Nitrogen sources and transport forms US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Nitrogen sources and transport forms. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Nitrogen sources and transport forms US Medical PG Question 1: A 9-year-old boy presents to the emergency department with a 12-hour history of severe vomiting and increased sleepiness. He experienced high fever and muscle pain about 5 days prior to presentation, and his parents gave him aspirin to control the fever at that time. On presentation, he is found to be afebrile though he is still somnolent and difficult to arouse. Physical exam reveals hepatomegaly and laboratory testing shows the following results:
Alanine aminotransferase: 85 U/L
Aspartate aminotransferase: 78 U/L
Which of the following is the most likely cause of this patient's neurologic changes?
- A. Subarachnoid hemorrhage
- B. Viral meningitis
- C. Reye syndrome
- D. Cerebral edema (Correct Answer)
- E. Bacterial sepsis
Nitrogen sources and transport forms Explanation: ***Cerebral edema***
- The combination of a recent **viral illness** treated with **aspirin** in a child, leading to severe vomiting, increased sleepiness, hepatomegaly, and elevated transaminases, is highly suggestive of **Reye syndrome**.
- **Cerebral edema** is a critical and life-threatening complication of **Reye syndrome**, causing the neurologic symptoms like somnolence, difficulty arousing, and ultimately coma.
*Subarachnoid hemorrhage*
- While subarachnoid hemorrhage can cause acute neurological changes, it typically presents with a **sudden, severe headache** ("thunderclap headache") and signs of meningeal irritation, which are not described here.
- There is no clinical indication such as trauma or ruptured aneurysm to suggest a subarachnoid hemorrhage in this patient.
*Viral meningitis*
- Viral meningitis would typically present with **fever**, headache, and **nuchal rigidity**, often accompanied by photophobia, which are not the prominent features in this case.
- The elevated liver enzymes and hepatomegaly are not characteristic of viral meningitis.
*Reye syndrome*
- **Reye syndrome** is the underlying diagnosis, characterized by acute **encephalopathy** and hepatic dysfunction following a viral infection treated with salicylates.
