Fat-soluble vitamins (A, D, E, K) US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Fat-soluble vitamins (A, D, E, K). These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Fat-soluble vitamins (A, D, E, K) US Medical PG Question 1: You are counseling a pregnant woman who plans to breast-feed exclusively regarding her newborn's nutritional requirements. The child was born at home and the mother only plans for her newborn to receive vaccinations but no other routine medical care. Which vitamins should be given to the newborn?
- A. Vitamin B6
- B. Vitamin K and Vitamin D (Correct Answer)
- C. Vitamin K
- D. Folic acid
- E. Vitamin D
Fat-soluble vitamins (A, D, E, K) Explanation: ***Vitamin K and Vitamin D***
- All newborns should receive a prophylactic dose of **Vitamin K** to prevent **Vitamin K Deficiency Bleeding (VKDB)**, as placental transfer is poor and breast milk contains low levels.
- Breastfed infants, especially those exclusively breastfed, require **Vitamin D** supplementation (400 IU daily) to prevent **rickets**, as breast milk Vitamin D levels are often insufficient.
*Vitamin B6*
- While essential for development, **Vitamin B6** supplementation is not routinely recommended for all healthy newborns, especially those exclusively breastfed by a healthy mother.
- Deficiency in newborns is rare and typically associated with specific metabolic disorders or maternal malnutrition, which are not suggested here.
*Vitamin K*
- While **Vitamin K** is critically important for all newborns, it is only one of the essential vitamins needed for breastfed infants.
- Exclusive breastfeeding also necessitates **Vitamin D** supplementation, making this option incomplete.
*Folic acid*
- **Folic acid** (Vitamin B9) is crucial during pregnancy for preventing neural tube defects and is found in adequate amounts in breast milk for a healthy full-term infant.
- Routine supplementation of folic acid is not recommended for healthy newborns, as deficiency is rare.
*Vitamin D*
- While **Vitamin D** supplementation is essential for exclusively breastfed infants, this option is incomplete as it misses the critical need for **Vitamin K** prophylaxis at birth.
- Both vitamins are critical for newborn health in this scenario.
Fat-soluble vitamins (A, D, E, K) US Medical PG Question 2: A 48-year-old man comes to the emergency department because of a 1-hour history of heavy nasal bleeding. He drinks half a bottle of sherry daily. His pulse is 112/min, and blood pressure is 92/54 mm Hg. Physical examination shows scattered ecchymoses across the extremities and oozing from a venipuncture site. Laboratory studies show a prothrombin time of 28 seconds and a partial thromboplastin time of 36 seconds. Impaired function of which of the following proteins is the most likely cause of this patient's hemorrhage?
- A. Von Willebrand factor
- B. Protein S
- C. Epoxide reductase
- D. Prolyl hydroxylase
- E. Gamma-glutamyl carboxylase (Correct Answer)
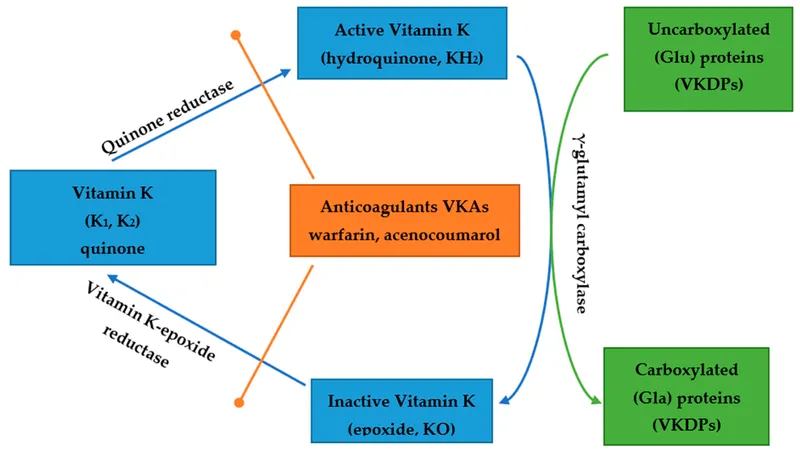
Fat-soluble vitamins (A, D, E, K) Explanation: ***Gamma-glutamyl carboxylase***
- This enzyme is crucial for the post-translational modification of vitamin K-dependent clotting factors (II, VII, IX, X, protein C, protein S) by adding a **gamma-carboxyglutamate** residue, which is essential for their function.
