Hyperammonemia causes and effects US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Hyperammonemia causes and effects. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Hyperammonemia causes and effects US Medical PG Question 1: A 23-year-old man presents to the emergency department for altered mental status after a finishing a marathon. He has a past medical history of obesity and anxiety and is not currently taking any medications. His temperature is 104°F (40°C), blood pressure is 147/88 mmHg, pulse is 200/min, respirations are 33/min, and oxygen saturation is 99% on room air. Physical exam reveals dry mucous membranes, hot flushed skin, and inappropriate responses to the physician's questions. Laboratory values are ordered as seen below.
Hemoglobin: 15 g/dL
Hematocrit: 44%
Leukocyte count: 8,500/mm^3 with normal differential
Platelet count: 199,000/mm^3
Serum:
Na+: 165 mEq/L
Cl-: 100 mEq/L
K+: 4.0 mEq/L
HCO3-: 22 mEq/L
BUN: 30 mg/dL
Glucose: 133 mg/dL
Creatinine: 1.5 mg/dL
Ca2+: 10.2 mg/dL
AST: 12 U/L
ALT: 10 U/L
Which of the following is the best next step in management?
- A. Lactated ringer
- B. Hypotonic saline
- C. 50% normal saline 50% dextrose
- D. Normal saline (Correct Answer)
- E. Dextrose solution
Hyperammonemia causes and effects Explanation: ***Normal saline***
- The patient presents with **heat stroke** (temperature 104°F, altered mental status after marathon) complicated by **severe hypernatremia (Na+ 165 mEq/L)** and **hypovolemia** (elevated BUN/Cr ratio, tachycardia, dry mucous membranes).
- In **hypovolemic hypernatremia**, the best initial step is to restore **intravascular volume** with **isotonic crystalloid** (normal saline or lactated Ringer's) to stabilize hemodynamics and organ perfusion.
- **Normal saline (0.9% NaCl, 154 mEq/L Na+)** is hypotonic relative to the patient's serum (165 mEq/L), so it will begin **gradual correction** of hypernatremia while providing volume resuscitation.
- After volume restoration, hypotonic fluids (0.45% saline or D5W) may be used for further correction, but they should NOT be given initially to a volume-depleted patient due to risk of worsening hypotension.
- Correction rate should be **≤10-12 mEq/L per 24 hours** to avoid cerebral edema.
*Hypotonic saline*
- While hypotonic saline (0.45% NaCl) is used to correct hypernatremia, it should **not** be the first-line choice in a **hypovolemic** patient.
- Administering hypotonic fluids to a volume-depleted patient can worsen hypotension and compromise organ perfusion before adequately restoring intravascular volume.
- Hypotonic saline is appropriate **after** volume status has been restored with isotonic fluids.
*Lactated ringer*
- **Lactated Ringer's solution** is an isotonic crystalloid (130 mEq/L Na+) and would be an equally acceptable choice for initial volume resuscitation.
- It is slightly more hypotonic than normal saline, which could provide marginally faster correction of hypernatremia.
- Either normal saline or lactated Ringer's is appropriate for initial management; normal saline is more commonly cited in USMLE resources for hypernatremia management.
*50% normal saline 50% dextrose*
- This mixture would create a **hypertonic solution** that could worsen hypernatremia rather than correct it.
- The patient's glucose is normal (133 mg/dL), so dextrose supplementation is not indicated.
- This option is inappropriate for managing hypernatremia.
*Dextrose solution*
- **D5W (5% dextrose in water)** provides free water and would correct hypernatremia by diluting serum sodium.
- However, in a **volume-depleted** patient, giving free water without adequate sodium can lead to rapid osmotic shifts, worsening hypotension, and potentially causing cerebral edema if correction occurs too rapidly.
- D5W is reserved for **euvolemic or hypervolemic hypernatremia**, not hypovolemic hypernatremia.
