G-protein coupled receptors US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for G-protein coupled receptors. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
G-protein coupled receptors US Medical PG Question 1: A drug research team has synthesized a novel oral drug that acts as an agonist at multiple adrenergic receptors. When administered in animals, it has been shown to produce urinary retention at therapeutic doses with the absence of other manifestations of adrenergic stimulation. The researchers are interested in understanding signal transduction and molecular mechanisms behind the action of the novel drug. Which of the following receptors would most likely transduce signals across the plasma membrane following the administration of this novel drug?
- A. GoPCRs (Go protein-coupled receptors)
- B. GsPCRs (Gs protein-coupled receptors)
- C. GqPCRs (Gq protein-coupled receptors) (Correct Answer)
- D. GtPCRs (Gt protein-coupled receptors)
- E. GiPCRs (Gi protein-coupled receptors)
G-protein coupled receptors Explanation: ***GqPCRs (Gq protein-coupled receptors)***
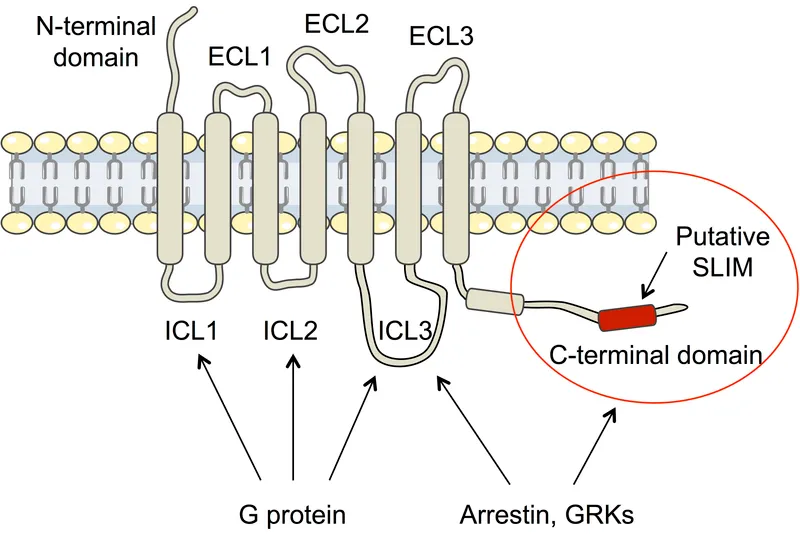
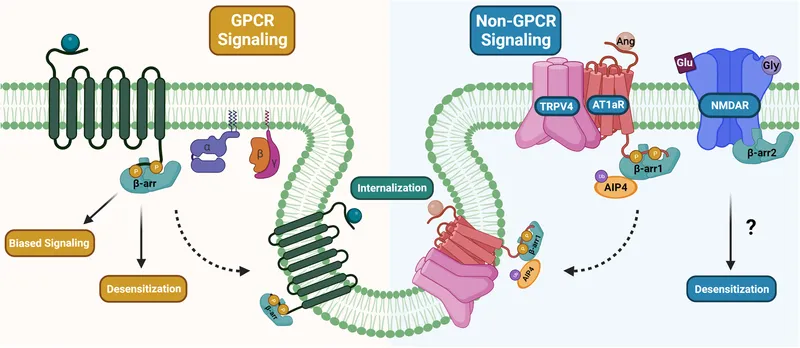
- **Urinary retention** is primarily mediated by the activation of **alpha-1 adrenergic receptors** in the bladder neck and prostate, which are classically Gq-protein coupled receptors.
- Activation of **GqPCRs** leads to the activation of **phospholipase C**, increased **IP3 (inositol trisphosphate)** and **DAG (diacylglycerol)**, and subsequently, a rise in intracellular **calcium**, causing smooth muscle contraction.
*GoPCRs (Go protein-coupled receptors)*
- While Go proteins are a subtype of Gi/Go family, their direct primary role in mediating **urinary retention** via **adrenergic agonism** is not as well-established as Gq.