- However, the question asks for the **most likely cause of the neurological changes**, which is specifically the brain swelling, or cerebral edema, that occurs as a direct result of Reye syndrome pathophysiology.
*Bacterial sepsis*
- Bacterial sepsis would present with signs of systemic infection, often including **high fever**, tachycardia, and hypotension, which are not present as the patient is afebrile.
- While sepsis can cause encephalopathy, the presence of **hepatomegaly** and the history of **aspirin use** point much more strongly toward Reye syndrome with its associated cerebral edema.
Nitrogen sources and transport forms US Medical PG Question 2: An investigator is studying severely ill patients who experience hypoglycemia and ketonuria during times of fasting. The investigator determines that during these episodes, amino acids liberated from muscle proteins are metabolized to serve as substrates for gluconeogenesis. Nitrogen from this process is transported to the liver primarily in the form of which of the following molecules?
- A. Glutamate
- B. α-ketoglutarate
- C. Alanine (Correct Answer)
- D. Arginine
- E. Pyruvate
Nitrogen sources and transport forms Explanation: ***Alanine***
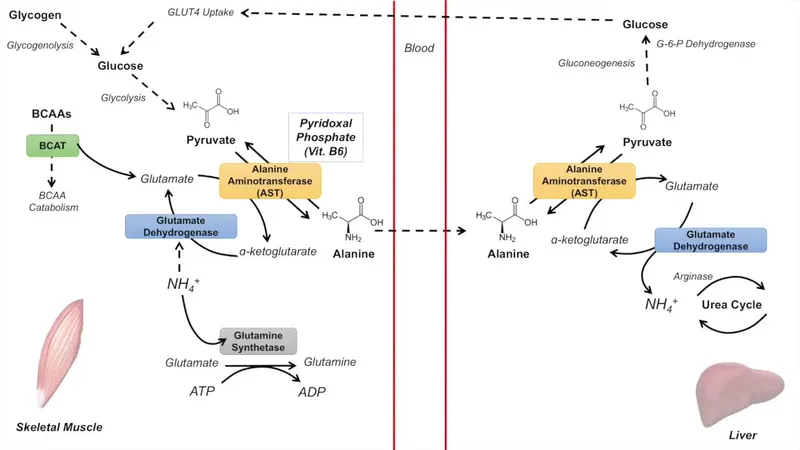
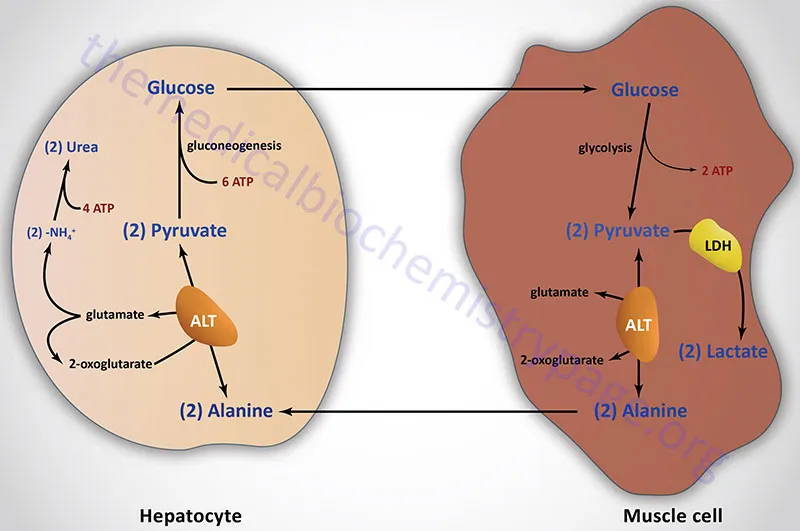
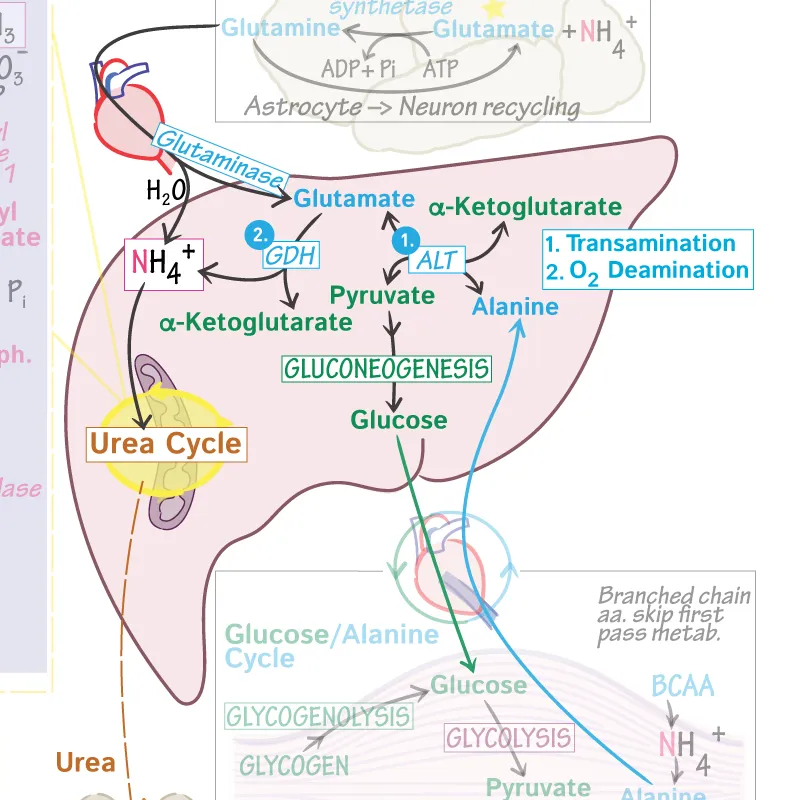
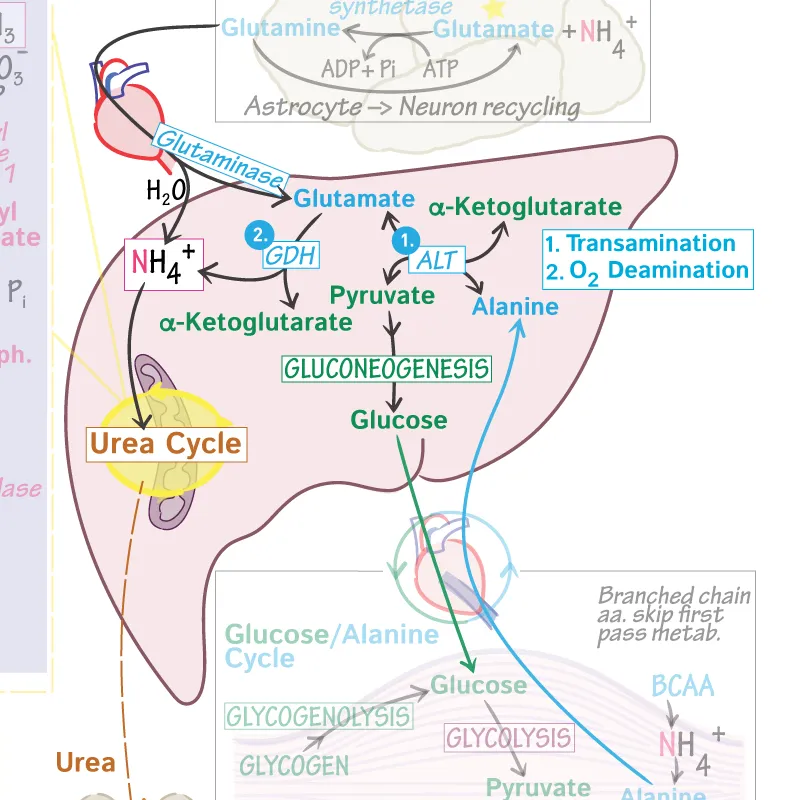
- During prolonged fasting, **muscle proteins are catabolized** to provide amino acids for gluconeogenesis in the liver.
- **Alanine** is the primary amino acid released from muscle into the bloodstream to transport nitrogen to the liver through the **glucose-alanine cycle (Cahill cycle)**.
- In this cycle, pyruvate in muscle accepts an amino group from glutamate to form alanine, which is then transported to the liver, where it is deaminated back to pyruvate (for gluconeogenesis) and ammonia (for the urea cycle).
- **Glutamine** also serves as an important nitrogen transporter, particularly to the kidneys and intestines.
*Glutamate*
- **Glutamate** is an important amino acid in nitrogen metabolism within tissues, but it is not the primary form in which nitrogen is transported from muscle to the liver in significant quantities.
- While glutamate participates in transamination reactions within muscle, its efflux from muscle into the blood is less prominent than alanine for inter-organ nitrogen transport.
