Mineral deficiency disorders US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Mineral deficiency disorders. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Mineral deficiency disorders US Medical PG Question 1: A 25-year-old African-American woman visits the doctor’s office complaining of fatigue for a couple of months. She says that she feels exhausted by the end of the day. She works as a dental assistant and is on her feet most of the time. However, she eats well and also tries to walk for 30 minutes every morning. She also says that she sometimes feels breathless and has to gasp for air, especially when she is walking or jogging. Her past medical history is insignificant, except for occasional bouts of cold during the winters. Her physical exam findings are within normal limits except for moderate conjunctival pallor. Complete blood count results and iron profile are as follows:
Hemoglobin 9 g/dL
Hematocrit 28.5%
RBC count 5.85 x 106/mm3
WBC count 5,500/mm3
Platelet count 212,000/mm3
MCV 56.1 fl
MCH 20.9 pg/cell
MCHC 25.6 g/dL
RDW 11.7% Hb/cell
Serum iron 170 mcg/dL
Total iron-binding capacity (TIBC) 458 mcg/dL
Transferrin saturation 60%
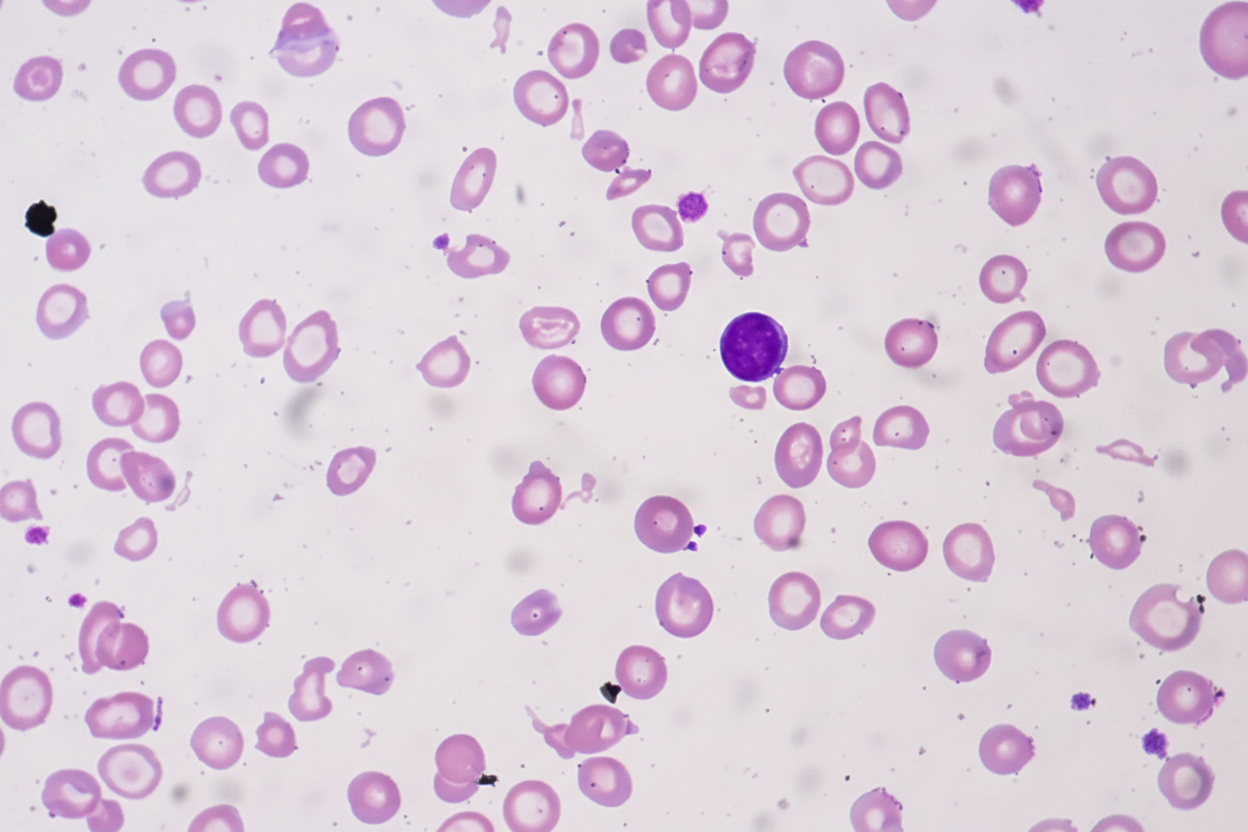
A peripheral blood smear is given. When questioned about her family history of anemia, she says that all she remembers is her dad was never allowed to donate blood as he was anemic. Which of the following most likely explains her cell counts and blood smear results?
