Assessment of vitamin/mineral status US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Assessment of vitamin/mineral status. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Assessment of vitamin/mineral status US Medical PG Question 1: A 34-year-old female with a past medical history of a gastric sleeve operation for morbid obesity presents for pre-surgical clearance prior to a knee arthroplasty. Work-up reveals a hemoglobin of 8.7 g/dL, hematocrit of 26.1%, and MCV of 106 fL. With concern for folate deficiency, she is started on high dose folate supplementation, and her follow-up labs are as follows: hemoglobin of 10.1 g/dL, hematocrit of 28.5%, and MCV of 96 fL. Given her history of gastric sleeve surgery and associated malabsorption risks, she is at long-term risk for which complication?
- A. Peripheral neuropathy (Correct Answer)
- B. Macular degeneration
- C. Hypothyroidism
- D. Microcytic anemia
- E. Neural tube defects
Assessment of vitamin/mineral status Explanation: ***Peripheral neuropathy***
- Gastric sleeve surgery can lead to **vitamin B12 deficiency** due to the removal of the fundus, which produces **intrinsic factor** necessary for B12 absorption.
- **Vitamin B12 deficiency** is a known cause of **peripheral neuropathy**, manifesting as numbness, tingling, and weakness.
*Macular degeneration*
- This condition is primarily associated with **aging**, **genetics**, and **environmental factors** like smoking, rather than micronutrient deficiencies post-gastric sleeve.
- While certain vitamins (e.g., A, C, E) and minerals can influence macular health, there's no direct strong causal link between bariatric surgery malabsorption and increased risk of **macular degeneration**.
*Hypothyroidism*
- Hypothyroidism is most commonly caused by **autoimmune conditions** like Hashimoto's thyroiditis or **iodine deficiency**.
- While bariatric surgery can influence overall metabolic health, it does not directly lead to an increased risk of primary hypothyroidism.
*Microcytic anemia*
- **Microcytic anemia** is characterized by **small red blood cells (low MCV)**, typically caused by **iron deficiency** or **thalassemia**.
- The patient initially presented with **macrocytic anemia (MCV 106 fL)**, which improved with folate, but the underlying risk remains for macrocytic rather than microcytic anemia from malabsorption of B12 or folate.
*Neural tube defects*
- **Neural tube defects** are congenital anomalies that occur during early fetal development, primarily linked to **folate deficiency during pregnancy**.
- While the patient had a folate deficiency, this complication is relevant to **fetal development** and not a long-term risk for the adult patient herself after surgery.
Assessment of vitamin/mineral status US Medical PG Question 2: A 35-year-old woman comes to the physician because of a 1-day history of swelling and pain in the left leg. Two days ago, she returned from a business trip on a long-distance flight. She has alcohol use disorder. Physical examination shows a tender, swollen, and warm left calf. Serum studies show an increased homocysteine concentration and a methylmalonic acid concentration within the reference range. Further evaluation of this patient is most likely to show which of the following serum findings?
- A. Decreased cobalamin concentration
- B. Decreased protein C concentration
- C. Increased fibrinogen concentration
- D. Decreased folate concentration (Correct Answer)
- E. Increased pyridoxine concentration
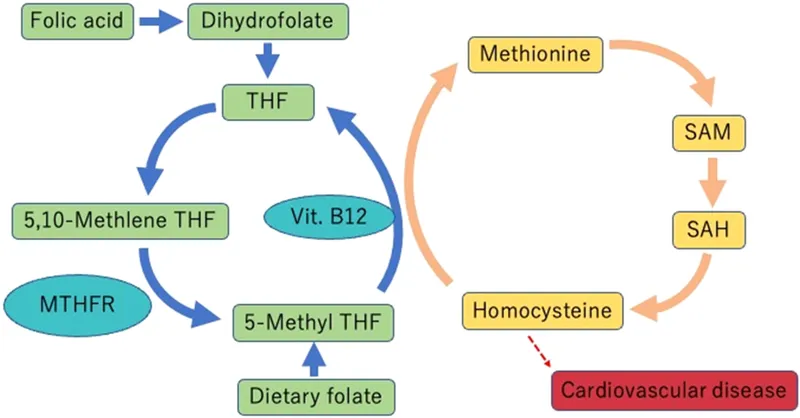
Assessment of vitamin/mineral status Explanation: ***Decreased folate concentration***
- The patient's presentation with **pain and swelling in the left leg following a long flight** suggests a **deep vein thrombosis (DVT)**. Increased homocysteine levels are a risk factor for DVT.
