Integration of metabolic pathways US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Integration of metabolic pathways. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Integration of metabolic pathways US Medical PG Question 1: A scientist is trying to design a drug to modulate cellular metabolism in the treatment of obesity. Specifically, he is interested in understanding how fats are processed in adipocytes in response to different energy states. His target is a protein within these cells that catalyzes catabolism of an energy source. The products of this reaction are subsequently used in gluconeogenesis or β-oxidation. Which of the following is true of the most likely protein that is being studied by this scientist?
- A. It is stimulated by epinephrine (Correct Answer)
- B. It is inhibited by glucagon
- C. It is inhibited by acetylcholine
- D. It is inhibited by cortisol
- E. It is stimulated by insulin
Integration of metabolic pathways Explanation: ***It is stimulated by epinephrine***
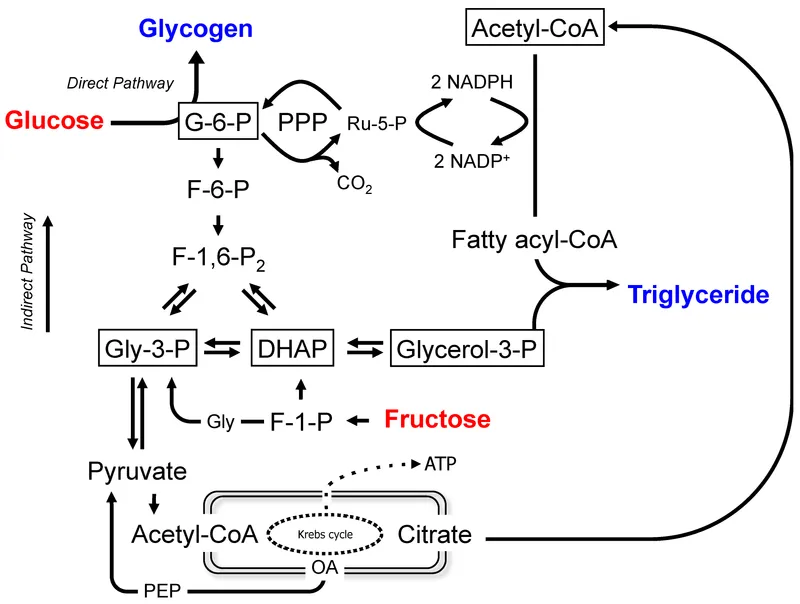
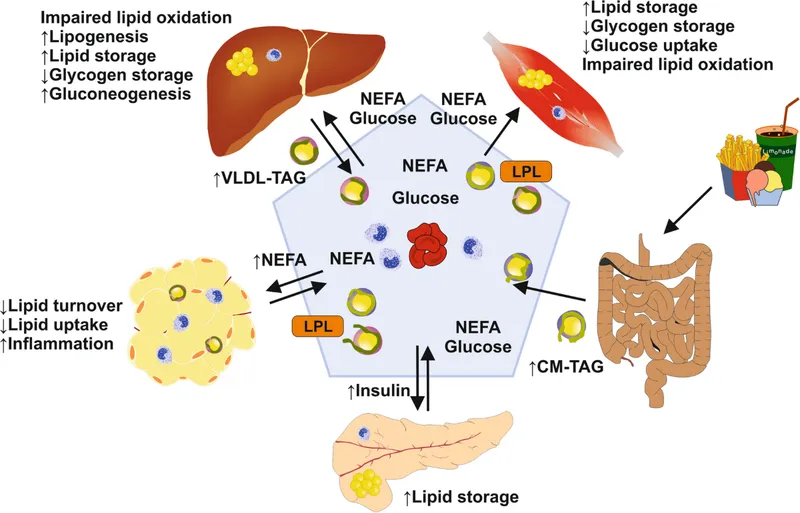
- The protein described is likely **hormone-sensitive lipase (HSL)**, which catabolizes **triglycerides** in adipocytes to **glycerol** and **fatty acids**.
- **Epinephrine** (and norepinephrine) stimulates HSL activity via a **cAMP-dependent protein kinase A (PKA)** pathway, leading to increased fatty acid release for energy.