- A. Thalassemia (Correct Answer)
- B. Iron-deficiency anemia
- C. B12 deficiency
- D. Hemolysis
- E. Folate deficiency
Mineral deficiency disorders Explanation: ***Thalassemia***
- The patient presents with **microcytic, hypochromic anemia** (low MCV, MCH, MCHC) despite elevated iron stores, which is characteristic of thalassemia.
- The **elevated RBC count** (5.85 x 10^6/mm³) in the presence of anemia (hemoglobin 9 g/dL) is a hallmark of thalassemia, as the body attempts to compensate for ineffective erythropoiesis.
- The **elevated serum iron (170 mcg/dL) and high transferrin saturation (60%)** indicate iron overload, not iron deficiency, which occurs in thalassemia due to ineffective erythropoiesis and increased iron absorption.
- The **low RDW (11.7%)** indicates uniform cell size despite microcytosis, typical of thalassemia (vs. high RDW in iron deficiency).
- **Positive family history** (father was anemic and couldn't donate blood) supports an inherited disorder.
*Iron-deficiency anemia*
- This condition typically presents with **low serum iron**, **high TIBC**, and **low transferrin saturation** (<20%), which contradicts the patient's iron profile showing elevated iron and high transferrin saturation (60%).
- While iron-deficiency anemia also causes **microcytic, hypochromic RBCs**, the RBC count would be low or normal (not elevated), and RDW would be elevated (>14%) due to anisocytosis.
*B12 deficiency*
- **B12 deficiency** causes **macrocytic anemia** (high MCV >100 fl), which is inconsistent with the patient's low MCV (56.1 fl).
- It also often presents with neurological symptoms (peripheral neuropathy, subacute combined degeneration), which are absent in this case.
*Hemolysis*
- While hemolysis can cause anemia and fatigue, it is usually associated with elevated **reticulocyte count**, **indirect bilirubin**, and **LDH**, and decreased **haptoglobin**, none of which are indicated here.
- Hemolysis typically presents with **normocytic anemia** (normal MCV), not the marked **microcytosis** (MCV 56.1 fl) seen in this patient.
*Folate deficiency*
- Similar to B12 deficiency, **folate deficiency** leads to **macrocytic anemia** (high MCV >100 fl), which is not observed in this patient with MCV of 56.1 fl.
- Folate deficiency does not cause neurological symptoms (unlike B12 deficiency), but the **macrocytic** red cell morphology is the key differentiator here.
Mineral deficiency disorders US Medical PG Question 2: A 37-year-old man is brought to the emergency department because he was found down on a city sidewalk. Upon presentation he is found to be disheveled with multiple poorly healed wounds on his hands and feet. He has had dozens of previous presentations for alcohol intoxication and is currently known to be homeless. Physical examination reveals multiple minor wounds, alopecia, and decreased axillary hair. Upon being aroused, the patient reveals that he has had difficulty with taste and smell and has also had severe diarrhea over the last week. The deficient substance most likely responsible for this patient's symptoms is associated with which of the following proteins?