- Go signaling often involves modulation of **ion channels** and can be involved in neuronal signaling, not directly causing smooth muscle contraction in the bladder.
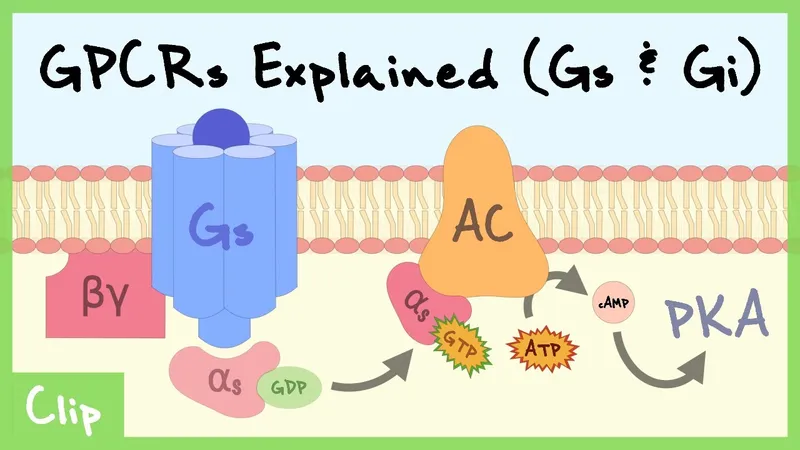
*GsPCRs (Gs protein-coupled receptors)*
- **GsPCRs** (e.g., beta-adrenergic receptors) activate **adenylate cyclase**, leading to increased **cAMP** levels, which typically causes smooth muscle relaxation.
- This effect would promote **urinary relaxation** and flow, not retention, and hence is contrary to the observed drug effect.
*GtPCRs (Gt protein-coupled receptors)*
- **GtPCRs** (transducin) are primarily involved in the **phototransduction** cascade in the retina, mediating vision.
- They have no known central role in mediating adrenergic effects on the **urinary tract smooth muscle**.
*GiPCRs (Gi protein-coupled receptors)*
- **GiPCRs** (e.g., alpha-2 adrenergic receptors) inhibit **adenylate cyclase**, leading to decreased **cAMP** levels, which generally causes smooth muscle contraction in some tissues, but also presynaptic inhibition.
- While Gi activation can lead to contraction in some contexts, the primary mechanism of **urinary retention** via bladder neck contraction is through alpha-1 receptors linked to Gq.
G-protein coupled receptors US Medical PG Question 2: A 47-year-old woman presents to a local medical shelter while on a mission trip with her church to help rebuild homes after a hurricane. She has been experiencing severe nausea, vomiting, and diarrhea for the last 2 days and was feeling too fatigued to walk this morning. On presentation, her temperature is 99.2°F (37.3°C), blood pressure is 95/62 mmHg, pulse is 121/min, and respirations are 17/min. Physical exam reveals decreased skin turgor, and a stool sample reveals off-white watery stools. Gram stain reveals a gram-negative, comma-shaped organism that produces a toxin. Which of the following is consistent with the action of the toxin most likely involved in the development of this patient's symptoms?
- A. Decreased ribosomal activity
- B. Increased membrane permeability
- C. Cleavage of junctional proteins
- D. Increased adenylyl cyclase activity (Correct Answer)
- E. Activation of receptor tyrosine kinase
G-protein coupled receptors Explanation: ***Increased adenylyl cyclase activity***
- The patient's symptoms (severe nausea, vomiting, diarrhea, dehydration, **hypotension**, and **tachycardia**) along with the presence of a **gram-negative, comma-shaped organism** producing an off-white watery stool are highly suggestive of **Cholera** caused by *Vibrio cholerae*.
