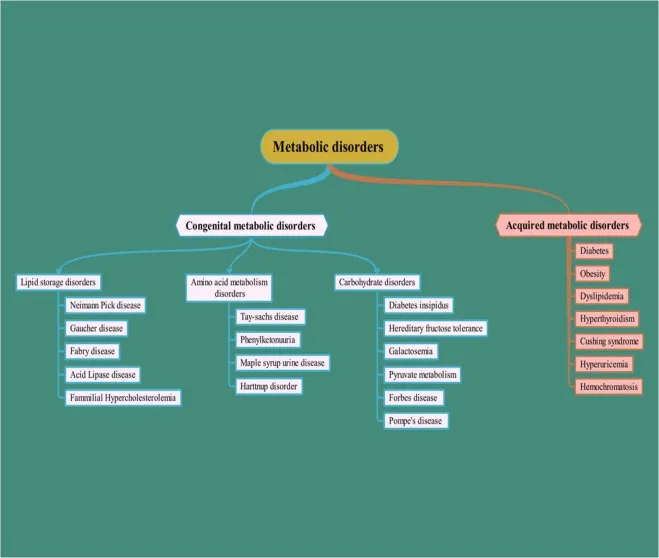
Metabolic disorders overview US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Metabolic disorders overview. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Metabolic disorders overview US Medical PG Question 1: A 6-month-old boy is brought to the emergency department by his mother because of recurrent vomiting and yellowing of his eyes. The mother says that he has been eating poorly since she started weaning him off of breast milk 5 days ago. At this time, mashed vegetables and fruits were added to his diet. Examination shows scleral jaundice and dry mucous membranes. The tip of the liver is palpable 4 cm below the right costal margin. His serum glucose concentration is 47 mg/dL, serum alanine aminotransferase is 55 U/L, and serum aspartate aminotransferase is 66 U/L. Which of the following enzymes is most likely deficient?
- A. Fructokinase
- B. Glucose-6-phosphatase
- C. Galactokinase
- D. Galactose-1 phosphate uridyltransferase
- E. Aldolase B (Correct Answer)
Metabolic disorders overview Explanation: ***Aldolase B***
- The symptoms, including **jaundice**, vomiting, **hepatomegaly**, and **hypoglycemia** following the introduction of solid foods (specifically fruits and vegetables containing **fructose**), are classic for **hereditary fructose intolerance**.
- **Aldolase B** is crucial for metabolizing fructose in the liver; its deficiency leads to the buildup of **fructose-1-phosphate**, which is toxic to hepatocytes and inhibits glucose production.
*Fructokinase*
- Fructokinase deficiency causes **essential fructosuria**, a benign condition characterized by fructose in the urine, but without the severe metabolic disturbances like hypoglycemia and liver damage seen in this patient.
- This condition does not typically present with the **jaundice**, vomiting, and liver enlargement found in the given case.
*Glucose-6-phosphatase*
- A deficiency in **glucose-6-phosphatase** causes **Type I glycogen storage disease (Von Gierke disease)**, which presents with severe hypoglycemia and hepatomegaly.
- However, it does not typically cause the **jaundice** or acute symptoms triggered by the introduction of solid foods containing fructose as described in this case.
*Galactokinase*
- Deficiency of galactokinase leads to **Type II galactosemia**, characterized primarily by **cataracts** and galactosemia, but typically without the profound liver damage, jaundice, or acute hypoglycemia seen here.
- The symptoms in this case are related to **fructose** intake, not galactose.
*Galactose-1 phosphate uridyltransferase*
- Deficiency in **galactose-1-phosphate uridyltransferase** causes **classic galactosemia**, which presents with **jaundice**, hepatosplenomegaly, vomiting, and cataracts, often triggered by lactose (galactose) intake.
- While it shares some symptoms with the patient's presentation, the trigger of symptoms upon introducing fruits and vegetables (high in fructose) points specifically to an issue with **fructose metabolism**, not galactose.
