Alternative nitrogen excretion pathways US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Alternative nitrogen excretion pathways. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Alternative nitrogen excretion pathways US Medical PG Question 1: A 61-year-old male is given acetazolamide to treat open-angle glaucoma. Upon diuresis, his urine is found to be highly alkaline. Which of the following accounts for the alkaline nature of this patient’s urine?
- A. Inhibition of bicarbonate reabsorption in the proximal tubule (Correct Answer)
- B. Inhibition of bicarbonate reabsorption in beta-intercalated cells
- C. Inhibition of acid secretion in alpha-intercalated cells
- D. Inhibition of chloride reabsorption in the distal convoluted tubule
- E. Inhibition of chloride reabsorption in the thick ascending loop of Henle
Alternative nitrogen excretion pathways Explanation: ***Inhibition of bicarbonate reabsorption in the proximal tubule***
- **Acetazolamide** is a **carbonic anhydrase inhibitor** that primarily acts on the **proximal tubule** of the kidney.
- Its action here prevents the reabsorption of **bicarbonate (HCO3-)**, leading to its increased excretion in the urine and thus making the urine alkaline.
*Inhibition of chloride reabsorption in the distal convoluted tubule*
- This effect is typically associated with **thiazide diuretics**, which inhibit the **Na-Cl cotransporter** in the distal convoluted tubule.
- While it affects electrolyte balance, it does not directly lead to the observed **alkaline urine** in the manner described.
*Inhibition of bicarbonate reabsorption in beta-intercalated cells*
- **Beta-intercalated cells** in the collecting duct secrete bicarbonate, and their inhibition would lead to **acidic urine**, not alkaline.
- They play a role in **bicarbonate secretion**, not reabsorption as seen with acetazolamide's primary action.
*Inhibition of acid secretion in alpha-intercalated cells*
- **Alpha-intercalated cells** secrete acid (H+) into the urine. Inhibiting their function would reduce acid excretion, making the urine less acidic or even alkaline.
- However, the primary mechanism of acetazolamide's effect on urine pH is through **bicarbonate wasting** in the proximal tubule, not direct inhibition of acid secretion in the collecting duct.
*Inhibition of chloride reabsorption in the thick ascending loop of Henle*
- This is the mechanism of action for **loop diuretics** like furosemide, which inhibit the **Na-K-2Cl cotransporter**.
- While loop diuretics cause significant diuresis, they do not directly lead to the pronounced **urinary alkalinization** seen with acetazolamide.
Alternative nitrogen excretion pathways US Medical PG Question 2: Which region of the nephron reabsorbs the highest percentage of filtered bicarbonate?
- A. Collecting duct
- B. Thick ascending limb
- C. Distal tubule
- D. Proximal tubule (Correct Answer)
Alternative nitrogen excretion pathways Explanation: ***Proximal tubule***
- The **proximal convoluted tubule (PCT)** reabsorbs approximately 80-90% of the **filtered bicarbonate** through a process involving **carbonic anhydrase** and the **Na+/H+ exchanger**.
- This vital function ensures that the majority of bicarbonate, a key buffer, is returned to the blood to maintain **acid-base balance**.
*Collecting duct*
- While the collecting duct does have the ability to reabsorb and secrete bicarbonate, its contribution is minor compared to the PCT, primarily for fine-tuning acid-base balance.
- Cells in the collecting duct, particularly **Type A intercalated cells**, are important for secreting acid (H+) in acidosis and therefore reabsorbing bicarbonate, but not the bulk of it.
*Thick ascending limb*
- The primary role of the **thick ascending limb** is the reabsorption of **sodium**, **potassium**, and **chloride** to create a concentrated interstitium, not significant bicarbonate reabsorption.
- It is largely impermeable to water and is relatively impermeable to bicarbonate.
*Distal tubule*
- The **distal convoluted tubule (DCT)** reabsorbs a small percentage of filtered bicarbonate, but its main role is regulated reabsorption of **sodium** and **calcium**, and secretion of **potassium** and **hydrogen ions**.
- Its contribution to bicarbonate reabsorption is much less significant than that of the proximal tubule.