- Cholera toxin is an **AB5 toxin** that irreversibly activates **adenylyl cyclase** in intestinal epithelial cells, leading to increased intracellular cyclic AMP (cAMP) levels. This increased cAMP then causes massive secretion of chloride and bicarbonate into the intestinal lumen, followed by water, resulting in the characteristic **"rice-water stool"**.
*Decreased ribosomal activity*
- This mechanism is characteristic of toxins like **Shiga toxin** (produced by *Shigella dysenteriae* and enterohemorrhagic *E. coli*) and **diphtheria toxin** (produced by *Corynebacterium diphtheriae*).
- These toxins inhibit protein synthesis by inactivating the 60S ribosomal subunit, which typically leads to **cytotoxicity** rather than the profuse watery diarrhea seen in cholera.
*Increased membrane permeability*
- Some toxins, such as **alpha-toxin** of *Clostridium perfringens* (gas gangrene) or **pore-forming toxins**, increase membrane permeability by creating pores in cell membranes.
- While this can lead to cell damage and lysis, it is not the primary mechanism by which the cholera toxin causes massive fluid secretion.
*Cleavage of junctional proteins*
- Toxins that cleave **tight junction proteins** (e.g., *Clostridium difficile* toxins A and B) can disrupt the intestinal barrier and lead to fluid leakage.
- However, the main mechanism of cholera toxin is fluid secretion due to ion channel activation rather than direct disruption of intercellular junctions.
*Activation of receptor tyrosine kinase*
- Activation of **receptor tyrosine kinases** is typically involved in cell growth, differentiation, and metabolism, not directly in acute, severe secretory diarrhea.
- While some bacterial toxins can modulate host signaling pathways, direct activation of receptor tyrosine kinases is not the primary mechanism of action for toxins causing cholera-like symptoms.
G-protein coupled receptors US Medical PG Question 3: A 25-year-old man presents to the physician with 2 days of profuse, watery diarrhea. He denies seeing blood or mucus in the stools. On further questioning, he reveals that he eats a well-balanced diet and generally prepares his meals at home. He remembers having some shellfish from a street vendor 3 days ago. He takes no medications. His past medical history is unremarkable. Which of the following mechanisms most likely accounts for this patient’s illness?
- A. Tyrosine kinase phosphorylation
- B. ADP-ribosylation of Gs protein (Correct Answer)
- C. Tyrosine kinase dephosphorylation
- D. Osmotic effect of intestinal contents
- E. Inflammation of the gastrointestinal wall
G-protein coupled receptors Explanation: ***ADP-ribosylation of Gs protein***
- The patient's history of consuming **shellfish from a street vendor** and presenting with **profuse, watery diarrhea** strongly suggests **cholera**.
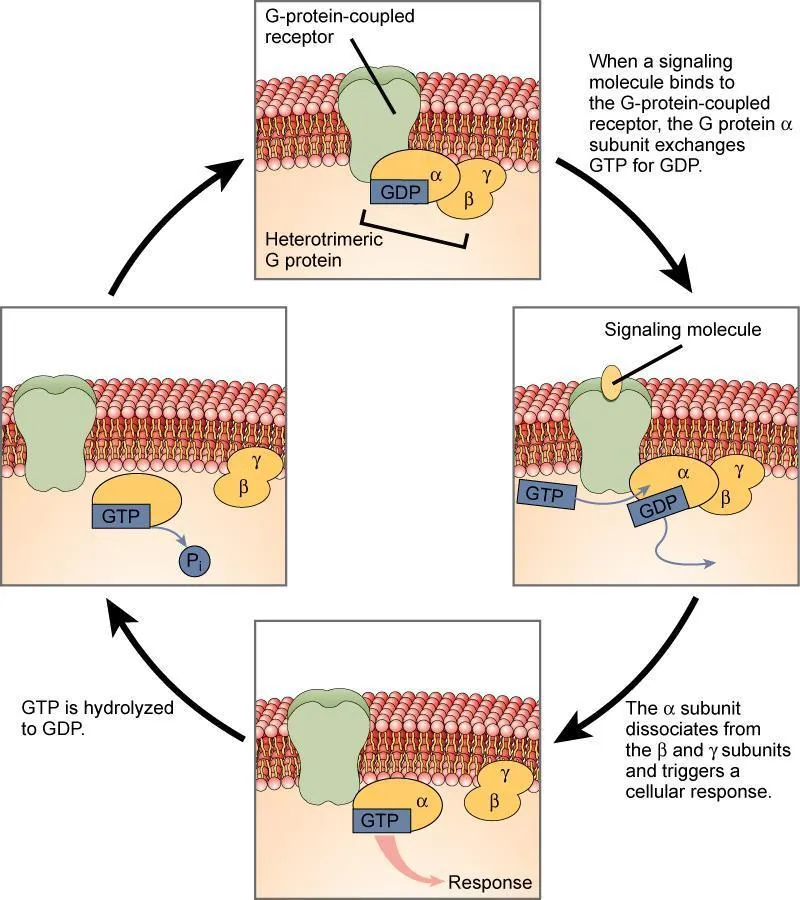
- **Cholera toxin** works by irreversibly ADP-ribosylating the **Gs alpha subunit**, leading to constitutive activation of **adenylate cyclase** and increased intracellular **cAMP**, which causes excessive fluid and electrolyte secretion into the intestinal lumen.