*It is inhibited by glucagon*
- **Glucagon primarily acts on the liver** to promote gluconeogenesis and glycogenolysis, but it does **not directly inhibit HSL** in adipocytes.
- While glucagon has a lipolytic effect, it doesn't inhibit the enzyme that releases fatty acids.
*It is inhibited by acetylcholine*
- **Acetylcholine** is a neurotransmitter involved in the **parasympathetic nervous system**, which generally promotes energy storage.
- It does **not directly inhibit HSL**; its effects on lipid metabolism are indirect and typically involve other pathways.
*It is inhibited by cortisol*
- **Cortisol**, a glucocorticoid, generally **promotes lipolysis** (breakdown of fats) in certain contexts, particularly during stress to provide energy substrates.
- Therefore, it would **not inhibit HSL**; rather, it often enhances its activity or provides a permissive effect for other lipolytic hormones.
*It is stimulated by insulin*
- **Insulin** is an **anabolic hormone** that promotes energy storage, including **lipogenesis** (fat synthesis) and inhibits lipolysis.
- Insulin **inhibits HSL activity** by activating phosphodiesterase, which reduces cAMP levels, thus deactivating PKA and preventing HSL phosphorylation.
Integration of metabolic pathways US Medical PG Question 2: A 65-year-old male prisoner goes on a hunger strike to protest the conditions of his detainment. After 5 days without food, he suffers a seizure for which he is taken into a medical facility. On physical examination, he looks pale and diaphoretic. His blood glucose level is 50 mg/dL. In order to keep a constant supply of energy to his brain, which of the following molecules is his liver releasing into the bloodstream?
- A. Glycogen
- B. Glucose-6-phosphate
- C. ß-hydroxybutyric acid (Correct Answer)
- D. Fatty acids
- E. Glucose-1-phosphate
Integration of metabolic pathways Explanation: ***ß-hydroxybutyric acid***
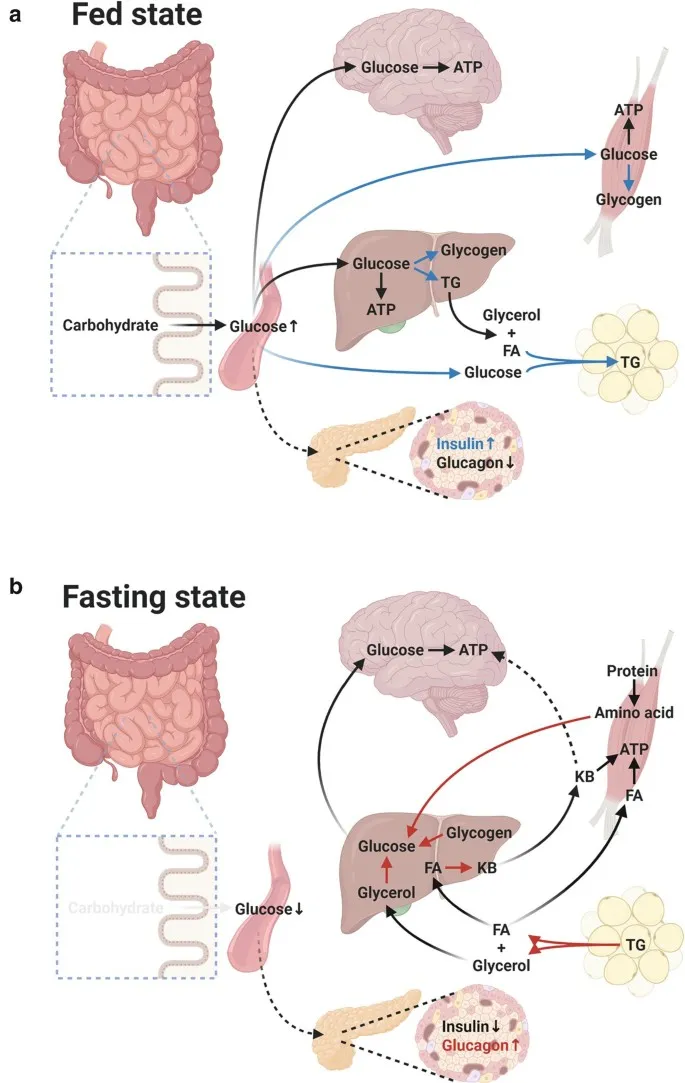
- After 5 days of a hunger strike, **glycogen stores** are depleted, forcing the body to rely on **fatty acid oxidation** and **ketone body production** in the liver as an alternative fuel source for the brain.
