Mutation types and consequences US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Mutation types and consequences. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Mutation types and consequences US Medical PG Question 1: A 25-year-old female comes to the clinic complaining of fatigue and palpitations. She has been undergoing immense stress from her thesis defense and has been extremely tired. The patient denies any weight loss, diarrhea, cold/heat intolerance. TSH was within normal limits. She reports a family history of "blood disease" and was later confirmed positive for β-thalassemia minor. It is believed that abnormal splicing of the beta globin gene results in β-thalassemia. What is removed during this process that allows RNA to be significantly shorter than DNA?
- A. 3'-poly(A) tail
- B. Exons
- C. Introns (Correct Answer)
- D. microRNAs
- E. snRNPs
Mutation types and consequences Explanation: **Introns**
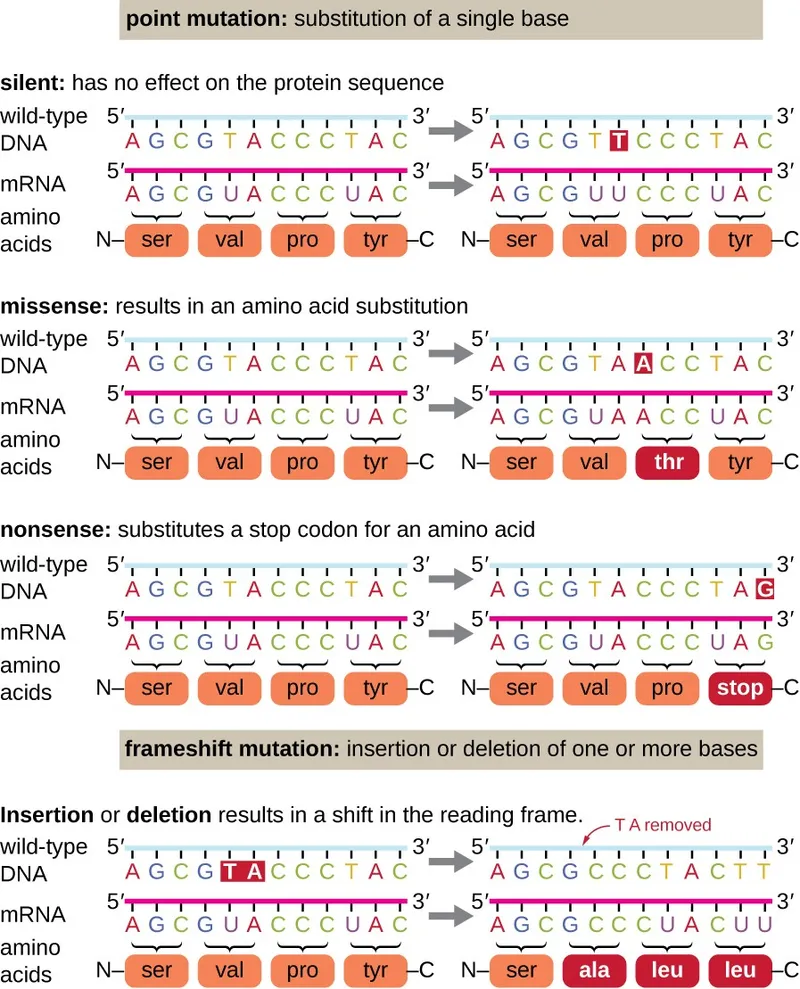
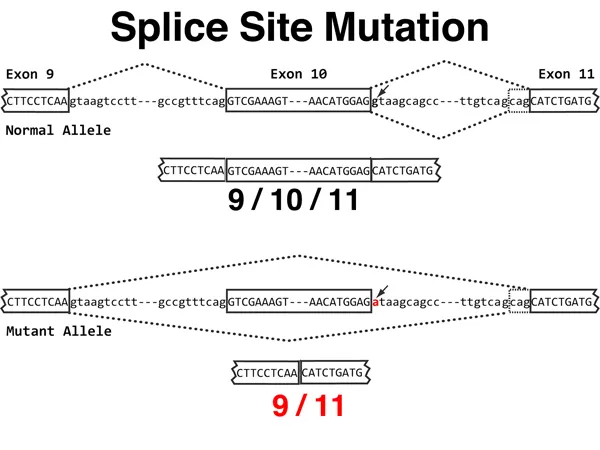
- **Introns** are non-coding regions within a gene that are removed from the pre-mRNA transcript during **splicing**.
