TCA cycle reactions and regulation US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for TCA cycle reactions and regulation. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
TCA cycle reactions and regulation US Medical PG Question 1: An investigator is studying severely ill patients who experience hypoglycemia and ketonuria during times of fasting. The investigator determines that during these episodes, amino acids liberated from muscle proteins are metabolized to serve as substrates for gluconeogenesis. Nitrogen from this process is transported to the liver primarily in the form of which of the following molecules?
- A. Glutamate
- B. α-ketoglutarate
- C. Alanine (Correct Answer)
- D. Arginine
- E. Pyruvate
TCA cycle reactions and regulation Explanation: ***Alanine***
- During prolonged fasting, **muscle proteins are catabolized** to provide amino acids for gluconeogenesis in the liver.
- **Alanine** is the primary amino acid released from muscle into the bloodstream to transport nitrogen to the liver through the **glucose-alanine cycle (Cahill cycle)**.
- In this cycle, pyruvate in muscle accepts an amino group from glutamate to form alanine, which is then transported to the liver, where it is deaminated back to pyruvate (for gluconeogenesis) and ammonia (for the urea cycle).
- **Glutamine** also serves as an important nitrogen transporter, particularly to the kidneys and intestines.
*Glutamate*
- **Glutamate** is an important amino acid in nitrogen metabolism within tissues, but it is not the primary form in which nitrogen is transported from muscle to the liver in significant quantities.
- While glutamate participates in transamination reactions within muscle, its efflux from muscle into the blood is less prominent than alanine for inter-organ nitrogen transport.
*α-ketoglutarate*
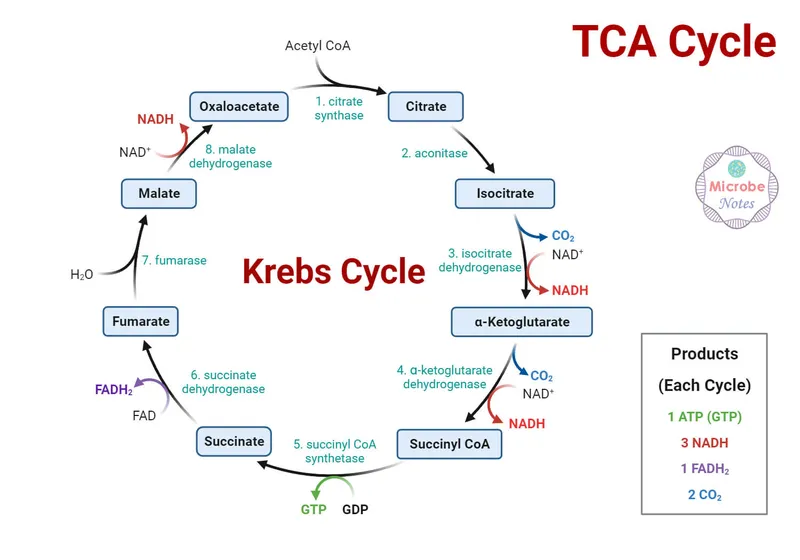
- **α-ketoglutarate** is a key intermediate in the **Krebs cycle** and accepts an amino group to form glutamate.
- It is an alpha-keto acid, not an amino acid, and therefore does not directly transport nitrogen in the form of an amino group to the liver via the bloodstream.
*Arginine*
- **Arginine** is primarily involved in the **urea cycle** within the liver, where it helps in the detoxification of ammonia, but it is not a major transporter of nitrogen from peripheral tissues to the liver for gluconeogenesis.
- Its role is mainly within the liver for urea synthesis, not for inter-organ nitrogen transport in this context.
*Pyruvate*
- **Pyruvate** is a keto acid that can be converted to alanine via transamination.
- While pyruvate is a precursor to alanine and a substrate for gluconeogenesis, it transports carbon skeletons and not nitrogen itself; **alanine is the actual nitrogen carrier** in this cycle.