- **ß-hydroxybutyrate** is one of the primary ketone bodies released by the liver into the bloodstream to provide energy, especially for the brain, during prolonged fasting.
*Glycogen*
- **Glycogenolysis** (breakdown of glycogen) is a short-term response to low blood glucose and supplies glucose for only about 24-36 hours of fasting. After 5 days, **hepatic glycogen stores** would be largely depleted.
- The liver releases **free glucose** into the bloodstream, not intact glycogen, from glycogen breakdown.
*Glucose-6-phosphate*
- **Glucose-6-phosphate** is an intermediate in glycolysis and gluconeogenesis, but it is not directly released into the bloodstream by the liver.
- It must be converted to **free glucose** by glucose-6-phosphatase before it can exit the hepatocyte and enter circulation.
*Fatty acids*
- The liver takes up **fatty acids** from adipose tissue breakdown during prolonged fasting to convert them into **ketone bodies**.
- While fatty acids are a major energy source for other tissues, the **brain cannot directly utilize fatty acids** for energy due to the inability of long-chain fatty acids to cross the blood-brain barrier.
*Glucose-1-phosphate*
- **Glucose-1-phosphate** is an intermediate formed during the breakdown of glycogen (glycogenolysis).
- Like glucose-6-phosphate, it is not directly released into the bloodstream but is further metabolized within the hepatocyte, eventually leading to the release of **free glucose**.
Integration of metabolic pathways US Medical PG Question 3: Certain glucose transporters that are expressed predominantly on skeletal muscle cells and adipocytes are unique compared to those transporters found on other cell types within the body. Without directly affecting glucose transport in other cell types, which of the following would be most likely to selectively increase glucose uptake in skeletal muscle cells and adipocytes?
- A. Increased plasma glucose concentration
- B. It is physiologically impossible to selectively increase glucose uptake in specific cells
- C. Increased levels of circulating insulin (Correct Answer)
- D. Decreased plasma glucose concentration
- E. Decreased levels of circulating insulin
Integration of metabolic pathways Explanation: ***Increased levels of circulating insulin***
- Insulin stimulates the translocation of **GLUT4 transporters** from intracellular vesicles to the cell membrane in **skeletal muscle** and **adipocytes**, thereby increasing glucose uptake.
- This mechanism is **selective** because other cell types (e.g., brain, liver) primarily use insulin-independent glucose transporters (e.g., GLUT1, GLUT2, GLUT3) that are constitutively active or respond to different signals.
*Increased plasma glucose concentration*
- While increased glucose concentration would drive glucose uptake in many cells, it is not **selective** for skeletal muscle and adipocytes since other cells also take up glucose.
- Insulin-independent tissues would also increase glucose uptake, making this a non-specific effect.
*It is physiologically impossible to selectively increase glucose uptake in specific cells*
- This statement is incorrect because the body has mechanisms, such as **insulin-mediated GLUT4 translocation**, that specifically regulate glucose uptake in certain cell types like skeletal muscle and adipocytes.
- This regulatory specificity is crucial for maintaining **glucose homeostasis**.
*Decreased plasma glucose concentration*
- A decrease in plasma glucose would generally **reduce** glucose uptake across all cell types, including skeletal muscle and adipocytes.
- It would not selectively increase uptake in any specific cell population.
*Decreased levels of circulating insulin*
- Decreased insulin levels would lead to **reduced** glucose uptake in insulin-sensitive tissues like skeletal muscle and adipocytes, as GLUT4 transporters would remain sequestered intracellularly.
- This would result in higher circulating glucose levels rather than increased uptake.
