JAK-STAT pathway US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for JAK-STAT pathway. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
JAK-STAT pathway US Medical PG Question 1: A 2-year-old girl presents to the pediatrician with an itchy rash. Her mother reports that she has had a crusty rash on the face and bilateral upper extremities intermittently for the past 2 months. The child's past medical history is notable for 3 similar episodes of severely itchy rashes since birth. She has also had 2 non-inflamed abscesses on her arms over the past year. Her temperature is 98.9°F (37.2°C), blood pressure is 108/68 mmHg, pulse is 94/min, and respirations are 18/min. On exam, she appears uncomfortable and is constantly itching her face and arms. There is an eczematous rash on the face and bilateral upper extremities. Her face has thickened skin with a wide-set nose. This patient's condition is most likely caused by a mutation in which of the following genes?
- A. STAT3 (Correct Answer)
- B. IL-12 receptor
- C. WAS
- D. LYST
- E. Adenosine deaminase
JAK-STAT pathway Explanation: ***STAT3***
- The patient's presentation with recurrent **abscesses**, widespread eczematous rash, and characteristic facial features (thickened skin, wide-set nose) is highly suggestive of **Job syndrome**, also known as hyper-IgE syndrome.
- Job syndrome is an autosomal dominant primary immunodeficiency caused by mutations in the **STAT3 gene**, leading to impaired Th17 cell function and recurrent infections, particularly with *Staphylococcus aureus*.
*IL-12 receptor*
- Mutations in the **IL-12 receptor** lead to a predisposition to infections with intracellular bacteria and mycobacteria (e.g., disseminated atypical mycobacterial infections, salmonella) due to impaired Th1 immune response.
- This condition is not typically associated with recurrent abscesses, eczematous rashes, or the specific facial features seen in this patient.
*WAS*
- Mutations in the **WAS gene** cause Wiskott-Aldrich syndrome, characterized by the triad of **thrombocytopenia** (leading to bleeding diathesis), **eczema**, and recurrent infections.
- While eczema is present in the patient, the absence of thrombocytopenia and the presence of recurrent abscesses and specific facial features make Wiskott-Aldrich syndrome less likely.
*LYST*
- Mutations in the **LYST gene** cause Chédiak-Higashi syndrome, an autosomal recessive disorder characterized by partial **oculocutaneous albinism**, recurrent pyogenic infections, and neurological abnormalities.
- The patient's presentation does not include albinism or significant neurological findings, nor the giant lysosomes characteristic of this syndrome.
*Adenosine deaminase*
- Deficiency of **adenosine deaminase (ADA)** leads to severe combined immunodeficiency (SCID), a profound impairment of both T and B cell immunity.
- Patients typically present with severe, life-threatening infections, chronic diarrhea, and failure to thrive early in life, a much more severe and generalized immunodeficiency than described in this patient.
JAK-STAT pathway US Medical PG Question 2: A research team develops a new monoclonal antibody checkpoint inhibitor for advanced melanoma that has shown promise in animal studies as well as high efficacy and low toxicity in early phase human clinical trials. The research team would now like to compare this drug to existing standard of care immunotherapy for advanced melanoma. The research team decides to conduct a non-randomized study where the novel drug will be offered to patients who are deemed to be at risk for toxicity with the current standard of care immunotherapy, while patients without such risk factors will receive the standard treatment. Which of the following best describes the level of evidence that this study can offer?
- A. Level 1
- B. Level 3 (Correct Answer)
- C. Level 5
- D. Level 4
- E. Level 2
JAK-STAT pathway Explanation: ***Level 3***
- A **non-randomized controlled trial** like the one described, where patient assignment to treatment groups is based on specific characteristics (risk of toxicity), falls into Level 3 evidence.
- This level typically includes **non-randomized controlled trials** and **well-designed cohort studies** with comparison groups, which are prone to selection bias and confounding.
- The study compares two treatments but lacks randomization, making it Level 3 evidence.