Hyperammonemia causes and effects US Medical PG Question 2: A 38-year-old man presents to his physician with double vision persisting for a week. When he enters the exam room, the physician notes that the patient has a broad-based gait. The man’s wife informs the doctor that he has been an alcoholic for the last 5 years and his consumption of alcohol has increased significantly over the past few months. She also reports that he has become indifferent to his family members over time and is frequently agitated. She also says that his memory has been affected significantly, and when asked about a particular detail, he often recollects it incorrectly, though he insists that his version is the true one. On physical examination, his vital signs are stable, but when the doctor asks him where he is, he seems to be confused. His neurological examination also shows nystagmus. Which of the following options describes the earliest change in the pathophysiology of the central nervous system in this man?
- A. Increased astrocyte lactate
- B. Increased extracellular concentration of glutamate
- C. Increased fragmentation of deoxyribonucleic acid within the neurons
- D. Breakdown of the blood-brain barrier
- E. Decreased α-ketoglutarate dehydrogenase activity in astrocytes (Correct Answer)
Hyperammonemia causes and effects Explanation: ***Decreased α-ketoglutarate dehydrogenase activity in astrocytes***
- Chronic **alcoholism** leads to **thiamine deficiency**, which impairs the activity of **α-ketoglutarate dehydrogenase** in the **Krebs cycle**.
- This enzyme is crucial for **neuronal energy metabolism** and its deficiency contributes to the earliest **neuropathological changes** observed in Wernicke-Korsakoff syndrome.
*Increased astrocyte lactate*
- While chronic alcoholism and thiamine deficiency can lead to metabolic dysfunction, increased **astrocyte lactate** is typically a response to **hypoxia** or **ischemia**, not the primary initiating event of thiamine deficiency.
- Lactate accumulation can be a downstream effect of impaired glucose metabolism, but not the earliest or most direct consequence of **α-ketoglutarate dehydrogenase** inhibition.
*Increased extracellular concentration of glutamate*
- **Glutamate excitotoxicity** can occur in chronic alcoholism, particularly during withdrawal, leading to neuronal damage.
- However, the primary insult in Wernicke-Korsakoff syndrome, which this patient's symptoms suggest, is **thiamine deficiency**, impacting the **Krebs cycle** before widespread glutamate release.
*Increased fragmentation of deoxyribonucleic acid within the neurons*
- **DNA fragmentation** indicates significant **neuronal damage** and **apoptosis**, which are later consequences of prolonged metabolic stress and oxidative injury.
- It is not the earliest pathophysiological change but rather a result of the progression of metabolic dysfunction caused by **thiamine deficiency**.
*Breakdown of the blood-brain barrier*
- **Blood-brain barrier (BBB) disruption** can occur in various neurological conditions, including chronic alcoholism, leading to inflammation and edema.
- While BBB dysfunction might contribute to the pathology, the initial and most direct effect of thiamine deficiency is on **cellular energy metabolism** within neurons and astrocytes, preceding widespread BBB breakdown.
Hyperammonemia causes and effects US Medical PG Question 3: A 36-year-old man is brought to the emergency department by his neighbor because of altered mental status. He was found 6 hours ago stumbling through his neighbor's bushes and yelling obscenities. The neighbor helped him home but found him again 1 hour ago slumped over on his driveway in a puddle of vomit. He is oriented to self but not to place or time. His temperature is 36.9°C (98.5°F), pulse is 82/min, respirations are 28/min, and blood pressure is 122/80 mm Hg. Cardiopulmonary exam shows no abnormalities. He is unable to cooperate for a neurological examination. Muscle spasms are seen in his arms and jaw. Serum laboratory studies show:
Na+ 140 mEq/L
K+ 5.5 mEq/L
Cl- 101 mEq/L
HCO3- 9 mEq/L
Urea nitrogen 28 mg/dL
Creatinine 2.3 mg/dL
Glucose 75 mg/dL
Calcium 7.2 mg/dL
Osmolality 320 mOsm/kg
Calculated serum osmolality is 294 mOsm/kg. Arterial blood gas shows a pH of 7.25 and lactate level of 3.2 mmol/L (N=< 1 mmol/L). Examination of the urine shows oxalate crystals and no ketones. This patient is most likely experiencing toxicity from which of the following substances?
