NF-κB signaling US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for NF-κB signaling. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
NF-κB signaling US Medical PG Question 1: A researcher is studying the interactions between foreign antigens and human immune cells. She has isolated a line of lymphocytes that is known to bind antigen-presenting cells. From this cell line, she has isolated a cell surface protein that binds to class I major histocompatibility complex molecules. The continued activation, proliferation and survival of this specific cell line requires which of the following signaling molecules?
- A. Interleukin 1
- B. Interleukin 4
- C. Interleukin 2 (Correct Answer)
- D. Interleukin 8
- E. Interleukin 6
NF-κB signaling Explanation: ***Interleukin 2***
- The description of the lymphocyte binding the **constant portion of MHC class I** and requiring a signaling molecule for activation, proliferation, and survival points to a **T cell**.
- **Interleukin-2 (IL-2)** is a crucial cytokine for the proliferation, differentiation, and survival of T lymphocytes, acting in an autocrine or paracrine fashion after T cell activation.
*Interleukin 1*
- **Interleukin-1 (IL-1)** is primarily involved in inflammation and fever, produced by macrophages and other innate immune cells.
- While it can act as a costimulator for T cells, it is not the primary cytokine required for their sustained proliferation and survival after initial activation.
*Interleukin 4*
- **Interleukin-4 (IL-4)** is a key cytokine in humoral immunity, promoting B cell proliferation and differentiation, and inducing IgE class switching.
- It also plays a role in the differentiation of naive T cells into **Th2 cells**, but it is not the main cytokine for general T cell proliferation and survival.
*Interleukin 8*
- **Interleukin-8 (IL-8)**, also known as CXCL8, is a chemokine primarily responsible for attracting and activating neutrophils to sites of infection or inflammation.
- It does not have a direct role in the sustained proliferation and survival of activated lymphocytes.
*Interleukin 6*
- **Interleukin-6 (IL-6)** is a pleiotropic cytokine involved in acute phase reactions, hematopoiesis, and the immune response, particularly B cell differentiation and antibody production.
- Although it can influence T cell responses, it is not the primary growth factor for activated T lymphocytes as IL-2 is.
NF-κB signaling US Medical PG Question 2: A 22-year-old man comes to the physician for a follow-up evaluation for chronic lower back pain. He has back stiffness that lasts all morning and slowly improves throughout the day. He has tried multiple over-the-counter medications, including ibuprofen, without any improvement in his symptoms. Physical examination shows tenderness over the iliac crest bilaterally and limited range of motion of the lumbar spine with forward flexion. The results of HLA-B27 testing are positive. An x-ray of the lumbar spine shows fusion of the lumbar vertebrae and sacroiliac joints. The physician plans to prescribe a new medication but first orders a tuberculin skin test to assess for the risk of latent tuberculosis reactivation. Inhibition of which of the following is the most likely primary mechanism of action of this drug?
- A. mTOR kinase
- B. Calcineurin
- C. NF-κB
- D. Inosine monophosphate dehydrogenase
- E. TNF-α (Correct Answer)
NF-κB signaling Explanation: **TNF-α**
- The clinical presentation with **chronic lower back pain**, morning stiffness, **limited lumbar spine range of motion**, positive **HLA-B27**, and **fusion of lumbar vertebrae and sacroiliac joints** is highly suggestive of **ankylosing spondylitis**.
- Biologic medications, specifically **TNF-α inhibitors**, are a cornerstone of treatment for ankylosing spondylitis, especially when conventional therapies like NSAIDs fail. The mention of screening for latent tuberculosis reactivation strongly points to the use of a TNF-α inhibitor, as these drugs increase the risk of TB reactivation.
*mTOR kinase*
- **mTOR inhibitors** (e.g., sirolimus, everolimus) are primarily used as **immunosuppressants** in organ transplantation and in some cancers.
- They are not a first-line or common treatment for ankylosing spondylitis or other spondyloarthropathies.
*Calcineurin*
- **Calcineurin inhibitors** (e.g., cyclosporine, tacrolimus) are potent **immunosuppressants** used in transplant rejection prevention and some autoimmune diseases.
- While they can have immunosuppressive effects, they are not the primary target for the treatment of ankylosing spondylitis.