*Level 1*
- Level 1 evidence is the **highest level of evidence**, derived from **systematic reviews and meta-analyses** of multiple well-designed randomized controlled trials or large, high-quality randomized controlled trials.
- The described study is explicitly stated as non-randomized, ruling out Level 1.
*Level 2*
- Level 2 evidence involves at least one **well-designed randomized controlled trial** (RCT) or **systematic reviews** of randomized trials.
- The current study is *non-randomized*, which means it cannot be classified as Level 2 evidence, as randomization is a key criterion for this level.
*Level 4*
- Level 4 evidence includes **case series**, **case-control studies**, and **poorly designed cohort or case-control studies**.
- While the study is non-randomized, it is a controlled comparative trial rather than a case series or retrospective case-control study, placing it at Level 3.
*Level 5*
- Level 5 evidence is the **lowest level of evidence**, typically consisting of **expert opinion** without explicit critical appraisal, or based on physiology, bench research, or animal studies.
- While the drug was initially tested in animal studies, the current human comparative study offers a higher level of evidence than expert opinion or preclinical data.
JAK-STAT pathway US Medical PG Question 3: A 70-year-old man presents to his physician for evaluation of fullness and swelling of the left side of the abdomen over the last month. During this time, he has had night sweats and lost 2 kg (4.4 lb) unintentionally. He has no history of severe illness and takes no medications. The vital signs include: blood pressure 115/75 mm Hg, pulse 75/min, and temperature 36.8℃ (98.2℉). The abdomen has asymmetric distention. Percussion and palpation of the left upper quadrant reveal splenomegaly. No lymphadenopathy is detected. Heart and lung examination shows no abnormalities. The laboratory studies show the following:
Hemoglobin 9.5 g/dL
Mean corpuscular volume 95 μm3
Leukocyte count 8,000/mm3
Platelet count 240,000/mm3
Ultrasound shows a spleen size of 15 cm, mild hepatomegaly, and mild ascites. The peripheral blood smear shows teardrop-shaped and nucleated red blood cells (RBCs) and immature myeloid cells. Marrow is very difficult to aspirate but reveals hyperplasia of all 3 lineages. The tartrate-resistant acid phosphatase (TRAP) test is negative. The cytogenetic analysis is negative for translocation between chromosomes 9 and 22. Which of the following laboratory findings is most likely to be present in this patient?
- A. Monoclonal elevation of IgG
- B. Hair-like cell-membrane projections
- C. JAK2 mutation (Correct Answer)
- D. Philadelphia chromosome
- E. Reed-Sternberg cells
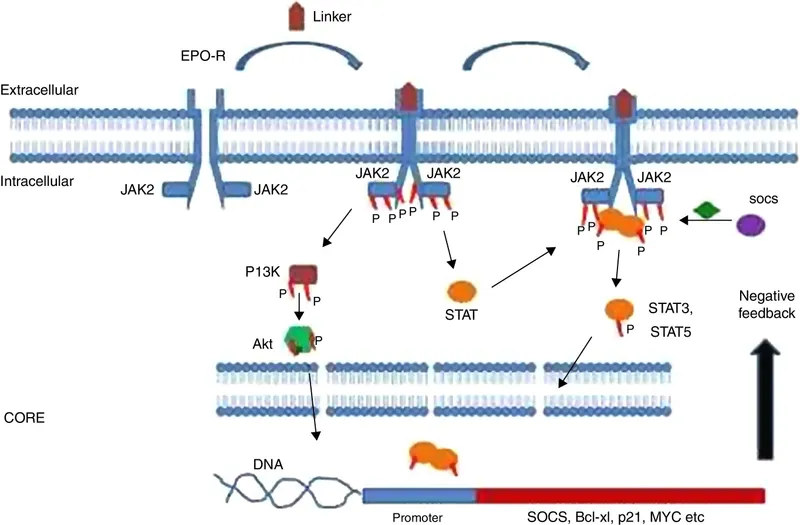
JAK-STAT pathway Explanation: ***JAK2 mutation***
- The patient's presentation with **splenomegaly**, **night sweats**, **weight loss**, **teardrop cells**, **nucleated red blood cells**, and a "dry tap" (difficulty aspirating marrow) are highly suggestive of **primary myelofibrosis**.
