dysfunction, manifesting as neurological and gastrointestinal symptoms like **irritability, abdominal cramps**, and **burning paresthesias**, which are classic signs of pantothenic acid deficiency.
*Gamma-glutamyl carboxylase*
- This enzyme is involved in the post-translational modification of several proteins, including **clotting factors**, and requires **vitamin K** as a cofactor.
- Its deficiency leads to bleeding disorders, not the neurological and GI symptoms described.
*Dopamine beta-hydroxylase*
- This enzyme converts **dopamine to norepinephrine** and requires vitamin C and copper.
- Its impairment can affect neurotransmitter synthesis but is not directly linked to pantothenic acid deficiency.
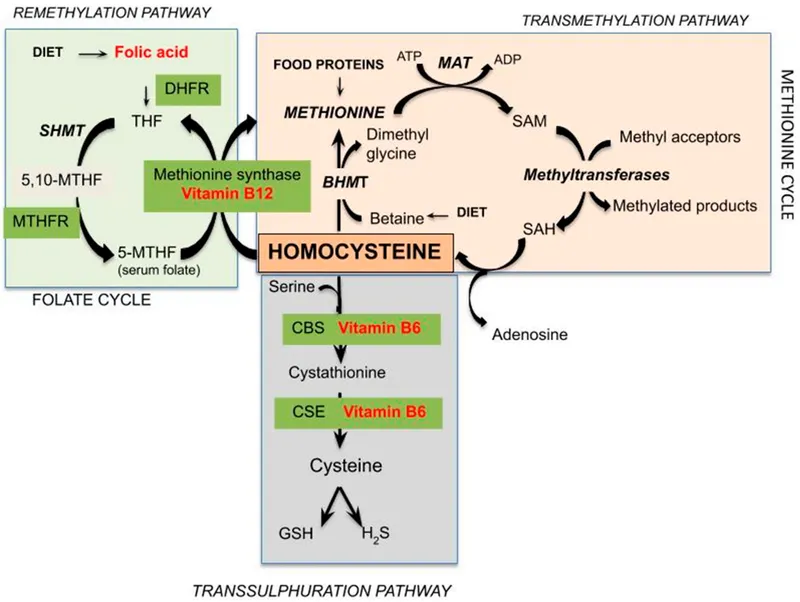
*Methionine synthase*
- This enzyme is crucial for the metabolism of **homocysteine** and requires **vitamin B12** and **folate** as cofactors.
- Its deficiency is associated with megaloblastic anemia and neurological symptoms, but not the specific presentation seen with pantothenic acid deficiency.
*Glutathione reductase*
- This enzyme is essential for maintaining the reduced state of **glutathione**, an antioxidant, and requires **riboflavin** (vitamin B2) in its coenzyme form, FAD.
- Dysfunction typically leads to oxidative stress, hemolytic anemia, and other symptoms different from those described.
Vitamin cofactor functions in metabolism US Medical PG Question 3: A 43-year-old woman visits her primary care provider complaining of fatigue. Although she has had it for several months, her fatigue has been worsening over the past few weeks. She has no other symptoms. Past medical history is significant for hypertension. She takes chlorthalidone, an oral contraceptive pill, and a multivitamin every day. Family history is noncontributory. She drinks about 1 bottle of wine every day and started taking a shot or two of whisky or vodka every morning before work to “clear out the cobwebs”. She was recently fired from her job. Today, her heart rate is 90/min, respiratory rate is 17/min, blood pressure is 110/65 mm Hg, and temperature is 36.7°C (98.1°F). On physical exam, she appears malnourished and anxious. Her conjunctiva are pale, and glossitis is noted on oral exam. Her heart has a regular rate and rhythm and her lungs are clear to auscultation bilaterally. She has no gait or balance abnormalities. Lab results show a hemoglobin of 10 g/dL, with a mean corpuscular volume (MCV) of 108 fl. Elevated level of which of the following will most likely to be found in this patient?
- A. Methionine
- B. Phenylalanine
- C. Cysteine
- D. Homocysteine
- E. Methylmalonic acid (Correct Answer)
Vitamin cofactor functions in metabolism Explanation: ***Methylmalonic acid***
- The patient's presentation with **macrocytic anemia** (MCV 108 fl, Hb 10 g/dL), **glossitis**, and **fatigue** suggests a **vitamin B12 deficiency**.