- A. Methanol
- B. Ethanol
- C. Ethylene glycol (Correct Answer)
- D. Isopropyl alcohol
- E. Toluene
Hyperammonemia causes and effects Explanation: ***Ethylene glycol***
- The presence of **calcium oxalate crystals** in the urine, a **high anion gap metabolic acidosis** (HCO3- 9 mEq/L, lactate 3.2 mmol/L), and an **elevated osmolal gap** (320 - 294 = 26 mOsm/kg) are classic indicators of ethylene glycol poisoning.
- **Ethylene glycol** is metabolized into toxic compounds like oxalic acid and glycolic acid, which cause kidney damage, metabolic acidosis, and neurological symptoms such as altered mental status and muscle spasms.
*Methanol*
- While methanol poisoning also causes a **high anion gap metabolic acidosis** and an **elevated osmolal gap**, it typically leads to **visual disturbances** (e.g., "snowstorm" vision, blindness) which are not mentioned here.
- The key differentiating factor here is the presence of **oxalate crystals** in the urine, which are characteristic of ethylene glycol, not methanol.
*Ethanol*
- Ethanol intoxication can cause altered mental status but usually does not lead to a **high anion gap metabolic acidosis** unless there is severe co-ingestion or underlying conditions.
- It would not typically cause **oxalate crystals in the urine** or significant **renal failure (creatinine 2.3 mg/dL)** in this acute setting.
*Isopropyl alcohol*
- Isopropyl alcohol causes an **elevated osmolal gap** but typically results in **ketosis without acidosis** (due to its metabolism to acetone).
- It does not produce **oxalate crystals** in the urine or a **high anion gap metabolic acidosis**.
*Toluene*
- Toluene poisoning is associated with a **non-anion gap metabolic acidosis** (renal tubular acidosis) and hypokalemia, which is in contrast to the high anion gap acidosis and hyperkalemia (K+ 5.5 mEq/L) seen in this patient.
- It would not cause **oxalate crystals in the urine** or a significant **osmolal gap**.
Hyperammonemia causes and effects US Medical PG Question 4: A 3-week old boy is brought to the physician for the evaluation of lethargy, recurrent vomiting, and poor weight gain since birth. Physical examination shows decreased skin turgor and a bulging frontal fontanelle. Serum studies show an ammonia concentration of 170 μmol/L (N < 30) and low serum citrulline levels. The oral intake of which of the following nutrients should be restricted in this patient?
- A. Gluten
- B. Lactose
- C. Fructose
- D. Protein (Correct Answer)
- E. Vitamin A
Hyperammonemia causes and effects Explanation: ***Protein***
- Elevated **ammonia** and low **citrulline** levels indicate a **urea cycle disorder**, which impairs the body's ability to excrete nitrogenous waste from protein metabolism.
- Restricting **protein intake** limits the production of ammonia, thereby reducing the toxic burden on the system and preventing further neurological damage.
*Gluten*
- **Gluten restriction** is primarily indicated for **celiac disease**, which presents with gastrointestinal symptoms like diarrhea, malabsorption, and poor weight gain, but not directly with hyperammonemia or urea cycle dysfunction.
- While malabsorption can cause poor weight gain, the specific metabolic derangements here point away from celiac disease.
*Lactose*
- **Lactose intolerance** or **galactosemia** would necessitate **lactose restriction**. Symptoms usually include vomiting, diarrhea, and failure to thrive, but they do not typically present with the extreme hyperammonemia seen here.
- Galactosemia specifically would show elevated galactose and galactose-1-phosphate, not ammonia.
*Fructose*
- **Hereditary fructose intolerance** requires **fructose restriction**. It generally presents with vomiting, hypoglycemia, and liver dysfunction (jaundice, hepatomegaly) upon exposure to fructose, not primarily with hyperammonemia.
- The metabolic pathway for fructose metabolism does not directly generate ammonia in the quantities seen with urea cycle disorders.
*Vitamin A*
- **Vitamin A restriction** is not a primary treatment for any known inborn error of metabolism or hyperammonemia.
- While deficiencies or toxicities of vitamins can occur, they do not present with the specific metabolic profile described (high ammonia, low citrulline).
