Electron transport chain and oxidative phosphorylation US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Electron transport chain and oxidative phosphorylation. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Electron transport chain and oxidative phosphorylation US Medical PG Question 1: An investigator is developing a drug that selectively inhibits the retrograde axonal transport of rabies virus towards the central nervous system. To achieve this effect, this drug must target which of the following?
- A. Dynein (Correct Answer)
- B. Tubulin
- C. Nidogen
- D. Kinesin
- E. Acetylcholine
Electron transport chain and oxidative phosphorylation Explanation: ***Dynein***
- **Dynein** is a microtubule-dependent motor protein responsible for **retrograde axonal transport**, moving cargo (like rabies virus) away from the axon terminals towards the cell body and ultimately the central nervous system.
- Inhibiting dynein would therefore prevent the **rabies virus** from traveling from the site of infection (e.g., muscle cell) to the central nervous system.
*Tubulin*
- **Tubulin** is the primary protein subunit that polymerizes to form **microtubules**, which serve as the tracks for axonal transport.
- Inhibiting tubulin polymerization would disrupt both **anterograde** and **retrograde transport** nonspecifically, leading to severe neurotoxicity rather than selective inhibition of rabies virus transport.
*Nidogen*
- **Nidogen** (also known as entactin) is a glycoprotein component of the **basal lamina**, an extracellular matrix structure.
- It plays a role in cell adhesion and tissue organization but is not directly involved in the intracellular motor processes of axonal transport.
*Kinesin*
- **Kinesin** is a microtubule-dependent motor protein primarily responsible for **anterograde axonal transport**, moving cargo from the cell body towards the axon terminals.
- Inhibiting kinesin would disrupt the outward movement of vesicles and organelles, but would not prevent the **inward retrograde transport** of the rabies virus.
*Acetylcholine*
- **Acetylcholine** is a neurotransmitter that plays a role in synaptic transmission in both the peripheral and central nervous systems.
- While rabies virus can affect neuronal function, acetylcholine itself is not a motor protein or a structural component directly involved in the physical process of **axonal transport**.
Electron transport chain and oxidative phosphorylation US Medical PG Question 2: In your peripheral tissues and lungs, carbonic anhydrase works to control the equilibrium between carbon dioxide and carbonic acid in order to maintain proper blood pH. Through which mechanism does carbonic anhydrase exert its influence on reaction kinetics?
- A. Changes the delta G of the reaction
- B. Lowers the free energy of products
- C. Raises the activation energy
- D. Lowers the activation energy (Correct Answer)
- E. Lowers the free energy of reactants
Electron transport chain and oxidative phosphorylation Explanation: ***Lowers the activation energy***
- Enzymes like **carbonic anhydrase** function by providing an alternative reaction pathway with a **lower activation energy**.
- This reduction in activation energy leads to a significant increase in the **reaction rate**, allowing the reaction to proceed more quickly without altering its equilibrium.
*Changes the delta G of the reaction*
- Enzymes do not alter the **overall Gibbs free energy change (ΔG)** of a reaction.
- The **ΔG** is a thermodynamic property determined by the difference in free energy between reactants and products, which is unaffected by catalyst.
*Lowers the free energy of products*
- Enzymes do not change the **free energy** of either the products or the reactants.
- Affecting the free energy of products would alter the overall **ΔG** of the reaction and thus the **equilibrium constant**.
*Raises the activation energy*
- Raising the **activation energy** would slow down the reaction rate, which is the opposite of an enzyme's function.
- Enzymes are catalysts designed to **accelerate reactions** by lowering the energy barrier.
*Lowers the free energy of reactants*
- Enzymes do not change the **free energy** of reactants.
- Altering the free energy of reactants would also change the overall **ΔG** of the reaction and its equilibrium.
Electron transport chain and oxidative phosphorylation US Medical PG Question 3: In skeletal muscle, which step of excitation-contraction coupling requires ATP?
- A. Cross-bridge cycling (Correct Answer)
- B. Action potential propagation
- C. Troponin binding to calcium
- D. Calcium release from SR
Electron transport chain and oxidative phosphorylation Explanation: ***Cross-bridge cycling***
- ATP is essential for two key actions in **cross-bridge cycling**: the **detachment of myosin heads from actin** and the **re-cocking of the myosin heads** for the next power stroke.
- Without ATP, myosin heads remain attached to actin, leading to **rigor mortis**.
*Action potential propagation*
- This process involves the flow of **ions (Na+ and K+)** across the sarcolemma through voltage-gated channels, which is a passive event down their electrochemical gradients.
- While ion pumps (like the Na+/K+ pump) maintain these gradients over time, the **propagation itself is not a direct ATP-dependent step** in the immediate sense of the action potential.
*Troponin binding to calcium*
- The binding of **calcium to troponin C** is a passive chemical interaction driven by the *concentration gradient* of calcium ions.
