Overview and purpose of urea cycle US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Overview and purpose of urea cycle. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Overview and purpose of urea cycle US Medical PG Question 1: A 3-week old boy is brought to the physician for the evaluation of lethargy, recurrent vomiting, and poor weight gain since birth. Physical examination shows decreased skin turgor and a bulging frontal fontanelle. Serum studies show an ammonia concentration of 170 μmol/L (N < 30) and low serum citrulline levels. The oral intake of which of the following nutrients should be restricted in this patient?
- A. Gluten
- B. Lactose
- C. Fructose
- D. Protein (Correct Answer)
- E. Vitamin A
Overview and purpose of urea cycle Explanation: ***Protein***
- Elevated **ammonia** and low **citrulline** levels indicate a **urea cycle disorder**, which impairs the body's ability to excrete nitrogenous waste from protein metabolism.
- Restricting **protein intake** limits the production of ammonia, thereby reducing the toxic burden on the system and preventing further neurological damage.
*Gluten*
- **Gluten restriction** is primarily indicated for **celiac disease**, which presents with gastrointestinal symptoms like diarrhea, malabsorption, and poor weight gain, but not directly with hyperammonemia or urea cycle dysfunction.
- While malabsorption can cause poor weight gain, the specific metabolic derangements here point away from celiac disease.
*Lactose*
- **Lactose intolerance** or **galactosemia** would necessitate **lactose restriction**. Symptoms usually include vomiting, diarrhea, and failure to thrive, but they do not typically present with the extreme hyperammonemia seen here.
- Galactosemia specifically would show elevated galactose and galactose-1-phosphate, not ammonia.
*Fructose*
- **Hereditary fructose intolerance** requires **fructose restriction**. It generally presents with vomiting, hypoglycemia, and liver dysfunction (jaundice, hepatomegaly) upon exposure to fructose, not primarily with hyperammonemia.
- The metabolic pathway for fructose metabolism does not directly generate ammonia in the quantities seen with urea cycle disorders.
*Vitamin A*
- **Vitamin A restriction** is not a primary treatment for any known inborn error of metabolism or hyperammonemia.
- While deficiencies or toxicities of vitamins can occur, they do not present with the specific metabolic profile described (high ammonia, low citrulline).
Overview and purpose of urea cycle US Medical PG Question 2: A 2-week-old boy presents to the emergency department because of unusual irritability and lethargy. The patient is admitted to the pediatric intensive care unit and minutes later develops metabolic encephalopathy. This progressed to a coma, followed by death before any laboratory tests are completed. The infant was born at home via vaginal delivery at 39 weeks' of gestation. His mother says that the symptoms started since the infant was 4-days-old, but since he only seemed ‘tired’, she decided not to seek medical attention. Further testing during autopsy shows hyperammonemia, low citrulline, and increased orotic acid. Which of the following enzymes is most likely deficient in this patient?
- A. Branched-chain alpha-ketoacid dehydrogenase
- B. Propionyl-CoA carboxylase
- C. Homogentisic acid dioxygenase
- D. Ornithine transcarbamylase (Correct Answer)
- E. Cystathionine beta-synthase
Overview and purpose of urea cycle Explanation: **Ornithine transcarbamylase**
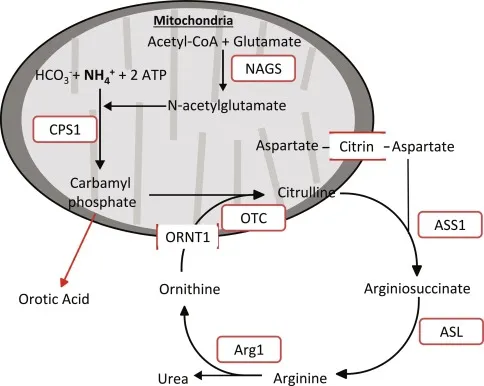
- **Hyperammonemia**, **low citrulline**, and **increased orotic acid** are classic findings in **Ornithine Transcarbamylase (OTC) deficiency**. OTC is an X-linked urea cycle disorder.
- The rapid progression to **metabolic encephalopathy** and death in a neonate with these laboratory findings is highly characteristic of severe OTC deficiency, often presenting in the first few days of life.
*Branched-chain alpha-ketoacid dehydrogenase*
- Deficiency of this enzyme causes **Maple Syrup Urine Disease**, characterized by elevated **branched-chain amino acids** and their corresponding ketoacids in blood and urine.