- **Elevated methylmalonic acid (MMA)** is a sensitive and specific marker for **vitamin B12 deficiency**, as **B12** acts as a cofactor for the enzyme **methylmalonyl-CoA mutase**, which converts MMA to succinyl-CoA.
*Methionine*
- **Methionine** is an essential amino acid, and its levels are not directly elevated in **vitamin B12 deficiency**; rather, **B12** is involved in the conversion of **homocysteine to methionine**.
- In **B12 deficiency**, the conversion of **homocysteine to methionine** is impaired, leading to **elevated homocysteine**, not necessarily methionine.
*Phenylalanine*
- **Phenylalanine** is an essential amino acid whose metabolism is primarily linked to **phenylketonuria (PKU)** if its levels are elevated due to deficient **phenylalanine hydroxylase**, which is unrelated to **vitamin B12 deficiency**.
- Elevated phenylalanine would not be an expected finding in this patient's clinical scenario.
*Cysteine*
- **Cysteine** is a non-essential amino acid, and its levels are not typically elevated as a direct consequence or marker of **vitamin B12 deficiency**.
- While involved in various metabolic pathways, it doesn't serve as a diagnostic indicator for B12 status.
*Homocysteine*
- While **homocysteine levels are elevated in vitamin B12 deficiency**, as B12 is a cofactor for **methionine synthase**, which converts homocysteine to methionine, **methylmalonic acid** is a more specific marker for **B12 deficiency**.
- **Elevated homocysteine** can also be caused by **folate deficiency** or **vitamin B6 deficiency**, making it less specific than **MMA** for isolating B12 deficiency.
Vitamin cofactor functions in metabolism US Medical PG Question 4: A 51-year-old gentleman presents with new onset bilateral paresthesias of his feet. He also admits that he has not been able to exercise as much as previously and his friends have commented that he looks pale. Upon physical exam you find that he has conjunctival pallor and mildly decreased sensation and proprioception on his feet bilaterally. Based on your suspicions you decide to obtain a blood smear where you see megaloblasts as well as hypersegmented neutrophils. Given these findings you decide to investigate the cause of his disorder by injecting an intramuscular vitamin, then feeding him a radiolabeled version of the same vitamin orally. After waiting 24 hours you see that no radiolabeled vitamin appears in the urine so you repeat the test with intrinsic factor added to the oral mixture, at which point 20% of the radiolabeled vitamin appears in the urine. Which of the following is the most likely etiology of this gentleman's symptoms?
- A. Bacterial overgrowth
- B. Pancreatic insufficiency
- C. Insufficient vitamin intake
- D. Pernicious anemia (Correct Answer)
- E. Folate deficiency
Vitamin cofactor functions in metabolism Explanation: ***Pernicious anemia***
- The combination of **neurological symptoms** (paresthesias, decreased proprioception), **anemia symptoms** (pallor, fatigue), **megaloblastic anemia** on blood smear (megaloblasts, hypersegmented neutrophils), and the specific Schilling test results (vitamin B12 malabsorption corrected by added **intrinsic factor**) is diagnostic for pernicious anemia.
- Pernicious anemia is an autoimmune condition targeting **gastric parietal cells** or **intrinsic factor** itself, leading to **vitamin B12 deficiency** due to impaired absorption.
*Bacterial overgrowth*
- **Bacterial overgrowth in the small intestine** can consume vitamin B12, leading to deficiency, but the Schilling test would show improvement with **antibiotics**, not intrinsic factor.
- While it can cause B12 deficiency and megaloblastic anemia, improvement upon adding intrinsic factor points away from this diagnosis.
*Pancreatic insufficiency*
- **Pancreatic enzymes** are required to cleave vitamin B12 from its binding proteins, but the **Schilling test** would show improvement with **pancreatic enzyme supplements**, not intrinsic factor.
- While pancreatic insufficiency can lead to B12 malabsorption, the specific Schillings test results rule it out.
*Insufficient vitamin intake*
- **Insufficient dietary intake** of vitamin B12 would lead to B12 deficiency, but in such a case, the **Schilling test** would show normal absorption of radiolabeled B12 even without intrinsic factor in the second stage.
- The initial B12 malabsorption indicates an absorption problem, not solely a dietary lack.
*Folate deficiency*
- **Folate deficiency** also causes **megaloblastic anemia** and can present with fatigue and pallor, but it does **not cause neurological symptoms** like paresthesias or proprioception deficits.