- This removal and the subsequent ligation of exons lead to a mature mRNA molecule that is significantly shorter than the initial DNA template.
*3'-poly(A) tail*
- The **3'-poly(A) tail** is an addition to the 3' end of the mRNA molecule, not a removed segment during splicing, and it provides stability and aids in translation.
- While it contributes to mRNA processing, its addition does not involve removing existing sequences to shorten the transcript.
*Exons*
- **Exons** are the coding regions of a gene that are retained and ligated together to form the mature mRNA, which is then translated into protein.
- If exons were removed, the resulting protein would be truncated or non-functional, and the mRNA would not contain the necessary genetic information.
*microRNAs*
- **MicroRNAs (miRNAs)** are small non-coding RNA molecules that regulate gene expression by inhibiting translation or promoting mRNA degradation.
- They are not part of the pre-mRNA transcript that is processed into mRNA; rather, they are distinct regulatory molecules.
*snRNPs*
- **Small nuclear ribonucleoproteins (snRNPs)** are components of the spliceosome, the molecular machine responsible for carrying out splicing.
- They are involved in the process of intron removal but are not themselves removed from the RNA; they are catalytic machinery.
Mutation types and consequences US Medical PG Question 2: A 4-year-old boy with beta thalassemia requires regular blood transfusions a few times per month because of persistent anemia. He is scheduled for a splenectomy in the next several months. Samples obtained from the boy’s red blood cells show a malformed protein with a length of 160 amino acids (in normal, healthy red blood cells, the functional protein has a length of 146 amino acids). Which of the following best accounts for these findings?
- A. Nonsense mutation
- B. Silent mutation
- C. Missense mutation
- D. Splice site mutation (Correct Answer)
- E. Frameshift mutation
Mutation types and consequences Explanation: ***Splice site mutation***
- A **splice site mutation** can lead to the retention of an **intron** or the **skipping of an exon**, resulting in an abnormal mRNA sequence.
- If a cryptic splice site is used or an intron is retained, it can lead to the inclusion of additional amino acids in the final protein, thus increasing its length from 146 to 160 amino acids.
*Nonsense mutation*
- A **nonsense mutation** results in a **premature stop codon**, which would produce a **truncated protein** shorter than 146 amino acids.
- This type of mutation does not explain the observed increase in protein length.
*Silent mutation*
- A **silent mutation** changes a single nucleotide but does **not alter the amino acid sequence** of the protein due to the redundancy of the genetic code.
- This would result in a normal protein length of 146 amino acids and no observed malformation.
*Missense mutation*
- A **missense mutation** changes a single nucleotide leading to a **different amino acid**, but it typically **does not alter the total length** of the protein.
- While it can lead to a *malformed protein*, it wouldn't explain the increased length from 146 to 160 amino acids.