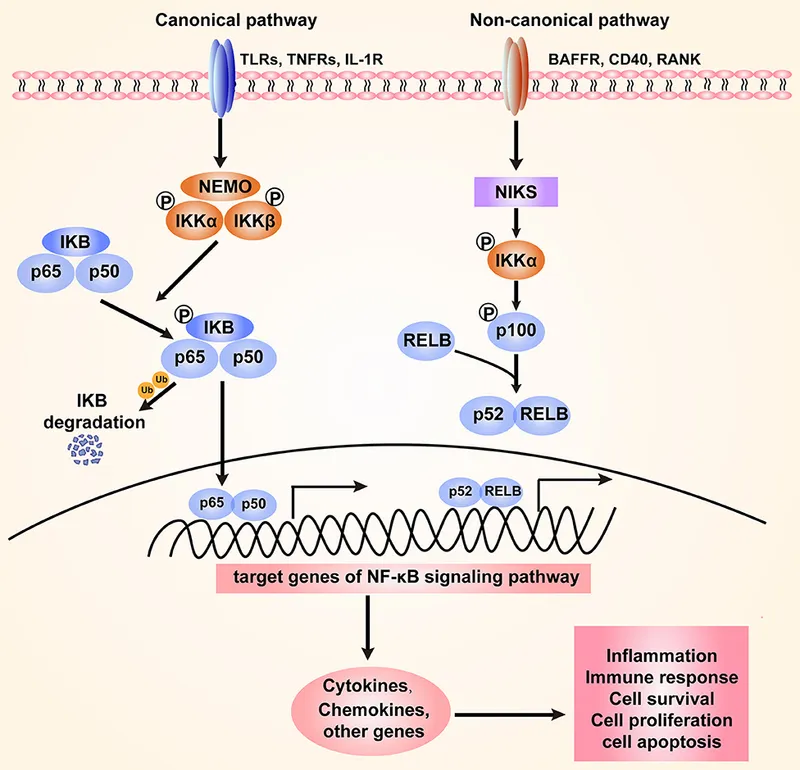
*NF-κB*
- **NF-κB** is a crucial transcription factor involved in inflammation and immune responses. While relevant to inflammatory conditions, directly targeting NF-κB is not the primary mechanism of action for the most effective biologic therapies used in ankylosing spondylitis.
- **Glucocorticoids** can inhibit NF-κB, but they are not the main long-term treatment for ankylosing spondylitis, and the context points to a biologic.
*Inosine monophosphate dehydrogenase*
- **Inosine monophosphate dehydrogenase (IMPDH) inhibitors** (e.g., mycophenolate mofetil) block purine synthesis, thus inhibiting lymphocyte proliferation.
- These drugs are used in **transplantation** and some **autoimmune diseases** (e.g., lupus, vasculitis) but are not typically used for ankylosing spondylitis.
NF-κB signaling US Medical PG Question 3: A researcher is studying the circulating factors that are released when immune cells are exposed to antigens. Specifically, she is studying a population of CD2+ cells that have been activated acutely. In order to determine which factors are secreted by these cells, she cultures the cells in media and collects the used media from these plates after several days. She then purifies a small factor from this media and uses it to stimulate various immune cell types. She finds that this factor primarily seems to increase the growth and prolong the survival of other CD2+ cells. Which of the following is most likely the factor that was purified by this researcher?
- A. Interleukin-2 (Correct Answer)
- B. Interleukin-3
- C. Interleukin-4
- D. Interleukin-5
- E. Interleukin-1
NF-κB signaling Explanation: ***Interleukin-2***
- **Interleukin-2 (IL-2)** is a crucial cytokine for the **growth**, **proliferation**, and **survival** of T lymphocytes, which are CD2+ cells.
- Activated T cells, like the acute CD2+ cells in the scenario, are a primary source of IL-2, and IL-2 acts in an **autocrine** and **paracrine** fashion to stimulate other T cells.
*Interleukin-3*
- **Interleukin-3 (IL-3)** primarily stimulates the growth and differentiation of **hematopoietic stem cells** and progenitors, not specifically mature CD2+ cells.
- It plays a role in the development of various myeloid cell lineages and mast cells, and its main effect is not confined to T cells.
*Interleukin-4*
- **Interleukin-4 (IL-4)** is critical for the differentiation of naive T helper cells into **Th2 cells** and is a key cytokine for **B cell proliferation** and **antibody class switching** to IgE.
- While it has immunomodulatory effects on T cells, its primary role is not in promoting the generalized growth and survival of other CD2+ cells.
*Interleukin-5*
- **Interleukin-5 (IL-5)** is predominantly involved in the growth, differentiation, and activation of **eosinophils**.