- A. Tyrosinase
- B. Hemoglobin
- C. Glutathione peroxidase
- D. RNA polymerase (Correct Answer)
- E. Thyroid hormone
Mineral deficiency disorders Explanation: ***Correct: RNA polymerase***
* The clinical presentation of **poorly healed wounds, alopecia, decreased axillary hair, dysgeusia/anosmia, and diarrhea** in a homeless patient with chronic alcoholism is classic for **zinc deficiency**.
* **Zinc is an essential cofactor for RNA polymerase**, the enzyme responsible for DNA transcription and ultimately protein synthesis. Zinc deficiency impairs cellular proliferation and protein synthesis, which explains the poor wound healing, hair loss, and other manifestations.
* Zinc is also a cofactor for over 300 enzymes including alkaline phosphatase, carbonic anhydrase, superoxide dismutase, and various matrix metalloproteinases critical for wound healing and tissue maintenance.
*Incorrect: Glutathione peroxidase*
* **Glutathione peroxidase requires SELENIUM, not zinc**, as its essential cofactor. This enzyme protects against oxidative damage by reducing hydrogen peroxide.
* Selenium deficiency presents with **cardiomyopathy (Keshan disease), myopathy, and thyroid dysfunction**, not the constellation of symptoms seen in this patient.
*Incorrect: Tyrosinase*
* **Tyrosinase is a copper-dependent enzyme** involved in melanin synthesis. Copper deficiency causes **anemia, neutropenia, and neurological symptoms** (myelopathy), not the dermatologic and sensory changes seen here.
* While copper deficiency can occur in alcoholism, the specific symptoms of taste/smell disturbances and characteristic skin findings point to zinc deficiency.
*Incorrect: Thyroid hormone*
* Thyroid hormone synthesis requires **iodine**, not zinc. Hypothyroidism presents with **fatigue, weight gain, cold intolerance, and bradycardia**.
* The patient's acute presentation with diarrhea, taste/smell disturbances, and poor wound healing does not fit thyroid dysfunction.
*Incorrect: Hemoglobin*
* Hemoglobin requires **iron** for oxygen transport. Iron deficiency causes **microcytic anemia with fatigue, pallor, and koilonychia**.
* While chronic alcoholics may develop anemia (often macrocytic from folate/B12 deficiency), the specific symptoms of dysgeusia, anosmia, and characteristic dermatologic findings indicate zinc deficiency as the primary issue.
Mineral deficiency disorders US Medical PG Question 3: A previously healthy 44-year-old man comes to his physician because of frequent urination and increased thirst for several weeks. Physical examination shows darkened skin and a firm mass in the right upper quadrant. His blood glucose is 220 mg/dL. A photomicrograph of a specimen obtained on liver biopsy is shown. Which of the following best describes the pathogenesis of the disease process in this patient?
- A. Defective serum copper transportation
- B. Defective transferrin receptor binding (Correct Answer)
- C. Absence of a serine protease inhibitor
- D. Upregulation of erythropoietin production
- E. Absence of β-globin synthesis
Mineral deficiency disorders Explanation: ***Defective transferrin receptor binding***
- This patient presents with symptoms of **diabetes mellitus** (frequent urination, increased thirst, elevated blood glucose), **bronze diabetes** (darkened skin), and signs of **liver disease** (firm mass in RUQ, biopsy showing iron deposition). This constellation of symptoms is characteristic of **hereditary hemochromatosis**.
- Hereditary hemochromatosis is an **autosomal recessive disorder** most commonly caused by mutations in the **HFE gene** (especially **C282Y mutation**). The HFE protein normally binds to **transferrin receptor 1 (TfR1)** on cell surfaces to sense iron levels. When HFE is mutated, this **interaction is defective**, impairing the cell's ability to sense iron status.
- This defective HFE-TfR1 binding leads to **inappropriately low hepcidin production** by the liver. With insufficient hepcidin, **ferroportin** (iron exporter) remains active on intestinal enterocytes, resulting in **excessive intestinal iron absorption** and **iron deposition** in multiple organs (liver, pancreas, heart, skin).
- The liver biopsy shows **iron accumulation within hepatocytes**, confirming the diagnosis.