*Frameshift mutation*
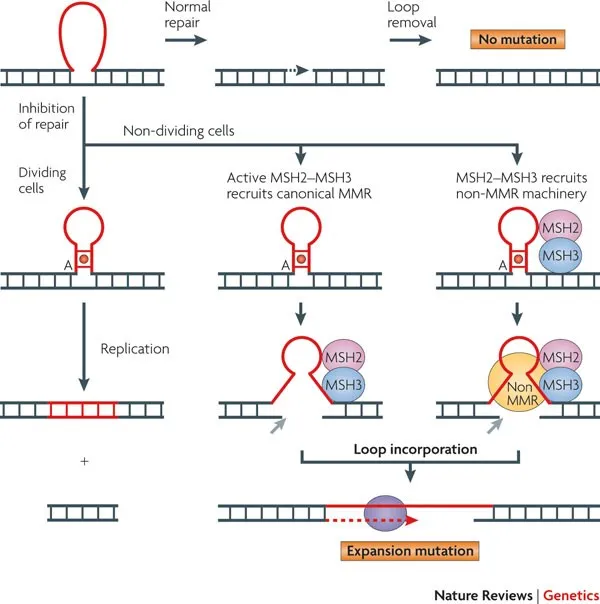
- A **frameshift mutation** is caused by the **insertion or deletion of nucleotides** not divisible by three, leading to a shift in the reading frame downstream.
- This often results in a **premature stop codon** and a **shorter, non-functional protein**, or a completely altered sequence that is usually unstable, rather than a longer protein with 160 amino acids.
Mutation types and consequences US Medical PG Question 3: A 33-year-old man presents to his physician with a 3-year history of gradually worsening tics and difficulty walking. He was last seen by the physician 5 years ago for anxiety, and he has been buying anti-anxiety medications from an internet website without a prescription as he cannot afford to pay for doctor’s visits. Now, the patient notes that his anxiety is somewhat controlled, but motor difficulties are making it difficult for him to work and socialize. Family history is unobtainable as his parents died in an accident when he was an infant. He grew up in foster care and was always a bright child. An MRI of the brain is ordered; it shows prominent atrophy of the caudate nucleus. Repeats of which of the following trinucleotides are most likely responsible for this patient’s disorder?
- A. CCG
- B. CTG
- C. CGG
- D. CAG (Correct Answer)
- E. GAA
Mutation types and consequences Explanation: ***CAG***
- The clinical presentation of **worsening tics**, **difficulty walking** (suggesting motor dysfunction), and the MRI finding of **caudate nucleus atrophy** are classic signs of **Huntington's disease**.
- **Huntington's disease** is an autosomal dominant neurodegenerative disorder caused by an unstable expansion of **CAG trinucleotide repeats** within the *HTT* gene.
*CCG*
- Expansions of **CCG repeats** are associated with conditions like **fragile X-associated tremor/ataxia syndrome (FXTAS)**.
- While FXTAS involves neurological symptoms, the specific presentation of prominent tics and caudate atrophy points more strongly to Huntington's.
*CTG*
- **CTG trinucleotide repeat** expansions are characteristic of **myotonic dystrophy type 1 (DM1)**.
- Myotonic dystrophy primarily manifests with muscle weakness, myotonia, and cataracts, which are not the primary presenting symptoms here.
*CGG*
- Expansions of **CGG repeats** are the genetic basis of **Fragile X syndrome**, the most common inherited cause of intellectual disability.
- While Fragile X syndrome can have neurological features, it typically presents with developmental delay and distinctive physical features, rather than adult-onset tics and caudate atrophy.
*GAA*
- An expansion of **GAA trinucleotide repeats** is responsible for **Friedreich's ataxia**.
- Friedreich's ataxia is characterized by progressive ataxia, dysarthria, and loss of proprioception, which differ from the motor tics and specific caudate atrophy seen in this patient.
Mutation types and consequences US Medical PG Question 4: An 8-year-old African American girl is brought to the clinic by her mother for her regular blood exchange. They come in every 2–3 months for the procedure. The child is in good health with no symptoms. Her last trip to the emergency department was 6 months ago due to bone pain. She was treated with morphine and oxygen and a blood transfusion. She takes hydroxyurea and folic acid daily. She has an uncle that also has to get blood exchanges. Today, her heart rate is 90/min, respiratory rate is 17/min, blood pressure is 110/65 mm Hg, and temperature is 37.0°C (98.6°F). She calmly waits for the machine to be set up and catheters inserted into both of her arms. She watches a movie as her blood is slowly replaced with 6 L of red blood cells. Based on this history, which of the following mechanisms most likely explains this patient's condition?