- It also plays a role in B cell growth and IgA production, but its effects are not primarily on universal CD2+ cell growth and survival.
*Interleukin-1*
- **Interleukin-1 (IL-1)** is a **pro-inflammatory cytokine** produced by macrophages, monocytes, and other immune cells in response to infection or injury.
- It primarily mediates **acute phase responses**, fever, and activates endothelial cells, but its main function is not to promote the growth and survival of T lymphocytes.
NF-κB signaling US Medical PG Question 4: An 85-year-old woman presents to her physician with complaints of significant weakness and weight loss. She recently has been diagnosed with stage IV breast cancer for which she currently is receiving treatment. She mentions that, despite taking a diet rich in protein and calories, she continues to lose weight. On physical examination, her vital signs are stable, but muscle wasting is clearly evident in her upper limbs, lower limbs, and face. The physician explains to her that her advanced cancer is the most important cause for the weight loss and muscle wasting. This cachexia is mediated by the proteolysis-inducing factor released from cancer cells. Which of the following effects is produced by this factor?
- A. Activation of hormone-sensitive lipase in adipose tissue
- B. Suppression of the appetite center in the hypothalamus
- C. Stimulation of apoptosis
- D. Increased release of tumor necrosis factor (TNF) from macrophages
- E. Activation of NF-κB (Correct Answer)
NF-κB signaling Explanation: ***Activation of NF-κB***
- Proteolysis-inducing factor (PIF) released from cancer cells leads to the **activation of NF-κB** in muscle cells.
- This activation results in an increased expression of **ubiquitin-proteasome pathway** components, which promotes protein degradation and muscle wasting in **cancer cachexia**.
*Activation of hormone-sensitive lipase in adipose tissue*
- While **cachexia** involves fat loss, PIF's primary effect on muscle wasting is through protein degradation, not direct activation of hormone-sensitive lipase.
- **Hormone-sensitive lipase** is mainly activated by catecholamines and cortisol during stress.
*Suppression of the appetite center in the hypothalamus*
- **Anorexia** (loss of appetite) is a component of cachexia, but PIF directly mediates muscle breakdown rather than directly suppressing hypothalamic appetite centers.
- Various cytokines like IL-1, IL-6, and TNF-α, as well as neurotransmitters, influence appetite.
*Stimulation of apoptosis*
- While **apoptosis** can contribute to cell loss in various contexts, PIF's main mechanism for muscle wasting is through the **ubiquitin-proteasome system**, not primarily by inducing apoptosis.
- Muscle atrophy in cachexia is often characterized more by protein breakdown than widespread myocyte death via apoptosis.
*Increased release of tumor necrosis factor (TNF) from macrophages*
- **TNF-α** is a major cytokine implicated in cachexia, but PIF itself is an independent factor released by tumor cells.
- PIF can act synergistically with cytokines like TNF-α to exacerbate muscle wasting, but it does not primarily cause the release of TNF-α from macrophages.
NF-κB signaling US Medical PG Question 5: A 31-year-old woman scrapes her finger on an exposed nail and sustains a minor laceration. Five minutes later, her finger is red, swollen, and painful. She has no past medical history and does not take any medications. She drinks socially with her friends and does not smoke. The inflammatory cell type most likely to be prominent in this patient's finger has which of the following characteristics?
- A. Segmented nuclei (Correct Answer)
- B. Dramatically expanded endoplasmic reticulum
- C. Large cell with amoeboid movement
- D. Multiple peripheral processes
- E. Dark histamine containing granules
NF-κB signaling Explanation: ***Segmented nuclei***
- This scenario describes **acute inflammation** following a minor injury, with classic signs of **redness, swelling, and pain** within minutes.
- **Neutrophils** are the primary inflammatory cells in acute inflammation and are characterized by their **segmented (multi-lobed) nuclei.**
*Dramatically expanded endoplasmic reticulum*
- An expanded endoplasmic reticulum is characteristic of cells highly active in protein synthesis and secretion, such as **plasma cells** producing antibodies.
- Plasma cells are typically involved in **chronic inflammation** and adaptive immune responses, not rapid acute inflammation.
*Large cell with amoeboid movement*
- This describes **macrophages**, which are phagocytic cells important in both acute and chronic inflammation, and in cleaning up debris.
- While macrophages are present, **neutrophils** are the predominant early responders in acute bacterial infections and tissue injury.