TCA cycle reactions and regulation US Medical PG Question 2: An investigator is studying a hereditary defect in the mitochondrial enzyme succinyl-CoA synthetase. In addition to succinate, the reaction catalyzed by this enzyme produces a molecule that is utilized as an energy source for protein translation. This molecule is also required for which of the following conversion reactions?
- A. Oxaloacetate to phosphoenolpyruvate (Correct Answer)
- B. Pyruvate to acetyl-CoA
- C. Acetaldehyde to acetate
- D. Glucose-6-phosphate to 6-phosphogluconolactone
- E. Fructose-6-phosphate to fructose-1,6-bisphosphate
TCA cycle reactions and regulation Explanation: ***Oxaloacetate to phosphoenolpyruvate***
- The reaction catalyzed by **succinyl-CoA synthetase** (also known as succinate thiokinase) produces **GTP** (guanosine triphosphate) from GDP and Pi, in addition to succinate.
- **GTP** is required for the conversion of **oxaloacetate** to **phosphoenolpyruvate** in gluconeogenesis, catalyzed by **PEP carboxykinase**.
*Pyruvate to acetyl-CoA*
- This reaction is catalyzed by the **pyruvate dehydrogenase complex** and produces NADH, not GTP.
- It is an irreversible step linking glycolysis to the citric acid cycle.
*Acetaldehyde to acetate*
- This reaction is catalyzed by **aldehyde dehydrogenase** and uses **NAD+** as a cofactor, producing NADH.
- It is involved in alcohol metabolism.
*Glucose-6-phosphate to 6-phosphogluconolactone*
- This is the first committed step of the **pentose phosphate pathway**, catalyzed by **glucose-6-phosphate dehydrogenase**.
- It uses **NADP+** as a cofactor, producing NADPH.
*Fructose-6-phosphate to fructose-1,6-bisphosphate*
- This reaction is a key regulatory step in **glycolysis**, catalyzed by **phosphofructokinase-1 (PFK-1)**.
- It consumes **ATP**, rather than producing GTP or utilizing it as a cofactor in the context of this question.
TCA cycle reactions and regulation US Medical PG Question 3: After being warned by the locals not to consume the freshwater, a group of American backpackers set off on a week-long hike into a region of the Ecuadorean Amazon forest known for large gold mines. The group of hikers stopped near a small stream and used the water they filtered from the stream to make dinner. Within the next half hour, the hikers began to experience headaches, vertigo, visual disturbances, confusion, tachycardia, and altered levels of consciousness. Which of the following enzymes was most likely inhibited in this group of hikers?
- A. NADH dehydrogenase
- B. ATP synthase
- C. Cytochrome c oxidase (Correct Answer)
- D. Cytochrome bc1 complex
- E. Succinate dehydrogenase
TCA cycle reactions and regulation Explanation: ***Cytochrome c oxidase***
- The symptoms described (headaches, vertigo, visual disturbances, confusion, tachycardia, altered consciousness occurring within 30 minutes) are characteristic of **acute cyanide poisoning**.
- **Cyanide** is commonly found in water near **gold mining operations**, where it is used in the gold extraction process and can contaminate local water sources.
- **Cyanide** is a potent inhibitor of **cytochrome c oxidase** (Complex IV) in the electron transport chain, binding to the heme iron (Fe³⁺) and preventing oxygen utilization, leading to **histotoxic hypoxia**.
- This results in cellular energy failure, particularly affecting high-energy-demand organs like the brain and heart, explaining the acute neurological and cardiovascular symptoms.
*NADH dehydrogenase*
- While NADH dehydrogenase (Complex I) is a component of the electron transport chain, it is not the primary target of **cyanide poisoning**.
- Inhibitors of Complex I include rotenone and barbiturates, which cause different clinical presentations and do not produce the rapid onset of symptoms seen with cyanide.