- A. Nonsense mutation
- B. Amino acid substitution (Correct Answer)
- C. Enzyme deficiency
- D. Amino acid deletion
- E. Trinucleotide repeat
Mutation types and consequences Explanation: ***Amino acid substitution***
- This patient's symptoms (bone pain requiring emergency treatment, need for chronic exchange transfusions, hydroxyurea therapy, African American ethnicity, family history) are characteristic of **sickle cell disease**
- Sickle cell disease is caused by a **single point mutation** (GAG → GTG) in the beta-globin gene, resulting in substitution of **glutamic acid with valine at position 6** of the beta-globin chain
- This amino acid substitution causes hemoglobin to polymerize under low oxygen conditions, leading to **sickling of red blood cells** and vaso-occlusive crises
*Nonsense mutation*
- A nonsense mutation creates a **premature stop codon**, resulting in a **truncated, nonfunctional protein**
- This mechanism causes conditions like **beta-thalassemia major** (some cases), but is not the mechanism of sickle cell disease
- Sickle cell involves a missense mutation (amino acid substitution), not a nonsense mutation
*Enzyme deficiency*
- Enzyme deficiencies such as **glucose-6-phosphate dehydrogenase (G6PD) deficiency** or **pyruvate kinase deficiency** can cause hemolytic anemias
- However, these typically present with episodic hemolysis triggered by oxidative stress, not chronic vaso-occlusive crises requiring regular exchange transfusions
- The mechanism in sickle cell disease is a **structural hemoglobin defect**, not an enzyme deficiency
*Amino acid deletion*
- An amino acid deletion involves **removal of one or more amino acids** from the protein sequence
- This mechanism causes conditions like **cystic fibrosis** (ΔF508 deletion in CFTR protein)
- Sickle cell disease involves **substitution**, not deletion of an amino acid
*Trinucleotide repeat*
- Trinucleotide repeat disorders involve **expansion of a three-nucleotide sequence** within a gene, showing anticipation across generations
- Examples include **Huntington disease (CAG repeats)**, **myotonic dystrophy (CTG repeats)**, and **fragile X syndrome (CGG repeats)**
- These affect neurological or muscular function and are unrelated to hemoglobinopathies
Mutation types and consequences US Medical PG Question 5: A 3-year-old boy is brought to the physician for a well-child examination. He has had multiple falls while walking and running for the past 4 months. He used to be able to climb stairs independently but now requires assistance. He started speaking in 2-word sentences at 2 years of age. He is at the 50th percentile for height and the 60th percentile for weight. Examination shows a waddling gait and enlargement of bilateral calves. Muscle strength is decreased in the bilateral lower extremities. Patellar and ankle reflexes are 1+ bilaterally. To rise from a sitting position, he uses his hands to support himself to an upright position. Diagnosis is confirmed by a muscle biopsy and immunohistochemistry. Which of the following is most likely responsible for the most severe clinical presentation of this disease?
- A. Frameshift mutation (Correct Answer)
- B. Missense mutation
- C. Silent mutation
- D. Splice site mutation
- E. Same sense mutation
Mutation types and consequences Explanation: ***Frameshift mutation***
- The patient's presentation with **waddling gait**, **Gowers' sign**, **calf pseudohypertrophy**, and progressive muscle weakness is characteristic of **Duchenne Muscular Dystrophy (DMD)**.
- **Frameshift mutations** in the **dystrophin gene** lead to a premature stop codon, resulting in a severely truncated and non-functional dystrophin protein, causing the most severe form of the disease.
*Missense mutation*
- A **missense mutation** results in a single amino acid change, which may lead to a partially functional protein.
- This type of mutation typically causes **Becker Muscular Dystrophy (BMD)**, which is a milder form compared to DMD, with later onset and slower progression.
*Silent mutation*
- A **silent mutation** codes for the same amino acid, having no effect on the protein sequence or function.
- Therefore, it would not lead to any clinical disease, let alone the severe presentation described.