- Chronic alcohol abuse, suggested by drinking half a bottle of sherry daily, often leads to **hepatic dysfunction** and **nutritional deficiencies**, including vitamin K deficiency. Vitamin K deficiency impairs gamma-glutamyl carboxylase activity by depriving it of its essential cofactor (reduced vitamin K), leading to dysfunctional clotting factors. The prolonged **PT (extrinsic and common pathways)** and slightly prolonged **aPTT (intrinsic and common pathways)**, along with bleeding signs (epistaxis, ecchymoses, oozing from venipuncture), are consistent with this.
*Von Willebrand factor*
- Deficiency or dysfunction of **von Willebrand factor** primarily causes defects in **primary hemostasis**, leading to mucosal bleeding (like epistaxis) and increased bleeding time.
- However, it would typically not cause significant prolongation of both **PT** and **aPTT**, as it is not directly involved in the coagulation cascade measured by these tests.
*Protein S*
- **Protein S** is a natural anticoagulant and a cofactor for activated protein C, which inactivates factors Va and VIIIa.
- A deficiency would lead to a **procoagulant state**, increasing the risk of thrombosis, not a bleeding disorder like the one described.
*Epoxide reductase*
- **Vitamin K epoxide reductase (VKOR)** is responsible for recycling oxidized vitamin K back to its reduced form, which serves as the cofactor for gamma-glutamyl carboxylase.
- While VKOR dysfunction (e.g., by warfarin inhibition) would also lead to similar coagulation abnormalities, in the context of vitamin K deficiency from chronic alcoholism and malnutrition, the primary functional impairment occurs at the level of **gamma-glutamyl carboxylase**, which lacks its essential cofactor (reduced vitamin K) to perform the carboxylation reaction. This makes gamma-glutamyl carboxylase the most direct answer to the question of which protein's function is impaired.
*Prolyl hydroxylase*
- **Prolyl hydroxylase** is involved in the hydroxylation of proline residues, primarily in collagen synthesis.
- A deficiency or impaired function would lead to disorders like **scurvy** (due to vitamin C deficiency), which can cause bleeding due to fragile blood vessels, but it would not typically cause the specific pattern of prolonged **PT** and **aPTT** seen in this patient, which points directly to a defect in the coagulation cascade.
Fat-soluble vitamins (A, D, E, K) US Medical PG Question 3: A 10-year-old boy is brought into your clinic by his mother for sunburns that have not been healing. The mother states that he easily gets sunburned. The mother admits she gave birth to him at home and has never taken him to see a doctor. The patient walks with a wide stance gait and appears unstable on his feet. He has an extensive erythematous, scaling, hyperkeratotic rash on his face, neck, arms and legs. After extensive workup, the patient is found to have a genetic disorder that results in defective absorption of an important vitamin. Which of the following is likely to be low if measured?
- A. Vitamin K
- B. Niacin (Correct Answer)
- C. Folate
- D. Vitamin A
- E. Vitamin B12
Fat-soluble vitamins (A, D, E, K) Explanation: ***Niacin***
- The constellation of **sunburns that don't heal**, a **wide-stanced unstable gait**, and an **erythematous, scaling, hyperkeratotic rash** (consistent with dermatitis) strongly suggests **pellagra**.
- Pellagra is caused by a deficiency of **niacin (Vitamin B3)**, which is characterized by the "3 Ds": **dermatitis**, **diarrhea**, and **dementia (or neurological symptoms like ataxia)**.
*Vitamin K*
- Deficiency typically leads to **bleeding disorders** due to impaired coagulation, which is not indicated by the patient's symptoms.