- The Schilling test specifically evaluates **vitamin B12 absorption**, not folate levels, so it would be irrelevant for diagnosing pure folate deficiency.
Vitamin cofactor functions in metabolism US Medical PG Question 5: A 2-week-old boy is brought to the emergency department after he was found to have blood in his stool. The mother says the baby was born by home birth at 38 weeks without complications. The mother denies fever, vomiting, or rash but says the baby has been fussier recently. The mother denies a family history of any similar problems. On exam, the patient is well-developed and meets all developmental markers. His heart rate is tachycardic but with regular rhythms. There is oozing blood from the umbilical site which has not fully healed. A guaiac stool test is positive. What is the underlying cause of this presentation?
- A. Factor VIII deficiency
- B. Bacterial infection
- C. Vitamin B12 deficiency
- D. Vitamin K deficiency (Correct Answer)
- E. Factor IX deficiency
Vitamin cofactor functions in metabolism Explanation: ***Vitamin K deficiency***
- The bleeding in a 2-week-old infant, specifically gastrointestinal bleeding (blood in stool) and umbilical oozing, is highly suspicious for **Vitamin K deficiency bleeding (VKDB)**, particularly given the home birth setting where prophylactic vitamin K administration may have been missed.
- The mother's denial of fever, vomiting, or rash, and the absence of a family history of bleeding disorders, makes other conditions less likely, while the isolated bleeding signs point strongly to a **coagulation factor deficiency** related to vitamin K.
*Factor VIII deficiency*
- **Hemophilia A (Factor VIII deficiency)** typically presents with spontaneous bleeding into joints and muscles, or prolonged bleeding after trauma/surgery.
- While it can manifest in neonates (e.g., intracranial hemorrhage), it's less commonly associated with **umbilical stump bleeding** or **gastrointestinal bleeding** as the primary presentation in this early neonatal period compared to VKDB, and there is no family history of a similar problem.
*Bacterial infection*
- A bacterial infection causing gastrointestinal bleeding would likely present with other systemic symptoms such as **fever, vomiting, lethargy**, or signs of sepsis, which are explicitly denied by the mother.
- Although some severe infections can cause disseminated intravascular coagulation (DIC) and bleeding, isolated bleeding without other signs of infection makes this less probable.
*Vitamin B12 deficiency*
- Vitamin B12 deficiency is primarily associated with **megaloblastic anemia** and **neurological symptoms**, not acute bleeding.
- It is not a direct cause of coagulation factor deficiencies resulting in acute bleeding in neonates.
*Factor IX deficiency*
- **Hemophilia B (Factor IX deficiency)**, like Hemophilia A, presents similarly with joint and muscle hematomas or prolonged bleeding, and usually has a family history of X-linked bleeding.
- The absence of a family history and the specific constellation of gastrointestinal and umbilical bleeding make **VKDB** a more direct fit, as Factor IX is also a vitamin K-dependent clotting factor, but the overall clinical picture without a family history points more broadly to VKDB due to lack of prophylaxis.
Vitamin cofactor functions in metabolism US Medical PG Question 6: A 29-year-old Mediterranean man presents to the clinic for fatigue and lightheadedness for the past week. He reports an inability to exercise as his heart would beat extremely fast. He was recently diagnosed with active tuberculosis and started on treatment 2 weeks ago. He denies fever, weight loss, vision changes, chest pain, dyspnea, or bloody/dark stools. A physical examination is unremarkable. A peripheral blood smear is shown in figure A. What is the most likely explanation for this patient’s symptoms?
- A. Hereditary mutations of beta-globin
- B. Inhibition of ferrochelatase and ALA dehydratase
- C. Abnormally low level of glutathione activity
- D. Drug-induced deficiency in vitamin B6 (Correct Answer)
- E. Iron deficiency
Vitamin cofactor functions in metabolism Explanation: ***Drug-induced deficiency in vitamin B6***
- The patient's symptoms of **fatigue** and **lightheadedness**, along with the peripheral blood smear showing **sideroblasts** (ringed forms, indicated by the accumulation of iron in mitochondria around the nucleus of immature red blood cells) suggest **sideroblastic anemia**.
- The patient was recently started on treatment for **tuberculosis**, which commonly includes **isoniazid**. Isoniazid is known to **inhibit vitamin B6 (pyridoxine)**, leading to **sideroblastic anemia**.