Alternative nitrogen excretion pathways US Medical PG Question 3: You are examining a 3-day-old newborn who was delivered vaginally without any complications. The newborn presents with vomiting, hyperventilation, lethargy, and seizures. Blood work demonstrates hyperammonemia, elevated glutamine levels, and decreased blood urea nitrogen. A CT scan demonstrates cerebral edema. Defects in which of the following enzymes would result in a clinical presentation similar to this infant?
- A. Carbamoyl phosphate synthetase I (Correct Answer)
- B. Homogentisate oxidase
- C. Cystathionine synthase
- D. Branched-chain ketoacid dehydrogenase
- E. Phenylalanine hydroxylase
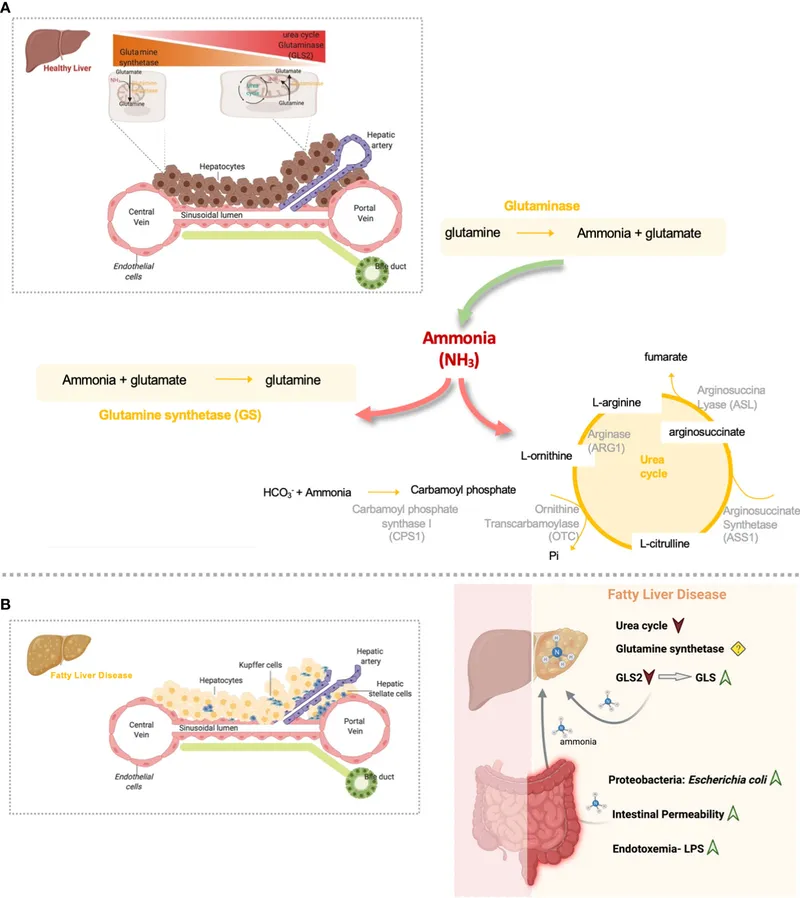
Alternative nitrogen excretion pathways Explanation: **Carbamoyl phosphate synthetase I**
- **Carbamoyl phosphate synthetase I (CPSI)** deficiency is a severe **urea cycle disorder** that typically presents in the neonatal period with **hyperammonemia**, **vomiting**, **lethargy**, **seizures**, and **hyperventilation**.
- The enzyme CPSI catalyzes the first step of the urea cycle, which is crucial for detoxifying ammonia, leading to **elevated glutamine** and **decreased blood urea nitrogen** when defective.
*Homogentisate oxidase*
- Deficiency in **homogentisate oxidase** causes **alkaptonuria**, a disorder of tyrosine metabolism.
- This condition is characterized by **dark urine** upon standing, **ochronosis** (bluish-black discoloration of cartilage and connective tissue later in life), and **arthropathy**, not hyperammonemia or acute neonatal crisis.
*Cystathionine synthase*
- A defect in **cystathionine synthase** leads to **homocystinuria**, an inherited disorder of methionine metabolism.
- Symptoms include **ectopia lentis**, **skeletal abnormalities**, **thromboembolic events**, and **developmental delay**, not acute neonatal hyperammonemic encephalopathy.