*Tyrosine kinase phosphorylation*
- This mechanism is characteristic of signaling pathways involved in growth and differentiation, often seen with **growth factor receptors**, and is not the primary cause of acute, watery diarrhea from food poisoning.
- While some bacterial toxins can affect intracellular signaling, **tyrosine kinase phosphorylation** is not the direct mechanism for the massive fluid loss seen in cholera.
*Tyrosine kinase dephosphorylation*
- This process typically downregulates cell signaling pathways, which would likely **decrease** cellular activity, rather than trigger the profuse secretion seen in this patient's presentation.
- It is not a known mechanism for the pathogenesis of infectious diarrheal diseases such as cholera.
*Osmotic effect of intestinal contents*
- While **osmotic diarrhea** is characterized by the presence of non-absorbable solutes in the gut lumen, drawing water in, the history here points more to an actively secreted fluid loss.
- The sheer volume and rapid onset of the diarrhea suggest an active secretory mechanism rather than simply an osmotic effect from malabsorption.
*Inflammation of the gastrointestinal wall*
- **Inflammatory diarrhea** typically involves blood or mucus in the stool, fever, and abdominal pain, none of which are reported by the patient.
- The patient's "profuse, watery" diarrhea without blood or mucus signifies a non-inflammatory, secretory etiology often caused by toxins.
G-protein coupled receptors US Medical PG Question 4: A stool sample was taken from a 19-year-old male who presented with profuse watery diarrhea. He recently returned from a trip to Central America. A microbiologist identified the causative agent as a gram-negative, oxidase-positive, comma-shaped bacteria that is able to grow well in a pH > 8. Which of the following is a mechanism of action of the toxin produced by this bacteria?
- A. Overactivation of adenylate cyclase by inhibition of Gi subunit by ADP-ribosylation
- B. Inactivation of the 60S ribosomal subunit by cleaving an adenine from the 28S rRNA
- C. Overactivation of guanylate cyclase
- D. Overactivation of adenylate cyclase by activation of Gs subunit by ADP-ribosylation (Correct Answer)
- E. Degradation of cell membranes by hydrolysis of the phospholipids
G-protein coupled receptors Explanation: ***Overactivation of adenylate cyclase by activation of Gs subunit by ADP-ribosylation***
- The description of the bacterium as **gram-negative, oxidase-positive, comma-shaped, growing well in pH > 8**, and causing **profuse watery diarrhea** after travel to Central America points to *Vibrio cholerae*.
- **Cholera toxin** (CTX) produced by *V. cholerae* is an A-B toxin that **ADP-ribosylates the Gs α-subunit**, permanently activating **adenylate cyclase**. This leads to increased cAMP levels, causing secretion of water and electrolytes into the intestinal lumen.