Metabolic disorders overview US Medical PG Question 2: A 2-year-old boy is brought to the emergency department by his mother 30 minutes after having a generalized tonic-clonic seizure. He was born at home and has not attended any well-child visits. He is not yet able to walk and does not use recognizable words. His paternal uncle has a severe intellectual disability and has been living in an assisted-living facility all of his life. The boy's urine phenylacetate level is markedly elevated. Which of the following amino acids is most likely nutritionally essential for this patient because of his underlying condition?
- A. Alanine
- B. Glutamate
- C. Phenylalanine
- D. Cysteine
- E. Tyrosine (Correct Answer)
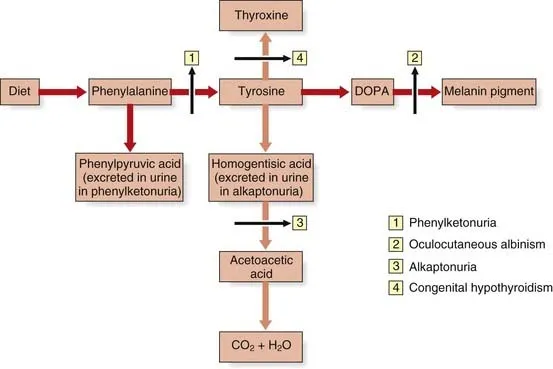
Metabolic disorders overview Explanation: ***Tyrosine***
- The patient's presentation with seizures, developmental delay, and elevated **phenylacetate (a phenylalanine metabolite)** strongly suggest **phenylketonuria (PKU)**.
- In PKU, the enzyme **phenylalanine hydroxylase (PAH)** is deficient, preventing the conversion of **phenylalanine** to **tyrosine**, making **tyrosine** a **nutritionally essential** amino acid.
*Alanine*
- **Alanine** is a **non-essential** amino acid synthesized from pyruvate and other amino acids, and its synthesis is not impaired in PKU.
- It plays a role in **gluconeogenesis** but is not directly related to the metabolic defect in PKU.
*Glutamate*
- **Glutamate** is a **non-essential** amino acid, crucial for neurotransmission and protein synthesis, and is not affected by PKU.
- It can be synthesized from various metabolic intermediates, and its status is not altered in patients with PKU.
*Phenylalanine*
- **Phenylalanine** is an **essential amino acid** that becomes **toxic** when accumulated due to PKU, making it necessary to restrict it in the diet.
- It is the precursor to **tyrosine**, but its inability to be metabolized is the core problem in PKU, not a nutritional essentiality related to the disease.
*Cysteine*
- **Cysteine** is a **conditionally essential** amino acid, often synthesized from methionine, and its synthesis is not directly impacted by PKU.
- While potentially essential in certain conditions, it is not the primary amino acid that becomes essential due to the specific enzymatic defect in PKU.
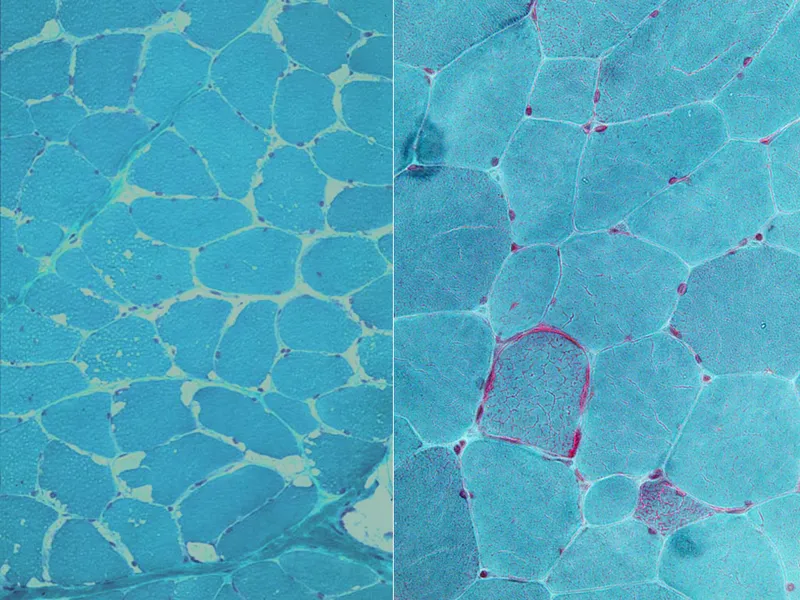
Metabolic disorders overview US Medical PG Question 3: A mother brings her 3-year-old daughter to the pediatrician because she is concerned about her development. She states that her daughter seemed to regress in her motor development. Furthermore, she states she has been having brief episodes of uncontrollable shaking, which has been very distressing to the family. During the subsequent work-up, a muscle biopsy is obtained which demonstrates red ragged fibers and a presumptive diagnosis of a genetic disease is made. The mother states that she has another 6-year-old son who does not seem to be affected or have any similar symptoms. What genetic term explains this phenomenon?