- While the patient's **Mediterranean ethnicity** raises consideration for G6PD deficiency (another potential complication of TB treatment), the **presence of sideroblasts** on smear is diagnostic for sideroblastic anemia, not hemolytic anemia.
*Hereditary mutations of beta-globin*
- Hereditary mutations in beta-globin are characteristic of **beta-thalassemia**, which typically presents in childhood and is associated with significant **hemolysis** and **microcytic, hypochromic anemia**, usually without sideroblasts.
- While patients with thalassemia may experience fatigue and lightheadedness due to anemia, the presence of sideroblasts on smear and recent initiation of TB treatment point away from this diagnosis.
*Inhibition of ferrochelatase and ALA dehydratase*
- Inhibition of **ferrochelatase** and **ALA dehydratase** is characteristic of **lead poisoning**, which presents with signs of anemia and can cause sideroblastic anemia.
- However, there is no mention of lead exposure in the patient's history, and the recent initiation of TB treatment is a more direct and likely explanation for drug-induced sideroblastic anemia.
*Abnormally low level of glutathione activity*
- Abnormally low levels of **glutathione activity**, often due to **glucose-6-phosphate dehydrogenase (G6PD) deficiency**, lead to **hemolytic anemia** (e.g., after exposure to oxidative stressors like certain drugs or infections).
- G6PD deficiency is more common in **Mediterranean populations** and can be triggered by isoniazid. However, G6PD deficiency is associated with **Heinz bodies** and **bite cells** on peripheral smear, **not sideroblasts**.
- The smear findings are definitive in distinguishing between these two complications of TB treatment.
*Iron deficiency*
- **Iron deficiency** leads to **microcytic, hypochromic anemia** due to insufficient heme synthesis.
- While it causes fatigue and lightheadedness, **iron deficiency anemia does not cause sideroblastic anemia** and would not present with sideroblasts on the peripheral blood smear.
Vitamin cofactor functions in metabolism US Medical PG Question 7: A homeless woman presents with shortness of breath on exertion and pedal edema. Cardiac workup performed shows evidence of dilated cardiomyopathy and increased cardiac output. She also has decreased sensation over both extremities bilaterally. Which vitamin deficiency most likely caused these symptoms?
- A. Vitamin B6
- B. Vitamin C
- C. Vitamin B1 (Correct Answer)
- D. Vitamin B3
- E. Vitamin A
Vitamin cofactor functions in metabolism Explanation: ***Vitamin B1***
- The combination of **dilated cardiomyopathy**, **high-output heart failure** (manifesting as shortness of breath and pedal edema), and **peripheral neuropathy** (decreased sensation) is classic for **wet beriberi**, caused by thiamine (Vitamin B1) deficiency.
- **Homelessness** is a significant risk factor for nutritional deficiencies, including thiamine deficiency, due to inadequate diet.
*Vitamin B6*
- Deficiency can cause **peripheral neuropathy**, but it does not typically lead to **dilated cardiomyopathy** or **high-output heart failure**.
- Other manifestations of B6 deficiency include **sideroblastic anemia** and **seizures**.
*Vitamin C*
- Deficiency causes **scurvy**, characterized by **gingivitis**, **poor wound healing**, **petechiae**, and joint pain.
- It does not present with **cardiomyopathy** or **neuropathy** as described.
*Vitamin B3*
- Deficiency causes **pellagra**, characterized by the "3 Ds": **dermatitis**, **diarrhea**, and **dementia**.
- While it can affect the nervous system (dementia), it does not typically cause **dilated cardiomyopathy** or **peripheral neuropathy**.
*Vitamin A*
- Deficiency primarily affects **vision** (e.g., **night blindness**, **xerophthalmia**) and immune function.
- It is not associated with **cardiac** or **neurological symptoms** like those described in the patient.
Vitamin cofactor functions in metabolism US Medical PG Question 8: A 58-year-old man presents to the Emergency Department after 3 hours of intense suprapubic pain associated with inability to urinate for the past day or two. His medical history is relevant for benign prostatic hyperplasia (BPH) that has been under treatment with prazosin and tadalafil. Upon admission, he is found to have a blood pressure of 180/100 mm Hg, a pulse of 80/min, a respiratory rate of 23/min, and a temperature of 36.5°C (97.7°F). He weighs 84 kg (185.1 lb) and is 175 cm (5 ft 7 in) tall. Physical exam, he has suprapubic tenderness. A bladder scan reveals 700 ml of urine. A Foley catheter is inserted and the urine is drained. Initial laboratory tests and their follow up 8 hours after admission are shown below.