- A **JAK2 mutation** (specifically JAK2 V617F) is found in approximately 50-60% of patients with primary myelofibrosis and is a crucial diagnostic marker, distinguishing it from other myeloproliferative neoplasms. Other driver mutations include CALR (~25-30%) and MPL (~5-10%).
*Monoclonal elevation of IgG*
- **Monoclonal elevation of IgG** is characteristic of **plasma cell disorders** such as **multiple myeloma** or **monoclonal gammopathy of undetermined significance (MGUS)**.
- This patient's symptoms and laboratory findings, particularly the peripheral blood smear with **teardrop cells** and a "dry tap," do not align with a plasma cell dyscrasia.
*Hair-like cell-membrane projections*
- **Hair-like cell-membrane projections** are the hallmark of **hairy cell leukemia**, a rare B-cell lymphoproliferative disorder.
- While hairy cell leukemia can cause **splenomegaly** and **pancytopenia**, the presence of **teardrop cells** and **immature myeloid cells** in the peripheral smear, along with a "dry tap," makes this diagnosis unlikely. The **negative TRAP test** also argues against hairy cell leukemia since TRAP positivity is characteristic of this condition.
*Philadelphia chromosome*
- The **Philadelphia chromosome (t(9;22))** encoding the **BCR-ABL1 fusion gene** is the defining characteristic of **chronic myeloid leukemia (CML)**.
- While CML can present with **splenomegaly** and **myeloid immature cells**, the absence of the Philadelphia chromosome on cytogenetic analysis (as stated in the stem) and the presence of **teardrop cells** and **dry tap** rule out CML in favor of myelofibrosis.
*Reed-Sternberg cells*
- **Reed-Sternberg cells** are large, multinucleated cells characteristic of **Hodgkin lymphoma**.
- Hodgkin lymphoma typically presents with **lymphadenopathy** and systemic symptoms, but the hematological findings and evidence of myelofibrosis in this patient do not support a diagnosis of lymphoma.
JAK-STAT pathway US Medical PG Question 4: A 10-year-old boy from Sri Lanka suffers from an autosomal dominant condition, the hallmark of which is hyperimmunoglobulinemia E and eosinophilia. He suffers from recurrent infections and takes antibiotic chemoprophylaxis. A STAT3 mutation analysis has been performed to confirm the diagnosis of Job syndrome.
I. Eosinophilia
II. Eczema
III. Hay fever
IV. Atopic dermatitis
V. Recurrent skin and lung infections
VI. Bronchial asthma
What combination of symptoms above is characteristic of this condition?
- A. I, II, III
- B. I, II, IV, V
- C. I, III, IV
- D. I, II, V (Correct Answer)
- E. IV, V, VI
JAK-STAT pathway Explanation: ***I, II, V***
- **Job syndrome** (Hyper-IgE syndrome) is characterized by a triad of **recurrent infections** (recurrent skin and lung infections), **severe eczema**, and **eosinophilia**.
- The patient's presentation with hyperimmunoglobulinemia E, eosinophilia, and recurrent infections, coupled with a confirmed **STAT3 mutation**, directly aligns with the key features of this syndrome.
*I, II, III*
- While **eosinophilia** and **eczema** are characteristic of Job syndrome, **hay fever** (allergic rhinitis) is not a primary diagnostic criterion, although allergic manifestations can occur.
- The core clinical presentation focuses on immune dysregulation leading to infections and severe skin involvement, which are more specific than hay fever.
*I, II, IV, V*
- This option includes **atopic dermatitis** which is essentially synonymous with **eczema**, leading to redundancy.
- The combination should focus on distinct major clinical features rather than overlapping terms.