- A. Allelic heterogeneity
- B. Heteroplasmy (Correct Answer)
- C. Locus heterogeneity
- D. Phenotypic heterogeneity
- E. Genetic heterogeneity
Metabolic disorders overview Explanation: ***Heteroplasmy***
- **Heteroplasmy** refers to the presence of more than one type of mitochondrial DNA (mtDNA) within the same cell or individual. The varying proportions of mutated mtDNA can lead to a wide spectrum of disease severity, explaining why the daughter is severely affected while her brother is unaffected.
- The daughter's symptoms (developmental regression, seizures), combined with the muscle biopsy showing **red ragged fibers**, are characteristic of **mitochondrial disorders**, which are often maternally inherited and can manifest with variable expressivity due to heteroplasmy.
*Allelic heterogeneity*
- **Allelic heterogeneity** occurs when different mutations at the *same gene locus* can cause the same disease.
- This term does not explain the differential severity or presence of disease in siblings with a maternally inherited mitochondrial disorder, as it focuses on different mutations within a single gene rather than varying proportions of mutated mitochondria.
*Locus heterogeneity*
- **Locus heterogeneity** describes situations where mutations in *different genes* can cause the same disease phenotype.
- This concept is not applicable here because the clinical picture and red ragged fibers point towards a specific mitochondrial disorder, and the siblings would typically be expected to share the same genetic locus underlying their condition if it were present.
*Phenotypic heterogeneity*
- **Phenotypic heterogeneity** refers to different clinical manifestations or phenotypes resulting from mutations in the *same gene*.
- While there is varying severity of the disease (different phenotypes) between the siblings, this term doesn't specifically explain the underlying *genetic mechanism* of varying mitochondrial mutation loads, which is crucial for mitochondrial disorders.
*Genetic heterogeneity*
- **Genetic heterogeneity** is a broad term encompassing both allelic and locus heterogeneity, meaning that a single phenotype can be caused by mutations at different loci (locus heterogeneity) or by different mutations within the same gene (allelic heterogeneity).
- While mitochondrial disorders can exhibit genetic heterogeneity, this general term doesn't specifically address the mechanism of variable penetrance and expressivity seen in mitochondrial inheritance due to the varying proportions of mutated mtDNA within cells, which is uniquely explained by heteroplasmy.
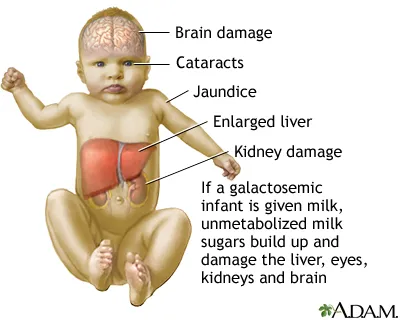
Metabolic disorders overview US Medical PG Question 4: A 3-week-old newborn is brought to the pediatrician by his mother. His mother is concerned about her son’s irritability and vomiting, particularly after breastfeeding him. The infant was born at 39 weeks via spontaneous vaginal delivery. His initial physical was benign. Today the newborn appears mildly jaundiced with palpable hepatomegaly, and his eyes appear cloudy, consistent with the development of cataracts. The newborn is also in the lower weight-age percentile. The physician considers a hereditary enzyme deficiency and orders blood work and a urinalysis to confirm his diagnosis. He recommends that milk and foods high in galactose and/or lactose be eliminated from the diet. Which of the following is the most likely deficient enzyme in this metabolic disorder?