- Alcohol use disorder often leads to **malabsorption and poor nutritional intake**, profoundly affecting **folate metabolism** and leading to **folate deficiency**. This deficiency is a common cause of **hyperhomocysteinemia**, especially when methylmalonic acid levels are normal (ruling out B12 deficiency as the primary cause of hyperhomocysteinemia).
*Decreased cobalamin concentration*
- While alcohol use disorder can decrease **cobalamin (vitamin B12) concentration**, the **normal methylmalonic acid (MMA) concentration** in this patient makes a significant B12 deficiency unlikely to be the cause of the elevated homocysteine.
- Elevated MMA is a more specific indicator of **cobalamin deficiency**, as B12 is a cofactor for the enzyme that converts methylmalonyl-CoA to succinyl-CoA.
*Decreased protein C concentration*
- Decreased protein C concentration is a **thrombophilic condition** that increases the risk of DVT, but there is no direct evidence in the patient's history or lab results pointing specifically to this deficiency.
- While hereditary thrombophilias can contribute, a **primary nutritional deficiency** explains the constellation of findings better in this context.
*Increased fibrinogen concentration*
- **Fibrinogen** is an **acute-phase reactant** and would likely be elevated in the context of inflammation or thrombosis, but it is not directly linked to the patient's hyperhomocysteinemia due to alcohol use disorder.
- Elevated fibrinogen is a **consequence** of the thrombotic process, not typically a direct cause of the hyperhomocysteinemia in this scenario.
*Increased pyridoxine concentration*
- **Pyridoxine (vitamin B6) levels** are generally not increased in individuals with alcohol use disorder; in fact, chronic alcohol abuse can lead to **pyridoxine deficiency**.
- Pyridoxine is a cofactor in homocysteine metabolism, and deficiency can lead to elevated homocysteine, but an *increase* is not expected.
Assessment of vitamin/mineral status US Medical PG Question 3: A 70-year-old woman presents to the office for a yearly physical. She states she has recently started experiencing pain in her legs and her back. Last year, she experienced a fracture of her left arm while trying to lift groceries. The patient states that she does not consume any dairy and does not go outside often because of the pain in her legs and back. Of note, she takes carbamazepine for seizures. On exam, her vitals are within normal limits. You suspect the patient might have osteomalacia. Testing for which of the following is the next best step to confirm your suspicion?
- A. Vitamin D2 (ergocalciferol)
- B. 25-hydroxyvitamin D (Correct Answer)
- C. Pre-vitamin D3
- D. 1,25-hydroxyvitamin D
- E. 7-dehydrocholesterol
Assessment of vitamin/mineral status Explanation: ***25-hydroxyvitamin D***
- This is the **best initial test** for evaluating vitamin D deficiency, which leads to **osteomalacia**.
- It reflects the circulating levels of vitamin D and is the **most accurate indicator** of the body's vitamin D stores.
*Vitamin D2 (ergocalciferol)*
- While D2 is a form of vitamin D, measuring only D2 levels is **not sufficient** to assess overall vitamin D status.
- The standard test measures total circulating vitamin D, which includes both D2 and D3, but specifically **25-hydroxyvitamin D** reflects the active usable form.
*Pre-vitamin D3*
- **Pre-vitamin D3** is a precursor molecule formed in the skin from 7-dehydrocholesterol upon UV exposure, and it rapidly isomerizes to vitamin D3.
- It is **not a stable measurable form** in the blood for assessing vitamin D status or diagnosing osteomalacia.
*1,25-hydroxyvitamin D*
- This is the **active hormonal form of vitamin D**, primarily regulated by parathyroid hormone (PTH) and kidney function.
- Levels can be normal or even elevated in early vitamin D deficiency due to increased PTH, making it **less reliable** for initial assessment of deficiency.