Integration of metabolic pathways US Medical PG Question 4: An investigator is studying a hereditary defect in the mitochondrial enzyme succinyl-CoA synthetase. In addition to succinate, the reaction catalyzed by this enzyme produces a molecule that is utilized as an energy source for protein translation. This molecule is also required for which of the following conversion reactions?
- A. Oxaloacetate to phosphoenolpyruvate (Correct Answer)
- B. Pyruvate to acetyl-CoA
- C. Acetaldehyde to acetate
- D. Glucose-6-phosphate to 6-phosphogluconolactone
- E. Fructose-6-phosphate to fructose-1,6-bisphosphate
Integration of metabolic pathways Explanation: ***Oxaloacetate to phosphoenolpyruvate***
- The reaction catalyzed by **succinyl-CoA synthetase** (also known as succinate thiokinase) produces **GTP** (guanosine triphosphate) from GDP and Pi, in addition to succinate.
- **GTP** is required for the conversion of **oxaloacetate** to **phosphoenolpyruvate** in gluconeogenesis, catalyzed by **PEP carboxykinase**.
*Pyruvate to acetyl-CoA*
- This reaction is catalyzed by the **pyruvate dehydrogenase complex** and produces NADH, not GTP.
- It is an irreversible step linking glycolysis to the citric acid cycle.
*Acetaldehyde to acetate*
- This reaction is catalyzed by **aldehyde dehydrogenase** and uses **NAD+** as a cofactor, producing NADH.
- It is involved in alcohol metabolism.
*Glucose-6-phosphate to 6-phosphogluconolactone*
- This is the first committed step of the **pentose phosphate pathway**, catalyzed by **glucose-6-phosphate dehydrogenase**.
- It uses **NADP+** as a cofactor, producing NADPH.
*Fructose-6-phosphate to fructose-1,6-bisphosphate*
- This reaction is a key regulatory step in **glycolysis**, catalyzed by **phosphofructokinase-1 (PFK-1)**.
- It consumes **ATP**, rather than producing GTP or utilizing it as a cofactor in the context of this question.
Integration of metabolic pathways US Medical PG Question 5: A 10-month-old boy with a seizure disorder is brought to the physician by his mother because of a 2-day history of vomiting and lethargy. Laboratory studies show a decreased serum glucose concentration with low ketones. Further testing confirms a deficiency in an enzyme involved in fatty acid oxidation. Which of the following enzymes is most likely deficient in this patient?
- A. Acyl-CoA dehydrogenase (Correct Answer)
- B. HMG-CoA reductase
- C. Glycerol kinase
- D. Acetyl-CoA carboxylase
- E. Glycerol-3-phosphate dehydrogenase
Integration of metabolic pathways Explanation: ***Acyl-CoA dehydrogenase***
- The combination of **hypoglycemia** with **low ketones** in a setting of prolonged vomiting (stress) strongly suggests a **disorder of fatty acid oxidation**. These disorders impair the body's ability to produce ketones when glucose stores are low.
- **Acyl-CoA dehydrogenase** is a key enzyme in the mitochondrial β-oxidation of fatty acids. A deficiency prevents the breakdown of fatty acids into acetyl-CoA, which is necessary for ketogenesis and to fuel gluconeogenesis indirectly.
*HMG-CoA reductase*
- This enzyme is involved in **cholesterol synthesis**, not directly in fatty acid oxidation or ketone body formation from fatty acids.
- Deficiency would primarily affect cholesterol levels and not typically present with the described metabolic crisis of hypoglycemia and low ketones.
*Glycerol kinase*
- **Glycerol kinase** phosphorylates glycerol, a product of triglyceride hydrolysis, allowing it to enter glycolysis or gluconeogenesis.
- A deficiency would impair glycerol utilization but would not directly impact fatty acid oxidation pathways that are critical for ketone production during hypoglycemia.
*Acetyl-CoA carboxylase*
- **Acetyl-CoA carboxylase** is the rate-limiting enzyme in **fatty acid synthesis**, not degradation.
- A deficiency would lead to impaired fatty acid synthesis, which is the opposite of the metabolic problem described (impaired breakdown of fatty acids).