*Multiple peripheral processes*
- This description is characteristic of **dendritic cells**, which are antigen-presenting cells that initiate adaptive immune responses.
- Dendritic cells play a role in linking innate and adaptive immunity but are not the primary inflammatory cell type in the immediate acute response.
*Dark histamine containing granules*
- This description applies to **mast cells** and **basophils**, which release histamine and other mediators in allergic reactions and acute inflammation.
- While mast cells are involved in the immediate response by releasing mediators, **neutrophils** are the main cellular players migrating to the site of injury.
NF-κB signaling US Medical PG Question 6: A biology student is studying apoptosis pathways. One of the experiments conducted involves the binding of a ligand to a CD95 receptor. A defect of this pathway will most likely cause which of the conditions listed below?
- A. Chronic granulomatous disease
- B. Chédiak-Higashi syndrome
- C. Follicular lymphoma
- D. Autoimmune lymphoproliferative syndrome (Correct Answer)
- E. Leukocyte adhesion deficiency
NF-κB signaling Explanation: ***Autoimmune lymphoproliferative syndrome***
- A defect in the **CD95 (Fas) receptor pathway** impairs the normal **apoptotic deletion of self-reactive lymphocytes**, leading to their accumulation.
- This accumulation results in **lymphadenopathy, splenomegaly, and autoimmune manifestations** due to uncontrolled lymphocyte proliferation.
*Chronic granulomatous disease*
- This condition is characterized by a defect in **NADPH oxidase**, leading to recurrent infections and granuloma formation due to the inability of phagocytes to produce **reactive oxygen species**.
- It does not primarily involve the CD95 apoptosis pathway.
*Chédiak-Higashi syndrome*
- This is an **autosomal recessive disorder** involving a defect in lysosomal trafficking, leading to impaired function of phagocytes, melanocytes, and platelets.
- Symptoms include **recurrent pyogenic infections, partial albinism, and neurological abnormalities**, not directly linked to the CD95 pathway.
*Follicular lymphoma*
- This is a type of non-Hodgkin lymphoma characterized by a **t(14;18) translocation**, which causes overexpression of the **BCL2 gene**, an anti-apoptotic protein.
- While it involves impaired apoptosis, the primary defect is not in the CD95 receptor itself but rather in the regulation of apoptosis through BCL2.
*Leukocyte adhesion deficiency*
- This is a rare **immunodeficiency disorder** characterized by defects in **leukocyte adhesion molecules (integrins)**, impairing the ability of white blood cells to adhere to endothelial surfaces and migrate to sites of infection.
- It results in **recurrent bacterial infections and impaired wound healing**, unrelated to the CD95 apoptosis pathway.
NF-κB signaling US Medical PG Question 7: A 12-year-old boy admitted to the intensive care unit 1 day ago for severe pneumonia suddenly develops hypotension. He was started on empiric antibiotics and his blood culture reports are pending. According to the nurse, the patient was doing fine until his blood pressure suddenly dropped. Vital signs include: blood pressure is 88/58 mm Hg, temperature is 39.4°C (103.0°F), pulse is 120/min, and respiratory rate is 24/min. His limbs feel warm. The resident physician decides to start him on intravenous vasopressors, as the blood pressure is not responding to intravenous fluids. The on-call intensivist suspects shock due to a bacterial toxin. What is the primary mechanism responsible for the pathogenesis of this patient's condition?
- A. Inactivation of elongation factor (EF) 2
- B. Inhibition of GABA and glycine
- C. Inhibition of acetylcholine release
- D. Release of tumor necrosis factor (TNF) (Correct Answer)
- E. Degradation of lecithin in cell membranes
NF-κB signaling Explanation: ***Release of tumor necrosis factor (TNF)***
- The patient's presentation with **warm limbs** and **hypotension** despite fluid resuscitation in the setting of severe pneumonia is highly suggestive of **septic shock**.
- **Bacterial toxins**, particularly **endotoxins** from gram-negative bacteria or **exotoxins** like superantigens, trigger a massive **inflammatory response** by stimulating immune cells to release pro-inflammatory cytokines such as **TNF-α**, IL-1, and IL-6, leading to systemic vasodilation and capillary leak.
*Inactivation of elongation factor (EF) 2*
- This is the mechanism of action of **diphtheria toxin** and **exotoxin A** from *Pseudomonas aeruginosa*.
- While these toxins can cause severe systemic illness, their primary role is not typically the induction of septic shock characterized by widespread vasodilation and warm extremities.