*Branched-chain ketoacid dehydrogenase*
- Deficiency in **branched-chain ketoacid dehydrogenase** causes **maple syrup urine disease (MSUD)**, a disorder of branched-chain amino acid metabolism.
- While it can present with vomiting, lethargy, and seizures in neonates, it is characterized by a distinctive **maple syrup odor** in urine and elevated branched-chain amino acids, not hyperammonemia and low BUN.
*Phenylalanine hydroxylase*
- A deficiency in **phenylalanine hydroxylase** causes **phenylketonuria (PKU)**, an amino acid metabolism disorder.
- PKU typically presents with intellectual disability, seizures, and a musty odor if untreated, but generally does not manifest as an acute neonatal crisis with hyperammonemia, as seen in urea cycle defects.
Alternative nitrogen excretion pathways US Medical PG Question 4: A 4-day-old male newborn delivered at 39 weeks' gestation is evaluated because of poor feeding, recurrent vomiting, and lethargy. Physical examination shows tachypnea with subcostal retractions. An enzyme assay performed on a liver biopsy specimen shows decreased activity of carbamoyl phosphate synthetase I. This enzyme plays an important role in the breakdown and excretion of amino groups that result from protein digestion. Which of the following is an immediate substrate for the synthesis of the molecule needed for the excretion of amino groups?
- A. N-acetylglutamate
- B. Homocysteine
- C. Phenylalanine
- D. Valine
- E. Aspartate (Correct Answer)
Alternative nitrogen excretion pathways Explanation: ***Aspartate***
- The question describes a case of **carbamoyl phosphate synthetase I (CPS I)** deficiency, which leads to **hyperammonemia** due to impaired urea cycle function.
- The urea cycle is responsible for excreting **amino groups** as urea; one of the key molecules directly incorporated into the urea molecule is **aspartate**, which donates an amino group to form **argininosuccinate**.
*N-acetylglutamate*
- **N-acetylglutamate** is an essential activator of **carbamoyl phosphate synthetase I (CPS I)**, the enzyme deficient in this patient.
- While crucial for the urea cycle's regulation, it is an **allosteric activator** rather than a direct substrate for the synthesis of molecules needed for amino group excretion.
*Homocysteine*
- **Homocysteine** is an intermediate in **methionine metabolism** and is primarily associated with cardiovascular disease and neurological issues when elevated.
- It plays no direct role as a substrate in the urea cycle for the excretion of amino groups.
*Phenylalanine*
- **Phenylalanine** is an **essential amino acid** that is a precursor to tyrosine and neurotransmitters.
- Its metabolism is separate from the urea cycle, and it is not a direct substrate for ammonia excretion in this pathway.
*Valine*
- **Valine** is a **branched-chain amino acid (BCAA)** primarily catabolized in muscles and used for energy.
- It is not a direct substrate in the urea cycle, which processes nitrogen from various amino acids into urea for excretion.
Alternative nitrogen excretion pathways US Medical PG Question 5: A 2-day-old male infant is brought to the emergency department by ambulance after his parents noticed that he was convulsing and unresponsive. He was born at home and appeared well initially; however, within 24 hours he became increasingly irritable and lethargic. Furthermore, he stopped feeding and began to experience worsening tachypnea. This continued for about 6 hours, at which point his parents noticed the convulsions and called for an ambulance. Laboratories are obtained with the following results:
Orotic acid: 9.2 mmol/mol creatinine (normal: 1.4-5.3 mmol/mol creatinine)
Ammonia: 135 µmol/L (normal: < 50 µmol/L)
Citrulline: 2 µmol/L (normal: 10-45 µmol/L)
Which of the following treatments would most likely be beneficial to this patient?
- A. Galactose avoidance
- B. Aspartame avoidance
- C. Benzoate administration (Correct Answer)
- D. Uridine administration
- E. Fructose avoidance
Alternative nitrogen excretion pathways Explanation: ***Benzoate administration***
- This patient presents with hyperammonemia (135 µmol/L), elevated orotic acid (9.2 mmol/mol creatinine), and **low citrulline (2 µmol/L)**, which is the classic triad for **ornithine transcarbamylase (OTC) deficiency**.