- A. Aldose reductase
- B. Galactose-1-phosphate uridyl transferase (Correct Answer)
- C. UDP-galactose-4-epimerase
- D. Galactokinase
- E. Glucose-6-phosphate dehydrogenase
Metabolic disorders overview Explanation: ***Galactose-1-phosphate uridyl transferase***
- The constellation of symptoms including **vomiting**, **irritability**, **jaundice**, **hepatomegaly**, **cataracts**, and **failure to thrive** in a neonate, with improvement upon eliminating galactose/lactose from the diet, is highly characteristic of **classic galactosemia**.
- **Classic galactosemia** is caused by a deficiency in **galactose-1-phosphate uridyl transferase (GALT)**, leading to the accumulation of galactose-1-phosphate, which is toxic to various tissues.
*Aldose reductase*
- This enzyme converts galactose to **galactitol**, which can accumulate in the lens and cause **cataracts** in all forms of galactosemia if left untreated.
- However, isolated aldose reductase deficiency does not explain the full spectrum of severe systemic symptoms like hepatomegaly, jaundice, and failure to thrive observed in this neonate, which are indicative of classic galactosemia.
*UDP-galactose-4-epimerase*
- Deficiency in **UDP-galactose-4-epimerase (GALE)**, also known as epimerase deficiency galactosemia, has a wide range of severity.
- While it can present with similar symptoms to GALT deficiency, its severe form is rarer, and the classic, pronounced presentation described here is more commonly associated with GALT deficiency.
*Galactokinase*
- Deficiency in **galactokinase (GALK)** causes **Type II galactosemia**, which primarily manifests as **cataracts** due to galactitol accumulation.
- It typically does not present with the severe hepatic (jaundice, hepatomegaly) or systemic symptoms (vomiting, failure to thrive) seen in classic galactosemia.
*Glucose-6-phosphate dehydrogenase*
- **Glucose-6-phosphate dehydrogenase (G6PD) deficiency** primarily causes **hemolytic anemia** triggered by certain drugs, infections, or fava beans.
- It does not present with the specific constellation of symptoms related to galactose metabolism, such as cataracts, hepatomegaly, and vomiting upon milk ingestion, as described in this case.
Metabolic disorders overview US Medical PG Question 5: An 18-month-old boy of Ashkenazi-Jewish descent presents with loss of developmental milestones. On ocular exam, a cherry-red macular spot is observed. No hepatomegaly is observed on physical exam. Microscopic exam shows lysosomes with onion-skin appearance.
What is the most likely underlying biochemical abnormality?
- A. Accumulation of ceramide trihexoside
- B. Accumulation of glucocerebroside
- C. Accumulation of galactocerebroside
- D. Accumulation of sphingomyelin
- E. Accumulation of GM2 ganglioside (Correct Answer)
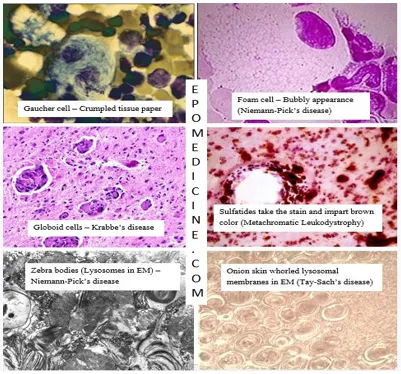
Metabolic disorders overview Explanation: ***Accumulation of GM2 ganglioside***
- This constellation of symptoms—**loss of developmental milestones**, **cherry-red macular spot**, absence of hepatomegaly, and **lysosomes with onion-skin appearance** in an individual of **Ashkenazi-Jewish descent**—is classic for **Tay-Sachs disease**.