*Splice site mutation*
- A **splice site mutation** can lead to altered mRNA splicing, potentially resulting in exon skipping or intron retention.
- If the mutation disrupts the reading frame (out-of-frame), it causes DMD with complete loss of dystrophin; if the reading frame is maintained (in-frame), it causes milder BMD with partially functional dystrophin.
- However, a frameshift mutation specifically guarantees reading frame disruption and the most severe phenotype.
*Same sense mutation*
- This term is synonymous with a **silent mutation** or a **synonymous mutation**, meaning it results in the same, unchanged amino acid sequence due to the redundancy of the genetic code.
- As such, it would not alter protein function and would not cause a clinical disease.
Mutation types and consequences US Medical PG Question 6: An 8-year-old girl is brought to the pediatrician because she is significantly shorter than her classmates. Her mother notes that she has had thick, oral secretions for the past several months, along with a chronic cough. Her exam is notable for clubbed fingernails. Her pediatrician sends a genetic test for a transmembrane channel mutation, which shows a normal DNA sequence, except for the deletion of three nucleotides that code for a phenylalanine at position 508. What type of mutation has caused her presentation?
- A. Triplet expansion
- B. Nonsense mutation
- C. Frameshift mutation
- D. In-frame mutation (Correct Answer)
- E. Silent mutation
Mutation types and consequences Explanation: ***In-frame mutation***
- The deletion of three nucleotides, which together code for a single amino acid (phenylalanine), results in an **in-frame mutation** because the reading frame of the mRNA is maintained.
- This specific mutation is **ΔF508**, the most common mutation in **cystic fibrosis (CF)**, consistent with the patient's symptoms of growth failure, thick secretions, chronic cough, and clubbed fingernails.
*Triplet expansion*
- This involves the **increase in the number of repeats of a trinucleotide sequence**, such as in Huntington's disease or fragile X syndrome.
- The patient's mutation is a **deletion**, not an expansion of a trinucleotide repeat.
*Nonsense mutation*
- A nonsense mutation involves a **point mutation** that results in a **premature stop codon**, leading to a truncated protein.
- The patient's mutation is a **deletion of an entire codon**, not a single base change leading to a stop codon.
*Frameshift mutation*
- A frameshift mutation occurs when the deletion or insertion of nucleotides is **not a multiple of three**, leading to a shift in the reading frame and alteration of all downstream amino acids.
- In this case, the deletion of **three nucleotides** maintains the reading frame, so it is not a frameshift.
*Silent mutation*
- A silent mutation is a **point mutation** where a change in a single nucleotide does not alter the amino acid sequence due to the degeneracy of the genetic code.
- Here, the **deletion of a codon** results in the loss of an amino acid, clearly altering the protein product, hence it is not silent.
Mutation types and consequences US Medical PG Question 7: A 5-year-old boy is brought to the emergency department after he fell on the playground in kindergarten and was unable to get up. His right leg was found to be bent abnormally at the femur, and he was splinted on site by first responders. His past medical history is significant for multiple prior fractures in his left humerus and femur. Otherwise, he has been hitting normal developmental milestones and appears to be excelling in kindergarten. Physical exam also reveals the finding shown in figure A. Which of the following is the most likely cause of this patient's multiple fractures?
- A. Decreased collagen hydroxylation
- B. Non-accidental trauma
- C. Abnormal collagen production (Correct Answer)
- D. Mutation in neurofibromin
- E. Increased adenylyl cyclase activity
Mutation types and consequences Explanation: ***Abnormal collagen production***
- This patient presents with **recurrent fractures** from minor trauma and **blue sclerae**, which are classic features of **osteogenesis imperfecta (OI)**.
- OI is caused by **genetic defects in type I collagen synthesis**, leading to fragile bones and thin sclerae that allow the underlying choroid to show through.
*Decreased collagen hydroxylation*
- This refers to a defect in post-translational modification of collagen, a core issue in **scurvy** (Vitamin C deficiency).