*Overactivation of adenylate cyclase by inhibition of Gi subunit by ADP-ribosylation*
- This mechanism describes the action of **pertussis toxin** from *Bordetella pertussis*, which ADP-ribosylates and **inhibits the Gi subunit**, preventing adenylate cyclase inhibition.
- While both ultimately increase cAMP, the specific target and mechanism (inhibition of Gi vs. activation of Gs) differ from cholera toxin.
*Inactivation of the 60S ribosomal subunit by cleaving an adenine from the 28S rRNA*
- This mechanism is characteristic of **Shiga toxin** produced by *Shigella dysenteriae* and Shiga-like toxins (verotoxins) produced by **enterohemorrhagic *E. coli*** (EHEC).
- These toxins inhibit protein synthesis, leading to cell death and often bloody diarrhea and hemolytic uremic syndrome, which is not described here.
*Overactivation of guanylate cyclase*
- **Heat-stable enterotoxins (ST)** produced by **enterotoxigenic *E. coli*** (ETEC) activate **guanylate cyclase**, leading to increased cGMP and subsequent fluid secretion.
- While ETEC can cause watery diarrhea, the bacterial characteristics provided (oxidase-positive, comma-shaped) do not fit *E. coli*.
*Degradation of cell membranes by hydrolysis of the phospholipids*
- This mechanism is associated with toxins like **phospholipases** or **lecithinases** (e.g., alpha-toxin of *Clostridium perfringens*).
- These toxins cause direct cell lysis and tissue damage, which is not the primary mechanism of action for the watery diarrhea seen in cholera.
G-protein coupled receptors US Medical PG Question 5: Which neurotransmitter is primarily responsible for parasympathetic effects on heart rate?
- A. Norepinephrine
- B. Dopamine
- C. Acetylcholine (Correct Answer)
- D. Epinephrine
G-protein coupled receptors Explanation: ***Acetylcholine***
- **Acetylcholine** is the primary neurotransmitter released by postganglionic parasympathetic neurons.
- It acts on **muscarinic receptors** (M2 receptors) in the heart to decrease heart rate.
*Norepinephrine*
- **Norepinephrine** is primarily associated with the **sympathetic nervous system**, increasing heart rate and contractility.
- It acts on **beta-1 adrenergic receptors** in the heart.
*Dopamine*
- **Dopamine** is a precursor to norepinephrine and epinephrine, and primarily functions as a neurotransmitter in the **central nervous system** and in regulating renal blood flow.
- While it can have cardiac effects, it is not the primary neurotransmitter for parasympathetic actions on heart rate.
*Epinephrine*
- **Epinephrine** (adrenaline) is a hormone released by the adrenal medulla and a neurotransmitter in the sympathetic nervous system, causing an **increase in heart rate** and contractility.
- It works through **beta-1 adrenergic receptors**, antagonistic to parasympathetic effects.
G-protein coupled receptors US Medical PG Question 6: A 78-year-old man receives chemotherapy for advanced hepatocellular carcinoma. Despite appropriate therapy, he dies 4 months later. Histopathological examination of the cancer cells shows the presence of a transmembrane efflux pump protein that is known to cause decreased intracellular concentrations of chemotherapeutic drugs. Which of the following best describes this membrane protein?
- A. G protein
- B. Cadherin
- C. P-glycoprotein (Correct Answer)
- D. Tyrosine receptor
- E. Channel protein
G-protein coupled receptors Explanation: **P-glycoprotein**
- **P-glycoprotein** (also known as **MDR1**) is a well-known **efflux pump** that actively transports many chemotherapy drugs out of cancer cells, leading to **multidrug resistance**.
- Its presence explains the **decreased intracellular concentrations** of chemotherapy drugs and the poor response to treatment in this patient.
*G protein*
- **G proteins** are intracellular signaling molecules that mediate responses to various extracellular stimuli, not primarily involved in drug efflux.