*I, III, IV*
- This option includes **hay fever** and **atopic dermatitis**, neither of which are as central to the diagnostic criteria as recurrent infections.
- The most critical elements for diagnosis are the immune dysfunction leading to severe infections and the hallmark skin condition.
*IV, V, VI*
- This option lists **atopic dermatitis**, **recurrent skin and lung infections**, and **bronchial asthma**. While these can be seen in Job syndrome, it omits **eosinophilia**, which is a defining laboratory finding.
- **Bronchial asthma** is also not a primary diagnostic feature, and the absence of eosinophilia makes this option less accurate.
JAK-STAT pathway US Medical PG Question 5: A 55-year-old man comes to the physician with a 3-month history of headache, periodic loss of vision, and easy bruising. Physical examination shows splenomegaly. His hemoglobin concentration is 13.8 g/dL, leukocyte count is 8000/mm3, and platelet count is 995,000/mm3. Bone marrow biopsy shows markedly increased megakaryocytes with hyperlobulated nuclei. Genetic analysis shows upregulation of the JAK-STAT genes. The pathway encoded by these genes is also physiologically responsible for signal transmission of which of the following hormones?
- A. Oxytocin
- B. Adrenocorticotropic hormone
- C. Prolactin (Correct Answer)
- D. Cortisol
- E. Insulin
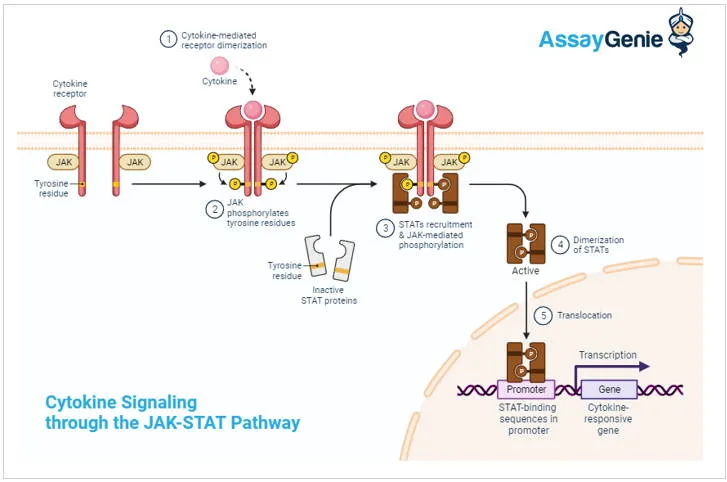
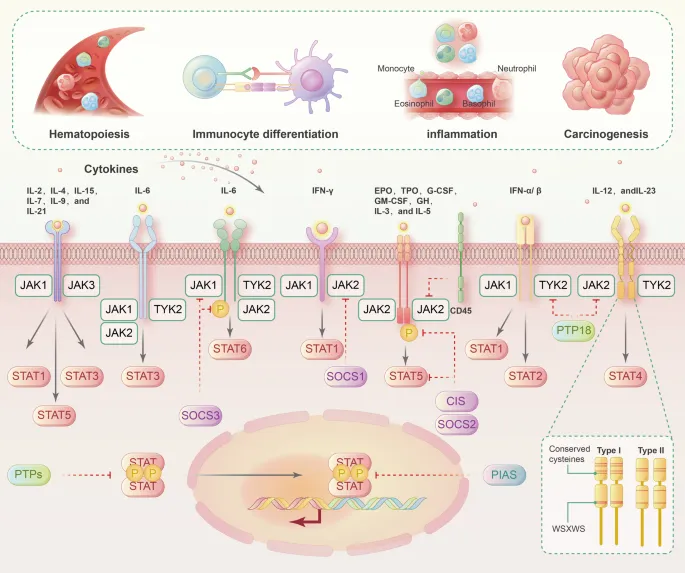
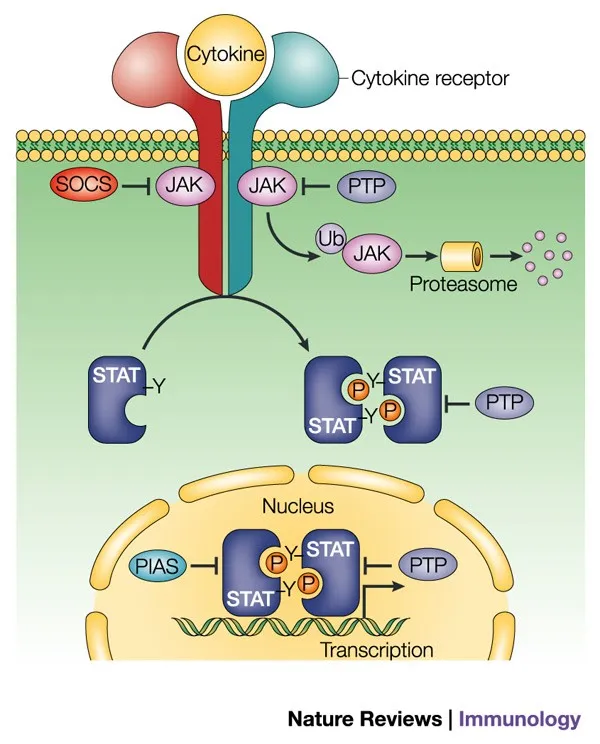
JAK-STAT pathway Explanation: ***Prolactin***
- Prolactin utilizes the **JAK-STAT signaling pathway** to exert its effects on target cells, particularly in the mammary glands.
- The **JAK-STAT pathway** is crucial for cell growth, differentiation, and immune response, and its dysregulation is linked to myeloproliferative disorders like those involving megakaryocyte proliferation.
*Oxytocin*
- Oxytocin primarily acts through **G-protein coupled receptors** that activate the phospholipase C/inositol triphosphate pathway, not the JAK-STAT pathway.