Hyperammonemia causes and effects US Medical PG Question 5: A 48-year-old man is brought to the emergency department by his wife 20 minutes after she witnessed him vigorously shaking for about 1 minute. During this episode, he urinated on himself. He feels drowsy and has nausea. He has a history of chronic alcoholism; he has been drinking 15 beers daily for the past 3 days. Before this time, he drank 8 beers daily. His last drink was 2 hours ago. He appears lethargic. His vital signs are within normal limits. Physical and neurologic examinations show no other abnormalities. On mental status examination, he is confused and not oriented to time. Laboratory studies show:
Hematocrit 44.0%
Leukocyte count 12,000/mm3
Platelet count 320,000/mm3
Serum
Na+ 112 mEq/L
Cl- 75 mEq/L
K+ 3.8 mEq/L
HCO3- 13 mEq/L
Urea nitrogen 6 mEq/L
Creatinine 0.6 mg/dL
Albumin 2.1 g/dL
Glucose 80 mg/dL
Urgent treatment for this patient's current condition puts him at increased risk for which of the following adverse events?
- A. Cardiac arrhythmia
- B. Osmotic myelinolysis (Correct Answer)
- C. Cerebral edema
- D. Wernicke encephalopathy
- E. Hyperglycemia
Hyperammonemia causes and effects Explanation: **Osmotic myelinolysis**
- The severe **hyponatremia (Na+ 112 mEq/L)** in a chronic alcoholic, likely due to increased ADH from excessive beer intake (beer potomania) and possible malnutrition, places him at risk.
- **Rapid correction** of chronic hyponatremia can cause water to leave brain cells too quickly, leading to **demyelination** of neurons, particularly in the pons.
*Cardiac arrhythmia*
- While severe **electrolyte imbalances** such as hypokalemia or hypomagnesemia can cause cardiac arrhythmias, his potassium is normal, and there's no indication of magnesium deficiency.
- **Alcohol withdrawal** can also cause arrhythmias, but the immediate treatment for his hyponatremia does not directly increase this risk.
*Cerebral edema*
- **Cerebral edema** is a risk of **untreated severe hyponatremia**, where water shifts into brain cells, causing swelling.
- However, the question asks about the risk associated with **urgent treatment** for the condition, which, in this case, would involve raising serum sodium.
*Wernicke encephalopathy*
- **Wernicke encephalopathy** is caused by **thiamine deficiency**, common in chronic alcoholics, and presents with gait ataxia, ophthalmoplegia, and confusion.
- While this patient is at risk, treating hyponatremia does not directly increase the risk of Wernicke encephalopathy; rather, thiamine administration is part of routine care for alcoholics.
*Hyperglycemia*
- **Hyperglycemia** is not a common adverse event of correcting hyponatremia in a patient with a normal blood glucose level.
- Insulin resistance or glucose intolerance might be present in chronic alcoholics, but the urgent treatment for hyponatremia itself does not typically induce hyperglycemia.
Hyperammonemia causes and effects US Medical PG Question 6: A 2-day-old male infant is brought to the emergency department by ambulance after his parents noticed that he was convulsing and unresponsive. He was born at home and appeared well initially; however, within 24 hours he became increasingly irritable and lethargic. Furthermore, he stopped feeding and began to experience worsening tachypnea. This continued for about 6 hours, at which point his parents noticed the convulsions and called for an ambulance. Laboratories are obtained with the following results:
Orotic acid: 9.2 mmol/mol creatinine (normal: 1.4-5.3 mmol/mol creatinine)
Ammonia: 135 µmol/L (normal: < 50 µmol/L)
Citrulline: 2 µmol/L (normal: 10-45 µmol/L)
Which of the following treatments would most likely be beneficial to this patient?