- While newborns often receive a **vitamin K shot**, his current symptoms are unrelated to its deficiency.
*Folate*
- Folate deficiency primarily causes **megaloblastic anemia** and can lead to **neural tube defects** in developing fetuses.
- It does not explain the characteristic dermatological and neurological symptoms described.
*Vitamin A*
- Vitamin A deficiency is known to cause **night blindness** and **xerophthalmia** (dry eyes), and impaired immune function.
- While it plays a role in skin health, the specific rash and gait abnormalities point away from primary vitamin A deficiency.
*Vitamin B12*
- Deficiency leads to **megaloblastic anemia** with **neurological symptoms** such as peripheral neuropathy, but the dermatological manifestations (scaling, hyperkeratotic rash) and unhealing sunburn are not typical.
- The gait could be linked to neurological symptoms, but the overall presentation is better explained by niacin deficiency.
Fat-soluble vitamins (A, D, E, K) US Medical PG Question 4: A 38-year-old, working, first-time mother brings her 9-month-old male infant to the pediatrician for "wounds that simply won't heal" and bleeding gums. She exclaims, "I have been extra careful with him making sure to not let him get dirty, I boil his baby formula for 15 minutes each morning before I leave for work to give to the caregiver, and he has gotten all of his vaccinations." This infant is deficient in a molecule that is also an essential co-factor for which of the following reactions?
- A. Conversion of homocysteine to methionine
- B. Conversion of alpha ketoglutarate to succinyl-CoA
- C. Conversion of dopamine to norepinephrine (Correct Answer)
- D. Conversion of pyruvate to acetyl-CoA
- E. Conversion of pyruvate to oxaloacetate
Fat-soluble vitamins (A, D, E, K) Explanation: ***Conversion of dopamine to norepinephrine***
- The infant's symptoms of "wounds that simply won't heal" and **bleeding gums** are classic signs of **scurvy**, caused by a deficiency in **vitamin C (ascorbic acid)**.
- **Vitamin C** is an essential cofactor for **dopamine beta-hydroxylase**, the enzyme responsible for converting **dopamine to norepinephrine**.
*Conversion of homocysteine to methionine*
- This reaction is catalyzed by **methionine synthase**, which requires **vitamin B12** (cobalamin) and **folate (vitamin B9)** as cofactors.
- Deficiency in these vitamins would lead to **megaloblastic anemia** and neurological symptoms, not delayed wound healing and bleeding gums.
*Conversion of alpha ketoglutarate to succinyl-CoA*
- This step in the **Krebs cycle** is catalyzed by **alpha-ketoglutarate dehydrogenase**, which requires **thiamine (vitamin B1)**, **lipoic acid**, **Mg2+**, **NAD+**, and **FAD** as cofactors.
- Thiamine deficiency can cause **beriberi** or **Wernicke-Korsakoff syndrome**, not scurvy symptoms.
*Conversion of pyruvate to acetyl-CoA*
- This reaction is catalyzed by the **pyruvate dehydrogenase complex**, which requires **thiamine (vitamin B1)**, **lipoic acid**, **coenzyme A**, **FAD**, and **NAD+** as cofactors.
- A deficiency in any of these, particularly thiamine, leads to impaired carbohydrate metabolism and lactic acidosis.
*Conversion of pyruvate to oxaloacetate*
- This reaction is catalyzed by **pyruvate carboxylase**, which requires **biotin (vitamin B7)** as a cofactor and is essential for **gluconeogenesis**.
- Biotin deficiency is rare and can present with dermatitis, hair loss, and neurological symptoms, not the classic signs of scurvy.
Fat-soluble vitamins (A, D, E, K) US Medical PG Question 5: A 52-year-old man comes to the physician because of a 4-month history of fatigue, weakness, constipation, decreased appetite, and intermittent flank pain. He takes ibuprofen for knee and shoulder pain. Physical examination shows mild tenderness bilaterally in the costovertebral areas. His serum calcium concentration is 11.2 mg/dL, phosphorus concentration is 2.5 mg/dL, and N-terminal parathyroid hormone concentration is 830 pg/mL. Which of the following steps in vitamin D metabolism is most likely increased in this patient?