*Glycerol-3-phosphate dehydrogenase*
- This enzyme is involved in the conversion of **dihydroxyacetone phosphate (DHAP)** to **glycerol-3-phosphate** in both triglyceride synthesis and the glycerol phosphate shuttle.
- While related to lipid metabolism, a deficiency would not directly cause the severe hypoglycemia and hypoketosis seen with a fatty acid oxidation defect.
Integration of metabolic pathways US Medical PG Question 6: Which hormone most strongly stimulates gluconeogenesis during prolonged fasting?
- A. Insulin
- B. Epinephrine
- C. Cortisol
- D. Glucagon (Correct Answer)
Integration of metabolic pathways Explanation: ***Glucagon***
- **Glucagon** is the primary hormone that promotes **gluconeogenesis** and glycogenolysis to maintain blood glucose during fasting.
- Its secretion is strongly stimulated by **low blood glucose levels**, making it critical throughout fasting states.
- Glucagon directly stimulates hepatic gluconeogenic enzymes and increases the availability of gluconeogenic substrates.
*Insulin*
- **Insulin** is an **anabolic hormone** that promotes glucose uptake and storage, thereby decreasing blood glucose levels.
- Its levels decrease during fasting, *suppressing* rather than stimulating gluconeogenesis.
- Insulin inhibits gluconeogenic enzyme expression and promotes glycolysis instead.
*Epinephrine*
- **Epinephrine** (adrenaline) is a stress hormone that rapidly increases blood glucose through both **glycogenolysis** and gluconeogenesis.
- Its effects are more prominent during **acute stress** or immediate energy demands (fight-or-flight response), rather than sustained fasting.
- Its action is rapid but transient compared to glucagon's sustained effect during fasting.
*Cortisol*
- **Cortisol** is a glucocorticoid that promotes **gluconeogenesis** by providing amino acid substrates through protein catabolysis and inducing gluconeogenic enzymes.
- While cortisol becomes increasingly important in **prolonged fasting** (>24-48 hours), **glucagon remains the primary and most potent direct stimulator** of hepatic gluconeogenesis throughout all phases of fasting.
- Cortisol's effects are slower in onset but more sustained, working synergistically with glucagon during extended fasting periods.
Integration of metabolic pathways US Medical PG Question 7: A 26-year-old man comes to the physician for evaluation of fatigue, facial rash, hair loss, and tingling of his hands and feet. He has followed a vegetarian diet for the past 3 years and has eaten 8 raw egg whites daily for the past year in preparation for a bodybuilding competition. Physical examination shows conjunctival injections and a scaly, erythematous rash around the eyes and mouth. Laboratory studies show decreased activity of propionyl-coenzyme A carboxylase in peripheral blood lymphocytes. Which of the following substances is most likely to be decreased in this patient?
- A. Methylmalonyl-CoA (Correct Answer)
- B. Cystathionine
- C. Lactate
- D. Adenine
- E. Ribulose-5-phosphate
Integration of metabolic pathways Explanation: ***Methylmalonyl-CoA***
- This patient has classic **biotin deficiency** due to consumption of raw egg whites. **Avidin** in raw egg whites binds biotin and prevents its absorption, leading to symptoms of dermatitis, alopecia, conjunctivitis, and neurological manifestations.
- Biotin is an essential cofactor for several carboxylase enzymes, including **propionyl-CoA carboxylase**, which catalyzes the conversion of **propionyl-CoA → methylmalonyl-CoA**.
- With **decreased propionyl-CoA carboxylase activity** (as stated in the question), the enzyme cannot efficiently convert its substrate to product. This results in **decreased formation of the product, methylmalonyl-CoA**.
- While propionyl-CoA (the substrate) would accumulate, methylmalonyl-CoA (the product) would be **decreased** due to impaired enzymatic conversion.
*Cystathionine*
- Cystathionine is an intermediate in the **transsulfuration pathway** (homocysteine → cysteine), which requires **vitamin B6** as a cofactor, not biotin.
- Its levels would not be directly affected by biotin deficiency or decreased propionyl-CoA carboxylase activity.
*Lactate*
- Lactate levels are elevated in conditions involving **anaerobic metabolism** or impaired mitochondrial function.