*α-ketoglutarate*
- **α-ketoglutarate** is a key intermediate in the **Krebs cycle** and accepts an amino group to form glutamate.
- It is an alpha-keto acid, not an amino acid, and therefore does not directly transport nitrogen in the form of an amino group to the liver via the bloodstream.
*Arginine*
- **Arginine** is primarily involved in the **urea cycle** within the liver, where it helps in the detoxification of ammonia, but it is not a major transporter of nitrogen from peripheral tissues to the liver for gluconeogenesis.
- Its role is mainly within the liver for urea synthesis, not for inter-organ nitrogen transport in this context.
*Pyruvate*
- **Pyruvate** is a keto acid that can be converted to alanine via transamination.
- While pyruvate is a precursor to alanine and a substrate for gluconeogenesis, it transports carbon skeletons and not nitrogen itself; **alanine is the actual nitrogen carrier** in this cycle.
Nitrogen sources and transport forms US Medical PG Question 3: A 4-day-old male newborn delivered at 39 weeks' gestation is evaluated because of poor feeding, recurrent vomiting, and lethargy. Physical examination shows tachypnea with subcostal retractions. An enzyme assay performed on a liver biopsy specimen shows decreased activity of carbamoyl phosphate synthetase I. This enzyme plays an important role in the breakdown and excretion of amino groups that result from protein digestion. Which of the following is an immediate substrate for the synthesis of the molecule needed for the excretion of amino groups?
- A. N-acetylglutamate
- B. Homocysteine
- C. Phenylalanine
- D. Valine
- E. Aspartate (Correct Answer)
Nitrogen sources and transport forms Explanation: ***Aspartate***
- The question describes a case of **carbamoyl phosphate synthetase I (CPS I)** deficiency, which leads to **hyperammonemia** due to impaired urea cycle function.
- The urea cycle is responsible for excreting **amino groups** as urea; one of the key molecules directly incorporated into the urea molecule is **aspartate**, which donates an amino group to form **argininosuccinate**.
*N-acetylglutamate*
- **N-acetylglutamate** is an essential activator of **carbamoyl phosphate synthetase I (CPS I)**, the enzyme deficient in this patient.