*Inhibition of GABA and glycine*
- This mechanism is characteristic of **tetanus toxin**, which prevents the release of inhibitory neurotransmitters and leads to spastic paralysis.
- This is not consistent with the patient's presentation of septic shock.
*Inhibition of acetylcholine release*
- This is the mechanism of action of **botulinum toxin**, which causes flaccid paralysis by blocking acetylcholine release at the neuromuscular junction.
- This effect is not associated with the pathogenesis of septic shock.
*Degradation of lecithin in cell membranes*
- This mechanism is associated with **alpha toxin** of *Clostridium perfringens* (lecithinase), which causes gas gangrene and hemolysis.
- While this toxin contributes to tissue damage in certain infections, it is not the primary mechanism behind the systemic inflammatory response and vasodilation seen in septic shock.
NF-κB signaling US Medical PG Question 8: A 24-year-old woman comes to the physician because of progressively worsening episodes of severe, crampy abdominal pain and nonbloody diarrhea for the past 3 years. Examination of the abdomen shows mild distension and generalized tenderness. There is a fistula draining stool in the perianal region. Immunohistochemistry shows dysfunction of the nucleotide oligomerization binding domain 2 (NOD2) protein. This dysfunction most likely causes overactivity of which of the following immunological proteins in this patient?
- A. Interferon-γ
- B. β-catenin
- C. IL-1β
- D. IL-10
- E. NF-κB (Correct Answer)
NF-κB signaling Explanation: ***NF-κB***
- **NOD2** is a pattern recognition receptor that normally detects bacterial products and regulates inflammatory responses. In **Crohn's disease**, loss-of-function **NOD2 mutations** lead to impaired bacterial sensing and clearance.
- This defective NOD2 function results in **compensatory overactivation of NF-κB** through alternative inflammatory pathways (particularly TLR signaling), causing excessive **pro-inflammatory cytokine** production.
- This **NF-κB hyperactivation** is a key driver of chronic inflammation in **Crohn's disease**, contributing to symptoms like fistulas, strictures, and transmural inflammation.
*Interferon-γ*
- **Interferon-γ** is an important pro-inflammatory cytokine in Crohn's disease and is part of the Th1-mediated immune response.
- However, its production is downstream of **NF-κB** activation and other inflammatory cascades. **NOD2 dysfunction** does not directly cause **IFN-γ** overactivity through the primary molecular pathway.
*β-catenin*
- **β-catenin** is a key component of the **Wnt signaling pathway** involved in cell adhesion, proliferation, and differentiation.
- It is not directly affected by **NOD2 dysfunction**. Dysregulation of **β-catenin** is more commonly associated with colorectal adenomas and cancer, not the inflammatory mechanisms of Crohn's disease.
*IL-1β*
- **IL-1β** is a potent pro-inflammatory cytokine that is indeed elevated in **Crohn's disease**.
- However, **IL-1β** is produced **downstream** of **NF-κB** activation. The primary molecular consequence of **NOD2 dysfunction** is the overactivity of **NF-κB**, which then drives production of various cytokines including **IL-1β**.
*IL-10*
- **IL-10** is an **anti-inflammatory cytokine** essential for maintaining intestinal immune homeostasis and suppressing excessive inflammatory responses.
- In Crohn's disease, **IL-10** signaling is often **impaired or deficient** rather than overactive. The question asks about overactivity, making this the opposite of what occurs in the disease.
NF-κB signaling US Medical PG Question 9: A 62-year-old man comes to the physician because of progressive fatigue and dyspnea on exertion for 3 months. During this time, he has also had increased straining during defecation and a 10-kg (22-lb) weight loss. He has no personal or family history of serious medical illness. Physical examination shows conjunctival pallor. Laboratory studies show microcytic anemia. Test of the stool for occult blood is positive. Colonoscopy shows an exophytic mass in the ascending colon. Pathologic examination of the mass shows a well-differentiated adenocarcinoma. A gain-of-function mutation in which of the following genes is most likely involved in the pathogenesis of this patient's condition?
- A. APC
- B. TP53
- C. MLH1
- D. KRAS (Correct Answer)
- E. DCC
NF-κB signaling Explanation: ***KRAS***
- A **gain-of-function mutation** in **KRAS** is a common early event in the development of colorectal adenocarcinoma, driving uncontrolled cell growth and proliferation.