*Defective serum copper transportation*
- This describes **Wilson's disease**, caused by mutations in the **ATP7B gene**, leading to **copper accumulation** in the liver, brain, cornea, and other tissues.
- Clinical features include **neurological symptoms** (tremor, dystonia), **Kayser-Fleischer rings** in the cornea, and **liver cirrhosis**. The presentation differs from iron overload with bronze diabetes.
*Absence of a serine protease inhibitor*
- This refers to **alpha-1 antitrypsin deficiency**, where absence of this serine protease inhibitor leads to **uninhibited neutrophil elastase activity**, primarily causing **early-onset emphysema** and **liver cirrhosis**.
- Liver biopsy would show **PAS-positive, diastase-resistant globules** in hepatocytes, not iron deposition. The clinical presentation would not include bronze skin or secondary diabetes from pancreatic iron overload.
*Upregulation of erythropoietin production*
- **Upregulation of erythropoietin** occurs in response to **hypoxia** and stimulates **increased red blood cell production**, as seen in **polycythemia vera** or high-altitude adaptation.
- This mechanism does not cause the iron overload and multi-organ damage seen in hemochromatosis. While erythropoiesis requires iron, hemochromatosis results from primary defects in iron absorption regulation, not erythropoietin dysregulation.
*Absence of β-globin synthesis*
- This is characteristic of **beta-thalassemia**, where **reduced or absent beta-globin chain synthesis** leads to **ineffective erythropoiesis** and **hemolytic anemia**.
- While beta-thalassemia major can cause **secondary iron overload** (from chronic transfusions and increased GI absorption due to ineffective erythropoiesis), the **primary defect is in hemoglobin synthesis**, not in the iron regulatory pathway as seen in hereditary hemochromatosis.
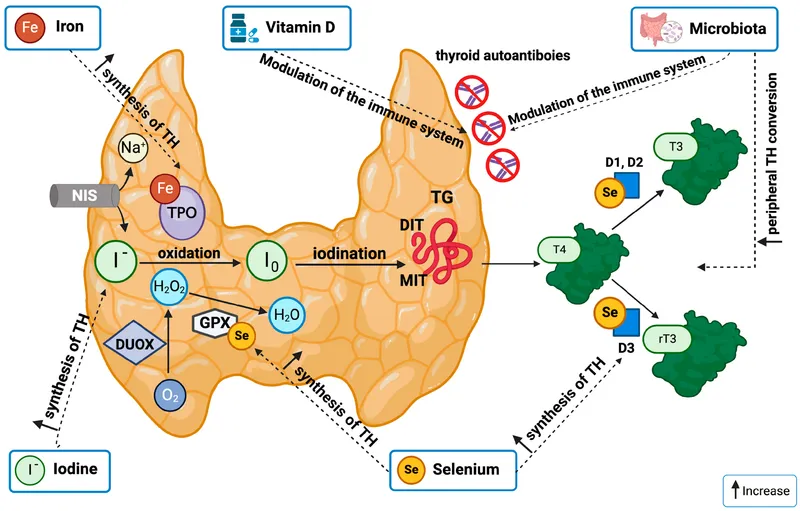
Mineral deficiency disorders US Medical PG Question 4: An investigator is studying a drug that acts on the thyroid hormone pathway. Levels of serum free T3 and T4 in healthy participants are measured before and after administration of the drug. After administration, there is a decrease in the average serum free T3 level, while the average serum free T4 level is increased compared to initial serum studies. Inhibition of which of the following is the most likely mechanism of action of this drug?
- A. Thyroid-stimulating hormone
- B. Follicular iodotyrosine deiodinase
- C. Follicular thyroid peroxidase
- D. Peripheral 5'-deiodinase (Correct Answer)
- E. Follicular thyroid proteases
Mineral deficiency disorders Explanation: ***Peripheral 5'-deiodinase***
- Inhibition of **peripheral 5'-deiodinase** would decrease the conversion of **T4 to T3** in the periphery, resulting in lower **free T3** and higher **free T4** levels.