- A. Ergocalciferol → 25-hydroxyergocalciferol
- B. 7-dehydrocholesterol → cholecalciferol
- C. 25-hydroxycholecalciferol → 1,25-dihydroxycholecalciferol (Correct Answer)
- D. 25-hydroxycholecalciferol → 24,25-dihydroxycholecalciferol
- E. Cholecalciferol → 25-hydroxycholecalciferol
Fat-soluble vitamins (A, D, E, K) Explanation: ***25-hydroxycholecalciferol → 1,25-dihydroxycholecalciferol***
- This patient presents with **hypercalcemia** (11.2 mg/dL), **hypophosphatemia** (2.5 mg/dL), and a markedly **elevated N-terminal parathyroid hormone (PTH)** concentration (830 pg/mL), which are classic findings for **primary hyperparathyroidism**.
- In primary hyperparathyroidism, elevated PTH directly stimulates the **renal 1-alpha-hydroxylase enzyme**, increasing the conversion of **25-hydroxycholecalciferol** (calcidiol) to its active form, **1,25-dihydroxycholecalciferol** (calcitriol), which raises calcium levels.
*Ergocalciferol → 25-hydroxyergocalciferol*
- This step involves the **hepatic 25-hydroxylase enzyme** converting dietary vitamin D2 (ergocalciferol) to its storage form, which is not primarily regulated by PTH in the context of hyperparathyroidism.
- While essential for vitamin D activation, this conversion rate is usually adequate and not the primary increased step responsible for the hypercalcemic state in this patient's presentation.
*7-dehydrocholesterol → cholecalciferol*
- This process is the **cutaneous synthesis of vitamin D3 (cholecalciferol)**, which is dependent on UV light exposure and is not directly regulated by PTH.
- This initial step of vitamin D synthesis occurs in the skin and is upstream of the metabolic pathway influenced by PTH.
*25-hydroxycholecalciferol → 24,25-dihydroxycholecalciferol*
- This conversion produces an **inactive form of vitamin D** and is catalyzed by the **24-hydroxylase enzyme**.
- This enzyme activity is typically **suppressed by high PTH** and **increased by high levels of 1,25-dihydroxycholecalciferol**, serving to degrade excess active vitamin D; therefore, this step would likely be decreased, not increased, in primary hyperparathyroidism.
*Cholecalciferol → 25-hydroxycholecalciferol*
- This is the **hepatic 25-hydroxylation** of vitamin D3, producing 25-hydroxycholecalciferol (calcidiol), the major circulating form of vitamin D.
- While critical for producing the substrate for further activation, this step is not the *most likely increased* step in response to high PTH in primary hyperparathyroidism.
Fat-soluble vitamins (A, D, E, K) US Medical PG Question 6: A 6-month-old boy presents with decreased growth, pigmented retinopathy, hemolytic anemia, and peripheral neuropathy. You suspect that these signs are the result of a vitamin deficiency leading to increased oxidative damage to lipids. Which of the following is most likely responsible for this patient's symptoms?
- A. Excessive boiling of formula
- B. Goat milk ingestion
- C. Abetalipoproteinemia (Correct Answer)
- D. Pernicious anemia
- E. Hartnup disease
Fat-soluble vitamins (A, D, E, K) Explanation: ***Abetalipoproteinemia***
- This condition is characterized by a defect in **microsomal triglyceride transfer protein (MTP)**, leading to an inability to synthesize ApoB-containing lipoproteins.
- The resulting **malabsorption of fat and fat-soluble vitamins (especially vitamin E)** leads to the neurological symptoms (retinopathy, neuropathy) and hemolytic anemia due to increased oxidative stress on red blood cell membranes.
*Excessive boiling of formula*
- Excessive boiling of formula could potentially degrade some **heat-sensitive vitamins**, such as vitamin C or thiamine (B1).