*ATP synthase*
- **ATP synthase** (Complex V) synthesizes ATP using the proton gradient, but it is not directly inhibited by **cyanide**.
- Inhibitors of ATP synthase, such as oligomycin, prevent ATP synthesis by blocking the enzyme directly, whereas cyanide acts upstream at Complex IV.
*Cytochrome bc1 complex*
- The **cytochrome bc1 complex** (Complex III) is involved in electron transfer and proton pumping, but it is not the primary enzyme inhibited by **cyanide**.
- Inhibitors of Complex III include antimycin A, which would disrupt the electron transport chain but do not cause the characteristic rapid-onset symptoms of cyanide poisoning.
*Succinate dehydrogenase*
- **Succinate dehydrogenase** (Complex II) participates in both the citric acid cycle and the electron transport chain, but it is not targeted by **cyanide**.
- Inhibitors of Complex II, such as malonate, competitively block succinate oxidation but do not produce the acute systemic toxicity characteristic of cyanide poisoning.
TCA cycle reactions and regulation US Medical PG Question 4: An investigator is studying biomolecular mechanisms in human cells. A radioactive isotope that is unable to cross into organelles is introduced into a sample of cells. The cells are then fragmented via centrifugation and the isotope-containing components are isolated. Which of the following reactions is most likely to be present in this cell component?
- A. Glucose-6-phosphate to glucose
- B. Isocitrate to α-ketoglutarate
- C. Carbamoyl phosphate to citrulline
- D. Fatty acyl-CoA to acetyl-CoA
- E. Glucose-6-phosphate to 6-phosphogluconolactone (Correct Answer)
TCA cycle reactions and regulation Explanation: ***Glucose-6-phosphate to 6-phosphogluconolactone***
- This reaction is the first step of the **pentose phosphate pathway (PPP)**, which occurs in the **cytosol**.
- Since the isotope cannot cross into organelles and is found in the cytosolic fraction, this pathway is a likely candidate.
*Glucose-6-phosphate to glucose*
- This reaction describes the dephosphorylation of **glucose-6-phosphate** to **glucose**, catalyzed by **glucose-6-phosphatase**.
- While important for glucose release, this enzyme is primarily located in the **endoplasmic reticulum** of the liver and kidneys, an organelle.
*Isocitrate to α-ketoglutarate*
- This is a step in the **Krebs cycle (citric acid cycle)**, which takes place in the **mitochondrial matrix**.
- The isotope would not be found in this compartmentalized reaction because it cannot enter organelles.
*Carbamoyl phosphate to citrulline*
- This reaction is part of the **urea cycle**, which has steps occurring in both the **mitochondrial matrix** and the cytosol. The initial step, forming carbamoyl phosphate, is mitochondrial.
- The isotope, being unable to cross into organelles, would not readily participate in the mitochondrial portion of this pathway.
*Fatty acyl-CoA to acetyl-CoA*
- This reaction represents **beta-oxidation of fatty acids**, a process that primarily occurs in the **mitochondria** and peroxisomes.
- As the isotope is excluded from organelles, it would not be involved in these reactions.
TCA cycle reactions and regulation US Medical PG Question 5: A 22-year-old medical student decides to fast for 24 hours after reading about the possible health benefits of fasting. She read that blood glucose levels are maintained by metabolic processes such as hepatic glycogenolysis and hepatic gluconeogenesis during the initial 3 days of fasting. During the day, she did not suffer from the symptoms of hypoglycemia. Which of the following signaling molecules most likely stimulated the reaction which maintained her blood glucose after all her stored glucose was broken down and used up?