- **Tay-Sachs disease** is caused by a deficiency of **hexosaminidase A**, leading to the accumulation of **GM2 ganglioside** in neuronal lysosomes.
*Accumulation of ceramide trihexoside*
- This refers to **Fabry disease**, which is an **X-linked disorder** presenting in adolescence or adulthood with acroparesthesias, angiokeratomas, and renal/cardiac complications.
- While it involves a lysosomal storage, its clinical presentation and the absence of a cherry-red spot differentiate it from the case described.
*Accumulation of glucocerebroside*
- This is characteristic of **Gaucher disease**, which is caused by a deficiency in **glucocerebrosidase**.
- Key features include **hepatosplenomegaly**, bone pain, and pancytopenia, which are not consistent with the patient's presentation.
*Accumulation of galactocerebroside*
- This describes **Krabbe disease**, a **globoid cell leukodystrophy** caused by a deficiency in galactocerebrosidase.
- Krabbe disease primarily affects the **myelin sheath** in the nervous system, leading to neurological degeneration but typically does not present with a cherry-red macular spot.
*Accumulation of sphingomyelin*
- This is the hallmark of **Niemann-Pick disease**, caused by **sphingomyelinase deficiency**.
- While Niemann-Pick disease also presents with a **cherry-red macular spot** and neurodegeneration, it is classically associated with **hepatosplenomegaly**, which is explicitly stated to be absent in this patient.
Metabolic disorders overview US Medical PG Question 6: An 8-month-old female infant from a first-degree consanguineous couple was brought to the physician because the mother noticed abnormalities in the growth of her child as well as the different lengths of her child's legs. The infant had gingival hyperplasia, restricted movement in both shoulders, a prominent, pointed forehead, and enophthalmos with a slight opacity in both corneas. A blood test revealed 10 fold higher than normal levels of the following enzymes: N-acetyl-ß-glucosaminidase, ß-glucuronidase, ß-hexosaminidase A, and alkaline phosphatase. Which of the following is most likely deficient in this patient?
- A. Lysosomal alpha-1,4-glucosidase
- B. Glucose-6-phosphate dehydrogenase
- C. N-acetyl-glucosamine-1-phosphotransferase (Correct Answer)
- D. Glucocerebrosidase
- E. Alpha-galactosidase A
Metabolic disorders overview Explanation: ***N-acetyl-glucosamine-1-phosphotransferase***
- The clinical presentation with **gingival hyperplasia**, **restricted joint movement**, **skeletal abnormalities** (growth abnormalities, leg length discrepancy, prominent forehead), and **corneal opacity** with elevated lysosomal enzymes (N-acetyl-ß-glucosaminidase, ß-glucuronidase, ß-hexosaminidase A) is highly characteristic of **I-cell disease** (mucolipidosis II).
- I-cell disease is caused by a deficiency in **N-acetyl-glucosamine-1-phosphotransferase**, an enzyme crucial for phosphorylating mannose residues on lysosomal enzymes, tagging them for delivery to lysosomes. Without this tag, lysosomal enzymes are secreted extracellularly, leading to their accumulation in the blood and their deficiency within lysosomes, causing the clinical features.
*Lysosomal alpha-1,4-glucosidase*
- Deficiency of **lysosomal alpha-1,4-glucosidase** causes **Pompe disease (glycogen storage disease type II)**, which is characterized by **cardiomegaly**, hypotonia, and liver involvement, but typically does not present with the skeletal dysplasias, gingival hyperplasia, or corneal clouding seen in this patient.
- While it is a lysosomal storage disorder, the specific clinical features and panel of elevated enzymes differ significantly from this case.
*Glucose-6-phosphate dehydrogenase*
- Deficiency of **glucose-6-phosphate dehydrogenase (G6PD)** causes **G6PD deficiency**, an X-linked disorder leading to **hemolytic anemia** in response to oxidative stress (e.g., fava beans, certain drugs, infections).