- This binding triggers a **conformational change** in the troponin-tropomyosin complex, exposing actin binding sites, and does not directly consume ATP.
*Calcium release from SR*
- The release of calcium from the **sarcoplasmic reticulum (SR)** into the sarcoplasm occurs through **ryanodine receptors**, which are mechanically or voltage-gated channels.
- This is a passive efflux down the **calcium concentration gradient**, and does not directly consume ATP.
Electron transport chain and oxidative phosphorylation US Medical PG Question 4: After being warned by the locals not to consume the freshwater, a group of American backpackers set off on a week-long hike into a region of the Ecuadorean Amazon forest known for large gold mines. The group of hikers stopped near a small stream and used the water they filtered from the stream to make dinner. Within the next half hour, the hikers began to experience headaches, vertigo, visual disturbances, confusion, tachycardia, and altered levels of consciousness. Which of the following enzymes was most likely inhibited in this group of hikers?
- A. NADH dehydrogenase
- B. ATP synthase
- C. Cytochrome c oxidase (Correct Answer)
- D. Cytochrome bc1 complex
- E. Succinate dehydrogenase
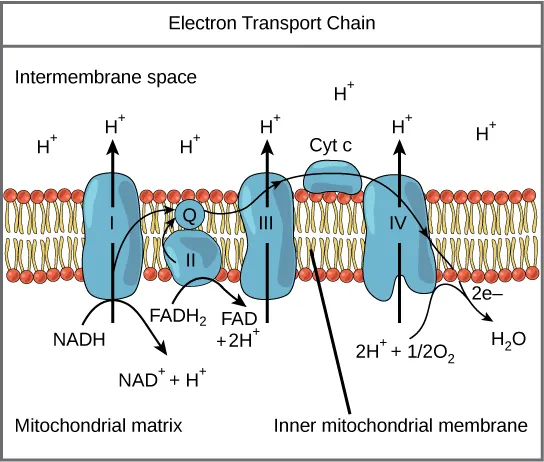
Electron transport chain and oxidative phosphorylation Explanation: ***Cytochrome c oxidase***
- The symptoms described (headaches, vertigo, visual disturbances, confusion, tachycardia, altered consciousness occurring within 30 minutes) are characteristic of **acute cyanide poisoning**.
- **Cyanide** is commonly found in water near **gold mining operations**, where it is used in the gold extraction process and can contaminate local water sources.
- **Cyanide** is a potent inhibitor of **cytochrome c oxidase** (Complex IV) in the electron transport chain, binding to the heme iron (Fe³⁺) and preventing oxygen utilization, leading to **histotoxic hypoxia**.
- This results in cellular energy failure, particularly affecting high-energy-demand organs like the brain and heart, explaining the acute neurological and cardiovascular symptoms.
*NADH dehydrogenase*
- While NADH dehydrogenase (Complex I) is a component of the electron transport chain, it is not the primary target of **cyanide poisoning**.
- Inhibitors of Complex I include rotenone and barbiturates, which cause different clinical presentations and do not produce the rapid onset of symptoms seen with cyanide.
*ATP synthase*
- **ATP synthase** (Complex V) synthesizes ATP using the proton gradient, but it is not directly inhibited by **cyanide**.
- Inhibitors of ATP synthase, such as oligomycin, prevent ATP synthesis by blocking the enzyme directly, whereas cyanide acts upstream at Complex IV.
*Cytochrome bc1 complex*
- The **cytochrome bc1 complex** (Complex III) is involved in electron transfer and proton pumping, but it is not the primary enzyme inhibited by **cyanide**.
- Inhibitors of Complex III include antimycin A, which would disrupt the electron transport chain but do not cause the characteristic rapid-onset symptoms of cyanide poisoning.
*Succinate dehydrogenase*
- **Succinate dehydrogenase** (Complex II) participates in both the citric acid cycle and the electron transport chain, but it is not targeted by **cyanide**.
- Inhibitors of Complex II, such as malonate, competitively block succinate oxidation but do not produce the acute systemic toxicity characteristic of cyanide poisoning.
Electron transport chain and oxidative phosphorylation US Medical PG Question 5: An investigator is studying muscle tissue in high-performance athletes. He obtains blood samples from athletes before and after a workout session consisting of short, fast sprints. Which of the following findings is most likely upon evaluation of blood obtained after the workout session?
- A. Decreased concentration of NADH
- B. Increased concentration of H+ (Correct Answer)
- C. Decreased concentration of lactate
- D. Increased concentration of insulin
- E. Increased concentration of ATP
Electron transport chain and oxidative phosphorylation Explanation: ***Increased concentration of H+***
- During **anaerobic metabolism** in high-intensity exercise like sprints, pyruvate is converted to **lactate** by **lactate dehydrogenase** to regenerate NAD+. This process produces H+, leading to a decrease in pH and an increase in H+ concentration in the blood.