- While it can cause neurological symptoms, it does not typically present with the specific constellation of **hyperammonemia**, low citrulline, and high orotic acid.
*Propionyl-CoA carboxylase*
- Deficiency of this enzyme leads to **Propionic acidemia**, a type of organic acidemia, characterized by **propionic acid accumulation** and often **metabolic acidosis**, ketosis, and hyperammonemia.
- However, it would not typically cause **low citrulline** or isolated **elevated orotic acid** as seen in urea cycle disorders.
*Homogentisic acid dioxygenase*
- Deficiency of this enzyme causes **Alkaptonuria**, an inborn error of metabolism characterized by the accumulation of **homogentisic acid**.
- This condition is usually benign in infancy, with symptoms appearing later in life such as **dark urine** on standing and **ochronosis** (darkening of cartilage). It does not present with acute hyperammonemia or metabolic encephalopathy.
*Cystathionine beta-synthase*
- Deficiency of this enzyme causes **homocystinuria**, an inborn error of methionine metabolism, leading to elevated **homocysteine** and methionine.
- Clinical features include **ectopia lentis**, skeletal abnormalities, and intellectual disability, but not usually acute neonatal hyperammonemia or the specific findings of low citrulline and high orotic acid.
Overview and purpose of urea cycle US Medical PG Question 3: A 20-year-old male presents with confusion, asterixis, and odd behavior. Very early in the morning, his mother found him urinating on the floor of his bedroom. A detailed history taken from the mother revealed that he has been a vegetarian his entire life but decided to "bulk up" by working out and consuming whey protein several times a day. A blood test revealed increased levels of ammonia and orotic acid but a decreased BUN. The patient began hemodialysis and was given oral sodium benzoate and phenylbutyrate, which improved his condition. Gene therapy of the enzyme producing which product would correct his condition?
- A. Citrulline (Correct Answer)
- B. Fructose-1-phosphate
- C. Homocysteine
- D. Phenylalanine
- E. Uridine monophosphate
Overview and purpose of urea cycle Explanation: ***Citrulline***
- The clinical presentation (confusion, asterixis, bizarre behavior, high ammonia, low BUN, high orotic acid, improvement with sodium benzoate and phenylbutyrate) is classic for a **urea cycle disorder**, specifically **ornithine transcarbamylase (OTC) deficiency**.
- OTC catalyzes the conversion of ornithine and carbamoyl phosphate to citrulline. A deficiency in OTC leads to a buildup of carbamoyl phosphate, which is then shunted to the pyrimidine synthesis pathway, leading to increased orotic acid. Therefore, gene therapy for the enzyme producing citrulline (OTC) would address the underlying defect.
*Fructose-1-phosphate*
- This is an intermediate in **fructose metabolism**. Disorders related to this, such as **hereditary fructose intolerance**, are not associated with hyperammonemia or orotic aciduria in this manner.
- Symptoms typically involve hypoglycemia, vomiting, and liver dysfunction upon fructose ingestion.
*Homocysteine*
- Elevated homocysteine levels are characteristic of **homocystinuria**, which is due to defects in methionine metabolism, often involving **cystathionine beta-synthase** or enzymes in the folate/B12 pathways.
- Homocystinuria presents with developmental delay, skeletal abnormalities, and thromboembolic events, distinct from the patient's symptoms.
*Phenylalanine*
- Elevated phenylalanine is the hallmark of **phenylketonuria (PKU)**, an inherited disorder of amino acid metabolism where the body cannot process **phenylalanine**.
- PKU primarily causes neurological issues if untreated, but not typically hyperammonemia or orotic aciduria.
*Uridine monophosphate*
- While orotic acid is a precursor to uridine monophosphate in pyrimidine synthesis, a direct gene therapy for the enzyme producing uridine monophosphate is not the primary intervention for the underlying urea cycle disorder.
- The high orotic acid is a consequence of the urea cycle blockade, not the primary defect itself.
Overview and purpose of urea cycle US Medical PG Question 4: A 4-day-old boy is brought to the physician because of somnolence, poor feeding, and vomiting after his first few breast feedings. He appears lethargic. His respiratory rate is 73/min. Serum ammonia is markedly increased. Genetic analysis shows deficiency in N-acetylglutamate synthase. The activity of which of the following enzymes is most likely directly affected by this genetic defect?