- They are typically associated with **G protein-coupled receptors** and downstream signaling pathways, not direct drug transport.
*Cadherin*
- **Cadherins** are cell adhesion molecules that play a crucial role in cell-cell binding and maintaining tissue structure.
- They are not involved in the active transport of drugs across the cell membrane.
*Tyrosine receptor*
- **Tyrosine kinase receptors** are transmembrane proteins that bind to growth factors and initiate intracellular signaling cascades, promoting cell growth and differentiation.
- They are involved in signaling, not in the active transport of chemotherapy drugs out of the cell.
*Channel protein*
- **Channel proteins** facilitate the passive diffusion of ions or small molecules across the cell membrane, typically down their electrochemical gradient.
- While they are transmembrane proteins, they do not actively pump drugs out against a concentration gradient, which is characteristic of multidrug resistance.
G-protein coupled receptors US Medical PG Question 7: An investigator is studying the principles of cell-to-cell signaling of the autonomic nervous system. It is found that the adrenal medulla has receptors that, when activated, result in the immediate opening of Na+, Ca2+, and K+ channels, which subsequently leads to the secretion of epinephrine and norepinephrine. These receptors are structurally most similar to which of the following receptors?
- A. Alpha 1 receptors of the bladder neck
- B. D2 receptors of the basal ganglia
- C. M2 receptors of heart
- D. NM receptors of the quadriceps femoris muscle (Correct Answer)
- E. H2 receptors of the stomach
G-protein coupled receptors Explanation: ***NM receptors of the quadriceps femoris muscle***
- The adrenal medulla's chromaffin cells are modified **postganglionic sympathetic neurons** that release catecholamines upon stimulation by preganglionic neurons.
- The activation of **Na+, Ca2+, and K+ channels** leading to rapid depolarization and neurotransmitter release is characteristic of **nicotinic acetylcholine receptors (NM type)**, which are ligand-gated ion channels.
*Alpha 1 receptors of the bladder neck*
- **Alpha-1 receptors** are **G-protein coupled receptors** that primarily activate phospholipase C, leading to increased intracellular calcium and smooth muscle contraction.
- Their activation does not directly result in the immediate opening of Na+, Ca2+, and K+ channels.
*D2 receptors of the basal ganglia*
- **D2 receptors** are **G-protein coupled receptors**, specifically inhibitory (Gi-coupled), that decrease adenylyl cyclase activity and reduce intracellular cAMP.
- They do not function as direct ligand-gated ion channels.
*M2 receptors of heart*
- **M2 receptors** are **G-protein coupled receptors** (Gi-coupled) that decrease heart rate by inhibiting adenylyl cyclase and opening potassium channels indirectly via G-protein subunits.
- While they affect ion channels, this is an indirect G-protein mediated process, not a direct ligand-gated ion channel mechanism.
*H2 receptors of the stomach*
- **H2 receptors** are **G-protein coupled receptors** (Gs-coupled) that increase adenylyl cyclase activity, leading to increased cAMP and stimulation of gastric acid secretion.
- They are not ligand-gated ion channels and do not directly open Na+, K+, and Ca2+ channels.
G-protein coupled receptors US Medical PG Question 8: An investigator is studying the structure of the amino-terminal of the Huntingtin protein using x-ray crystallography. The terminal region is determined to have an α-helix conformation. Which of the following forces is most likely responsible for maintaining this conformation?
- A. Electrostatic side chain attraction
- B. Hydrophobic interactions
- C. Hydrogen bonds (Correct Answer)
- D. Disulfide bonds
- E. Peptide bonds
G-protein coupled receptors Explanation: **Correct: Hydrogen bonds**
- **Hydrogen bonds** are the primary forces responsible for stabilizing the regular secondary structures of proteins, such as **α-helices**.
- In an α-helix, hydrogen bonds form between the **carbonyl oxygen** of one peptide bond and the **amide hydrogen** of a peptide bond four residues away, creating a stable coiled structure.