- However, this is unlikely to cause a severe, combined deficiency leading to the specific constellation of symptoms seen, particularly the ophthalmologic and neurological signs related to **fat-soluble vitamin malabsorption**.
*Goat milk ingestion*
- Goat milk is naturally low in **folate** and **vitamin D** and can cause **folate deficiency anemia** and rickets if it's the sole source of nutrition for an infant.
- However, it does not typically cause the entire spectrum of symptoms described, particularly **pigmented retinopathy** and **peripheral neuropathy**, which are more indicative of **vitamin E deficiency**.
*Pernicious anemia*
- Pernicious anemia is caused by a deficiency in **intrinsic factor**, leading to **vitamin B12 malabsorption**.
- Symptoms primarily include **megaloblastic anemia**, **glossitis**, and **neurological deficits** (subacute combined degeneration of the spinal cord), but not pigmented retinopathy or hemolytic anemia due to increased fatty acid oxidation via vitamin E malabsorption.
*Hartnup disease*
- Hartnup disease is an inherited disorder of **amino acid transport**, specifically affecting the absorption of **neutral amino acids** like tryptophan.
- It leads to **niacin deficiency** (pellagra-like symptoms) and can cause skin rashes, ataxia, and psychiatric symptoms, but not hemolytic anemia or pigmented retinopathy.
Fat-soluble vitamins (A, D, E, K) US Medical PG Question 7: A 35-year-old female presents to her primary care physician complaining of right upper quadrant pain over the last 6 months. Pain is worst after eating and feels like intermittent squeezing. She also admits to lighter colored stools and a feeling of itchiness on her skin. Physical exam demonstrates a positive Murphy's sign. The vitamin level least likely to be affected by this condition is associated with which of the following deficiency syndromes?
- A. Rickets and osteomalacia
- B. Hemolytic anemia
- C. Night blindness
- D. Increased prothrombin time and easy bleeding
- E. Scurvy (Correct Answer)
Fat-soluble vitamins (A, D, E, K) Explanation: ***Scurvy***
- This condition is likely **cholestasis** due to common bile duct obstruction, given the RUQ pain after eating, light-colored stools, itchiness, and **positive Murphy's sign**.
- Cholestasis impairs the absorption of **fat-soluble vitamins** (A, D, E, K), but not **water-soluble vitamins** like vitamin C, which prevents scurvy.
*Rickets and osteomalacia*
- These conditions are caused by **vitamin D deficiency**, which is a **fat-soluble vitamin**.
- Impaired fat absorption in cholestasis would significantly impact vitamin D levels, leading to increased risk of rickets in children and osteomalacia in adults.
*Hemolytic anemia*
- This can be caused by **vitamin E deficiency**, a **fat-soluble vitamin**.
- Cholestasis impairs vitamin E absorption, which can lead to increased red blood cell fragility and hemolytic anemia.
*Night blindness*
- This is a classic symptom of **vitamin A deficiency**, which is a **fat-soluble vitamin**.
- Impaired fat absorption in cholestasis would reduce vitamin A uptake, contributing to night blindness.
*Increased prothrombin time and easy bleeding*
- These symptoms are indicative of **vitamin K deficiency**, a **fat-soluble vitamin**.
- Vitamin K is essential for the synthesis of clotting factors, and its absorption is severely hindered in cholestasis, leading to coagulopathies.
Fat-soluble vitamins (A, D, E, K) US Medical PG Question 8: A 4-year-old girl is brought to the physician for a routine checkup. She was recently adopted and has never seen a doctor before. The patient's parents state she was very emaciated when they adopted her and noticed she has trouble seeing in the evening. They also noted that she was experiencing profuse foul-smelling diarrhea as well, which is currently being worked up by a gastroenterologist. Her temperature is 97.8°F (36.6°C), blood pressure is 104/54 mmHg, pulse is 100/min, respirations are 19/min, and oxygen saturation is 98% on room air. The girl appears very thin. She has dry skin noted on physical exam. Laboratory studies are ordered as seen below.