- While crucial for the urea cycle's regulation, it is an **allosteric activator** rather than a direct substrate for the synthesis of molecules needed for amino group excretion.
*Homocysteine*
- **Homocysteine** is an intermediate in **methionine metabolism** and is primarily associated with cardiovascular disease and neurological issues when elevated.
- It plays no direct role as a substrate in the urea cycle for the excretion of amino groups.
*Phenylalanine*
- **Phenylalanine** is an **essential amino acid** that is a precursor to tyrosine and neurotransmitters.
- Its metabolism is separate from the urea cycle, and it is not a direct substrate for ammonia excretion in this pathway.
*Valine*
- **Valine** is a **branched-chain amino acid (BCAA)** primarily catabolized in muscles and used for energy.
- It is not a direct substrate in the urea cycle, which processes nitrogen from various amino acids into urea for excretion.
Nitrogen sources and transport forms US Medical PG Question 4: A 36-year-old man is brought to the emergency department by his girlfriend because of increasing confusion for the past 6 hours. He drinks large amounts of alcohol daily and occasionally uses illicit drugs. He is lethargic and oriented only to person. Physical examination shows jaundice, hepatomegaly, and scattered petechiae over the trunk and back. Neurologic examination shows normal, reactive pupils and a flapping tremor when the wrists are extended. A drug with which of the following mechanism of action would be most appropriate for this patient's condition?
- A. Production of NH3
- B. Activation of GABA receptors
- C. Excretion of free iron
- D. Inhibition of D2 receptors
- E. Excretion of NH4 (Correct Answer)
Nitrogen sources and transport forms Explanation: ***Excretion of NH4***
- The patient presents with **hepatic encephalopathy**, characterized by **confusion**, **jaundice**, **hepatomegaly**, **petechiae**, and a **flapping tremor (asterixis)**, stemming from chronic alcohol abuse and liver damage. The main pathophysiology in hepatic encephalopathy is the accumulation of **ammonia (NH3)**, which is neurotoxic.
- Excretion of **NH4** (ammonium) through drug mechanisms such as **lactulose** (which acidifies the colon, trapping ammonia as ammonium for excretion) is the primary therapeutic target to reduce ammonia levels and improve neurological symptoms.
*Production of NH3*
- This mechanism would exacerbate the patient's condition by increasing the toxic load of **ammonia (NH3)**, which is already elevated in hepatic encephalopathy.
- Therapeutic interventions aim to decrease, not increase, ammonia production or absorption.
*Activation of GABA receptors*
- While **GABA receptor activation** is involved in the neurological effects of some substances that contribute to confusion, it is not the primary target for treating the underlying pathophysiology of **hepatic encephalopathy**.
- Medications that activate GABA receptors (e.g., benzodiazepines) can worsen encephalopathy by further depressing CNS function.
*Excretion of free iron*
- **Iron overload** can cause liver damage, but the acute confusion and flapping tremor are more indicative of **hepatic encephalopathy** due to ammonia toxicity, not primarily iron accumulation.
- Excreting free iron (e.g., with chelation therapy) is for conditions like hemochromatosis and would not address the immediate, life-threatening neurological symptoms in this patient.
*Inhibition of D2 receptors*
- This mechanism is characteristic of some **antipsychotic medications**. While dopamine imbalances can play a role in some neurological disorders, inhibiting D2 receptors is not a primary therapeutic target for **hepatic encephalopathy**.
- Such medications could have side effects that might complicate the clinical picture in a patient with acute liver failure.
Nitrogen sources and transport forms US Medical PG Question 5: A 24-year-old man is running a marathon. Upon reaching the finish line, his serum lactate levels were measured and were significantly increased as compared to his baseline. Which of the following pathways converts the lactate produced by muscles into glucose and transports it back to the muscles?
- A. Citric acid cycle
- B. Glycolysis
- C. Glycogenesis
- D. Pentose phosphate pathway
- E. Cori cycle (Correct Answer)
Nitrogen sources and transport forms Explanation: ***Cori cycle***
- The **Cori cycle** is the metabolic pathway that converts **lactate** produced by anaerobic glycolysis in muscles (especially during intense exercise) back to **glucose in the liver** via gluconeogenesis.
- During strenuous exercise, muscles rely on anaerobic glycolysis when oxygen supply is insufficient, producing lactate and 2 ATP per glucose.