- A. Ornithine translocase
- B. Carbamoyl phosphate synthetase I (Correct Answer)
- C. Argininosuccinase
- D. Argininosuccinate synthetase
- E. Arginase
Overview and purpose of urea cycle Explanation: ***Carbamoyl phosphate synthetase I***
- **N-acetylglutamate** (NAG) is an essential allosteric activator of **carbamoyl phosphate synthetase I (CPS I)**, the rate-limiting enzyme of the urea cycle.
- A deficiency in **N-acetylglutamate synthase** directly leads to a lack of NAG, significantly impairing CPS I activity and causing severe hyperammonemia.
*Ornithine translocase*
- This enzyme is responsible for transporting **ornithine** into the mitochondria for the urea cycle.
- While a defect in **ornithine translocase** also causes hyperammonemia, it is due to accumulation of ornithine and upstream substrates, not a defect in N-acetylglutamate synthase.
*Argininosuccinase*
- Also known as **argininosuccinate lyase**, this enzyme cleaves argininosuccinate into arginine and fumarate.
- A deficiency would lead to accumulation of **argininosuccinate**, and while it is a urea cycle disorder, it is not directly affected by N-acetylglutamate synthase deficiency.
*Argininosuccinate synthetase*
- This enzyme catalyzes the condensation of **citrulline** and **aspartate** to form argininosuccinate.
- A defect in **argininosuccinate synthetase** causes citrullinemia but is not directly regulated by N-acetylglutamate.
*Arginase*
- **Arginase** is the final enzyme in the urea cycle, hydrolyzing arginine to form urea and ornithine.
- A deficiency would lead to hyperargininemia, which typically presents later in childhood and is not directly affected by N-acetylglutamate.
Overview and purpose of urea cycle US Medical PG Question 5: A 2-day-old male is seen in the newborn nursery for repeated emesis and lethargy. He was born at 39 weeks to a 24-year-old mother following an uncomplicated pregnancy and birth. He has been breastfeeding every 2 hours and has 10 wet diapers per day. His father has a history of beta-thalassemia minor. Laboratory results are as follows:
Hemoglobin: 12 g/dL
Platelet count: 200,000/mm³
Mean corpuscular volume: 95 µm³
Reticulocyte count: 0.5%
Leukocyte count: 5,000/mm³ with normal differential
Serum:
Na+: 134 mEq/L
Cl-: 100 mEq/L
K+: 3.3 mEq/L
HCO3-: 24 mEq/L
Urea nitrogen: 1 mg/dL
Creatinine: 0.6 mg/dL
Ammonia: 150 µmol/L (normal: 50-80 µmol/L)
Which of the following is the most likely diagnosis?
- A. Phenylketonuria
- B. Orotic aciduria
- C. Alkaptonuria
- D. Ornithine transcarbamylase deficiency (Correct Answer)
- E. Beta-thalassemia minor
Overview and purpose of urea cycle Explanation: ***Ornithine transcarbamylase deficiency***
- The combination of **lethargy**, vomiting (emesis), and **significantly elevated ammonia levels** in a neonate strongly points to a **urea cycle disorder**, with ornithine transcarbamylase (OTC) deficiency being the most common.
- This X-linked disorder leads to a buildup of ammonia due to the inability to convert carbamoyl phosphate and ornithine into citrulline, a crucial step in the urea cycle.
*Phenylketonuria*
- Characterized by the inability to metabolize **phenylalanine**, leading to its accumulation and neurological damage if untreated.
- Typically presents with developmental delay, seizures, and a musty odor, not acute hyperammonemia and vomiting in the neonatal period.
*Orotic aciduria*
- A rare metabolic disorder caused by a defect in **pyrimidine synthesis**, leading to accumulation of **orotic acid**.
- Presents with megaloblastic anemia, developmental delay, and failure to thrive, but not typically with severe neonatal hyperammonemia.
*Alkaptonuria*
- An autosomal recessive disorder of **tyrosine metabolism** where homogentisic acid oxidase is deficient, leading to a buildup of **homogentisic acid**.
- Characterized by dark urine when exposed to air, ochronosis (bluish-black pigmentation of cartilage), and early-onset osteoarthritis; it does not cause acute neonatal illness with hyperammonemia.
*Beta-thalassemia minor*
- This is an **inherited blood disorder** causing mild anemia, often asymptomatic, due to reduced or absent beta-globin chain production.
- While the father has this condition, the infant's symptoms of lethargy, vomiting, and hyperammonemia are **not consistent** with beta-thalassemia minor.