- A. Galactose avoidance
- B. Aspartame avoidance
- C. Benzoate administration (Correct Answer)
- D. Uridine administration
- E. Fructose avoidance
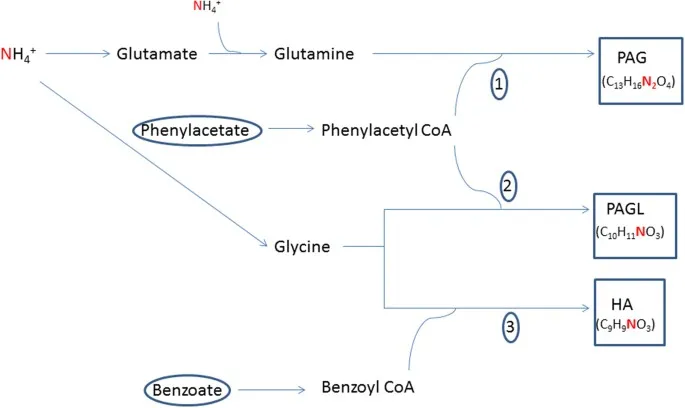
Hyperammonemia causes and effects Explanation: ***Benzoate administration***
- This patient presents with hyperammonemia (135 µmol/L), elevated orotic acid (9.2 mmol/mol creatinine), and **low citrulline (2 µmol/L)**, which is the classic triad for **ornithine transcarbamylase (OTC) deficiency**.
- The low citrulline distinguishes OTC deficiency from other urea cycle defects, while elevated orotic acid results from accumulation of carbamoyl phosphate that gets shunted into pyrimidine synthesis.
- **Sodium benzoate** is a nitrogen scavenger that conjugates with glycine to form hippurate, which is excreted renally, providing an alternative pathway for nitrogen disposal and reducing toxic ammonia levels.
- This is a life-saving acute treatment for hyperammonemia in urea cycle disorders.
*Galactose avoidance*
- This is the treatment for **galactosemia**, a disorder of galactose metabolism caused by galactose-1-phosphate uridyltransferase deficiency.
- Galactosemia presents with hepatomegaly, jaundice, cataracts, intellectual disability, and hypoglycemia after milk feeding.
- The patient's hyperammonemia and elevated orotic acid pattern is incompatible with galactosemia.
*Aspartame avoidance*
- This is relevant for **phenylketonuria (PKU)** dietary management, as aspartame contains phenylalanine.
- PKU presents with developmental delay, intellectual disability, musty odor, and eczema, with elevated phenylalanine levels.
- Ammonia and orotic acid are normal in PKU, making this diagnosis inconsistent with the lab findings.
*Uridine administration*
- **Uridine** treats **hereditary orotic aciduria** (UMP synthase deficiency), which presents with megaloblastic anemia, growth retardation, and developmental delays.
- While orotic acid is elevated in both conditions, hereditary orotic aciduria has **normal ammonia** and the primary pathology is impaired pyrimidine synthesis, not ammonia disposal.
- This patient's life-threatening hyperammonemia requires immediate nitrogen scavenging, which uridine does not provide.
*Fructose avoidance*
- This treats **hereditary fructose intolerance** (aldolase B deficiency), which causes hypoglycemia, vomiting, hepatomegaly, and jaundice after fructose ingestion.
- The presentation is triggered by dietary fructose exposure and does not cause hyperammonemia or elevated orotic acid.
- The patient's metabolic profile is inconsistent with a fructose metabolism disorder.
Hyperammonemia causes and effects US Medical PG Question 7: A 36-year-old man is brought to the emergency department by his girlfriend because of increasing confusion for the past 6 hours. He drinks large amounts of alcohol daily and occasionally uses illicit drugs. He is lethargic and oriented only to person. Physical examination shows jaundice, hepatomegaly, and scattered petechiae over the trunk and back. Neurologic examination shows normal, reactive pupils and a flapping tremor when the wrists are extended. A drug with which of the following mechanism of action would be most appropriate for this patient's condition?