- The low citrulline distinguishes OTC deficiency from other urea cycle defects, while elevated orotic acid results from accumulation of carbamoyl phosphate that gets shunted into pyrimidine synthesis.
- **Sodium benzoate** is a nitrogen scavenger that conjugates with glycine to form hippurate, which is excreted renally, providing an alternative pathway for nitrogen disposal and reducing toxic ammonia levels.
- This is a life-saving acute treatment for hyperammonemia in urea cycle disorders.
*Galactose avoidance*
- This is the treatment for **galactosemia**, a disorder of galactose metabolism caused by galactose-1-phosphate uridyltransferase deficiency.
- Galactosemia presents with hepatomegaly, jaundice, cataracts, intellectual disability, and hypoglycemia after milk feeding.
- The patient's hyperammonemia and elevated orotic acid pattern is incompatible with galactosemia.
*Aspartame avoidance*
- This is relevant for **phenylketonuria (PKU)** dietary management, as aspartame contains phenylalanine.
- PKU presents with developmental delay, intellectual disability, musty odor, and eczema, with elevated phenylalanine levels.
- Ammonia and orotic acid are normal in PKU, making this diagnosis inconsistent with the lab findings.
*Uridine administration*
- **Uridine** treats **hereditary orotic aciduria** (UMP synthase deficiency), which presents with megaloblastic anemia, growth retardation, and developmental delays.
- While orotic acid is elevated in both conditions, hereditary orotic aciduria has **normal ammonia** and the primary pathology is impaired pyrimidine synthesis, not ammonia disposal.
- This patient's life-threatening hyperammonemia requires immediate nitrogen scavenging, which uridine does not provide.
*Fructose avoidance*
- This treats **hereditary fructose intolerance** (aldolase B deficiency), which causes hypoglycemia, vomiting, hepatomegaly, and jaundice after fructose ingestion.
- The presentation is triggered by dietary fructose exposure and does not cause hyperammonemia or elevated orotic acid.
- The patient's metabolic profile is inconsistent with a fructose metabolism disorder.
Alternative nitrogen excretion pathways US Medical PG Question 6: A 2-week-old boy presents to the emergency department because of unusual irritability and lethargy. The patient is admitted to the pediatric intensive care unit and minutes later develops metabolic encephalopathy. This progressed to a coma, followed by death before any laboratory tests are completed. The infant was born at home via vaginal delivery at 39 weeks' of gestation. His mother says that the symptoms started since the infant was 4-days-old, but since he only seemed ‘tired’, she decided not to seek medical attention. Further testing during autopsy shows hyperammonemia, low citrulline, and increased orotic acid. Which of the following enzymes is most likely deficient in this patient?
- A. Branched-chain alpha-ketoacid dehydrogenase
- B. Propionyl-CoA carboxylase
- C. Homogentisic acid dioxygenase
- D. Ornithine transcarbamylase (Correct Answer)
- E. Cystathionine beta-synthase
Alternative nitrogen excretion pathways Explanation: **Ornithine transcarbamylase**
- **Hyperammonemia**, **low citrulline**, and **increased orotic acid** are classic findings in **Ornithine Transcarbamylase (OTC) deficiency**. OTC is an X-linked urea cycle disorder.
- The rapid progression to **metabolic encephalopathy** and death in a neonate with these laboratory findings is highly characteristic of severe OTC deficiency, often presenting in the first few days of life.
*Branched-chain alpha-ketoacid dehydrogenase*
- Deficiency of this enzyme causes **Maple Syrup Urine Disease**, characterized by elevated **branched-chain amino acids** and their corresponding ketoacids in blood and urine.
- While it can cause neurological symptoms, it does not typically present with the specific constellation of **hyperammonemia**, low citrulline, and high orotic acid.
*Propionyl-CoA carboxylase*
- Deficiency of this enzyme leads to **Propionic acidemia**, a type of organic acidemia, characterized by **propionic acid accumulation** and often **metabolic acidosis**, ketosis, and hyperammonemia.
- However, it would not typically cause **low citrulline** or isolated **elevated orotic acid** as seen in urea cycle disorders.