- This enzyme is crucial for activating T4 into the more potent T3, and its blockade explains the observed changes in hormone levels.
*Thyroid-stimulating hormone*
- Inhibition of **TSH** would lead to a decrease in the production and release of both **T3 and T4** from the thyroid gland.
- This contradicts the observed increase in **free T4** levels.
*Follicular iodotyrosine deiodinase*
- This enzyme is involved in recycling iodine from **monoiodotyrosine (MIT)** and **diiodotyrosine (DIT)** within the thyroid follicular cells, which is important for efficient thyroid hormone synthesis.
- Its inhibition would primarily affect iodine availability and synthesis, not directly lead to increased T4 and decreased T3 in the periphery.
*Follicular thyroid peroxidase*
- **Thyroid peroxidase (TPO)** is critical for the **iodination of tyrosine residues** on thyroglobulin and the **coupling of MIT and DIT** to form T3 and T4.
- Inhibition of TPO would decrease the synthesis of both **T3 and T4**, contrary to the observed increase in **free T4**.
*Follicular thyroid proteases*
- **Thyroid proteases** cleave thyroglobulin to release mature **T3 and T4** into the bloodstream.
- Inhibition of these proteases would lead to a decrease in the release of both **T3 and T4**, which does not align with the observed increase in **free T4**.
Mineral deficiency disorders US Medical PG Question 5: A 57-year-old woman comes to the physician because of a 3-month history of easy fatigability and dyspnea on exertion. Menopause occurred 5 years ago. Her pulse is 105/min and blood pressure is 100/70 mm Hg. Physical examination shows pallor of the nail beds and conjunctivae. A peripheral blood smear shows small, pale red blood cells. Further evaluation is most likely to show which of the following findings?
- A. Increased concentration of HbA2
- B. Decreased serum haptoglobin concentration
- C. Positive stool guaiac test (Correct Answer)
- D. Dry bone marrow tap
- E. Increased serum methylmalonic acid concentration
Mineral deficiency disorders Explanation: ***Positive stool guaiac test***
* The patient's symptoms of **fatigability**, **dyspnea on exertion**, and signs like **pallor**, along with a peripheral blood smear showing **small, pale red blood cells** (**microcytic hypochromic anemia**), are highly indicative of **iron deficiency anemia**.
* In a 57-year-old postmenopausal woman, the most common cause of **iron deficiency anemia** is **chronic blood loss from the gastrointestinal (GI) tract**, which would be detected by a **positive stool guaiac test**.
*Increased concentration of HbA2*
* An increased concentration of **HbA2** is characteristic of **beta-thalassemia minor**, a genetic disorder, which presents as microcytic anemia, but the clinical context and age make iron deficiency due to blood loss more likely in this patient.
* While both can cause microcytic anemia, the patient's acute presentation of symptoms and postmenopausal status strongly point to an acquired cause like chronic blood loss rather than a lifelong genetic condition.
*Decreased serum haptoglobin concentration*
* **Decreased serum haptoglobin concentration** is a marker of **hemolytic anemia**, where red blood cells are prematurely destroyed, leading to the release of free hemoglobin that binds to haptoglobin.
* The patient's peripheral smear finding of **small, pale red blood cells** (microcytic hypochromic) is inconsistent with hemolysis as the primary cause; hemolytic anemias often present with normocytic or macrocytic red blood cells.
*Dry bone marrow tap*
* A **dry bone marrow tap** is typically associated with **myelofibrosis** or sometimes **hairy cell leukemia** or severe aplastic anemia, where the bone marrow is fibrotic or hypocellular and cannot be aspirated.
* Iron deficiency anemia, while causing anemia, does not typically lead to a dry bone marrow tap; the marrow would usually be hypercellular with erythroid hyperplasia, reflecting the body's attempt to compensate for the anemia.
*Increased serum methylmalonic acid concentration*
* An **increased serum methylmalonic acid concentration** is a specific marker for **vitamin B12 deficiency**, which causes **megaloblastic (macrocytic) anemia**.