- A. Production of NH3
- B. Activation of GABA receptors
- C. Excretion of free iron
- D. Inhibition of D2 receptors
- E. Excretion of NH4 (Correct Answer)
Hyperammonemia causes and effects Explanation: ***Excretion of NH4***
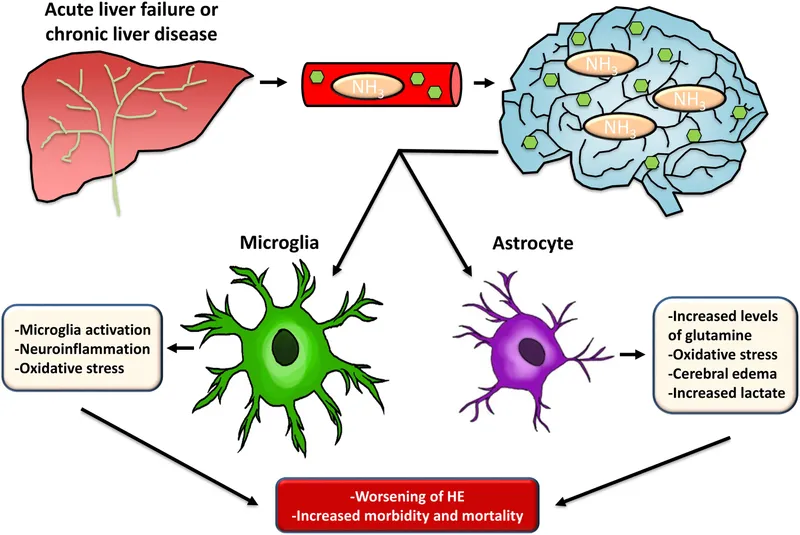
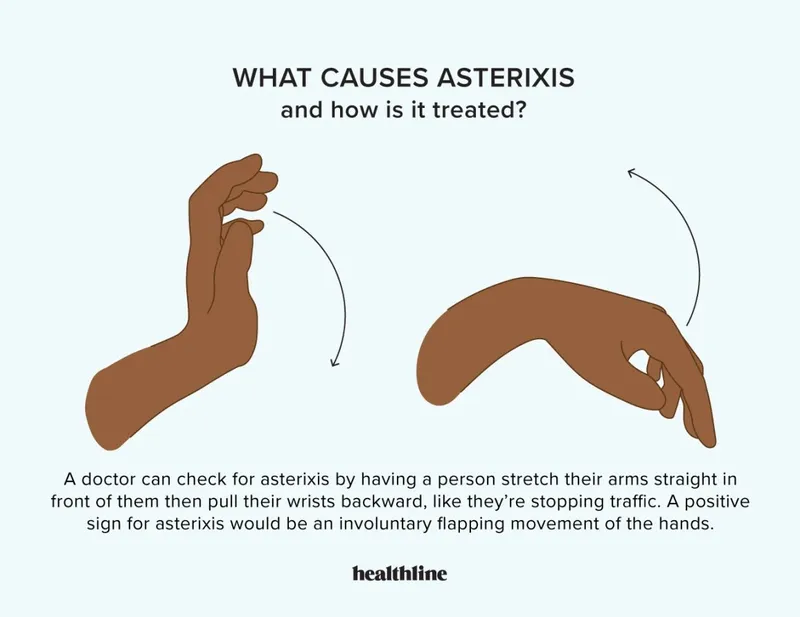
- The patient presents with **hepatic encephalopathy**, characterized by **confusion**, **jaundice**, **hepatomegaly**, **petechiae**, and a **flapping tremor (asterixis)**, stemming from chronic alcohol abuse and liver damage. The main pathophysiology in hepatic encephalopathy is the accumulation of **ammonia (NH3)**, which is neurotoxic.
- Excretion of **NH4** (ammonium) through drug mechanisms such as **lactulose** (which acidifies the colon, trapping ammonia as ammonium for excretion) is the primary therapeutic target to reduce ammonia levels and improve neurological symptoms.
*Production of NH3*
- This mechanism would exacerbate the patient's condition by increasing the toxic load of **ammonia (NH3)**, which is already elevated in hepatic encephalopathy.
- Therapeutic interventions aim to decrease, not increase, ammonia production or absorption.
*Activation of GABA receptors*
- While **GABA receptor activation** is involved in the neurological effects of some substances that contribute to confusion, it is not the primary target for treating the underlying pathophysiology of **hepatic encephalopathy**.