*Homogentisic acid dioxygenase*
- Deficiency of this enzyme causes **Alkaptonuria**, an inborn error of metabolism characterized by the accumulation of **homogentisic acid**.
- This condition is usually benign in infancy, with symptoms appearing later in life such as **dark urine** on standing and **ochronosis** (darkening of cartilage). It does not present with acute hyperammonemia or metabolic encephalopathy.
*Cystathionine beta-synthase*
- Deficiency of this enzyme causes **homocystinuria**, an inborn error of methionine metabolism, leading to elevated **homocysteine** and methionine.
- Clinical features include **ectopia lentis**, skeletal abnormalities, and intellectual disability, but not usually acute neonatal hyperammonemia or the specific findings of low citrulline and high orotic acid.
Alternative nitrogen excretion pathways US Medical PG Question 7: A 4-day-old boy is brought to the physician because of somnolence, poor feeding, and vomiting after his first few breast feedings. He appears lethargic. His respiratory rate is 73/min. Serum ammonia is markedly increased. Genetic analysis shows deficiency in N-acetylglutamate synthase. The activity of which of the following enzymes is most likely directly affected by this genetic defect?
- A. Ornithine translocase
- B. Carbamoyl phosphate synthetase I (Correct Answer)
- C. Argininosuccinase
- D. Argininosuccinate synthetase
- E. Arginase
Alternative nitrogen excretion pathways Explanation: ***Carbamoyl phosphate synthetase I***
- **N-acetylglutamate** (NAG) is an essential allosteric activator of **carbamoyl phosphate synthetase I (CPS I)**, the rate-limiting enzyme of the urea cycle.
- A deficiency in **N-acetylglutamate synthase** directly leads to a lack of NAG, significantly impairing CPS I activity and causing severe hyperammonemia.
*Ornithine translocase*
- This enzyme is responsible for transporting **ornithine** into the mitochondria for the urea cycle.
- While a defect in **ornithine translocase** also causes hyperammonemia, it is due to accumulation of ornithine and upstream substrates, not a defect in N-acetylglutamate synthase.
*Argininosuccinase*
- Also known as **argininosuccinate lyase**, this enzyme cleaves argininosuccinate into arginine and fumarate.
- A deficiency would lead to accumulation of **argininosuccinate**, and while it is a urea cycle disorder, it is not directly affected by N-acetylglutamate synthase deficiency.
*Argininosuccinate synthetase*
- This enzyme catalyzes the condensation of **citrulline** and **aspartate** to form argininosuccinate.
- A defect in **argininosuccinate synthetase** causes citrullinemia but is not directly regulated by N-acetylglutamate.
*Arginase*
- **Arginase** is the final enzyme in the urea cycle, hydrolyzing arginine to form urea and ornithine.
- A deficiency would lead to hyperargininemia, which typically presents later in childhood and is not directly affected by N-acetylglutamate.
Alternative nitrogen excretion pathways US Medical PG Question 8: A 17-year-old boy is brought to the physician by his father because of a 7-month history of fatigue, recurrent leg cramps, and increased urinary frequency. His pulse is 94/min and blood pressure is 118/85 mm Hg. Physical examination shows dry mucous membranes. Laboratory studies show:
Serum
Na+ 130 mEq/L
K+ 2.8 mEq/L
Cl- 92 mEq/L
Mg2+ 1.1 mEq/L
Ca2+ 10.6 mg/dL
Albumin 5.2 g/dL
Urine
Ca2+ 70 mg/24 h
Cl- 375 mEq/24h (N = 110–250)
Arterial blood gas analysis on room air shows a pH of 7.55 and an HCO3- concentration of 45 mEq/L. Impaired function of which of the following structures is the most likely cause of this patient's condition?
- A. Ascending loop of Henle
- B. Collecting duct
- C. Distal convoluted tubule (Correct Answer)
- D. Descending loop of Henle
- E. Proximal convoluted tubule
Alternative nitrogen excretion pathways Explanation: ***Distal convoluted tubule***
- The patient presents with **hypokalemia**, **metabolic alkalosis**, **hypomagnesemia**, and **hypocalciuria** (24-hour urine Ca2+ 70 mg, normal up to 250 mg), which are characteristic findings of **Gitelman syndrome**.