- Biotin deficiency can affect pyruvate carboxylase (another biotin-dependent enzyme), but this would not specifically decrease lactate levels. If anything, impaired pyruvate carboxylase might increase lactate by limiting pyruvate's entry into gluconeogenesis.
*Adenine*
- Adenine is a purine nucleobase involved in nucleotide synthesis and salvage pathways.
- Its metabolism is unrelated to biotin-dependent carboxylases and would not be affected in this patient.
*Ribulose-5-phosphate*
- Ribulose-5-phosphate is an intermediate in the **pentose phosphate pathway**, which generates NADPH and ribose-5-phosphate for nucleotide synthesis.
- This pathway is independent of biotin-dependent enzymes and would not be directly affected by propionyl-CoA carboxylase deficiency.
Integration of metabolic pathways US Medical PG Question 8: An investigator is studying biomolecular mechanisms in human cells. A radioactive isotope that is unable to cross into organelles is introduced into a sample of cells. The cells are then fragmented via centrifugation and the isotope-containing components are isolated. Which of the following reactions is most likely to be present in this cell component?
- A. Glucose-6-phosphate to glucose
- B. Isocitrate to α-ketoglutarate
- C. Carbamoyl phosphate to citrulline
- D. Fatty acyl-CoA to acetyl-CoA
- E. Glucose-6-phosphate to 6-phosphogluconolactone (Correct Answer)
Integration of metabolic pathways Explanation: ***Glucose-6-phosphate to 6-phosphogluconolactone***
- This reaction is the first step of the **pentose phosphate pathway (PPP)**, which occurs in the **cytosol**.
- Since the isotope cannot cross into organelles and is found in the cytosolic fraction, this pathway is a likely candidate.
*Glucose-6-phosphate to glucose*
- This reaction describes the dephosphorylation of **glucose-6-phosphate** to **glucose**, catalyzed by **glucose-6-phosphatase**.
- While important for glucose release, this enzyme is primarily located in the **endoplasmic reticulum** of the liver and kidneys, an organelle.
*Isocitrate to α-ketoglutarate*
- This is a step in the **Krebs cycle (citric acid cycle)**, which takes place in the **mitochondrial matrix**.
- The isotope would not be found in this compartmentalized reaction because it cannot enter organelles.
*Carbamoyl phosphate to citrulline*
- This reaction is part of the **urea cycle**, which has steps occurring in both the **mitochondrial matrix** and the cytosol. The initial step, forming carbamoyl phosphate, is mitochondrial.
- The isotope, being unable to cross into organelles, would not readily participate in the mitochondrial portion of this pathway.
*Fatty acyl-CoA to acetyl-CoA*
- This reaction represents **beta-oxidation of fatty acids**, a process that primarily occurs in the **mitochondria** and peroxisomes.
- As the isotope is excluded from organelles, it would not be involved in these reactions.
Integration of metabolic pathways US Medical PG Question 9: A 45-year-old patient presents with joint pain and weakness and is known to have homocystinuria. Which vitamin is required in the treatment?
- A. Vitamin B6 (Correct Answer)
- B. Vitamin B12
- C. Vitamin B7
- D. Vitamin B1
- E. Vitamin B9
Integration of metabolic pathways Explanation: ***Vitamin B6***
- **Homocystinuria** is often caused by a deficiency in the enzyme **cystathionine beta-synthase**, which requires **pyridoxal phosphate (active form of B6)** as a cofactor.
- Supplementation with high-dose **vitamin B6** can help some patients by increasing the residual activity of the enzyme, thereby reducing **homocysteine levels**.
- This is the **primary treatment** for **B6-responsive homocystinuria** (approximately 50% of cases respond to B6 therapy).
*Vitamin B12*
- Vitamin B12 is a cofactor for the enzyme **methionine synthase**, which converts homocysteine back to methionine.
- While it plays a role in homocysteine metabolism, **vitamin B6** is typically the primary treatment for homocystinuria caused by **cystathionine beta-synthase deficiency**.