- Its main roles involve uterine contraction and milk ejection, which are distinct from the cellular proliferation regulated by JAK-STAT.
*Adrenocorticotropic hormone*
- ACTH binds to **G-protein coupled receptors** in the adrenal cortex, stimulating adenylyl cyclase and increasing cAMP levels.
- This mechanism of action is distinct from the tyrosine kinase activity characteristic of the JAK-STAT pathway.
*Cortisol*
- Cortisol, a steroid hormone, primarily acts via **intracellular glucocorticoid receptors** that translocate to the nucleus to regulate gene transcription.
- Its signaling mechanism involves direct gene regulation rather than a membrane-bound receptor-kinase cascade like JAK-STAT.
*Insulin*
- Insulin signals through a **receptor tyrosine kinase**, which, upon binding, autophosphorylates and initiates a cascade involving IRS proteins and the PI3K/Akt and MAPK pathways.
- While it involves tyrosine phosphorylation, it is distinct from the JAK-STAT pathway, which is primarily activated by cytokine and growth hormone type I receptors.
JAK-STAT pathway US Medical PG Question 6: A 62-year-old man, a retired oil pipeline engineer, presents to his primary care physician with complaints of headaches, fatigue, and constant ringing in his ears. Recurrently he has developed pruritus, usually after a hot shower. He also noted a constant burning sensation in his fingers and toes, independent of physical activity. On examination, he has a red face and his blood pressure levels are 147/89 mm Hg. A CBC revealed that his Hb is 19.0 g/dL and Hct is 59%. Because of his condition, his physician prescribes him 81 mg of aspirin to be taken daily in addition to therapeutic phlebotomy. Which of the statements below is true about this patient’s condition?
- A. Warfarin and phlebotomy are the preferred course of treatment.
- B. The patient has a decreased risk of developing myelofibrosis.
- C. Serum erythropoietin is expected to be high.
- D. Arterial oxygen saturation is usually higher than normal values in this condition.