- A. Adenosine diphosphate
- B. Acetyl CoA (Correct Answer)
- C. Acetate
- D. Citrate
- E. Adenosine monophosphate
TCA cycle reactions and regulation Explanation: ***Acetyl CoA***
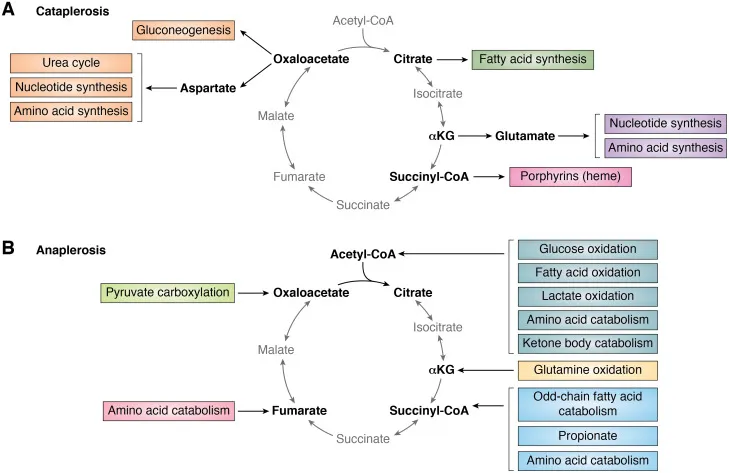
- **Acetyl CoA** is the key **allosteric activator of pyruvate carboxylase**, the first committed enzyme of gluconeogenesis that converts pyruvate to oxaloacetate.
- During prolonged fasting after glycogen stores are depleted, the body shifts to **fatty acid oxidation** (β-oxidation), which produces large amounts of **Acetyl CoA**.
- High **Acetyl CoA** levels signal that fat is being oxidized for energy, and simultaneously **activate gluconeogenesis** to maintain blood glucose for glucose-dependent tissues (brain, RBCs).
- This is the primary signaling mechanism that directly stimulates the gluconeogenic pathway after glycogen is exhausted.
*Adenosine monophosphate (AMP)*
- **AMP** levels rise during energy depletion and activate **AMP-activated protein kinase (AMPK)**.
- However, AMPK **inhibits gluconeogenesis** (not stimulates it) because gluconeogenesis is an **ATP-consuming** anabolic process (requires 6 ATP per glucose).
- AMPK promotes ATP-generating catabolic processes like fatty acid oxidation, but suppresses ATP-consuming processes like gluconeogenesis and fatty acid synthesis.
*Adenosine diphosphate (ADP)*
- **ADP** accumulates when ATP is hydrolyzed and signals moderate energy deficit.
- ADP is primarily a substrate for ATP regeneration via oxidative phosphorylation and does not directly regulate gluconeogenesis.
- Its role in metabolic regulation is less specific than allosteric activators like Acetyl CoA.
*Acetate*
- **Acetate** can be converted to Acetyl CoA but is not a direct signaling molecule for gluconeogenesis.
- It is a minor metabolite that may be produced in specific conditions (e.g., alcohol metabolism, ketoacidosis) but does not play a primary role in fasting-induced glucose homeostasis.
*Citrate*
- **Citrate** is a Krebs cycle intermediate that inhibits **phosphofructokinase-1 (PFK-1)** in glycolysis, thus reducing glucose breakdown.
- While citrate inhibition of glycolysis indirectly favors gluconeogenesis by preventing futile cycling, citrate does not **directly activate** gluconeogenic enzymes.
- Citrate primarily signals energy sufficiency and promotes fatty acid synthesis in the fed state, not fasting gluconeogenesis.
TCA cycle reactions and regulation US Medical PG Question 6: A 5-year-old boy is brought to the physician’s office with complaints of being tired constantly, which has limited his ability to walk or play with his friends. Physical examination in the physician’s office is normal. Further testing reveals that the patient has a genetic mutation in an enzyme and muscle biopsy shows high levels of alpha-ketoglutarate and low levels of succinyl-CoA as compared to normal. The enzyme that is most likely deficient in this patient requires which of the following as a cofactor?