*Vitamin B9*
- Vitamin B9 (folic acid) works together with **vitamin B12** as a cofactor in the **remethylation pathway** via methionine synthase.
- While folate supplementation may help lower homocysteine levels, it is **not the primary treatment** for classical homocystinuria due to cystathionine beta-synthase deficiency.
- **Vitamin B6** remains the first-line vitamin therapy for enzyme deficiency-related homocystinuria.
*Vitamin B7*
- Vitamin B7, or **biotin**, is a cofactor for carboxylase enzymes and is involved in fatty acid synthesis and gluconeogenesis.
- It has no direct role in the metabolism of **homocysteine** or the treatment of homocystinuria.
*Vitamin B1*
- Vitamin B1, or **thiamine**, is essential for carbohydrate metabolism and nerve function.
- It is not involved in the metabolic pathways that regulate **homocysteine levels** or the treatment of homocystinuria.
Integration of metabolic pathways US Medical PG Question 10: A 15-year-old boy presents with sudden onset right sided weakness of his arm and face and difficulty speaking. He denies any problems with hearing or comprehension. The patient has no history of chest pain, hypertension, or diabetes mellitus. No significant past medical history. The patient is afebrile, and vital signs are within normal limits. On physical examination, the patient is thin, with long arms and slender fingers. There is a right-sided facial droop present. Ophthalmic examination reveals a dislocated lens in the right eye. Strength is 3 out of 5 in the right upper extremity, and there is a positive Babinski reflex on the right. The CT scan of the head shows no evidence of hemorrhage. Laboratory findings are significant for increased concentrations of a metabolic intermediate in his serum and urine. Which of the following enzymes is most likely deficient in this patient?
- A. Homogentisate oxidase
- B. Branched-chain ketoacid dehydrogenase
- C. Hydroxymethylbilane (HMB) synthase
- D. Cystathionine β-synthase (Correct Answer)
- E. Phenylalanine hydroxylase
Integration of metabolic pathways Explanation: ***Cystathionine β-synthase***
- This patient's presentation with **Marfanoid habitus** (long arms, slender fingers, dislocated lens), sudden onset neurological deficits (weakness, facial droop, positive Babinski), and elevated metabolic intermediates points to **homocystinuria**. Homocystinuria is most commonly caused by a deficiency in **cystathionine β-synthase (CBS)**, leading to the accumulation of homocysteine.
- Elevated homocysteine levels are highly prothrombotic, explaining the **stroke-like symptoms** (right-sided weakness, facial droop, aphasia) in a young patient without traditional risk factors for stroke.
*Homogentisate oxidase*
- Deficiency in **homogentisate oxidase** causes **alkaptonuria**, characterized by **dark urine** upon standing, ochronosis (bluish-black discoloration of cartilage and connective tissues), and severe arthritis.
- Alkaptonuria does not typically present with acute thrombotic events, Marfanoid features, or specific neurological deficits.
*Branched-chain ketoacid dehydrogenase*
- A defect in **branched-chain ketoacid dehydrogenase** is responsible for **Maple Syrup Urine Disease (MSUD)**, which typically presents in infancy with poor feeding, vomiting, lethargy, developmental delay, and urine smelling like maple syrup.
- This enzyme deficiency is not associated with the Marfanoid habitus or acute thrombotic neurological events described in this patient.
*Hydroxymethylbilane (HMB) synthase*
- Deficiency of **HMB synthase** (also known as porphobilinogen deaminase) causes **Acute Intermittent Porphyria (AIP)**, characterized by acute attacks of severe abdominal pain, psychiatric symptoms (anxiety, depression, hallucinations), and neurological dysfunction (peripheral neuropathy, seizures).
- AIP does not cause Marfanoid features or tend to present with acute stroke-like symptoms due to thrombosis.
*Phenylalanine hydroxylase*
- A deficiency in **phenylalanine hydroxylase** causes **phenylketonuria (PKU)**, which is typically identified through newborn screening. Symptoms, if untreated, include intellectual disability, seizures, and a musty odor.
- PKU does not present with Marfanoid features, dislocated lenses, or acute thrombotic complications leading to stroke.
More Integration of metabolic pathways US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.