- E. Mutation of the JAK2 gene is commonly seen in this condition. (Correct Answer)
JAK-STAT pathway Explanation: ***Mutation of the JAK2 gene is commonly seen in this condition.***
* The patient's symptoms (headaches, fatigue, tinnitus, pruritus after hot showers, erythromelalgia, facial plethora, hypertension, and elevated hemoglobin/hematocrit) are highly suggestive of **polycythemia vera (PV)**.
* Over 95% of patients with PV have a **JAK2 V617F mutation**, leading to constitutive activation of the JAK-STAT pathway, resulting in uncontrolled erythrocyte production.
*Warfarin and phlebotomy are the preferred course of treatment.*
* While **phlebotomy** is a cornerstone of PV management to reduce hematocrit and prevent thrombotic events, **warfarin** is generally not indicated for primary thromboprophylaxis in PV.
* **Low-dose aspirin** is preferred for reducing thrombotic risk, as indicated by the physician's prescription, along with phlebotomy.
*The patient has a decreased risk of developing myelofibrosis.*
* Polycythemia vera is a **myeloproliferative neoplasm**, and a significant percentage of patients (10-15%) will progress to **post-polycythemia vera myelofibrosis** over time.
* This progression is a natural history of the disease rather than a decreased risk, occurring as the bone marrow becomes exhausted and fibrotic.
*Serum erythropoietin is expected to be high.*
* In polycythemia vera, the **erythroid progenitors** are hypersensitive to erythropoietin (EPO), and red blood cell production occurs independently of EPO.
* Consequently, the **serum erythropoietin level is typically low or undetectable** due to feedback inhibition from the high red blood cell mass.
*Arterial oxygen saturation is usually higher than normal values in this condition.*
* Arterial oxygen saturation is generally **normal** in polycythemia vera, differentiating it from secondary polycythemia caused by hypoxemia (where oxygen saturation would be low).
* The increased red blood cell mass in PV does not inherently lead to higher-than-normal arterial oxygen saturation; it leads to increased oxygen-carrying capacity.
JAK-STAT pathway US Medical PG Question 7: A 65-year-old man comes to the physician because of a 6-month history of progressive fatigue and abdominal pain. Physical examination shows pale mucous membranes and splenomegaly. Hemoglobin concentration is 9.1 g/dL and leukocyte count is 3,400/mm3. Peripheral blood smear shows nucleated red blood cells and teardrop poikilocytosis. A Janus kinase 2 gene mutation is present. Which of the following is the most likely underlying mechanism of this patient's condition?
- A. Elevated levels of circulating hepcidin
- B. Lymphocytic infiltration of reticuloendothelial system
- C. Viral replication in lymphoid cells
- D. Fibrosis in the bone marrow (Correct Answer)
- E. Translocation between chromosome 9 and 22
JAK-STAT pathway Explanation: ***Fibrosis in the bone marrow***
- The constellation of **fatigue**, **anemia** (Hb 9.1 g/dL), **splenomegaly**, **teardrop poikilocytosis**, and a **JAK2 mutation** is highly suggestive of **primary myelofibrosis**.
- **Bone marrow fibrosis** is the hallmark of primary myelofibrosis, leading to ineffective hematopoiesis and extramedullary hematopoiesis (causing splenomegaly).
*Elevated levels of circulating hepcidin*
- **Elevated hepcidin** is characteristic of **anemia of chronic disease** or **iron-refractory iron deficiency anemia**, where iron is trapped in macrophages despite adequate stores.
- While anemia is present, the other features (splenomegaly, teardrop cells, JAK2 mutation) are not consistent with anemia of chronic disease as the primary mechanism.
*Lymphocytic infiltration of reticuloendothelial system*
- **Lymphocytic infiltration** is typical of **lymphoproliferative disorders** like leukemias or lymphomas, which would present with different CBC findings, not primarily myelofibrosis features.
- This mechanism would lead to different peripheral smear findings (e.g., lymphocytosis) rather than nucleated red cells and teardrop cells.