- Medications that activate GABA receptors (e.g., benzodiazepines) can worsen encephalopathy by further depressing CNS function.
*Excretion of free iron*
- **Iron overload** can cause liver damage, but the acute confusion and flapping tremor are more indicative of **hepatic encephalopathy** due to ammonia toxicity, not primarily iron accumulation.
- Excreting free iron (e.g., with chelation therapy) is for conditions like hemochromatosis and would not address the immediate, life-threatening neurological symptoms in this patient.
*Inhibition of D2 receptors*
- This mechanism is characteristic of some **antipsychotic medications**. While dopamine imbalances can play a role in some neurological disorders, inhibiting D2 receptors is not a primary therapeutic target for **hepatic encephalopathy**.
- Such medications could have side effects that might complicate the clinical picture in a patient with acute liver failure.
Hyperammonemia causes and effects US Medical PG Question 8: A newborn boy develops projectile vomiting 48 hours after delivery. He is found to be lethargic, with poor muscle tone, and is hyperventilating. Within hours, he suffers important neurological deterioration, leading to seizures, coma, and, ultimately, death. An autopsy is performed and the pathology team makes a diagnosis of a rare genetic disorder that leads to low levels of N-acetylglutamate. Which of the following enzymes would be secondarily affected by this process?
- A. Argininosuccinate lyase
- B. Carbamoyl phosphate synthetase I (Correct Answer)
- C. Argininosuccinate synthetase
- D. Ornithine transcarbamylase
- E. Arginase
Hyperammonemia causes and effects Explanation: ***Carbamoyl phosphate synthetase I***
- **N-acetylglutamate** is an **obligate activator** for **Carbamoyl phosphate synthetase I (CPS I)**, the rate-limiting enzyme of the **urea cycle**. Low levels of N-acetylglutamate directly impair CPS I activity.
- Reduced CPS I activity leads to a severe **urea cycle disorder**, causing **hyperammonemia**, which manifests with lethargy, poor muscle tone, hyperventilation, neurological deterioration, seizures, coma, and death in newborns.
*Argininosuccinate lyase*
- This enzyme is involved downstream in the **urea cycle**, catalyzing the cleavage of **argininosuccinate** into **arginine** and **fumarate**.
- Its activity is not directly regulated by **N-acetylglutamate**, so it would not be secondarily affected in the same manner as CPS I.
*Argininosuccinate synthetase*
- This enzyme acts after CPS I and ornithine transcarbamylase in the **urea cycle**, synthesizing **argininosuccinate** from **citrulline** and **aspartate**.
- Its function is independent of **N-acetylglutamate** levels, making it unlikely to be secondarily affected.
*Ornithine transcarbamylase*
- This enzyme catalyzes the second step of the **urea cycle**, forming **citrulline** from **ornithine** and **carbamoyl phosphate**.
- While essential for the urea cycle, its activity is not directly modulated by **N-acetylglutamate**; rather, it depends on the availability of carbamoyl phosphate produced by CPS I.
*Arginase*
- This is the final enzyme in the **urea cycle**, converting **arginine** to **ornithine** and **urea**.
- Its activity is not directly or indirectly regulated by **N-acetylglutamate**, nor is it the enzyme primarily affected in this presentation.
Hyperammonemia causes and effects US Medical PG Question 9: A 4-day-old boy is brought to the physician because of somnolence, poor feeding, and vomiting after his first few breast feedings. He appears lethargic. His respiratory rate is 73/min. Serum ammonia is markedly increased. Genetic analysis shows deficiency in N-acetylglutamate synthase. The activity of which of the following enzymes is most likely directly affected by this genetic defect?
- A. Ornithine translocase
- B. Carbamoyl phosphate synthetase I (Correct Answer)
- C. Argininosuccinase
- D. Argininosuccinate synthetase
- E. Arginase
Hyperammonemia causes and effects Explanation: ***Carbamoyl phosphate synthetase I***
- **N-acetylglutamate** (NAG) is an essential allosteric activator of **carbamoyl phosphate synthetase I (CPS I)**, the rate-limiting enzyme of the urea cycle.