Overview and purpose of urea cycle US Medical PG Question 6: A 2-day-old male infant is brought to the emergency department by ambulance after his parents noticed that he was convulsing and unresponsive. He was born at home and appeared well initially; however, within 24 hours he became increasingly irritable and lethargic. Furthermore, he stopped feeding and began to experience worsening tachypnea. This continued for about 6 hours, at which point his parents noticed the convulsions and called for an ambulance. Laboratories are obtained with the following results:
Orotic acid: 9.2 mmol/mol creatinine (normal: 1.4-5.3 mmol/mol creatinine)
Ammonia: 135 µmol/L (normal: < 50 µmol/L)
Citrulline: 2 µmol/L (normal: 10-45 µmol/L)
Which of the following treatments would most likely be beneficial to this patient?
- A. Galactose avoidance
- B. Aspartame avoidance
- C. Benzoate administration (Correct Answer)
- D. Uridine administration
- E. Fructose avoidance
Overview and purpose of urea cycle Explanation: ***Benzoate administration***
- This patient presents with hyperammonemia (135 µmol/L), elevated orotic acid (9.2 mmol/mol creatinine), and **low citrulline (2 µmol/L)**, which is the classic triad for **ornithine transcarbamylase (OTC) deficiency**.
- The low citrulline distinguishes OTC deficiency from other urea cycle defects, while elevated orotic acid results from accumulation of carbamoyl phosphate that gets shunted into pyrimidine synthesis.
- **Sodium benzoate** is a nitrogen scavenger that conjugates with glycine to form hippurate, which is excreted renally, providing an alternative pathway for nitrogen disposal and reducing toxic ammonia levels.
- This is a life-saving acute treatment for hyperammonemia in urea cycle disorders.
*Galactose avoidance*
- This is the treatment for **galactosemia**, a disorder of galactose metabolism caused by galactose-1-phosphate uridyltransferase deficiency.
- Galactosemia presents with hepatomegaly, jaundice, cataracts, intellectual disability, and hypoglycemia after milk feeding.
- The patient's hyperammonemia and elevated orotic acid pattern is incompatible with galactosemia.
*Aspartame avoidance*
- This is relevant for **phenylketonuria (PKU)** dietary management, as aspartame contains phenylalanine.
- PKU presents with developmental delay, intellectual disability, musty odor, and eczema, with elevated phenylalanine levels.
- Ammonia and orotic acid are normal in PKU, making this diagnosis inconsistent with the lab findings.
*Uridine administration*
- **Uridine** treats **hereditary orotic aciduria** (UMP synthase deficiency), which presents with megaloblastic anemia, growth retardation, and developmental delays.
- While orotic acid is elevated in both conditions, hereditary orotic aciduria has **normal ammonia** and the primary pathology is impaired pyrimidine synthesis, not ammonia disposal.
- This patient's life-threatening hyperammonemia requires immediate nitrogen scavenging, which uridine does not provide.
*Fructose avoidance*
- This treats **hereditary fructose intolerance** (aldolase B deficiency), which causes hypoglycemia, vomiting, hepatomegaly, and jaundice after fructose ingestion.
- The presentation is triggered by dietary fructose exposure and does not cause hyperammonemia or elevated orotic acid.
- The patient's metabolic profile is inconsistent with a fructose metabolism disorder.
Overview and purpose of urea cycle US Medical PG Question 7: A 4-day-old male newborn delivered at 39 weeks' gestation is evaluated because of poor feeding, recurrent vomiting, and lethargy. Physical examination shows tachypnea with subcostal retractions. An enzyme assay performed on a liver biopsy specimen shows decreased activity of carbamoyl phosphate synthetase I. This enzyme plays an important role in the breakdown and excretion of amino groups that result from protein digestion. Which of the following is an immediate substrate for the synthesis of the molecule needed for the excretion of amino groups?
- A. N-acetylglutamate
- B. Homocysteine
- C. Phenylalanine
- D. Valine
- E. Aspartate (Correct Answer)
Overview and purpose of urea cycle Explanation: ***Aspartate***
- The question describes a case of **carbamoyl phosphate synthetase I (CPS I)** deficiency, which leads to **hyperammonemia** due to impaired urea cycle function.
- The urea cycle is responsible for excreting **amino groups** as urea; one of the key molecules directly incorporated into the urea molecule is **aspartate**, which donates an amino group to form **argininosuccinate**.