- This backbone hydrogen bonding pattern is the defining characteristic of the α-helix conformation.
*Incorrect: Electrostatic side chain attraction*
- While important for **tertiary and quaternary structures**, electrostatic interactions between charged **R-groups** are not the primary forces defining the backbone conformation of an α-helix.
- These forces arise from charged side chains, which may influence helix stability but do not form the fundamental helical structure.
*Incorrect: Hydrophobic interactions*
- **Hydrophobic interactions** are crucial for maintaining **tertiary and quaternary protein structures**, especially in an aqueous environment, by driving nonpolar residues to the interior of the protein.
- They do not directly stabilize the backbone structure of the α-helix itself.
*Incorrect: Disulfide bonds*
- **Disulfide bonds** are **covalent bonds** between two cysteine residues and are involved in stabilizing the **tertiary and quaternary structure** of proteins.
- They are not typically found within α-helices and are not the primary force responsible for forming the helical shape.
*Incorrect: Peptide bonds*
- **Peptide bonds** are the **covalent bonds** that link amino acids together to form the primary sequence of a polypeptide chain.
- While essential for the very existence of the protein sequence, they do not dictate the specific **α-helical conformation**; rather, the rotation around these bonds (phi and psi angles) allows for various secondary structures, which are then stabilized by hydrogen bonds.
G-protein coupled receptors US Medical PG Question 9: An 11-month-old boy is brought to a pediatrician by his parents with a recurrent cough, which he has had since the age of 2 months. He has required 3 hospitalizations for severe wheezing episodes. His mother also mentions that he often has diarrhea. The boy’s detailed history reveals that he required hospitalization for meconium ileus during the neonatal period. Upon physical examination, his temperature is 37.0°C (98.6ºF), pulse rate is 104/min, respiratory rate is 40/min, and blood pressure is 55/33 mm Hg. An examination of the boy’s respiratory system reveals the presence of bilateral wheezing and scattered crepitations. An examination of his cardiovascular system does not reveal any abnormality. His length is 67.3 cm (26.5 in) and weight is 15 kg (33 lbs). His sweat chloride level is 74 mmol/L. His genetic evaluation confirms that he has an autosomal recessive disorder resulting in a dysfunctional membrane-bound protein. Which of the following best describes the mechanism associated with the most common mutation that causes this disorder?
- A. Decreased chloride transport through the protein
- B. Disordered regulation of the protein
- C. Decreased transcription of the protein due to splicing defect
- D. Complete absence of the protein
- E. Defective maturation and early degradation of the protein (Correct Answer)
G-protein coupled receptors Explanation: ***Defective maturation and early degradation of the protein***
- The clinical picture (recurrent cough, wheezing, diarrhea, meconium ileus, elevated sweat chloride, autosomal recessive inheritance) strongly points to **cystic fibrosis (CF)**. The most common mutation in CF is **F508del**, which leads to misfolding of the **CFTR protein**, causing retention in the endoplasmic reticulum and subsequent degradation before reaching the cell membrane.
- This **defective processing and early degradation** result in a significant reduction or absence of functional CFTR protein at the cell surface, leading to impaired chloride transport.
*Decreased chloride transport through the protein*
- While **decreased chloride transport** is the ultimate functional consequence of cystic fibrosis, it is not the direct mechanism associated with the **F508del mutation's impact** on the CFTR protein itself.
- This option describes the **physiological result** of the protein defect, not the cellular/molecular mechanism of the most common mutation.
*Disordered regulation of the protein*
- **Disordered regulation** could be a potential mechanism for some CFTR mutations (Class IV mutations), affecting how the channel opens and closes or responds to signaling.
- However, for the **F508del mutation** (Class II mutation), the primary issue is the **lack of properly localized protein** due to misfolding and degradation, rather than a problem with the regulation or gating of the protein once it reaches the membrane.