Hemoglobin: 12 g/dL
Hematocrit: 36%
Leukocyte count: 4,500/mm^3 with normal differential
Platelet count: 191,000/mm^3
Serum:
Na+: 139 mEq/L
Cl-: 100 mEq/L
K+: 3.8 mEq/L
HCO3-: 28 mEq/L
BUN: 20 mg/dL
Glucose: 88 mg/dL
Creatinine: 0.7 mg/dL
Ca2+: 9.0 mg/dL
Which of the following findings is also likely to be seen in this patient?
- A. Xerophthalmia (Correct Answer)
- B. Cheilosis
- C. Ataxia
- D. Perifollicular hemorrhages
- E. Diarrhea
Fat-soluble vitamins (A, D, E, K) Explanation: **Xerophthalmia**
- The patient's history of **malnutrition** and **night blindness** strongly suggests **vitamin A deficiency**, which can lead to **xerophthalmia** (dry eyes and corneal damage).
- Her **foul-smelling diarrhea** indicates **fat malabsorption**, which impairs the absorption of fat-soluble vitamins, including **vitamin A**.
*Cheilosis*
- **Cheilosis** (cracking at the corners of the mouth) is primarily a symptom of **riboflavin (vitamin B2)** or **pyridoxine (vitamin B6)** deficiency.
- While the patient is malnourished, the specific symptoms point more directly to a fat-soluble vitamin deficiency.
*Ataxia*
- **Ataxia** (lack of voluntary coordination of muscle movements) is a neurological symptom associated with **vitamin B12** or **vitamin E deficiency**.
- While possible in severe malnutrition, it is not directly linked to the presented symptoms of night blindness and dry skin.
*Perifollicular hemorrhages*
- **Perifollicular hemorrhages** (small bruising especially around hair follicles) are characteristic of **scurvy**, caused by severe **vitamin C deficiency**.
- The patient's symptoms do not align with scurvy, which typically presents with bleeding gums, poor wound healing, and joint pain.
*Diarrhea*
- The patient is already described as experiencing **profuse foul-smelling diarrhea**, which is being worked up by a gastroenterologist.
- The question asks for an additional finding likely to be seen, not a symptom already present.
Fat-soluble vitamins (A, D, E, K) US Medical PG Question 9: A 68-year-old man comes to the physician because of fatigue and muscle cramps for the past 4 weeks. He has also noticed several episodes of tingling in both hands. He has not had fever or nausea. He has had a chronic cough for 10 years. He has chronic bronchitis, hypertension, and osteoarthritis of both knees. His father died from lung cancer. Current medications include salbutamol, ibuprofen, and ramipril. He has smoked 1 pack of cigarettes daily for 45 years. He is 175 cm (5 ft 9 in) tall and weighs 68 kg (163 lb); BMI is 22 kg/m2. His temperature is 36.7°C (98°F), pulse is 60/min, and blood pressure is 115/76 mm Hg. While measuring the patient's blood pressure, the physician observes carpopedal spasm. Cardiopulmonary examination shows no abnormalities. His hematocrit is 41%, leukocyte count is 5,800/mm3, and platelet count is 195,000/mm3. Serum alkaline phosphatase activity is 55 U/L. An ECG shows sinus rhythm with a prolonged QT interval. Which of the following is the most likely underlying cause of this patient's symptoms?
- A. Multiple endocrine neoplasia
- B. Ectopic hormone production
- C. Medication side effect
- D. Destruction of parathyroid glands
- E. Vitamin D deficiency (Correct Answer)
Fat-soluble vitamins (A, D, E, K) Explanation: ***Vitamin D deficiency***
- The patient's symptoms of **fatigue**, **muscle cramps**, **paresthesias** (tingling in hands), and **carpopedal spasm** (Trousseau's sign) are classic manifestations of **hypocalcemia**.
- The **prolonged QT interval** on ECG further confirms hypocalcemia.