*N-acetylglutamate*
- **N-acetylglutamate** is an essential activator of **carbamoyl phosphate synthetase I (CPS I)**, the enzyme deficient in this patient.
- While crucial for the urea cycle's regulation, it is an **allosteric activator** rather than a direct substrate for the synthesis of molecules needed for amino group excretion.
*Homocysteine*
- **Homocysteine** is an intermediate in **methionine metabolism** and is primarily associated with cardiovascular disease and neurological issues when elevated.
- It plays no direct role as a substrate in the urea cycle for the excretion of amino groups.
*Phenylalanine*
- **Phenylalanine** is an **essential amino acid** that is a precursor to tyrosine and neurotransmitters.
- Its metabolism is separate from the urea cycle, and it is not a direct substrate for ammonia excretion in this pathway.
*Valine*
- **Valine** is a **branched-chain amino acid (BCAA)** primarily catabolized in muscles and used for energy.
- It is not a direct substrate in the urea cycle, which processes nitrogen from various amino acids into urea for excretion.
Overview and purpose of urea cycle US Medical PG Question 8: A 26-year-old African American man comes to the physician because of a 3-day history of fatigue, back pain, and dark urine. One week ago, he developed a headache and was treated with aspirin. He does not smoke or use illicit drugs. Physical examination shows conjunctival pallor. A peripheral blood smear shows erythrocytes with inclusions of denatured hemoglobin. Which of the following enzymes is involved in providing precursors for nucleotide synthesis in this patient?
- A. Glucose-6-phosphatase
- B. Carbamoyl phosphate synthetase I
- C. Pyruvate carboxylase
- D. Transaldolase (Correct Answer)
- E. Enolase
Overview and purpose of urea cycle Explanation: ***Transaldolase***
- This patient likely has **glucose-6-phosphate dehydrogenase (G6PD) deficiency**, indicated by fatigue, dark urine (hemolysis), and **Heinz bodies** (erythrocytes with inclusions of denatured hemoglobin) after aspirin exposure, which is an **oxidative stressor**.
- **Transaldolase** is an enzyme in the **non-oxidative phase of the pentose phosphate pathway (PPP)**, which produces **ribose-5-phosphate**, a precursor for nucleotide synthesis.
*Glucose-6-phosphatase*
- **Glucose-6-phosphatase** is involved in **gluconeogenesis** and glycogenolysis, primarily in the liver and kidneys, to release free glucose into the bloodstream.
- Deficiency leads to **Von Gierke disease**, characterized by hypoglycemia, hepatomegaly, lactic acidosis, and hyperlipidemia, which are not described here.
*Carbamoyl phosphate synthetase I*
- **Carbamoyl phosphate synthetase I (CPS I)** is a mitochondrial enzyme that catalyzes the first committed step in the **urea cycle**, converting ammonia and bicarbonate into carbamoyl phosphate.
- Its deficiency causes **hyperammonemia**, not hemolytic anemia or issues with nucleotide synthesis.
*Pyruvate carboxylase*
- **Pyruvate carboxylase** is a mitochondrial enzyme that converts **pyruvate to oxaloacetate**, a crucial step in **gluconeogenesis** and replenishing intermediates of the citric acid cycle.
- Deficiency can lead to lactic acidosis and hypoglycemia, which are not the primary symptoms here.
*Enolase*
- **Enolase** is an enzyme in **glycolysis** that catalyzes the dehydration of 2-phosphoglycerate to phosphoenolpyruvate.
- It is not directly involved in providing precursors for nucleotide synthesis.
Overview and purpose of urea cycle US Medical PG Question 9: A 9-year-old boy is brought to the emergency department for the evaluation of diarrhea and vomiting for the last 2 days. During this period, he has had about 12 watery, non-bloody bowel movements and has vomited three times. He came back from a trip to India 3 days ago, where he and his family were visiting relatives. He has not been able to eat anything since the symptoms started. The patient has not urinated since yesterday. He appears pale. His temperature is 38°C (100.4°F), pulse is 106/min, and blood pressure is 96/60 mm Hg. Examination shows dry mucous membranes. The abdomen is soft with no organomegaly. Bowel sounds are hyperactive. Laboratory studies show:
Hemoglobin 13 g/dL
Serum
Na+ 148 mEq/L
Cl- 103 mEq/L
K+ 3.7 mEq/L
HCO3- 19 mEq/L
Urea nitrogen 80 mg/dL
Glucose 90 mg/dL
Creatinine 2 mg/dL
Intravenous fluid resuscitation is begun. Which of the following is the most likely cause of this patient's abnormal renal laboratory findings?