*7-dehydrocholesterol*
- **7-dehydrocholesterol** is a precursor molecule in the skin that is converted to pre-vitamin D3 by UV radiation.
- Measuring this precursor is **not clinically significant** for diagnosing osteomalacia or assessing vitamin D deficiency.
Assessment of vitamin/mineral status US Medical PG Question 4: A 37-year-old man is brought to the emergency department because he was found down on a city sidewalk. Upon presentation he is found to be disheveled with multiple poorly healed wounds on his hands and feet. He has had dozens of previous presentations for alcohol intoxication and is currently known to be homeless. Physical examination reveals multiple minor wounds, alopecia, and decreased axillary hair. Upon being aroused, the patient reveals that he has had difficulty with taste and smell and has also had severe diarrhea over the last week. The deficient substance most likely responsible for this patient's symptoms is associated with which of the following proteins?
- A. Tyrosinase
- B. Hemoglobin
- C. Glutathione peroxidase
- D. RNA polymerase (Correct Answer)
- E. Thyroid hormone
Assessment of vitamin/mineral status Explanation: ***Correct: RNA polymerase***
* The clinical presentation of **poorly healed wounds, alopecia, decreased axillary hair, dysgeusia/anosmia, and diarrhea** in a homeless patient with chronic alcoholism is classic for **zinc deficiency**.
* **Zinc is an essential cofactor for RNA polymerase**, the enzyme responsible for DNA transcription and ultimately protein synthesis. Zinc deficiency impairs cellular proliferation and protein synthesis, which explains the poor wound healing, hair loss, and other manifestations.
* Zinc is also a cofactor for over 300 enzymes including alkaline phosphatase, carbonic anhydrase, superoxide dismutase, and various matrix metalloproteinases critical for wound healing and tissue maintenance.
*Incorrect: Glutathione peroxidase*
* **Glutathione peroxidase requires SELENIUM, not zinc**, as its essential cofactor. This enzyme protects against oxidative damage by reducing hydrogen peroxide.
* Selenium deficiency presents with **cardiomyopathy (Keshan disease), myopathy, and thyroid dysfunction**, not the constellation of symptoms seen in this patient.
*Incorrect: Tyrosinase*
* **Tyrosinase is a copper-dependent enzyme** involved in melanin synthesis. Copper deficiency causes **anemia, neutropenia, and neurological symptoms** (myelopathy), not the dermatologic and sensory changes seen here.
* While copper deficiency can occur in alcoholism, the specific symptoms of taste/smell disturbances and characteristic skin findings point to zinc deficiency.
*Incorrect: Thyroid hormone*
* Thyroid hormone synthesis requires **iodine**, not zinc. Hypothyroidism presents with **fatigue, weight gain, cold intolerance, and bradycardia**.
* The patient's acute presentation with diarrhea, taste/smell disturbances, and poor wound healing does not fit thyroid dysfunction.
*Incorrect: Hemoglobin*
* Hemoglobin requires **iron** for oxygen transport. Iron deficiency causes **microcytic anemia with fatigue, pallor, and koilonychia**.
* While chronic alcoholics may develop anemia (often macrocytic from folate/B12 deficiency), the specific symptoms of dysgeusia, anosmia, and characteristic dermatologic findings indicate zinc deficiency as the primary issue.
Assessment of vitamin/mineral status US Medical PG Question 5: A 60-year-old woman presents to the physician because of shortness of breath and easy fatigability over the past 3 months. Her symptoms become worse with physical activity. She notes no chest pain, cough, or wheezing. Her last menstrual period was 10 years ago. She currently takes calcium and vitamin D supplements as well as a vaginal estrogen cream. For several years, her diet has been poor, as she often does not feel like eating. The patient’s medical history is otherwise unremarkable. She works as a piano teacher at the local community center. She does not use tobacco or illicit drugs and enjoys an occasional glass of red wine with dinner. Her vital signs include: pulse 100/min, respiratory rate 16/min, and blood pressure 140/84 mm Hg. Physical examination reveals impaired vibratory sensation in the legs. Pallor is evident on her hands. Which of the following laboratory tests is expected to be abnormal in this patient?