* The patient's peripheral blood smear findings of **small, pale red blood cells** (microcytic hypochromic) are inconsistent with **vitamin B12 deficiency**, which leads to **large red blood cells**.
Mineral deficiency disorders US Medical PG Question 6: A 52-year-old male presents to clinic with complaints of anxiety and fatigue for 4 months. He has also been experiencing palpitations, muscle weakness, increased sweating, and an increase in the frequency of defecation. Past medical history is insignificant. He neither consumes alcohol nor smokes cigarettes. His pulse is 104/min and irregular, blood pressure is 140/80 mm Hg. On examination, you notice that he has bilateral exophthalmos. There are fine tremors in both hands. Which of the following results would you expect to see on a thyroid panel?
- A. High TSH; Low T4; Low T3
- B. High TSH; High T4; High T3
- C. Normal TSH; Low total T4; Normal Free T4 and T3
- D. Low TSH; High T4; High T3 (Correct Answer)
- E. Normal TSH; Low T4; Low T3
Mineral deficiency disorders Explanation: ***Low TSH; High T4; High T3***
- The patient's symptoms (anxiety, fatigue, palpitations, muscle weakness, increased sweating, increased defecation frequency, tachycardia, hypertension, exophthalmos, fine tremors) are classic for **hyperthyroidism**, particularly **Graves' disease**.
- In primary hyperthyroidism, the thyroid gland overproduces T3 and T4, leading to **high levels of T4 and T3**. This then causes a negative feedback loop to the pituitary, resulting in **suppressed (low) TSH** levels.
*High TSH; Low T4; Low T3*
- This pattern is indicative of **primary hypothyroidism**, where the thyroid gland is underactive and cannot produce sufficient T4 and T3, leading to low levels of these hormones and a compensatory rise in TSH.
- The presented symptoms are directly opposite to those seen in hypothyroidism.
*High TSH; High T4; High T3*
- This combination is characteristic of **secondary hyperthyroidism**, which is much rarer and caused by a TSH-secreting pituitary adenoma.
- While it presents with hyperthyroid symptoms, the TSH level would be elevated or inappropriately normal, not suppressed.
*Normal TSH; Low total T4; Normal Free T4 and T3*
- This pattern is often seen in **euthyroid sick syndrome** or conditions causing a decrease in thyroid-binding globulin (TBG).
- The patient's clinical presentation is clearly that of hyperthyroidism, not a euthyroid state.
*Normal TSH; Low T4; Low T3*
- This result is atypical for any specific thyroid disorder and does not align with the patient's symptoms of hyperthyroidism, which demand high circulating thyroid hormone levels.
- A "normal TSH, low T4, low T3" might suggest central hypothyroidism if TSH was inappropriately normal for the low thyroid hormones, but this patient's symptoms definitively point to thyroid hormone excess.
Mineral deficiency disorders US Medical PG Question 7: A homeless woman presents with shortness of breath on exertion and pedal edema. Cardiac workup performed shows evidence of dilated cardiomyopathy and increased cardiac output. She also has decreased sensation over both extremities bilaterally. Which vitamin deficiency most likely caused these symptoms?
- A. Vitamin B6
- B. Vitamin C
- C. Vitamin B1 (Correct Answer)
- D. Vitamin B3
- E. Vitamin A
Mineral deficiency disorders Explanation: ***Vitamin B1***
- The combination of **dilated cardiomyopathy**, **high-output heart failure** (manifesting as shortness of breath and pedal edema), and **peripheral neuropathy** (decreased sensation) is classic for **wet beriberi**, caused by thiamine (Vitamin B1) deficiency.
- **Homelessness** is a significant risk factor for nutritional deficiencies, including thiamine deficiency, due to inadequate diet.
*Vitamin B6*
- Deficiency can cause **peripheral neuropathy**, but it does not typically lead to **dilated cardiomyopathy** or **high-output heart failure**.