- Scurvy is characterized by **bleeding gums, petechiae, and impaired wound healing**, not recurrent fractures, and is not associated with blue sclerae.
*Non-accidental trauma*
- While recurrent fractures raise suspicion for **child abuse**, the presence of an underlying genetic condition like **osteogenesis imperfecta** (indicated by blue sclerae and easy fracturability) must be ruled out.
- The combination of **blue sclerae** and multiple fractures points strongly towards a genetic disorder, making child abuse less likely as the primary cause.
*Mutation in neurofibromin*
- A mutation in **neurofibromin** is characteristic of **Neurofibromatosis Type 1 (NF1)**.
- NF1 is associated with **café-au-lait spots, neurofibromas, Lisch nodules, and optic nerve gliomas**, but not blue sclerae or repeated fractures as the primary manifestation.
*Increased adenylyl cyclase activity*
- Increased adenylyl cyclase activity is seen in conditions like **McCune-Albright syndrome**, which involves somatic mutations in the **GNAS gene**.
- While McCune-Albright can cause **polyostotic fibrous dysplasia** (leading to fractures), **café-au-lait spots**, and **precocious puberty**, it is not associated with blue sclerae.
Mutation types and consequences US Medical PG Question 8: A baby is delivered at 39 weeks without complications. Upon delivery, there are obvious craniofacial abnormalities, including micrognathia, cleft lip, and cleft palate. On further inspection, downward slanting eyes and malformed ears are seen. The child has an APGAR score of 9 and 9 at 1 and 5 minutes respectively. There are no signs of cyanosis or evidence of a heart murmur. Which of the following is the most likely underlying cause of this patient’s presentation at birth?
- A. Microdeletion at chromosome 22q11.2
- B. Mutation in the TCOF1 gene (Correct Answer)
- C. Retinoic acid use during gestation
- D. Mutation of the SOX9 gene
- E. Trisomy 18
Mutation types and consequences Explanation: ***Mutation in the TCOF1 gene***
- This clinical presentation, characterized by craniofacial abnormalities such as **micrognathia**, **cleft lip/palate**, **downward-slanting palpebral fissures**, and **malformed ears**, is highly consistent with **Treacher Collins syndrome**.
- **Treacher Collins syndrome** is an autosomal dominant disorder usually caused by a **mutation in the TCOF1 gene**, which affects cranial neural crest cell development.
*Microdeletion at chromosome 22q11.2*
- This describes **DiGeorge syndrome** (also known as 22q11.2 deletion syndrome), which typically presents with **cardiac defects** (e.g., tetralogy of Fallot), **abnormal facies** (e.g., short palpebral fissures, bulbous nose), **thymic hypoplasia** (T-cell immunodeficiency), **cleft palate**, and **hypocalcemia**.
- While cleft palate is present, the absence of cardiac or immunodeficiency signs makes Treacher Collins syndrome a more likely fit given the specific constellation of craniofacial findings.
*Retinoic acid use during gestation*
- **Retinoic acid embryopathy** (isotretinoin teratogenicity) can cause a range of birth defects, including **craniofacial dysmorphism** (e.g., microtia, micrognathia), **cardiac malformations**, and **central nervous system abnormalities** (e.g., hydrocephalus).
- While some features overlap, the specific pattern of severe craniofacial abnormalities without mention of CNS or cardiac issues makes Treacher Collins syndrome a stronger diagnosis.
*Mutation of the SOX9 gene*
- A **mutation in the SOX9 gene** is associated with **Campomelic Dysplasia**, a severe skeletal dysplasia characterized by **bowing of long bones**, short stature, and **sex reversal** in XY individuals.
- Although it can present with some facial anomalies (e.g., flat face, micrognathia), the absence of skeletal bowing and the specific combination of craniofacial defects make another diagnosis more likely.
*Trisomy 18*
- **Trisomy 18** (Edwards syndrome) typically presents with severe **growth retardation**, **developmental delay**, **micrognathia**, **rocker-bottom feet**, **clenched hands with overlapping fingers**, and often serious **cardiac defects**.