Admission 8 hours after admission
Serum potassium 4.2 mmol/L Serum potassium 4.0 mmol/L
Serum sodium 140 mmol/L Serum sodium 142 mmol/L
Serum chloride 102 mmol/L Serum chloride 110 mmol/L
Serum creatinine 1.4 mg/dL Serum creatinine 1.6 mg/dL
Serum blood urea nitrogen 64 mg/dL Serum blood urea nitrogen 62 mg/dL
Urine output 250 mL Urine output 260 mL
A senior attending suggests a consultation with Nephrology. Which of the following best justifies this suggestion?
- A. Estimated glomerular filtration rate (eGFR)
- B. Urine output (Correct Answer)
- C. Serum creatinine (SCr)
- D. Serum blood urea nitrogen (BUN)
- E. Serum potassium
Vitamin cofactor functions in metabolism Explanation: ***Urine output***
- The patient's **urine output is severely reduced** at 260 mL over 8 hours (approximately **32.5 mL/hour**), which constitutes **oliguria** (defined as <0.5 mL/kg/hr; this patient at 84 kg should produce ≥42 mL/hr).
- Despite **relief of the post-renal obstruction** via Foley catheterization, the persistent oliguria indicates **intrinsic kidney injury** rather than simple mechanical obstruction.
- The combination of **oliguria persisting after decompression** + **rising serum creatinine** (1.4→1.6 mg/dL) meets **KDIGO criteria for Stage 2 AKI** (urine output <0.5 mL/kg/hr for ≥12 hours).
- This requires **urgent nephrology consultation** to assess for acute tubular necrosis (ATN), guide fluid management during potential post-obstructive diuresis, and consider renal replacement therapy if oliguria worsens.
*Serum creatinine (SCr)*
- The serum creatinine **rose from 1.4 to 1.6 mg/dL** despite bladder decompression, which is concerning and suggests intrinsic renal injury.
- However, creatinine is a **lagging indicator** of kidney function - it takes 24-48 hours to reflect acute changes in GFR, whereas **urine output is a real-time indicator** of kidney function.
- While the rising creatinine supports the need for nephrology involvement, **urine output is the more immediate and actionable parameter** that prompted the attending's suggestion at this early time point.
*Estimated glomerular filtration rate (eGFR)*
- eGFR is **calculated from serum creatinine** using equations that assume steady-state conditions, which **do not apply in acute kidney injury**.
- In the **acute setting with rapidly changing kidney function**, eGFR calculations are unreliable and can significantly overestimate or underestimate true GFR.
- Clinicians rely more on **urine output and serial creatinine measurements** rather than eGFR when managing AKI.
*Serum blood urea nitrogen (BUN)*
- The BUN decreased slightly from 64 to 62 mg/dL, remaining elevated but showing minimal change after catheterization.
- Elevated BUN can reflect **pre-renal azotemia, dehydration, or upper GI bleeding** and is less specific for intrinsic kidney injury than oliguria.
- The **BUN:Cr ratio** is approximately 40:1 (64/1.6), suggesting a **pre-renal component**, but this alone doesn't justify urgent nephrology consultation as strongly as the persistent oliguria does.
*Serum potassium*
- Serum potassium levels remain **normal** (4.2→4.0 mmol/L) and do not indicate a metabolic emergency.
- While **hyperkalemia** is a common complication of AKI that would warrant nephrology involvement, this patient's potassium is well-controlled and not the driving concern at this time.
Vitamin cofactor functions in metabolism US Medical PG Question 9: A previously healthy 18-year-old woman comes to the physician because of a 2-day history of swelling and itchiness of her mouth and lips. It decreases when she eats cold foods such as frozen fruit. Four days ago, she underwent orthodontic wire-placement on her upper and lower teeth. Since then, she has been taking ibuprofen twice daily for the pain. For the past 6 months, she has been on a strict vegan diet. She is sexually active with one partner and uses condoms consistently. She had chickenpox that resolved spontaneously when she was 6 years old. Her vitals are within normal limits. Examination shows diffuse erythema and edema of the buccal mucosa with multiple serous vesicles and shallow ulcers. Stroking the skin with pressure does not cause blistering of the skin. The remainder of the examination shows no abnormalities. Which of the following is the most likely cause of these symptoms?