- A. Serum methylmalonic acid level (Correct Answer)
- B. Erythrocyte pyruvate kinase activity
- C. Erythrocyte glutathione reductase activity
- D. Serum folate level
- E. Serum protoporphyrin level
Assessment of vitamin/mineral status Explanation: ***Serum methylmalonic acid level***
- The patient's symptoms of **shortness of breath**, **fatigability**, **pallor**, and **impaired vibratory sensation** suggest **vitamin B12 deficiency**, which leads to **megaloblastic anemia** and **neurological deficits**.
- **Vitamin B12** is a cofactor for the enzyme **methylmalonyl-CoA mutase**. A deficiency leads to the accumulation of **methylmalonic acid (MMA)**, making an elevated serum MMA level an expected abnormal finding.
*Erythrocyte pyruvate kinase activity*
- **Pyruvate kinase deficiency** is a rare cause of **hemolytic anemia**, which presents as chronic anemia, jaundice, and splenomegaly.
- The symptoms in this patient are more consistent with a **nutritional deficiency**, not a genetic enzymatic defect.
*Erythrocyte glutathione reductase activity*
- **Glutathione reductase deficiency** can impair the erythrocyte's ability to handle **oxidative stress**, potentially causing **hemolytic anemia**.
- This deficiency is less common and symptoms like impaired vibratory sensation are not characteristic.
*Serum folate level*
- While **folate deficiency** can also cause **megaloblastic anemia** with symptoms like fatigue and pallor, it does not typically cause **neurological symptoms** such as impaired vibratory sensation.
- The neurological signs strongly point towards **vitamin B12 deficiency**, which causes elevated MMA, whereas folate deficiency would show a low serum folate level.
*Serum protoporphyrin level*
- An elevated **serum protoporphyrin level** can indicate **iron deficiency anemia** or **lead poisoning**.
- While iron deficiency can cause fatigue and pallor, it typically does not cause neurological symptoms like impaired vibratory sensation, which is a hallmark of B12 deficiency.
Assessment of vitamin/mineral status US Medical PG Question 6: An exclusively breast-fed, 4-month-old boy is brought to the physician by his mother for a routine examination. He was born at term and delivery was uncomplicated. He received all standard treatment and testing prior to being discharged from the hospital. Examination shows no abnormalities. Without receiving additional supplementation at this time, this infant is at greatest risk of developing which of the following conditions?
- A. Intracranial bleed
- B. Microcytic anemia (Correct Answer)
- C. Rickets
- D. Scaly dermatitis
- E. Peripheral neuropathy
Assessment of vitamin/mineral status Explanation: ***Microcytic anemia***
- Exclusively breastfed infants are at risk for **iron deficiency anemia** because breast milk contains low levels of iron (~0.3 mg/L), and newborn iron stores are typically depleted by **4-6 months of age**.
- At 4 months, iron stores are beginning to deplete, and iron supplementation is typically initiated around this time; without supplementation, the infant is at greatest risk for developing **microcytic anemia** due to impaired hemoglobin synthesis.
- Iron deficiency causes red blood cells to be small (microcytic) and pale (hypochromic).
*Intracranial bleed*
- An intracranial bleed in an otherwise healthy infant is most commonly associated with **vitamin K deficiency bleeding (VKDB)**.
- However, the infant received **standard treatment** at birth, which includes vitamin K prophylaxis (typically 1 mg IM), making this highly unlikely.
*Rickets*
- Rickets is caused by **vitamin D deficiency**, leading to impaired bone mineralization.
- While breast milk is deficient in vitamin D, the **AAP recommends vitamin D supplementation (400 IU/day)** for all breastfed infants starting shortly after birth, which is part of standard care and would prevent rickets.
- No bone abnormalities are noted on examination.
*Scaly dermatitis*
- Scaly dermatitis, such as **seborrheic dermatitis (cradle cap)**, is common and physiological in infants but is not directly linked to a specific nutritional deficiency from exclusive breastfeeding.
- Severe, generalized scaly dermatitis could indicate **zinc deficiency** or **essential fatty acid deficiency**, but this is rare in otherwise healthy, exclusively breastfed term infants.