- A. Vitamin B6
- B. NADH
- C. Carbon dioxide
- D. ATP
- E. Vitamin B1 (Correct Answer)
TCA cycle reactions and regulation Explanation: ***Vitamin B1***
- The patient's symptoms of fatigue and exercise intolerance, along with high levels of **alpha-ketoglutarate** and low levels of **succinyl-CoA**, indicate a defect in the **alpha-ketoglutarate dehydrogenase complex**.
- This enzyme complex, crucial for the **Krebs cycle**, requires **thiamine pyrophosphate (TPP)**, a derivative of **Vitamin B1**, as a vital cofactor.
*Vitamin B6*
- **Vitamin B6 (pyridoxine)** is a cofactor for enzymes involved in amino acid metabolism, such as **transaminases** and **decarboxylases**, but not specifically for alpha-ketoglutarate dehydrogenase.
- A deficiency in Vitamin B6 would lead to different metabolic profiles, not the specific accumulation of alpha-ketoglutarate.
*NADH*
- **NADH** is a product of several enzymatic reactions within the Krebs cycle, including the one catalyzed by alpha-ketoglutarate dehydrogenase, rather than a cofactor for this specific enzyme.
- While essential for the electron transport chain, NADH's role is as an electron carrier, not a direct cofactor for the alpha-ketoglutarate dehydrogenase complex's catalytic activity.
*Carbon dioxide*
- **Carbon dioxide** is often a product of decarboxylation reactions within the Krebs cycle (e.g., isocitrate dehydrogenase and alpha-ketoglutarate dehydrogenase), but it does not serve as a cofactor.
- Its presence or absence as a cofactor would not directly explain the enzymatic deficiency observed in this patient.
*ATP*
- **ATP** (adenosine triphosphate) is the primary energy currency of the cell, consumed or produced by many metabolic pathways, but it is not a direct cofactor for the alpha-ketoglutarate dehydrogenase complex.
- While energy is needed for many cellular processes, a direct ATP deficiency would manifest differently and would not specifically cause a buildup of alpha-ketoglutarate.
TCA cycle reactions and regulation US Medical PG Question 7: During normal respiration in the lungs, oxygen is absorbed into the bloodstream and carbon dioxide is released. The oxygen is used in cells as the final electron acceptor during oxidative phosphorylation, and carbon dioxide is generated during each turn of the tricarboxylic citric acid cycle (TCA). Which of the following steps in the TCA cycle represents the first decarboxylation reaction that generates carbon dioxide?
- A. Isocitrate to alpha ketoglutarate (Correct Answer)
- B. Fumarate to Malate
- C. Citrate to isocitrate
- D. Malate to oxaloacetate
- E. Alpha-ketoglutarate to Succinyl-CoA
TCA cycle reactions and regulation Explanation: ***Isocitrate to alpha ketoglutarate***
- This is the **first decarboxylation reaction** in the TCA cycle, catalyzed by **isocitrate dehydrogenase**.
- During this reaction, **isocitrate** is oxidized and a molecule of **carbon dioxide** is released, along with the reduction of NAD+ to NADH.
- This is one of the three irreversible steps in the TCA cycle and a key regulatory point.
*Fumarate to Malate*
- This step involves the **hydration** of **fumarate** to **malate** by the enzyme **fumarase**.
- There is no release of carbon dioxide in this reaction; it's a simple addition of water.
*Citrate to isocitrate*
- This is an **isomerization** reaction, catalyzed by **aconitase**, where **citrate** is rearranged into its isomer, **isocitrate**.
- This step does not involve the removal of carbon atoms or the production of carbon dioxide.
*Malate to oxaloacetate*
- In this step, **malate** is oxidized to **oxaloacetate** by **malate dehydrogenase**, which produces NADH.
- This is an **oxidation** reaction, not a decarboxylation reaction, and no carbon dioxide is released.
*Alpha-ketoglutarate to Succinyl-CoA*
- This is the **second decarboxylation** step in the TCA cycle, catalyzed by the **alpha-ketoglutarate dehydrogenase complex**.