- **Gitelman syndrome** is caused by a loss-of-function mutation in the **thiazide-sensitive Na-Cl cotransporter (NCC)**, located in the **distal convoluted tubule**, leading to impaired reabsorption of Na+ and Cl- at this segment.
*Ascending loop of Henle*
- Impaired function of the **Na-K-2Cl cotransporter (NKCC2)** in the **thick ascending limb of the loop of Henle** causes **Bartter syndrome**.
- Bartter syndrome typically presents with **hypercalciuria**, in contrast to the hypocalciuria seen in this patient.
*Collecting duct*
- Dysfunction of the **collecting duct** can lead to various conditions, such as **renal tubular acidosis** or **diabetes insipidus**, depending on which channels or receptors are affected.
- However, the specific combination of **hypokalemia**, **metabolic alkalosis**, **hypomagnesemia**, and **hypocalciuria** points away from primary collecting duct dysfunction.
*Descending loop of Henle*
- The **descending loop of Henle** is primarily permeable to **water** and has a limited role in electrolyte reabsorption.
- Impairment here would primarily affect **urine concentration** and dilution but would not account for the specific electrolyte imbalances observed.
*Proximal convoluted tubule*
- The **proximal convoluted tubule** is responsible for reabsorbing a large fraction of filtered electrolytes, glucose, and amino acids.
- Dysfunction here (e.g., **Fanconi syndrome**) would typically present with **generalized aminoaciduria**, **glycosuria**, **phosphaturia**, and **proximal renal tubular acidosis**, which are not seen in this patient.
Alternative nitrogen excretion pathways US Medical PG Question 9: An investigator is studying severely ill patients who experience hypoglycemia and ketonuria during times of fasting. The investigator determines that during these episodes, amino acids liberated from muscle proteins are metabolized to serve as substrates for gluconeogenesis. Nitrogen from this process is transported to the liver primarily in the form of which of the following molecules?
- A. Glutamate
- B. α-ketoglutarate
- C. Alanine (Correct Answer)
- D. Arginine
- E. Pyruvate
Alternative nitrogen excretion pathways Explanation: ***Alanine***
- During prolonged fasting, **muscle proteins are catabolized** to provide amino acids for gluconeogenesis in the liver.
- **Alanine** is the primary amino acid released from muscle into the bloodstream to transport nitrogen to the liver through the **glucose-alanine cycle (Cahill cycle)**.
- In this cycle, pyruvate in muscle accepts an amino group from glutamate to form alanine, which is then transported to the liver, where it is deaminated back to pyruvate (for gluconeogenesis) and ammonia (for the urea cycle).
- **Glutamine** also serves as an important nitrogen transporter, particularly to the kidneys and intestines.
*Glutamate*
- **Glutamate** is an important amino acid in nitrogen metabolism within tissues, but it is not the primary form in which nitrogen is transported from muscle to the liver in significant quantities.
- While glutamate participates in transamination reactions within muscle, its efflux from muscle into the blood is less prominent than alanine for inter-organ nitrogen transport.
*α-ketoglutarate*
- **α-ketoglutarate** is a key intermediate in the **Krebs cycle** and accepts an amino group to form glutamate.
- It is an alpha-keto acid, not an amino acid, and therefore does not directly transport nitrogen in the form of an amino group to the liver via the bloodstream.
*Arginine*
- **Arginine** is primarily involved in the **urea cycle** within the liver, where it helps in the detoxification of ammonia, but it is not a major transporter of nitrogen from peripheral tissues to the liver for gluconeogenesis.
- Its role is mainly within the liver for urea synthesis, not for inter-organ nitrogen transport in this context.
*Pyruvate*
- **Pyruvate** is a keto acid that can be converted to alanine via transamination.
- While pyruvate is a precursor to alanine and a substrate for gluconeogenesis, it transports carbon skeletons and not nitrogen itself; **alanine is the actual nitrogen carrier** in this cycle.