*Peripheral neuropathy*
- Peripheral neuropathy in infants can be caused by genetic, metabolic, or toxic conditions.
- It is **not** a common complication associated with exclusive breastfeeding in an otherwise healthy term infant.
Assessment of vitamin/mineral status US Medical PG Question 7: A 3-year-old African-American female presents to the emergency department with fatigue. Her parents endorse malaise and weakness on behalf of the patient for two weeks. Her temperature is 98.9°F (37.2°C), blood pressure is 94/70 mmHg, pulse is 102/min, and respirations are 22/min. On physical exam, she is tired-appearing with conjunctival pallor. Her parents report that they immigrated from Liberia before the patient was born. They deny any family history of medical disorders, and the patient has no sick contacts at home.
Laboratory tests are performed and reveal the following:
Leukocyte count: 10,700/mm^3
Hemoglobin: 8.6 g/dL
Hematocrit: 24%
Mean corpuscular volume: 84 µm^3
Platelet count: 488,000/mm^3
Reticulocyte index: 3.8%
The patient should receive which of the following nutritional supplements?
- A. Vitamin D
- B. Vitamin B9 (Correct Answer)
- C. Iron
- D. Vitamin B6
- E. Vitamin B12
Assessment of vitamin/mineral status Explanation: ***Vitamin B9 (Folate)***
- The **elevated reticulocyte index of 3.8%** (normal <2%) indicates active bone marrow compensation for red blood cell destruction, suggesting **hemolytic anemia** rather than nutritional deficiency causing impaired production.
- The patient's **normocytic anemia** (MCV 84 µm³ is normal for a 3-year-old) with elevated reticulocyte count and **reactive thrombocytosis** (platelets 488,000) are classic features of chronic hemolysis.
- The **African-American ethnicity and Liberian ancestry** raise suspicion for inherited hemolytic conditions such as **G6PD deficiency or sickle cell disease**, both common in this population.
- In **chronic hemolytic states**, there is increased folate demand due to accelerated RBC turnover and erythropoiesis. **Folic acid supplementation** is routinely recommended to prevent megaloblastic crisis.
*Iron*
- Iron deficiency would present with **low reticulocyte count** (inadequate bone marrow response) and eventual **microcytic anemia** (MCV <80 in children), not the normocytic anemia with elevated reticulocytes seen here.
- The elevated reticulocyte index indicates the bone marrow is functioning well with adequate iron stores to produce new RBCs in response to hemolysis.
- Reactive thrombocytosis can occur in iron deficiency, but the elevated reticulocyte index makes this diagnosis unlikely.
*Vitamin B12*
- Vitamin B12 deficiency causes **macrocytic anemia** (MCV >100 µm³) with **low reticulocyte count** due to ineffective erythropoiesis.
- The patient's normocytic indices and elevated reticulocyte count are inconsistent with B12 deficiency.
- B12 deficiency is rare in young children without specific risk factors (strict vegan diet, malabsorption, pernicious anemia).
*Vitamin B6*
- Vitamin B6 deficiency can cause **sideroblastic anemia** (microcytic with ringed sideroblasts), typically with **low reticulocyte count**.
- This is extremely rare in children and usually associated with specific medications (isoniazid) or genetic disorders.
- The elevated reticulocyte response rules out a nutritional deficiency causing impaired RBC production.
*Vitamin D*
- Vitamin D deficiency affects **bone metabolism** (causing rickets in children) but does not directly cause anemia or affect erythropoiesis.
- While vitamin D may have indirect effects on hematopoiesis, it is not the primary treatment for anemia of any type.
Assessment of vitamin/mineral status US Medical PG Question 8: A 58-year-old man presents to the Emergency Department after 3 hours of intense suprapubic pain associated with inability to urinate for the past day or two. His medical history is relevant for benign prostatic hyperplasia (BPH) that has been under treatment with prazosin and tadalafil. Upon admission, he is found to have a blood pressure of 180/100 mm Hg, a pulse of 80/min, a respiratory rate of 23/min, and a temperature of 36.5°C (97.7°F). He weighs 84 kg (185.1 lb) and is 175 cm (5 ft 7 in) tall. Physical exam, he has suprapubic tenderness. A bladder scan reveals 700 ml of urine. A Foley catheter is inserted and the urine is drained. Initial laboratory tests and their follow up 8 hours after admission are shown below.