- It does not present with the systemic skeletal, connective tissue, and corneal abnormalities described, nor does it involve elevated lysosomal enzyme levels.
*Glucocerebrosidase*
- Deficiency of **glucocerebrosidase** causes **Gaucher disease**, which presents with **hepatosplenomegaly**, bone crises, pancytopenia, and sometimes neurological involvement.
- While it is a lysosomal storage disorder, the clinical features (e.g., absence of gingival hyperplasia, corneal opacity, or specific skeletal dysplasias like restricted joint movement) and the pattern of elevated enzymes do not match the patient's presentation.
*Alpha-galactosidase A*
- Deficiency of **alpha-galactosidase A** causes **Fabry disease**, an X-linked lysosomal storage disorder characterized by **neuropathic pain**, **angiokeratomas**, renal failure, and cardiac involvement.
- The clinical picture of Fabry disease does not include gingival hyperplasia, prominent skeletal abnormalities, or the specific pattern of elevated lysosomal enzymes observed in this patient.
Metabolic disorders overview US Medical PG Question 7: You are counseling a mother whose newborn has just screened positive for a deficit of phenylalanine hydroxylase enzyme. You inform her that her child will require dietary supplementation of which of the following?
- A. Aspartame
- B. Niacin
- C. Homogentisic Acid
- D. Tyrosine (Correct Answer)
- E. Leucine
Metabolic disorders overview Explanation: ***Tyrosine***
- A deficit of **phenylalanine hydroxylase** prevents the conversion of phenylalanine to tyrosine, making **tyrosine** an essential amino acid that must be supplemented.
- Dietary restriction of **phenylalanine** is also crucial to prevent the accumulation of toxic byproducts that can cause severe neurological damage.
*Aspartame*
- **Aspartame** is an artificial sweetener that contains **phenylalanine**, which would be harmful for a child with phenylalanine hydroxylase deficiency.
- Consumption of aspartame would increase the body's phenylalanine load, exacerbating the metabolic disorder.
*Niacin*
- **Niacin** (vitamin B3) is a vitamin and its supplementation is not related to the phenylalanine hydroxylase pathway or its deficiency.
- Deficiency of niacin is associated with **pellagra**, characterized by dermatitis, diarrhea, and dementia.
*Homogentisic Acid*
- **Homogentisic acid** is an intermediate in the metabolism of tyrosine, and its accumulation is characteristic of **alkaptonuria**, a different metabolic disorder.
- It is not a therapeutic supplement for phenylalanine hydroxylase deficiency.
*Leucine*
- **Leucine** is a branched-chain amino acid, and its metabolism is unrelated to phenylalanine hydroxylase deficiency.
- Supplemental leucine is not required in this condition and would not address the metabolic defect.
Metabolic disorders overview US Medical PG Question 8: A 2-day-old newborn boy is brought to the emergency department because of apnea, cyanosis, and seizures. He is severely hypoglycemic and does not improve with glucagon administration. His blood pressure is 100/62 mm Hg and heart rate is 75/min. Blood tests show high lactate levels. Physical examination is notable for hepatomegaly. Which of the following enzymes is most likely to be deficient in this baby?
- A. α-ketoacid dehydrogenase
- B. Phenylalanine hydroxylase
- C. Glucose-6-phosphatase (Correct Answer)
- D. Glucocerebrosidase
- E. Sphingomyelinase
Metabolic disorders overview Explanation: ***Correct: Glucose-6-phosphatase***
- The presentation of severe **hypoglycemia** not responsive to glucagon, coupled with **hepatomegaly** and **lactic acidosis** in a neonate, is highly suggestive of **Type I glycogen storage disease (von Gierke disease)**.
- Deficiency of **glucose-6-phosphatase** prevents the liver from releasing glucose into the bloodstream (the final step of both gluconeogenesis and glycogenolysis), leading to profound hypoglycemia.