- A deficiency in **N-acetylglutamate synthase** directly leads to a lack of NAG, significantly impairing CPS I activity and causing severe hyperammonemia.
*Ornithine translocase*
- This enzyme is responsible for transporting **ornithine** into the mitochondria for the urea cycle.
- While a defect in **ornithine translocase** also causes hyperammonemia, it is due to accumulation of ornithine and upstream substrates, not a defect in N-acetylglutamate synthase.
*Argininosuccinase*
- Also known as **argininosuccinate lyase**, this enzyme cleaves argininosuccinate into arginine and fumarate.
- A deficiency would lead to accumulation of **argininosuccinate**, and while it is a urea cycle disorder, it is not directly affected by N-acetylglutamate synthase deficiency.
*Argininosuccinate synthetase*
- This enzyme catalyzes the condensation of **citrulline** and **aspartate** to form argininosuccinate.
- A defect in **argininosuccinate synthetase** causes citrullinemia but is not directly regulated by N-acetylglutamate.
*Arginase*
- **Arginase** is the final enzyme in the urea cycle, hydrolyzing arginine to form urea and ornithine.
- A deficiency would lead to hyperargininemia, which typically presents later in childhood and is not directly affected by N-acetylglutamate.
Hyperammonemia causes and effects US Medical PG Question 10: A 4-year-old girl is brought to the physician by her mother because of fatigue and generalized weakness for 4 months. Examination shows decreased muscle tone. Her fasting serum glucose concentration is 41 mg/dL. The physician suspects a defect in one of the enzymes involved in the carnitine shuttle. Increased serum concentration of which of the following should most raise suspicion of a different diagnosis?
- A. Ammonia (Correct Answer)
- B. Creatine kinase
- C. Alanine aminotransferase
- D. Uric acid
- E. β-hydroxybutyrate
Hyperammonemia causes and effects Explanation: ***Ammonia***
- An elevated **ammonia** level in the context of hypoglycemia and muscle weakness in a child suggests an **inborn error of metabolism** that affects the **urea cycle** or **organic acidemia**, not primarily the carnitine shuttle.
- Urea cycle disorders lead to **hyperammonemia**, which can cause neurological symptoms, fatigue, and muscle weakness, often exacerbated by catabolic states.
- This finding would **strongly suggest a different diagnosis** from a carnitine shuttle defect.
*Creatine kinase*
- **Creatine kinase (CK)** levels are typically **elevated in carnitine shuttle defects** due to muscle damage and myopathy.
- Elevated CK would **support** the suspected diagnosis of a carnitine shuttle defect rather than suggest an alternative.
- This is an **expected finding** in fatty acid oxidation disorders.
*Alanine aminotransferase*
- **Alanine aminotransferase (ALT)** can be elevated in **carnitine shuttle defects** due to liver involvement and hepatic dysfunction.
- While elevated ALT indicates liver damage, it can occur in fatty acid oxidation disorders and would not necessarily point away from a carnitine shuttle defect.
- This finding is **consistent with** rather than against the suspected diagnosis.
*Uric acid*
- **Uric acid** levels are not directly affected by defects in the **carnitine shuttle**.
- While an elevated uric acid level might prompt investigation into conditions like **glycogen storage diseases** or purine metabolism disorders, it is not a strong discriminator for alternative diagnoses in this clinical context.
*β-hydroxybutyrate*
- **β-hydroxybutyrate** is a **ketone body** produced from fatty acid oxidation during fasting states.
- In carnitine shuttle defects, the body **cannot effectively oxidize fatty acids** to produce ketones, resulting in **hypoketotic hypoglycemia** (low or inappropriately low ketones despite low glucose).
- If β-hydroxybutyrate is **elevated** during fasting hypoglycemia, this indicates **intact fatty acid oxidation** and would suggest a different diagnosis such as **hyperinsulinism**, **glycogen storage disease**, or other causes of hypoglycemia where ketogenesis is preserved.
- However, **ammonia elevation** is a stronger indicator of an alternative diagnosis (urea cycle disorder) compared to the scenario presented.
More Hyperammonemia causes and effects US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.