- The lactate is transported via bloodstream to the liver, where it is converted back to glucose (requiring 6 ATP), which then returns to muscles for energy or glycogen storage.
- This cycle allows muscles to continue generating ATP anaerobically while the liver handles lactate clearance.
*Citric acid cycle*
- The **citric acid cycle** (Krebs cycle) oxidizes **acetyl-CoA** to generate ATP, NADH, and FADH₂ in the mitochondrial matrix under aerobic conditions.
- It does not convert lactate to glucose; rather, pyruvate can be converted to acetyl-CoA to enter this cycle for complete oxidation.
- This is an aerobic process and does not involve the liver-muscle lactate-glucose exchange.
*Glycolysis*
- **Glycolysis** is the metabolic pathway that breaks down **glucose into pyruvate**, generating 2 ATP and 2 NADH per glucose molecule.
- Under anaerobic conditions, pyruvate is converted to lactate to regenerate NAD⁺ for continued glycolysis.
- This is the opposite of what the question asks—glycolysis produces lactate from glucose, not glucose from lactate.
*Glycogenesis*
- **Glycogenesis** is the process of synthesizing **glycogen from glucose** for storage, primarily in liver and muscle tissue.
- While it involves glucose storage, it does not convert lactate back to glucose or involve the metabolic exchange between muscles and liver described in the question.
*Pentose phosphate pathway*
- The **pentose phosphate pathway** (hexose monophosphate shunt) produces **NADPH** for reductive biosynthesis and **ribose-5-phosphate** for nucleotide synthesis.
- It branches from glycolysis but is not involved in lactate metabolism or the muscle-liver glucose-lactate exchange.
Nitrogen sources and transport forms US Medical PG Question 6: What is the primary mechanism for glucose uptake in neurons?
- A. GLUT1
- B. GLUT2
- C. GLUT3 (Correct Answer)
- D. GLUT4
Nitrogen sources and transport forms Explanation: ***GLUT3***
- **GLUT3** is the primary glucose transporter in **neurons** and has a **high affinity** for glucose.
- This high affinity ensures that neurons can continuously take up glucose, even when blood glucose levels are relatively low, to meet their significant energy demands.
*GLUT1*
- **GLUT1** is abundant in **red blood cells** and at the **blood-brain barrier**, where it provides basal glucose transport to many cell types.
- While present in the brain, it is primarily responsible for glucose transport across the **blood-brain barrier** into the interstitial fluid, not directly into neurons as the main mechanism.
*GLUT2*
- **GLUT2** has a **low affinity** and **high capacity** for glucose, primarily found in the **liver, pancreatic beta cells, kidney, and intestine**.
- Its role is to sense high glucose levels and transport large amounts of glucose accordingly, which is not characteristic of neuronal glucose uptake.
*GLUT4*
- **GLUT4** is the **insulin-sensitive** glucose transporter, predominantly found in **adipose tissue** and **skeletal muscle**.
- Its translocation to the cell membrane is stimulated by insulin, a mechanism not central to neuronal glucose uptake.
Nitrogen sources and transport forms US Medical PG Question 7: An investigator is studying biomolecular mechanisms in human cells. A radioactive isotope that is unable to cross into organelles is introduced into a sample of cells. The cells are then fragmented via centrifugation and the isotope-containing components are isolated. Which of the following reactions is most likely to be present in this cell component?
- A. Glucose-6-phosphate to glucose
- B. Isocitrate to α-ketoglutarate
- C. Carbamoyl phosphate to citrulline
- D. Fatty acyl-CoA to acetyl-CoA
- E. Glucose-6-phosphate to 6-phosphogluconolactone (Correct Answer)
Nitrogen sources and transport forms Explanation: ***Glucose-6-phosphate to 6-phosphogluconolactone***
- This reaction is the first step of the **pentose phosphate pathway (PPP)**, which occurs in the **cytosol**.
- Since the isotope cannot cross into organelles and is found in the cytosolic fraction, this pathway is a likely candidate.
*Glucose-6-phosphate to glucose*
- This reaction describes the dephosphorylation of **glucose-6-phosphate** to **glucose**, catalyzed by **glucose-6-phosphatase**.
- While important for glucose release, this enzyme is primarily located in the **endoplasmic reticulum** of the liver and kidneys, an organelle.
*Isocitrate to α-ketoglutarate*
- This is a step in the **Krebs cycle (citric acid cycle)**, which takes place in the **mitochondrial matrix**.