Admission 8 hours after admission
Serum potassium 4.2 mmol/L Serum potassium 4.0 mmol/L
Serum sodium 140 mmol/L Serum sodium 142 mmol/L
Serum chloride 102 mmol/L Serum chloride 110 mmol/L
Serum creatinine 1.4 mg/dL Serum creatinine 1.6 mg/dL
Serum blood urea nitrogen 64 mg/dL Serum blood urea nitrogen 62 mg/dL
Urine output 250 mL Urine output 260 mL
A senior attending suggests a consultation with Nephrology. Which of the following best justifies this suggestion?
- A. Estimated glomerular filtration rate (eGFR)
- B. Urine output (Correct Answer)
- C. Serum creatinine (SCr)
- D. Serum blood urea nitrogen (BUN)
- E. Serum potassium
Assessment of vitamin/mineral status Explanation: ***Urine output***
- The patient's **urine output is severely reduced** at 260 mL over 8 hours (approximately **32.5 mL/hour**), which constitutes **oliguria** (defined as <0.5 mL/kg/hr; this patient at 84 kg should produce ≥42 mL/hr).
- Despite **relief of the post-renal obstruction** via Foley catheterization, the persistent oliguria indicates **intrinsic kidney injury** rather than simple mechanical obstruction.
- The combination of **oliguria persisting after decompression** + **rising serum creatinine** (1.4→1.6 mg/dL) meets **KDIGO criteria for Stage 2 AKI** (urine output <0.5 mL/kg/hr for ≥12 hours).
- This requires **urgent nephrology consultation** to assess for acute tubular necrosis (ATN), guide fluid management during potential post-obstructive diuresis, and consider renal replacement therapy if oliguria worsens.
*Serum creatinine (SCr)*
- The serum creatinine **rose from 1.4 to 1.6 mg/dL** despite bladder decompression, which is concerning and suggests intrinsic renal injury.
- However, creatinine is a **lagging indicator** of kidney function - it takes 24-48 hours to reflect acute changes in GFR, whereas **urine output is a real-time indicator** of kidney function.
- While the rising creatinine supports the need for nephrology involvement, **urine output is the more immediate and actionable parameter** that prompted the attending's suggestion at this early time point.
*Estimated glomerular filtration rate (eGFR)*
- eGFR is **calculated from serum creatinine** using equations that assume steady-state conditions, which **do not apply in acute kidney injury**.
- In the **acute setting with rapidly changing kidney function**, eGFR calculations are unreliable and can significantly overestimate or underestimate true GFR.
- Clinicians rely more on **urine output and serial creatinine measurements** rather than eGFR when managing AKI.
*Serum blood urea nitrogen (BUN)*
- The BUN decreased slightly from 64 to 62 mg/dL, remaining elevated but showing minimal change after catheterization.
- Elevated BUN can reflect **pre-renal azotemia, dehydration, or upper GI bleeding** and is less specific for intrinsic kidney injury than oliguria.
- The **BUN:Cr ratio** is approximately 40:1 (64/1.6), suggesting a **pre-renal component**, but this alone doesn't justify urgent nephrology consultation as strongly as the persistent oliguria does.
*Serum potassium*
- Serum potassium levels remain **normal** (4.2→4.0 mmol/L) and do not indicate a metabolic emergency.
- While **hyperkalemia** is a common complication of AKI that would warrant nephrology involvement, this patient's potassium is well-controlled and not the driving concern at this time.
Assessment of vitamin/mineral status US Medical PG Question 9: An 82-year-old woman is brought to the emergency room after her neighbor saw her fall in the hallway. She lives alone and remarks that she has been feeling weak lately. Her diet consists of packaged foods and canned meats. Her temperature is 97.6°F (36.4°C), blood pressure is 133/83 mmHg, pulse is 95/min, respirations are 16/min, and oxygen saturation is 98% on room air. Physical exam is notable for a weak, frail, and pale elderly woman. Laboratory studies are ordered as seen below.