- **Key diagnostic clue**: Lack of response to glucagon occurs because glucagon stimulates glycogenolysis, but without functional glucose-6-phosphatase, glucose-6-phosphate cannot be converted to free glucose for release.
- Accumulated glucose-6-phosphate shunts to glycolysis, producing **lactate** (lactic acidosis), and to glycogen synthesis, causing **hepatomegaly**.
*Incorrect: α-ketoacid dehydrogenase*
- Deficiency of **branched-chain α-ketoacid dehydrogenase** causes **maple syrup urine disease (MSUD)**, which presents with poor feeding, vomiting, lethargy, and a characteristic maple syrup odor in urine.
- While MSUD can cause neurological symptoms and seizures, **severe hypoglycemia unresponsive to glucagon** and **hepatomegaly** as primary features are not typical.
*Incorrect: Phenylalanine hydroxylase*
- Deficiency in **phenylalanine hydroxylase** causes **phenylketonuria (PKU)**, which is primarily characterized by intellectual disability, seizures (if untreated), and a musty odor, usually manifesting later in infancy.
- PKU does not present with acute neonatal hypoglycemia, lactic acidosis, or hepatomegaly.
*Incorrect: Glucocerebrosidase*
- Deficiency in **glucocerebrosidase** leads to **Gaucher disease**, a lysosomal storage disorder characterized by hepatosplenomegaly, bone crises, and neurological symptoms in severe infantile forms.
- While hepatomegaly may be present, Gaucher disease does not cause acute, severe neonatal hypoglycemia, lactic acidosis, or lack of response to glucagon.
*Incorrect: Sphingomyelinase*
- Deficiency in **sphingomyelinase** causes **Niemann-Pick disease**, another lysosomal storage disorder, which typically presents with hepatosplenomegaly, neurological deterioration, and "cherry-red spots" in the retina.
- This condition does not cause acute neonatal hypoglycemia, lactic acidosis, or glucagon unresponsiveness.
Metabolic disorders overview US Medical PG Question 9: A 7-month-old boy is brought to the pediatrician for a change in his behavior. The patient has been exclusively breastfeeding up until this point and has been meeting his developmental milestones. He is in the 90th percentile for weight and 89th percentile for height. Two weeks ago, his parents began introducing weaning foods including fruit purees and baby formula. This past week, the patient has been increasingly lethargic, vomiting, and has been refusing to eat. The patient's parents state that he had an episode this morning where he was not responsive and was moving his extremities abnormally followed by a period of somnolence. The patient's past medical history is notable for shoulder dystocia and poorly managed maternal diabetes during the pregnancy. His temperature is 99.5°F (37.5°C), blood pressure is 60/30 mmHg, pulse is 120/min, respirations are 17/min, and oxygen saturation is 98% on room air. On physical exam, you note a lethargic infant with a distinctive sweet, fruity smell to his breath. Which of the following is most likely deficient in this patient?
- A. Branched chain alpha-ketoacid dehydrogenase (Correct Answer)
- B. Galactose-1-phosphate uridyltransferase
- C. Aldolase B
- D. Glucose-6-phosphatase
- E. Ornithine transcarbamolase
Metabolic disorders overview Explanation: ***Branched chain alpha-ketoacid dehydrogenase***
- This patient's presentation is classic for **maple syrup urine disease (MSUD)**, caused by deficiency of branched chain alpha-ketoacid dehydrogenase complex.
- The **distinctive sweet, fruity smell to the breath** (and urine) is pathognomonic for MSUD, resulting from accumulation of branched chain amino acids (leucine, isoleucine, valine) and their ketoacid metabolites.
- Symptoms typically manifest upon introduction of **increased protein load** (baby formula), presenting with **lethargy, vomiting, poor feeding, seizures, and encephalopathy** due to neurotoxicity from elevated leucine and other metabolites.
- The timing (introduced weaning foods including formula) and clinical picture of acute metabolic crisis with characteristic odor make this the most likely diagnosis.