*Viral replication in lymphoid cells*
- **Viral replication in lymphoid cells** can cause various hematologic abnormalities (e.g., infectious mononucleosis, some lymphomas), but it is not the underlying mechanism for the specific features of primary myelofibrosis.
- This would not explain the **JAK2 mutation** or the characteristic **bone marrow fibrosis** and **extramedullary hematopoiesis**.
*Translocation between chromosome 9 and 22*
- A **translocation between chromosome 9 and 22** (the **Philadelphia chromosome**) is characteristic of **chronic myeloid leukemia (CML)**.
- While CML can cause splenomegaly and myeloid abnormalities, it typically presents with marked leukocytosis and does not feature the prominent teardrop cells or the primary myelofibrosis features seen here; CML is characterized by the **BCR-ABL1 fusion gene**, not primarily a JAK2 mutation.
JAK-STAT pathway US Medical PG Question 8: An epidemiologist is evaluating the efficacy of Noxbinle in preventing HCC deaths at the population level. A clinical trial shows that over 5 years, the mortality rate from HCC was 25% in the control group and 15% in patients treated with Noxbinle 100 mg daily. Based on this data, how many patients need to be treated with Noxbinle 100 mg to prevent, on average, one death from HCC?
- A. 20
- B. 73
- C. 10 (Correct Answer)
- D. 50
- E. 100
JAK-STAT pathway Explanation: ***10***
- The **number needed to treat (NNT)** is calculated by first finding the **absolute risk reduction (ARR)**.
- **ARR** = Risk in control group - Risk in treatment group = 25% - 15% = **10%** (or 0.10).
- **NNT = 1 / ARR** = 1 / 0.10 = **10 patients**.
- This means that **10 patients must be treated with Noxbinle to prevent one death from HCC** over 5 years.
*20*
- This would result from an ARR of 5% (1/0.05 = 20), which is not supported by the data.
- May arise from miscalculating the risk difference or incorrectly halving the actual ARR.
*73*
- This value does not correspond to any standard calculation of NNT from the given mortality rates.
- May result from confusion with other epidemiological measures or calculation error.
*50*
- This would correspond to an ARR of 2% (1/0.02 = 50), which significantly underestimates the actual risk reduction.
- Could result from incorrectly calculating the difference as a proportion rather than absolute percentage points.
*100*
- This would correspond to an ARR of 1% (1/0.01 = 100), grossly underestimating the treatment benefit.
- May result from confusing ARR with relative risk reduction or other calculation errors.
JAK-STAT pathway US Medical PG Question 9: An 8-year-old boy presents with recurrent infections including multiple episodes of pneumonia and diarrhea. He reports difficulty seeing in the dark. Physical examination reveals white patches on the sclera and conjunctival dryness. What is the most likely cause of these findings?
- A. Congenital rubella
- B. Spinocerebellar ataxia (SCA) type 1
- C. Deficiency of vitamin A (Correct Answer)
- D. Autoimmune neutropenia
- E. Vitamin B1 deficiency
JAK-STAT pathway Explanation: ***Deficiency of vitamin A***
- The combination of **recurrent infections** (pneumonia, diarrhea), **night blindness**, and **ocular signs** like white patches on the sclera (Bitot's spots due to keratinized epithelium) and conjunctival dryness (xerophthalmia) are classic manifestations of **vitamin A deficiency**.
- Vitamin A is crucial for **immune function**, **vision** (a component of rhodopsin), and the **maintenance of epithelial tissues**.
*Congenital rubella*
- This typically presents with a **triad of cataracts**, **heart defects** (e.g., patent ductus arteriosus), and **sensorineural hearing loss**, often detected earlier in infancy.
- It does not explain the recurrent infections, night blindness, or specific ocular epithelial changes described.
*Spinocerebellar ataxia (SCA) type 1*
- This is a **neurodegenerative disorder** primarily affecting coordination and balance, leading to progressive **ataxia**.
- It does not cause recurrent infections, night blindness, or xerophthalmia; its symptoms are distinct and neurological in nature.