- While this step also produces carbon dioxide and reduces NAD+ to NADH, it occurs after the isocitrate to alpha-ketoglutarate step, making it the second rather than the first decarboxylation reaction.
TCA cycle reactions and regulation US Medical PG Question 8: A 26-year-old man comes to the physician for evaluation of fatigue, facial rash, hair loss, and tingling of his hands and feet. He has followed a vegetarian diet for the past 3 years and has eaten 8 raw egg whites daily for the past year in preparation for a bodybuilding competition. Physical examination shows conjunctival injections and a scaly, erythematous rash around the eyes and mouth. Laboratory studies show decreased activity of propionyl-coenzyme A carboxylase in peripheral blood lymphocytes. Which of the following substances is most likely to be decreased in this patient?
- A. Methylmalonyl-CoA (Correct Answer)
- B. Cystathionine
- C. Lactate
- D. Adenine
- E. Ribulose-5-phosphate
TCA cycle reactions and regulation Explanation: ***Methylmalonyl-CoA***
- This patient has classic **biotin deficiency** due to consumption of raw egg whites. **Avidin** in raw egg whites binds biotin and prevents its absorption, leading to symptoms of dermatitis, alopecia, conjunctivitis, and neurological manifestations.
- Biotin is an essential cofactor for several carboxylase enzymes, including **propionyl-CoA carboxylase**, which catalyzes the conversion of **propionyl-CoA → methylmalonyl-CoA**.
- With **decreased propionyl-CoA carboxylase activity** (as stated in the question), the enzyme cannot efficiently convert its substrate to product. This results in **decreased formation of the product, methylmalonyl-CoA**.
- While propionyl-CoA (the substrate) would accumulate, methylmalonyl-CoA (the product) would be **decreased** due to impaired enzymatic conversion.
*Cystathionine*
- Cystathionine is an intermediate in the **transsulfuration pathway** (homocysteine → cysteine), which requires **vitamin B6** as a cofactor, not biotin.
- Its levels would not be directly affected by biotin deficiency or decreased propionyl-CoA carboxylase activity.
*Lactate*
- Lactate levels are elevated in conditions involving **anaerobic metabolism** or impaired mitochondrial function.
- Biotin deficiency can affect pyruvate carboxylase (another biotin-dependent enzyme), but this would not specifically decrease lactate levels. If anything, impaired pyruvate carboxylase might increase lactate by limiting pyruvate's entry into gluconeogenesis.
*Adenine*
- Adenine is a purine nucleobase involved in nucleotide synthesis and salvage pathways.
- Its metabolism is unrelated to biotin-dependent carboxylases and would not be affected in this patient.
*Ribulose-5-phosphate*
- Ribulose-5-phosphate is an intermediate in the **pentose phosphate pathway**, which generates NADPH and ribose-5-phosphate for nucleotide synthesis.
- This pathway is independent of biotin-dependent enzymes and would not be directly affected by propionyl-CoA carboxylase deficiency.
TCA cycle reactions and regulation US Medical PG Question 9: A 45-year-old man is brought to the emergency department by ambulance after vomiting blood. The patient reports that he only ate a small snack the morning before and had not eaten anything for over 24 hours. At the hospital, the patient is stabilized. He is admitted to a surgical floor and placed on NPO with a nasogastric tube set to intermittent suction. He has been previously diagnosed with liver cirrhosis. An esophagogastroduodenoscopy (EGD) has been planned for the next afternoon. At the time of endoscopy, some pathways were generating glucose to maintain serum glucose levels. Which of the following enzymes catalyzes the irreversible biochemical reaction of this process?
- A. Glucose-6-phosphate dehydrogenase
- B. Glycogen phosphorylase
- C. Enolase
- D. Glyceraldehyde-3-phosphate dehydrogenase
- E. Fructose-1,6-bisphosphatase (Correct Answer)
TCA cycle reactions and regulation Explanation: ***Fructose-1,6-bisphosphatase***
- The scenario describes a patient in a fasting state for over 24 hours, during which **gluconeogenesis** is crucial for maintaining blood glucose levels.