Alternative nitrogen excretion pathways US Medical PG Question 10: An 8-year-old boy is brought to the pediatrician by his mother with nausea, vomiting, and decreased frequency of urination. He has acute lymphoblastic leukemia for which he received the 1st dose of chemotherapy 5 days ago. His leukocyte count was 60,000/mm3 before starting chemotherapy. The vital signs include: pulse 110/min, temperature 37.0°C (98.6°F), and blood pressure 100/70 mm Hg. The physical examination shows bilateral pedal edema. Which of the following serum studies and urinalysis findings will be helpful in confirming the diagnosis of this condition?
- A. Hyperuricemia, hyperkalemia, hyperphosphatemia, and urinary monoclonal spike
- B. Hyperkalemia, hyperphosphatemia, hypocalcemia, hyperuricemia, urine supernatant pink, and positive for heme
- C. Hyperkalemia, hyperphosphatemia, hypocalcemia, and extremely elevated creatine kinase (MM)
- D. Hyperuricemia, hyperkalemia, hyperphosphatemia, lactic acidosis, and oxalate crystals
- E. Hyperuricemia, hyperkalemia, hyperphosphatemia, hypocalcemia, and urate crystals in the urine (Correct Answer)
Alternative nitrogen excretion pathways Explanation: ***Hyperuricemia, hyperkalemia, hyperphosphatemia, hypocalcemia, and urate crystals in the urine***
- This patient's presentation following chemotherapy, particularly with a high pre-treatment leukocyte count, is highly suggestive of **tumor lysis syndrome (TLS)**. TLS is characterized by rapid tumor cell breakdown, releasing intracellular contents into the bloodstream.
- The **four cardinal laboratory findings** of TLS are **hyperuricemia** (from nucleic acid breakdown), **hyperkalemia** (from intracellular potassium release), **hyperphosphatemia** (from intracellular phosphate release), and **hypocalcemia** (secondary to calcium-phosphate precipitation). The presence of **urate crystals in the urine** confirms the renal effects of uric acid overload, leading to acute kidney injury.
*Hyperuricemia, hyperkalemia, hyperphosphatemia, and urinary monoclonal spike*
- While **hyperuricemia, hyperkalemia, and hyperphosphatemia** are consistent with tumor lysis syndrome, a **urinary monoclonal spike** is typically associated with multiple myeloma or other plasma cell dyscrasias, not tumor lysis syndrome.
- The patient's history of acute lymphoblastic leukemia and recent chemotherapy points away from a monoclonal gammopathy.
- This option is also missing the key finding of **hypocalcemia**.
*Hyperkalemia, hyperphosphatemia, hypocalcemia, hyperuricemia, urine supernatant pink, and positive for heme*
- **Hyperkalemia, hyperphosphatemia, hyperuricemia, and hypocalcemia** are indeed the four cardinal metabolic abnormalities of TLS. However, a **pink urine supernatant and positive heme** indicate **hemoglobinuria** or **myoglobinuria**, pointing towards hemolysis or rhabdomyolysis, respectively.
- While TLS can lead to acute kidney injury, these specific urinalysis findings are not typical for TLS. The expected urinary finding would be **urate crystals**, not heme pigments.
*Hyperkalemia, hyperphosphatemia, hypocalcemia, and extremely elevated creatine kinase (MM)*
- **Hyperkalemia, hyperphosphatemia, and hypocalcemia** are consistent with TLS. However, **extremely elevated creatine kinase (MM)** is a hallmark of **rhabdomyolysis**, a condition involving breakdown of skeletal muscle.
- This option is also missing **hyperuricemia**, which is a cardinal feature of TLS.
- There is no clinical indication for rhabdomyolysis in this patient's presentation.
*Hyperuricemia, hyperkalemia, hyperphosphatemia, lactic acidosis, and oxalate crystals*
- While **hyperuricemia, hyperkalemia, and hyperphosphatemia** are characteristic of TLS, this option is missing **hypocalcemia**, one of the four cardinal metabolic abnormalities.
- Additionally, the presence of **oxalate crystals** in the urine is typically associated with **ethylene glycol poisoning** or primary hyperoxaluria, not tumor lysis syndrome. **Urate crystals**, not oxalate crystals, are expected due to the rapid breakdown of purines in TLS.
- **Lactic acidosis** can occur in severe TLS but is not a defining laboratory criterion.
More Alternative nitrogen excretion pathways US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.