- A. Vitamin deficiency
- B. Dermatitis herpetiformis
- C. Allergic contact dermatitis (Correct Answer)
- D. Reactivation of varicella zoster virus
- E. Herpes labialis
Vitamin cofactor functions in metabolism Explanation: ***Allergic contact dermatitis***
- The symptoms of **swelling, itchiness**, and **erythema of the buccal mucosa** with vesicles and shallow ulcers, occurring after orthodontic wire placement, strongly suggest an allergic reaction to materials in the wires (e.g., nickel).
- The improvement with **cold foods** (vasoconstriction and soothing effect) and the absence of skin blistering with pressure (differentiating from bullous diseases) further support this diagnosis.
*Vitamin deficiency*
- While a **vegan diet** can predispose to certain vitamin deficiencies (e.g., B12), the sudden onset of localized oral swelling and itchiness is not typical.
- Oral manifestations of vitamin deficiencies usually develop chronically and involve conditions like **glossitis, angular cheilitis, or stomatitis**, rather than acute localized swelling and vesicles.
*Dermatitis herpetiformis*
- This condition is characterized by intensely pruritic, vesicular lesions, primarily on **extensor surfaces** (elbows, knees, buttocks), and is strongly associated with **celiac disease**.
- Oral lesions are uncommon, and the lack of systemic GI symptoms or characteristic skin distribution makes this diagnosis less likely.
*Reactivation of varicella zoster virus*
- Reactivation (shingles) typically causes a **unilateral, dermatomal rash** with painful vesicles, usually occurring in older or immunocompromised individuals.
- The patient's age and healthy status, along with the bilateral involvement of the mouth and lips, do not fit the typical presentation of zoster reactivation.
*Herpes labialis*
- Caused by **Herpes Simplex Virus (HSV)**, it presents as clusters of painful vesicles, typically on the **lips or perioral region**.
- While vesicles are present, the diffuse erythema and edema of the buccal mucosa and the clear association with orthodontic hardware placement make allergic contact dermatitis a more likely etiology.
Vitamin cofactor functions in metabolism US Medical PG Question 10: An 8-year-old boy presents with recurrent infections including multiple episodes of pneumonia and diarrhea. He reports difficulty seeing in the dark. Physical examination reveals white patches on the sclera and conjunctival dryness. What is the most likely cause of these findings?
- A. Congenital rubella
- B. Spinocerebellar ataxia (SCA) type 1
- C. Deficiency of vitamin A (Correct Answer)
- D. Autoimmune neutropenia
- E. Vitamin B1 deficiency
Vitamin cofactor functions in metabolism Explanation: ***Deficiency of vitamin A***
- The combination of **recurrent infections** (pneumonia, diarrhea), **night blindness**, and **ocular signs** like white patches on the sclera (Bitot's spots due to keratinized epithelium) and conjunctival dryness (xerophthalmia) are classic manifestations of **vitamin A deficiency**.
- Vitamin A is crucial for **immune function**, **vision** (a component of rhodopsin), and the **maintenance of epithelial tissues**.
*Congenital rubella*
- This typically presents with a **triad of cataracts**, **heart defects** (e.g., patent ductus arteriosus), and **sensorineural hearing loss**, often detected earlier in infancy.
- It does not explain the recurrent infections, night blindness, or specific ocular epithelial changes described.
*Spinocerebellar ataxia (SCA) type 1*
- This is a **neurodegenerative disorder** primarily affecting coordination and balance, leading to progressive **ataxia**.
- It does not cause recurrent infections, night blindness, or xerophthalmia; its symptoms are distinct and neurological in nature.
*Autoimmune neutropenia*
- Primarily causes **recurrent bacterial infections** due to low neutrophil counts.
- It does not explain the night blindness, diarrhea, or the specific ocular findings of keratinization.
*Vitamin B1 deficiency*
- Also known as **thiamine deficiency**, it leads to **beriberi**, characterized by cardiac (wet beriberi) or neurological (dry beriberi) symptoms.
- Common symptoms include **peripheral neuropathy**, **heart failure**, and **Wernicke-Korsakoff syndrome**, none of which are descriptive of this patient's presentation.
More Vitamin cofactor functions in metabolism US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.