- **Fructose-1,6-bisphosphatase** is one of the key regulatory enzymes in gluconeogenesis, catalyzing an **irreversible reaction** that bypasses the phosphofructokinase-1 step of glycolysis.
*Glucose-6-phosphate dehydrogenase*
- This enzyme is involved in the **pentose phosphate pathway**, which generates NADPH and precursors for nucleotide synthesis.
- It does not directly participate in gluconeogenesis to produce glucose from non-carbohydrate sources.
*Glycogen phosphorylase*
- This enzyme is involved in **glycogenolysis**, the breakdown of glycogen into glucose-1-phosphate.
- While it releases glucose, the body's glycogen stores would likely be depleted after over 24 hours of fasting, making gluconeogenesis the primary pathway for glucose production.
*Enolase*
- Enolase is an enzyme in the glycolytic pathway, catalyzing the reversible conversion of 2-phosphoglycerate to phosphoenolpyruvate.
- It is not an enzyme of gluconeogenesis, nor does it catalyze an irreversible step in the glucose production process during fasting.
*Glyceraldehyde-3-phosphate dehydrogenase*
- This enzyme is also part of glycolysis, catalyzing the reversible oxidation and phosphorylation of glyceraldehyde-3-phosphate to 1,3-bisphosphoglycerate.
- Like enolase, it is not an irreversible enzyme in gluconeogenesis that would be generating glucose under fasting conditions.
TCA cycle reactions and regulation US Medical PG Question 10: A 2-year-old boy from a rural community is brought to the pediatrician after his parents noticed a white reflection in both of his eyes in recent pictures. Physical examination reveals bilateral leukocoria, nystagmus, and inflammation. When asked about family history of malignancy, the father of the child reports losing a brother to an eye tumor when they were children. With this in mind, which of the following processes are affected in this patient?
- A. Base excision repair
- B. Regulation of the G1-S transition (Correct Answer)
- C. DNA mismatch repair
- D. Stem cell self-renewal
- E. Nucleotide excision repair
TCA cycle reactions and regulation Explanation: ***Regulation of the G1-S transition***
- This patient's symptoms (bilateral **leukocoria**, **nystagmus**, family history of eye tumor) are characteristic of **retinoblastoma**, which is often caused by a mutation in the **RB1 gene**.
- The **RB1 gene** product (retinoblastoma protein) is a key **tumor suppressor** that regulates the G1-S cell cycle transition, and its dysfunction leads to uncontrolled cell proliferation.
*Base excision repair*
- This process is primarily involved in repairing damaged bases in DNA, often due to oxidation or alkylation.
- Defects in base excision repair are typically associated with conditions such as **MUTYH-associated polyposis**, not retinoblastoma.
*DNA mismatch repair*
- This system corrects errors that occur during DNA replication, such as incorrect base pairings or small insertions/deletions.
- Impairment of mismatch repair is a hallmark of **Lynch syndrome** (hereditary nonpolyposis colorectal cancer), which does not present with retinoblastoma.
*Stem cell self-renewal*
- While uncontrolled self-renewal can contribute to cancer, retinoblastoma is specifically linked to defects in the **RB1 gene**, which is a cell cycle regulator, not directly a primary regulator of stem cell self-renewal itself.
- Loss of G1-S checkpoint control is a more direct and proximal cause of the tumor formation in retinoblastoma.
*Nucleotide excision repair*
- This pathway is responsible for repairing bulkier DNA lesions, such as those caused by UV radiation.
- Deficiencies in nucleotide excision repair lead to diseases like **xeroderma pigmentosum**, characterized by extreme sensitivity to sunlight and increased skin cancer risk, which is unrelated to the presented case.
More TCA cycle reactions and regulation US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.