- Other manifestations of B6 deficiency include **sideroblastic anemia** and **seizures**.
*Vitamin C*
- Deficiency causes **scurvy**, characterized by **gingivitis**, **poor wound healing**, **petechiae**, and joint pain.
- It does not present with **cardiomyopathy** or **neuropathy** as described.
*Vitamin B3*
- Deficiency causes **pellagra**, characterized by the "3 Ds": **dermatitis**, **diarrhea**, and **dementia**.
- While it can affect the nervous system (dementia), it does not typically cause **dilated cardiomyopathy** or **peripheral neuropathy**.
*Vitamin A*
- Deficiency primarily affects **vision** (e.g., **night blindness**, **xerophthalmia**) and immune function.
- It is not associated with **cardiac** or **neurological symptoms** like those described in the patient.
Mineral deficiency disorders US Medical PG Question 8: A 6-month-old boy presents with decreased growth, pigmented retinopathy, hemolytic anemia, and peripheral neuropathy. You suspect that these signs are the result of a vitamin deficiency leading to increased oxidative damage to lipids. Which of the following is most likely responsible for this patient's symptoms?
- A. Excessive boiling of formula
- B. Goat milk ingestion
- C. Abetalipoproteinemia (Correct Answer)
- D. Pernicious anemia
- E. Hartnup disease
Mineral deficiency disorders Explanation: ***Abetalipoproteinemia***
- This condition is characterized by a defect in **microsomal triglyceride transfer protein (MTP)**, leading to an inability to synthesize ApoB-containing lipoproteins.
- The resulting **malabsorption of fat and fat-soluble vitamins (especially vitamin E)** leads to the neurological symptoms (retinopathy, neuropathy) and hemolytic anemia due to increased oxidative stress on red blood cell membranes.
*Excessive boiling of formula*
- Excessive boiling of formula could potentially degrade some **heat-sensitive vitamins**, such as vitamin C or thiamine (B1).
- However, this is unlikely to cause a severe, combined deficiency leading to the specific constellation of symptoms seen, particularly the ophthalmologic and neurological signs related to **fat-soluble vitamin malabsorption**.
*Goat milk ingestion*
- Goat milk is naturally low in **folate** and **vitamin D** and can cause **folate deficiency anemia** and rickets if it's the sole source of nutrition for an infant.
- However, it does not typically cause the entire spectrum of symptoms described, particularly **pigmented retinopathy** and **peripheral neuropathy**, which are more indicative of **vitamin E deficiency**.
*Pernicious anemia*
- Pernicious anemia is caused by a deficiency in **intrinsic factor**, leading to **vitamin B12 malabsorption**.
- Symptoms primarily include **megaloblastic anemia**, **glossitis**, and **neurological deficits** (subacute combined degeneration of the spinal cord), but not pigmented retinopathy or hemolytic anemia due to increased fatty acid oxidation via vitamin E malabsorption.
*Hartnup disease*
- Hartnup disease is an inherited disorder of **amino acid transport**, specifically affecting the absorption of **neutral amino acids** like tryptophan.
- It leads to **niacin deficiency** (pellagra-like symptoms) and can cause skin rashes, ataxia, and psychiatric symptoms, but not hemolytic anemia or pigmented retinopathy.
Mineral deficiency disorders US Medical PG Question 9: A 23-year-old woman presents to her primary care physician due to amenorrhea. The patient states that historically she has her period once every three months but recently has not had it at all. Otherwise, she has no other complaints. The patient recently started college and is a varsity athlete for the track team. She works part time in a coffee shop and is doing well in school. The patient is not sexually active and does not drink alcohol, use illicit drugs, or smoke. She has no significant past medical history and occasionally takes ibuprofen for headaches. Her temperature is 99.5°F (37.5°C), blood pressure is 100/55 mmHg, pulse is 50/min, respirations are 10/min, and oxygen saturation is 98% on room air. On physical exam, you note a young, lean, muscular woman in no acute distress. Which of the following is the most likely long-term outcome in this patient?