- The isotope would not be found in this compartmentalized reaction because it cannot enter organelles.
*Carbamoyl phosphate to citrulline*
- This reaction is part of the **urea cycle**, which has steps occurring in both the **mitochondrial matrix** and the cytosol. The initial step, forming carbamoyl phosphate, is mitochondrial.
- The isotope, being unable to cross into organelles, would not readily participate in the mitochondrial portion of this pathway.
*Fatty acyl-CoA to acetyl-CoA*
- This reaction represents **beta-oxidation of fatty acids**, a process that primarily occurs in the **mitochondria** and peroxisomes.
- As the isotope is excluded from organelles, it would not be involved in these reactions.
Nitrogen sources and transport forms US Medical PG Question 8: A 4-year-old boy presents with vomiting and one day of lethargy after a one week history of flu-like symptoms and low-grade fevers. The vomiting is nonbilious and nonbloody. The patient has had no other symptoms aside from mild rhinorrhea and cough. He has no past medical history, and is on no medications except for over-the-counter medications for his fever. His temperature is 98.5°F (36.9°C), pulse is 96/min, respirations are 14/min, and blood pressure is 108/80 mmHg. The patient appears lethargic and is oriented only to person. Otherwise, the physical exam is benign and the patient has no other neurologic symptoms. What is the mechanism of the most likely cause of this patient’s presentation?
- A. Deficient erythrocyte enzyme
- B. Chemical ingestion
- C. Bacterial infection
- D. Irreversible enzyme inhibition (Correct Answer)
- E. Reversible enzyme inhibition
Nitrogen sources and transport forms Explanation: ***Irreversible enzyme inhibition***
- This presentation is highly suggestive of **Reye syndrome**, which is associated with **aspirin use** in children with viral illnesses. Aspirin (acetylsalicylic acid) **irreversibly inhibits cyclooxygenase (COX) enzymes** by acetylating a serine residue at the active site.
- While aspirin's primary mechanism is COX inhibition, **Reye syndrome** involves **mitochondrial dysfunction** in hepatocytes, leading to impaired fatty acid beta-oxidation, hyperammonemia, hepatic steatosis, and **encephalopathy**. This explains the vomiting, lethargy, and altered mental status after flu-like symptoms.
- The key connection is that aspirin acts through **irreversible enzyme inhibition**, making this the correct mechanistic classification for the causative agent.
*Reversible enzyme inhibition*
- While some aspects of Reye syndrome involve mitochondrial enzyme dysfunction, aspirin itself does **not** act through reversible competitive inhibition—it **irreversibly acetylates** COX enzymes.
- Reversible inhibition would imply the drug effect could be easily overcome by increasing substrate concentration, which is not the case with aspirin's mechanism.
*Deficient erythrocyte enzyme*
- This mechanism is associated with conditions like **glucose-6-phosphate dehydrogenase (G6PD) deficiency**, which primarily causes **hemolytic anemia** with jaundice and pallor.
- While G6PD deficiency can be triggered by certain medications, it does not typically present with the **encephalopathy** and liver dysfunction seen in this patient.
*Chemical ingestion*
- While aspirin is technically a chemical, the question asks about the **mechanism** rather than the route of exposure. The specific mechanism is irreversible enzyme inhibition.
- The history of **flu-like symptoms** and use of over-the-counter fever medications strongly suggests aspirin-associated Reye syndrome rather than accidental toxic ingestion.
*Bacterial infection*
- A severe bacterial infection (e.g., **bacterial meningitis** or **sepsis**) could cause lethargy and vomiting, but the clinical picture (normal vital signs, benign physical exam, no fever) is not typical for acute bacterial infection.
- The association with a recent **viral illness** and potential over-the-counter medication use strongly favors Reye syndrome, a non-infectious etiology.
Nitrogen sources and transport forms US Medical PG Question 9: A 3-year-old boy is seen in clinic. He was born at home without perinatal care. He was apparently normal at birth, but later developed failure to thrive and developmental delay. He also has a history of cataracts. His older brother had a myocardial infarction at the age of 18 and is rather lanky and tall in appearance. Laboratory testing of his urine showed an increase in the level of an amino acid. What is the most likely mechanism responsible for this boy's pathology?