- **Vitamin D deficiency** is the most common cause of hypocalcemia in elderly patients, especially those with:
- **Chronic disease** (chronic bronchitis)
- **Limited sun exposure** (likely given chronic illness)
- **Poor nutrition** or malabsorption
- **Normal alkaline phosphatase** (55 U/L) helps rule out severe bone disease
- This is the most likely diagnosis given the clinical presentation and demographic factors.
*Multiple endocrine neoplasia*
- **MEN syndromes** (MEN1, MEN2a) typically cause **primary hyperparathyroidism** with **hypercalcemia**, not hypocalcemia.
- There is no evidence of other endocrine tumors or family history to suggest MEN.
*Ectopic hormone production*
- **Ectopic PTHrP production** (e.g., from squamous cell lung carcinoma) causes **hypercalcemia**, not hypocalcemia.
- While the patient has smoking history and chronic cough, his presentation is clearly hypocalcemia.
*Medication side effect*
- The patient's current medications (**salbutamol**, **ibuprofen**, **ramipril**) are not commonly associated with symptomatic hypocalcemia.
- None of these medications typically cause carpopedal spasm or prolonged QT interval from calcium disturbances.
*Destruction of parathyroid glands*
- **Hypoparathyroidism** from parathyroid destruction (surgical, autoimmune, or infiltrative) would cause hypocalcemia.
- However, there is **no history** of neck surgery, radiation, or autoimmune disease.
- Without such history, this is less likely than vitamin D deficiency in an elderly patient with chronic disease.
Fat-soluble vitamins (A, D, E, K) US Medical PG Question 10: A 55-year-old man with a history of repeated hospitalization for chronic pancreatitis comes to the physician because of difficulty walking and standing steadily. Neurological examination shows an unsteady, broad-based gait, distal muscle weakness, decreased deep tendon reflexes, and an abnormal Romberg test. His hemoglobin concentration is 11.9 g/dL, mean corpuscular volume is 89/μm3, and serum lactate dehydrogenase is 105 U/L. His serum haptoglobin is slightly decreased. A deficiency of which of the following substances is the most likely cause of this patient's findings?
- A. Niacin
- B. Folate
- C. Phytomenadione
- D. Tocopherol (Correct Answer)
- E. Pyridoxine
Fat-soluble vitamins (A, D, E, K) Explanation: ***Tocopherol***
- **Tocopherol (Vitamin E)** deficiency can cause neurological symptoms such as **ataxia**, **distal muscle weakness**, decreased deep tendon reflexes, and an **abnormal Romberg test** due to its role in nerve function and antioxidant properties.
- **Chronic pancreatitis** often leads to **fat malabsorption** as pancreatic enzymes are crucial for fat digestion, which impairs the absorption of fat-soluble vitamins like Vitamin E.
*Niacin*
- **Niacin (Vitamin B3)** deficiency causes **pellagra**, characterized by the "3 Ds": **dermatitis**, **diarrhea**, and **dementia**, none of which are the primary presenting symptoms here.
- While neurological symptoms can occur in severe cases, the specific presentation of ataxia and peripheral neuropathy points away from pellagra.
*Folate*
- **Folate (Vitamin B9)** deficiency primarily causes **megaloblastic anemia** with an elevated **mean corpuscular volume (MCV)**, which is normal in this patient (MCV 89/μm3).
- While neurological symptoms can be present, they are less specific to folate deficiency compared to the classic presentation seen here.
*Phytomenadione*
- **Phytomenadione (Vitamin K)** deficiency leads to **coagulopathy** due to impaired synthesis of clotting factors, resulting in bleeding tendencies.
- It does not typically cause neurological symptoms like ataxia or peripheral neuropathy.
*Pyridoxine*
- **Pyridoxine (Vitamin B6)** deficiency can cause **peripheral neuropathy** and **ataxia**, but it's often associated with **sideroblastic anemia** or seizures.
- While some symptoms overlap, the strong history of chronic pancreatitis and fat malabsorption makes a fat-soluble vitamin deficiency more likely.
More Fat-soluble vitamins (A, D, E, K) US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.