Hemoglobin: 9.1 g/dL
Hematocrit: 30%
Leukocyte count: 6,700/mm^3 with normal differential
Platelet count: 199,500/mm^3
MCV: 110 fL
Which of the following is the most likely deficiency?
- A. Zinc
- B. Vitamin B12
- C. Thiamine
- D. Niacin
- E. Folate (Correct Answer)
Assessment of vitamin/mineral status Explanation: ***Folate***
- The patient's **macrocytic anemia** (MCV 110 fL, hemoglobin 9.1 g/dL) combined with a diet of **packaged foods and canned meats** with **no fresh fruits or vegetables** strongly suggests folate deficiency.
- **Folate is found exclusively in fresh produce** (leafy greens, fruits, legumes), which is completely absent from this patient's diet.
- **Elderly individuals** living alone with inadequate nutrition are at particularly high risk for **folate deficiency**.
*Vitamin B12*
- While vitamin B12 deficiency also causes **macrocytic anemia**, her diet includes **canned meats which retain B12** (heat-stable vitamin).
- B12 deficiency typically requires years to develop due to large hepatic stores, and often presents with **neurological manifestations** (subacute combined degeneration, peripheral neuropathy), which are absent here.
- The dietary pattern makes folate deficiency more likely than B12 deficiency.
*Zinc*
- Zinc deficiency causes impaired immune function, delayed wound healing, skin lesions, and **taste disturbances**, but **not macrocytic anemia**.
- No clinical or laboratory findings suggest zinc deficiency.
*Thiamine*
- Thiamine (vitamin B1) deficiency causes **Wernicke-Korsakoff syndrome** or **beriberi** (wet or dry), presenting with neurological symptoms, heart failure, or peripheral neuropathy.
- Thiamine deficiency does **not cause macrocytic anemia**.
*Niacin*
- Niacin (vitamin B3) deficiency causes **pellagra**, characterized by the \"3 D's\": **dermatitis, diarrhea, and dementia**.
- Niacin deficiency is **not associated with macrocytic anemia**.
Assessment of vitamin/mineral status US Medical PG Question 10: Myeloperoxidase (MPO) is a heme-containing molecule that is found in the azurophilic granules of neutrophils. Upon release, the enzyme catalyzes hypochlorous acid production during the phagocytic response. In the setting of pneumonia, which of the following clinical findings is most directly associated with myeloperoxidase activity?
- A. Shortness of breath
- B. Green color of sputum (Correct Answer)
- C. Rust-tinged sputum
- D. Cough
- E. Fever
Assessment of vitamin/mineral status Explanation: ***Green color of sputum***
- Myeloperoxidase contributes to the **greenish color of sputum** due to its heme content and enzymatic activity, which involves the formation of a green pigment during the oxidation of chloride ions.
- In pneumonia, activated neutrophils release myeloperoxidase as part of the immune response, leading to the characteristic **greenish discoloration** often observed in a patient's sputum.
*Shortness of breath*
- Shortness of breath, or **dyspnea**, is a common symptom of pneumonia reflecting impaired gas exchange and increased work of breathing.
- It is a **physiological response** to lung inflammation and consolidation, not a direct end result of myeloperoxidase activity.
*Rust-tinged sputum*
- **Rust-tinged sputum** is classically associated with **Streptococcus pneumoniae** pneumonia and is due to the breakdown of red blood cells and the presence of hemoglobin metabolites.
- While it indicates an infection, it is not directly linked to the enzymatic action or color of myeloperoxidase itself.
*Cough*
- **Cough** is a vital **protective reflex** in pneumonia, aiming to clear respiratory secretions and foreign material from the airways.
- It is a symptom of airway irritation and inflammation, rather than a direct visual outcome of biochemical reactions involving myeloperoxidase.
*Fever*
- **Fever** is a systemic manifestation of the body's generalized **inflammatory response** to infection, mediated by pyrogens.
- It is a non-specific symptom indicating an active infection, not a direct consequence of myeloperoxidase activity or its visual manifestation.
More Assessment of vitamin/mineral status US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.