- This mutation is frequently found in **sporadic colorectal cancers**, particularly in the advanced stages of adenoma to carcinoma progression.
*APC*
- **APC** is a **tumor suppressor gene**, and mutations in it are typically **loss-of-function**, not gain-of-function.
- While APC mutations are crucial early steps in the adenoma-carcinoma sequence, they lead to inactivation of the gene, not increased function.
*TP53*
- **TP53** is a **tumor suppressor gene** which, when mutated, usually involves **loss-of-function** or dominant-negative effects, impairing its ability to induce apoptosis or cell cycle arrest.
- Mutations in TP53 are typically associated with **later stages** of colorectal cancer progression and tend to be loss-of-function, not gain-of-function.
*MLH1*
- **MLH1** is involved in **DNA mismatch repair**, and mutations here lead to **microsatellite instability** and are characteristic of hereditary nonpolyposis colorectal cancer (Lynch syndrome).
- These are typically **loss-of-function mutations** that impair DNA repair, not gain-of-function mutations promoting oncogenesis directly through signaling pathways.
*DCC*
- **DCC** (**Deleted in Colorectal Carcinoma**) is a **tumor suppressor gene**, and its inactivation or loss is associated with colorectal cancer progression, particularly the transition from adenoma to carcinoma.
- Mutations or deletions in DCC result in a **loss-of-function**, not a gain-of-function, contributing to tumor growth by failing to regulate cell differentiation and apoptosis.
NF-κB signaling US Medical PG Question 10: A research team discovers a novel bacterial toxin that causes severe hypotension in infected patients. In vitro studies show the toxin ADP-ribosylates a specific amino acid on Gq alpha subunits, preventing their activation by GPCRs. Patients develop hypotension despite elevated levels of vasopressin, angiotensin II, and endothelin-1. Synthesize the pathophysiological mechanism explaining why multiple vasopressor hormones fail to maintain blood pressure in these patients.
- A. The toxin depletes intracellular ATP preventing myosin-actin interaction
- B. The toxin prevents receptor binding of vasopressor hormones through allosteric inhibition
- C. ADP-ribosylation of Gq prevents PLC activation, blocking IP3-mediated calcium release and vascular smooth muscle contraction (Correct Answer)
- D. ADP-ribosylation increases cAMP levels causing smooth muscle relaxation
- E. The toxin activates Gi proteins causing excessive vasodilation that overwhelms vasoconstrictor signals
NF-κB signaling Explanation: ***ADP-ribosylation of Gq prevents PLC activation, blocking IP3-mediated calcium release and vascular smooth muscle contraction***
- Vasopressor hormones like **Vasopressin**, **Angiotensin II**, and **Endothelin-1** signal through **Gq-coupled receptors** to trigger **vascular smooth muscle contraction**.
- By ADP-ribosylating the **Gq alpha subunit**, the toxin inhibits **Phospholipase C (PLC)**, preventing the generation of **IP3 and DAG**, which are essential for releasing **intracellular calcium**.
*The toxin prevents receptor binding of vasopressor hormones through allosteric inhibition*
- The toxin targets the **G-protein (intracellular)** rather than the **extracellular binding site** of the G-protein coupled receptors (GPCRs).
- Since binding still occurs but **signal transduction** is blocked, this describes a post-receptor defect rather than **allosteric inhibition** of the receptor itself.
*The toxin activates Gi proteins causing excessive vasodilation that overwhelms vasoconstrictor signals*
- The prompt explicitly states the toxin modifies the **Gq alpha subunit**, not the **Gi subunit**.
- **Gi protein** activation primarily lowers **cAMP**, whereas the failure of pressors in this case is linked to the lack of **calcium mobilization** via Gq.
*ADP-ribosylation increases cAMP levels causing smooth muscle relaxation*
- Increased **cAMP** (via Gs activation or Gi inhibition) does cause relaxation, but this mechanism is associated with toxins like **Cholera** or **Pertussis**.
- The modification of **Gq** specifically disrupts the **phosphoinositol pathway**, not the **adenylyl cyclase** pathway that regulates cAMP.
*The toxin depletes intracellular ATP preventing myosin-actin interaction*
- ADP-ribosylation is a specific **post-translational modification** using **NAD+** as a substrate, which does not result in systemic **ATP depletion**.
- The failure of contraction is due to a lack of **calcium-calmodulin** activation of **Myosin Light Chain Kinase (MLCK)**, not a lack of energy supply for the motor proteins.
More NF-κB signaling US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.