*Ornithine transcarbamylase*
- OTC deficiency causes **hyperammonemic crisis** with similar neurological symptoms (lethargy, vomiting, seizures) triggered by protein intake.
- However, hyperammonemia typically produces a **musty or ammonia-like odor**, NOT the sweet, fruity smell described in this case.
- While the clinical timing fits, the **characteristic breath odor is inconsistent** with urea cycle disorders.
*Galactose-1-phosphate uridyltransferase*
- Deficiency causes **classic galactosemia**, presenting with **vomiting, lethargy, jaundice, hepatomegaly, and cataracts** after lactose exposure (milk/formula).
- The **sweet, fruity breath odor is NOT characteristic** of galactosemia.
- While formula introduction could trigger symptoms, the specific odor and predominant neurological presentation point away from this diagnosis.
*Aldolase B*
- **Hereditary fructose intolerance** manifests upon fructose exposure (fruit purees) with **vomiting, hypoglycemia, jaundice, hepatomegaly, and renal dysfunction**.
- The patient did consume fruit purees, but the **sweet, fruity breath odor is NOT a feature** of fructose intolerance.
- The severe acute encephalopathy and characteristic odor make MSUD more likely.
*Glucose-6-phosphatase*
- **Von Gierke disease (Type I GSD)** presents with **severe fasting hypoglycemia, lactic acidosis, hepatomegaly, and hyperlipidemia**.
- The **sweet, fruity odor is NOT characteristic**, and symptoms are primarily related to fasting/glucose homeostasis rather than acute protein-induced metabolic crisis.
- The clinical picture does not fit a glycogen storage disorder.
Metabolic disorders overview US Medical PG Question 10: A 4-year-old boy is brought to the physician for a well-child examination. He started walking at 20 months of age. He can use a cup to drink but cannot use silverware. He speaks in 2-word sentences and can build a tower of 4 blocks. He can scribble but cannot draw a circle. He is above the 99th percentile for height and at the 15th percentile for weight. Vital signs are within normal limits. Examination shows bilateral inferior lens dislocation. His fingers are long and slender. He has a high-arched palate. The thumb and 5th finger overlap when he grips a wrist with the opposite hand. The skin over the neck can be extended and stretched easily. Which of the following is the most likely cause of these findings?
- A. Hypoxanthine-guanine-phosphoribosyl transferase deficiency
- B. Galactokinase deficiency
- C. Fibrillin 1 deficiency
- D. Cystathionine synthase deficiency (Correct Answer)
- E. Type V collagen deficiency
Metabolic disorders overview Explanation: ***Cystathionine synthase deficiency***
- The combination of **inferior lens dislocation**, **marfanoid habitus** (tall stature, long slender fingers, high-arched palate), **developmental delay** (late walking, speech delay), and **hyperelastic skin** is highly suggestive of **homocystinuria** due to cystathionine synthase deficiency.
- **Homocystinuria** is an autosomal recessive disorder causing accumulation of **homocysteine**, leading to multisystem involvement.
*Hypoxanthine-guanine-phosphoribosyl transferase deficiency*
- This deficiency causes **Lesch-Nyhan syndrome**, characterized by **gout, intellectual disability, choreoathetosis, and self-mutilation**.
- It does not present with lens dislocation or marfanoid features.
*Galactokinase deficiency*
- This is a rare form of **galactosemia** primarily causing **cataracts**.
- It does not explain the developmental delay, marfanoid features, or lens dislocation.
*Fibrillin 1 deficiency*
- This causes **Marfan syndrome**, which shares features like **tall stature, long slender fingers, high-arched palate, and lens dislocation**.
- However, in Marfan syndrome, lens dislocation is typically **superior**, while in this case, it is **inferior**, pointing towards homocystinuria.
*Type V collagen deficiency*
- This can be associated with **Ehlers-Danlos syndrome**, which features **hyperelastic skin** and joint hypermobility.
- However, it does not typically cause lens dislocation or the specific marfanoid habitus described, and developmental delay is not a primary feature.
More Metabolic disorders overview US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.