- While micrognathia is present, the full spectrum of features for Trisomy 18 is not described, and the specific craniofacial abnormalities strongly point away from this diagnosis.
Mutation types and consequences US Medical PG Question 9: A 24-year-old man comes to the physician because his vision has worsened rapidly over the last 2 months. His maternal uncle lost his vision suddenly over a period of 3 months at 26 years of age. The patient's wife and 1-year-old son have normal vision. Funduscopic examination of the patient shows bilateral circumpapillary telangiectasia. Genetic testing shows a missense mutation in one of the genes of the electron transport chain complexes. The probability that this patient's son will be affected by the same disease is closest to which of the following?
- A. 33%
- B. 100%
- C. 0% (Correct Answer)
- D. 25%
- E. 50%
Mutation types and consequences Explanation: ***0%***
- This condition, **Leber's Hereditary Optic Neuropathy (LHON)**, is caused by a mutation in **mitochondrial DNA**.
- **Mitochondrial DNA** is exclusively inherited from the mother, meaning the father cannot pass it on to his children.
*33%*
- This percentage does not align with any known pattern of Mendelian inheritance or mitochondrial inheritance.
- It would be too low for a dominant mitochondrial disorder and too high for a recessive one if the mother were a carrier.
*100%*
- While all children of an affected mother would inherit the disease, the patient is a male, and mitochondria are inherited maternally.
- Therefore, the father cannot pass on his **mitochondrial DNA** to his son.
*25%*
- This percentage is typically associated with **autosomal recessive inheritance**, where both parents are carriers.
- LHON follows a **mitochondrial inheritance pattern**, which is distinct from autosomal inheritance.
*50%*
- This percentage is characteristic of **autosomal dominant inheritance** or X-linked recessive inheritance where the mother is a carrier.
- Since this is a **mitochondrial disorder**, the father's genes are not involved in transmission to his son.
Mutation types and consequences US Medical PG Question 10: An 8-month-old infant is brought to the physician by his mother because of a 1-month history of progressive listlessness. His mother says, "He used to crawl around, but now he can't even keep himself upright. He seems so weak!" Pregnancy and delivery were uncomplicated. Examination shows hypotonia and an increased startle response. Genetic analysis show insertion of four bases (TATC) into exon 11. Further evaluation shows decreased activity of hexosaminidase A. Which of the following mutations best explains these findings?
- A. Missense
- B. Nonsense
- C. Splice site
- D. Silent
- E. Frameshift (Correct Answer)
Mutation types and consequences Explanation: ***Frameshift***
- An insertion of four bases (TATC) is not a multiple of three, which will alter the **reading frame** of the codons downstream from the insertion.
- This typically results in a completely different protein sequence and often an early stop codon, leading to a **non-functional or truncated protein**, consistent with the severe symptoms and enzyme deficiency described.
*Missense*
- A missense mutation involves a **single nucleotide substitution** that results in a codon coding for a different amino acid.
- It does not involve an insertion of four bases and would not typically cause such a dramatic shift in protein structure as seen with a frameshift.
*Nonsense*
- A nonsense mutation is a **single nucleotide substitution** that results in a premature stop codon, leading to a truncated protein.
- While it can lead to a non-functional protein, the described insertion of four bases is not a single nucleotide change and would not directly result in a nonsense mutation unless the frameshift coincidentally created one.
*Splice site*
- A splice site mutation occurs at the **exon-intron boundaries** and affects the proper removal of introns during mRNA processing.
- While it can lead to abnormal proteins, the given mutation is an **insertion within an exon**, not at a splice site.
*Silent*
- A silent mutation is a **single nucleotide change** that does not alter the amino acid sequence of the protein due to the redundancy of the genetic code.
- This mutation involves an insertion of four bases and would drastically change the protein sequence, making a silent mutation impossible in this scenario.
More Mutation types and consequences US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.