- A. Hereditary defect of renal amino acid transporter
- B. Inability to degrade branched chain amino acids
- C. Cystathionine synthase deficiency (Correct Answer)
- D. Deficiency of homogentisic acid oxidase
- E. Deficiency of phenylalanine hydroxylase
Nitrogen sources and transport forms Explanation: ***Cystathionine synthase deficiency***
- The constellation of **developmental delay, failure to thrive, cataracts**, and a history of **myocardial infarction** in an older sibling with a **marfanoid habitus** points to **homocystinuria**.
- **Cystathionine synthase deficiency** is the most common cause of homocystinuria, leading to an **accumulation of homocysteine** and methionine, which can be detected in urine.
*Hereditary defect of renal amino acid transporter*
- Conditions like **cystinuria** involve defective renal transport of specific amino acids (cystine, ornithine, lysine, arginine) but typically present with **kidney stones**, not cataracts or thrombotic events.
- This defect would lead to elevated levels of the affected amino acids in the urine but does not explain the systemic features observed.
*Inability to degrade branched chain amino acids*
- This describes **Maple Syrup Urine Disease**, characterized by the inability to metabolize **leucine, isoleucine, and valine**.
- It presents with symptoms like **poor feeding, lethargy, seizures, and a distinctive sweet odor** in urine, which are not detailed here, and generally has a more acute and severe neonatal presentation without a typical marfanoid habitus or thrombotic events.
*Deficiency of homogentisic acid oxidase*
- This deficiency causes **alkaptonuria**, an inborn error of tyrosine metabolism.
- It is characterized by **dark urine** upon standing, **ochronosis** (darkening of connective tissues), and **arthropathy**, none of which are consistent with the patient's symptoms.
*Decreased in phenylalanine hydroxylase*
- This is the enzyme deficient in **phenylketonuria (PKU)**, which leads to the accumulation of **phenylalanine**.
- PKU typically presents with **intellectual disability, seizures, fair skin, and a musty odor** if untreated, but generally does not involve cataracts or thrombotic events.
Nitrogen sources and transport forms US Medical PG Question 10: A newborn boy develops projectile vomiting 48 hours after delivery. He is found to be lethargic, with poor muscle tone, and is hyperventilating. Within hours, he suffers important neurological deterioration, leading to seizures, coma, and, ultimately, death. An autopsy is performed and the pathology team makes a diagnosis of a rare genetic disorder that leads to low levels of N-acetylglutamate. Which of the following enzymes would be secondarily affected by this process?
- A. Argininosuccinate lyase
- B. Carbamoyl phosphate synthetase I (Correct Answer)
- C. Argininosuccinate synthetase
- D. Ornithine transcarbamylase
- E. Arginase
Nitrogen sources and transport forms Explanation: ***Carbamoyl phosphate synthetase I***
- **N-acetylglutamate** is an **obligate activator** for **Carbamoyl phosphate synthetase I (CPS I)**, the rate-limiting enzyme of the **urea cycle**. Low levels of N-acetylglutamate directly impair CPS I activity.
- Reduced CPS I activity leads to a severe **urea cycle disorder**, causing **hyperammonemia**, which manifests with lethargy, poor muscle tone, hyperventilation, neurological deterioration, seizures, coma, and death in newborns.
*Argininosuccinate lyase*
- This enzyme is involved downstream in the **urea cycle**, catalyzing the cleavage of **argininosuccinate** into **arginine** and **fumarate**.
- Its activity is not directly regulated by **N-acetylglutamate**, so it would not be secondarily affected in the same manner as CPS I.
*Argininosuccinate synthetase*
- This enzyme acts after CPS I and ornithine transcarbamylase in the **urea cycle**, synthesizing **argininosuccinate** from **citrulline** and **aspartate**.
- Its function is independent of **N-acetylglutamate** levels, making it unlikely to be secondarily affected.
*Ornithine transcarbamylase*
- This enzyme catalyzes the second step of the **urea cycle**, forming **citrulline** from **ornithine** and **carbamoyl phosphate**.
- While essential for the urea cycle, its activity is not directly modulated by **N-acetylglutamate**; rather, it depends on the availability of carbamoyl phosphate produced by CPS I.
*Arginase*
- This is the final enzyme in the **urea cycle**, converting **arginine** to **ornithine** and **urea**.
- Its activity is not directly or indirectly regulated by **N-acetylglutamate**, nor is it the enzyme primarily affected in this presentation.
More Nitrogen sources and transport forms US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.