- A. Osteoarthritis
- B. Infertility
- C. Endometrial cancer
- D. Anorexia nervosa
- E. Osteoporosis (Correct Answer)
Mineral deficiency disorders Explanation: ***Osteoporosis***
- This patient likely has **functional hypothalamic amenorrhea (FHA)** due to her athletic activity, low body weight, and stress, leading to low **estrogen** levels.
- **Chronic hypoestrogenism** is a significant risk factor for **decreased bone mineral density** and subsequent **osteoporosis** and stress fractures.
*Osteoarthritis*
- **Osteoarthritis** is a degenerative joint disease typically associated with aging, obesity, or joint injury, none of which are primary features in this patient's presentation.
- While intense athletic activity can contribute to joint wear over time, it is not a direct long-term consequence of the amenorrhea and hypoestrogenic state.
*Infertility*
- While **functional hypothalamic amenorrhea (FHA)** can cause temporary infertility as long as menstruation is suppressed, ovulation can resume once the underlying causes (e.g., intense exercise, low body weight, stress) are addressed.
- Therefore, infertility is not necessarily a permanent long-term outcome if the condition is managed.
*Endometrial cancer*
- Amenorrhea, particularly **anovulatory cycles** with prolonged estrogen exposure *without* progesterone withdrawal (as seen in PCOS), can increase the risk of endometrial hyperplasia and cancer.
- However, in **functional hypothalamic amenorrhea (FHA)**, low estrogen levels typically lead to a **thinner endometrium**, which *reduces* rather than increases the risk of endometrial cancer.
*Anorexia nervosa*
- Although **anorexia nervosa** can cause amenorrhea due to extremely low body weight and nutritional deficiencies, this patient's history and physical exam do not suggest an eating disorder.
- She is described as lean and muscular from athletic activity, not emaciated or exhibiting other signs of anorexia nervosa.
Mineral deficiency disorders US Medical PG Question 10: The parents of a newly adopted 5-year-old child brought him to the pediatrician after he started to have bouts of diarrhea and bloating. His symptoms are worse after consuming dairy products and ice cream. The immunization history is up to date. His height and weight are in the 60th and 70th percentiles, respectively. His physical examination is normal. The pediatrician orders some lab tests because she believes there is a biochemical disorder. What is the first-line therapy for the most likely condition?
- A. Omeprazole
- B. Cholestyramine
- C. Diet modification (Correct Answer)
- D. Metoclopramide
- E. Pancreatic lipase supplement
Mineral deficiency disorders Explanation: ***Diet modification***
- The child's symptoms of **diarrhea** and **bloating** worsening after consuming **dairy products** and **ice cream** are classic signs of **lactose intolerance**.
- The first-line therapy for lactose intolerance involves **reducing or eliminating lactose-containing foods** from the diet.
*Omeprazole*
- **Omeprazole** is a **proton pump inhibitor (PPI)** used to reduce stomach acid production.
- It is indicated for conditions like **gastroesophageal reflux disease (GERD)** or peptic ulcers, which are not suggested by the child's symptoms.
*Cholestyramine*
- **Cholestyramine** is a **bile acid sequestrant** used to lower cholesterol and treat **bile acid malabsorption**, which typically presents with chronic watery diarrhea.
- While it can cause diarrhea as a side effect, it would not be the primary therapy for symptoms related to dairy consumption.
*Metoclopramide*
- **Metoclopramide** is a **prokinetic agent** that increases gastrointestinal motility.
- It is used to treat **nausea, vomiting**, and **gastroparesis**, which are not the presenting complaints in this case.
*Pancreatic lipase supplement*
- **Pancreatic lipase supplements** are used to treat **exocrine pancreatic insufficiency**, where the pancreas does not produce enough enzymes to digest fats, proteins, and carbohydrates.
- This condition involves **steatorrhea** (fatty stools) and malabsorption of all macronutrients, which differs from the dairy-specific symptoms described.
More Mineral deficiency disorders US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.