*Autoimmune neutropenia*
- Primarily causes **recurrent bacterial infections** due to low neutrophil counts.
- It does not explain the night blindness, diarrhea, or the specific ocular findings of keratinization.
*Vitamin B1 deficiency*
- Also known as **thiamine deficiency**, it leads to **beriberi**, characterized by cardiac (wet beriberi) or neurological (dry beriberi) symptoms.
- Common symptoms include **peripheral neuropathy**, **heart failure**, and **Wernicke-Korsakoff syndrome**, none of which are descriptive of this patient's presentation.
JAK-STAT pathway US Medical PG Question 10: An 11-month-old boy is brought to a pediatrician by his parents with a recurrent cough, which he has had since the age of 2 months. He has required 3 hospitalizations for severe wheezing episodes. His mother also mentions that he often has diarrhea. The boy’s detailed history reveals that he required hospitalization for meconium ileus during the neonatal period. Upon physical examination, his temperature is 37.0°C (98.6ºF), pulse rate is 104/min, respiratory rate is 40/min, and blood pressure is 55/33 mm Hg. An examination of the boy’s respiratory system reveals the presence of bilateral wheezing and scattered crepitations. An examination of his cardiovascular system does not reveal any abnormality. His length is 67.3 cm (26.5 in) and weight is 15 kg (33 lbs). His sweat chloride level is 74 mmol/L. His genetic evaluation confirms that he has an autosomal recessive disorder resulting in a dysfunctional membrane-bound protein. Which of the following best describes the mechanism associated with the most common mutation that causes this disorder?
- A. Decreased chloride transport through the protein
- B. Disordered regulation of the protein
- C. Decreased transcription of the protein due to splicing defect
- D. Complete absence of the protein
- E. Defective maturation and early degradation of the protein (Correct Answer)
JAK-STAT pathway Explanation: ***Defective maturation and early degradation of the protein***
- The clinical picture (recurrent cough, wheezing, diarrhea, meconium ileus, elevated sweat chloride, autosomal recessive inheritance) strongly points to **cystic fibrosis (CF)**. The most common mutation in CF is **F508del**, which leads to misfolding of the **CFTR protein**, causing retention in the endoplasmic reticulum and subsequent degradation before reaching the cell membrane.
- This **defective processing and early degradation** result in a significant reduction or absence of functional CFTR protein at the cell surface, leading to impaired chloride transport.
*Decreased chloride transport through the protein*
- While **decreased chloride transport** is the ultimate functional consequence of cystic fibrosis, it is not the direct mechanism associated with the **F508del mutation's impact** on the CFTR protein itself.
- This option describes the **physiological result** of the protein defect, not the cellular/molecular mechanism of the most common mutation.
*Disordered regulation of the protein*
- **Disordered regulation** could be a potential mechanism for some CFTR mutations (Class IV mutations), affecting how the channel opens and closes or responds to signaling.
- However, for the **F508del mutation** (Class II mutation), the primary issue is the **lack of properly localized protein** due to misfolding and degradation, rather than a problem with the regulation or gating of the protein once it reaches the membrane.
*Decreased transcription of the protein due to splicing defect*
- **Decreased transcription** or **splicing defects** (Class I and V mutations) would result in reduced mRNA levels or incorrectly formed mRNA, leading to less protein synthesis.
- The **F508del mutation** involves a deletion of three nucleotides in exon 10, leading to a missing phenylalanine at position 508. Importantly, **transcription and splicing occur normally**; the mRNA is produced correctly. The problem arises at the **post-translational level** with protein folding, not at the transcriptional or splicing level.
*Complete absence of the protein*
- While functional CFTR protein is largely absent at the cell surface in F508del, the protein is **initially synthesized** in the endoplasmic reticulum.
- The problem is its **misfolding and rapid degradation**, preventing it from reaching the membrane, rather than a complete failure of protein synthesis from the outset (which would be seen in nonsense or frameshift mutations causing Class I defects).
More JAK-STAT pathway US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.