*Decreased transcription of the protein due to splicing defect*
- **Decreased transcription** or **splicing defects** (Class I and V mutations) would result in reduced mRNA levels or incorrectly formed mRNA, leading to less protein synthesis.
- The **F508del mutation** involves a deletion of three nucleotides in exon 10, leading to a missing phenylalanine at position 508. Importantly, **transcription and splicing occur normally**; the mRNA is produced correctly. The problem arises at the **post-translational level** with protein folding, not at the transcriptional or splicing level.
*Complete absence of the protein*
- While functional CFTR protein is largely absent at the cell surface in F508del, the protein is **initially synthesized** in the endoplasmic reticulum.
- The problem is its **misfolding and rapid degradation**, preventing it from reaching the membrane, rather than a complete failure of protein synthesis from the outset (which would be seen in nonsense or frameshift mutations causing Class I defects).
G-protein coupled receptors US Medical PG Question 10: A research team discovers a novel bacterial toxin that causes severe hypotension in infected patients. In vitro studies show the toxin ADP-ribosylates a specific amino acid on Gq alpha subunits, preventing their activation by GPCRs. Patients develop hypotension despite elevated levels of vasopressin, angiotensin II, and endothelin-1. Synthesize the pathophysiological mechanism explaining why multiple vasopressor hormones fail to maintain blood pressure in these patients.
- A. The toxin depletes intracellular ATP preventing myosin-actin interaction
- B. The toxin prevents receptor binding of vasopressor hormones through allosteric inhibition
- C. ADP-ribosylation of Gq prevents PLC activation, blocking IP3-mediated calcium release and vascular smooth muscle contraction (Correct Answer)
- D. ADP-ribosylation increases cAMP levels causing smooth muscle relaxation
- E. The toxin activates Gi proteins causing excessive vasodilation that overwhelms vasoconstrictor signals
G-protein coupled receptors Explanation: ***ADP-ribosylation of Gq prevents PLC activation, blocking IP3-mediated calcium release and vascular smooth muscle contraction***
- Vasopressor hormones like **Vasopressin**, **Angiotensin II**, and **Endothelin-1** signal through **Gq-coupled receptors** to trigger **vascular smooth muscle contraction**.
- By ADP-ribosylating the **Gq alpha subunit**, the toxin inhibits **Phospholipase C (PLC)**, preventing the generation of **IP3 and DAG**, which are essential for releasing **intracellular calcium**.
*The toxin prevents receptor binding of vasopressor hormones through allosteric inhibition*
- The toxin targets the **G-protein (intracellular)** rather than the **extracellular binding site** of the G-protein coupled receptors (GPCRs).
- Since binding still occurs but **signal transduction** is blocked, this describes a post-receptor defect rather than **allosteric inhibition** of the receptor itself.
*The toxin activates Gi proteins causing excessive vasodilation that overwhelms vasoconstrictor signals*
- The prompt explicitly states the toxin modifies the **Gq alpha subunit**, not the **Gi subunit**.
- **Gi protein** activation primarily lowers **cAMP**, whereas the failure of pressors in this case is linked to the lack of **calcium mobilization** via Gq.
*ADP-ribosylation increases cAMP levels causing smooth muscle relaxation*
- Increased **cAMP** (via Gs activation or Gi inhibition) does cause relaxation, but this mechanism is associated with toxins like **Cholera** or **Pertussis**.
- The modification of **Gq** specifically disrupts the **phosphoinositol pathway**, not the **adenylyl cyclase** pathway that regulates cAMP.
*The toxin depletes intracellular ATP preventing myosin-actin interaction*
- ADP-ribosylation is a specific **post-translational modification** using **NAD+** as a substrate, which does not result in systemic **ATP depletion**.
- The failure of contraction is due to a lack of **calcium-calmodulin** activation of **Myosin Light Chain Kinase (MLCK)**, not a lack of energy supply for the motor proteins.
More G-protein coupled receptors US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.