- A. Urinary tract obstruction
- B. IgA complex deposition
- C. Decreased renal perfusion (Correct Answer)
- D. Renal artery stenosis
- E. Glomerulonephritis
Overview and purpose of urea cycle Explanation: ***Decreased renal perfusion***
- The patient's presentation with **diarrhea and vomiting, dry mucous membranes**, **hypotension (96/60 mm Hg)**, **tachycardia (106/min)**, and **oliguria** (no urination since yesterday) indicates significant **volume depletion** and **dehydration**.
- This leads to **decreased blood flow to the kidneys (prerenal azotemia)**, resulting in **elevated BUN (80 mg/dL) and creatinine (2 mg/dL)**, along with a **high BUN/creatinine ratio** (40:1).
*Urinary tract obstruction*
- While it can cause elevated BUN and creatinine, it typically presents with **suprapubic pain, difficulty voiding**, or a **palpable bladder**, none of which are described.
- Obstruction does not explain the widespread signs of **dehydration** and **hypoperfusion**.
*IgA complex deposition*
- This refers to **IgA nephropathy**, a form of **glomerulonephritis**, which typically causes **hematuria** rather than primarily acute kidney injury from dehydration.
- The clinical picture of acute fluid loss and hypovolemia does not align with the typical presentation of IgA nephropathy.
*Renal artery stenosis*
- This condition involves **narrowing of the renal arteries**, leading to **chronic kidney disease** and often **hypertension**, which is contrary to the patient's **hypotension**.
- It does not present as an acute syndrome linked to a recent diarrheal illness and systemic dehydration.
*Glomerulonephritis*
- Glomerulonephritis usually presents with **hematuria, proteinuria, edema**, and **hypertension**, none of which are prominent features here.
- While it can cause elevated BUN and creatinine, the primary cause of renal dysfunction in this patient is clearly related to **volume depletion** from gastrointestinal losses.
Overview and purpose of urea cycle US Medical PG Question 10: An investigator is studying nutritional deficiencies in humans. A group of healthy volunteers are started on a diet deficient in pantothenic acid. After 4 weeks, several of the volunteers develop irritability, abdominal cramps, and burning paresthesias of their feet. These symptoms are fully reversed after reintroduction of pantothenic acid to their diet. The function of which of the following enzymes was most likely impaired in the volunteers during the study?
- A. Gamma-glutamyl carboxylase
- B. Alpha-ketoglutarate dehydrogenase (Correct Answer)
- C. Dopamine beta-hydroxylase
- D. Methionine synthase
- E. Glutathione reductase
Overview and purpose of urea cycle Explanation: ***Alpha-ketoglutarate dehydrogenase***
- **Pantothenic acid** (vitamin B5) is a precursor of **coenzyme A (CoA)**, which is essential for the function of alpha-ketoglutarate dehydrogenase in the **Krebs cycle**.
- Impairment of this enzyme, critical for energy production, can lead to widespread metabolic dysfunction, manifesting as neurological and gastrointestinal symptoms like **irritability, abdominal cramps**, and **burning paresthesias**, which are classic signs of pantothenic acid deficiency.
*Gamma-glutamyl carboxylase*
- This enzyme is involved in the post-translational modification of several proteins, including **clotting factors**, and requires **vitamin K** as a cofactor.
- Its deficiency leads to bleeding disorders, not the neurological and GI symptoms described.
*Dopamine beta-hydroxylase*
- This enzyme converts **dopamine to norepinephrine** and requires vitamin C and copper.
- Its impairment can affect neurotransmitter synthesis but is not directly linked to pantothenic acid deficiency.
*Methionine synthase*
- This enzyme is crucial for the metabolism of **homocysteine** and requires **vitamin B12** and **folate** as cofactors.
- Its deficiency is associated with megaloblastic anemia and neurological symptoms, but not the specific presentation seen with pantothenic acid deficiency.
*Glutathione reductase*
- This enzyme is essential for maintaining the reduced state of **glutathione**, an antioxidant, and requires **riboflavin** (vitamin B2) in its coenzyme form, FAD.
- Dysfunction typically leads to oxidative stress, hemolytic anemia, and other symptoms different from those described.
More Overview and purpose of urea cycle US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.