- The accumulation of **hydrogen ions (H+)** contributes to metabolic acidosis, muscle fatigue, and the burning sensation experienced during intense exertion.
- Blood gas analysis would show **decreased pH** and **increased H+ concentration**.
*Decreased concentration of NADH*
- NADH is primarily an **intracellular metabolite** and is not typically measured in blood samples as it does not circulate freely in significant concentrations.
- Within muscle cells during anaerobic glycolysis, NADH is consumed by lactate dehydrogenase to convert pyruvate to lactate, regenerating NAD+ for continued glycolysis.
- This option is not a realistic blood finding from a clinical laboratory perspective.
*Decreased concentration of lactate*
- **High-intensity sprints** primarily rely on **anaerobic metabolism**, which rapidly produces **lactate** from pyruvate.
- Therefore, the concentration of lactate in the blood would significantly **increase** after such a workout, not decrease.
- Elevated blood lactate is a hallmark finding after intense anaerobic exercise.
*Increased concentration of insulin*
- **Insulin** levels typically **decrease** during exercise, especially high-intensity exercise, due to **sympathetic nervous system activation** and the body's need to mobilize glucose from liver glycogen and fatty acids.
- Exercise promotes glucose uptake through **insulin-independent mechanisms** (GLUT4 translocation via AMP-activated protein kinase).
- Increased insulin would be counterproductive during intense exercise when glucose mobilization is needed.
*Increased concentration of ATP*
- ATP does not circulate in blood in measurable concentrations as a typical laboratory finding.
- Within muscle cells, ATP is rapidly **consumed** during intense exercise to fuel muscle contraction.
- While cells work to maintain ATP levels through anaerobic glycolysis and the creatine phosphate system, net ATP does not accumulate in the blood.
Electron transport chain and oxidative phosphorylation US Medical PG Question 6: A startup is working on a novel project in which they claim they can replicate the organelle that is defective in MELAS syndrome. Which of the following metabolic processes must they be able to replicate if their project is to mimic the metabolic processes of this organelle?
- A. Hexose monophosphate shunt
- B. Cholesterol synthesis
- C. Glycolysis
- D. Fatty acid (beta) oxidation (Correct Answer)
- E. Fatty acid synthesis
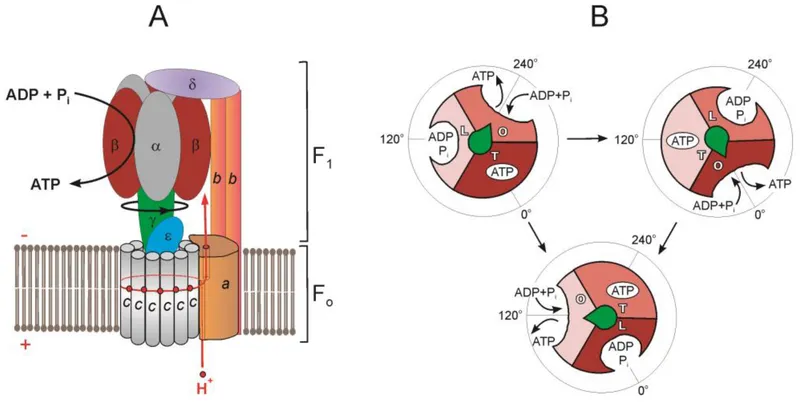
Electron transport chain and oxidative phosphorylation Explanation: ***Fatty acid (beta) oxidation***
- **MELAS syndrome** (Mitochondrial Encephalomyopathy, Lactic Acidosis, and Stroke-like episodes) is caused by defects in **mitochondrial function**.
- **Beta-oxidation of fatty acids** is a crucial metabolic process that occurs within the mitochondria, generating ATP.
*Hexose monophosphate shunt*
- The **hexose monophosphate shunt** (pentose phosphate pathway) occurs in the **cytosol** and is primarily involved in producing NADPH and synthesizing nucleotides, not a primary mitochondrial function.
- Its dysfunction is not directly linked to the core metabolic defects seen in MELAS syndrome.
*Cholesterol synthesis*
- **Cholesterol synthesis** primarily occurs in the **cytosol** and the **endoplasmic reticulum**, not within the mitochondria.
- While cholesterol metabolism can be indirectly affected by mitochondrial health, it is not a direct mitochondrial metabolic pathway.
*Glycolysis*
- **Glycolysis** is the metabolic pathway that converts glucose into pyruvate, occurring in the **cytosol**.
- Although it precedes mitochondrial oxidative phosphorylation, glycolysis itself does not occur within the mitochondria.
*Fatty acid synthesis*
- **Fatty acid synthesis** primarily takes place in the **cytosol** and endoplasmic reticulum, utilizing NADPH from the hexose monophosphate shunt.
- It is an anabolic process, while MELAS typically involves defects in catabolic/energy-producing mitochondrial pathways.
Electron transport chain and oxidative phosphorylation US Medical PG Question 7: A drug that inhibits mRNA synthesis has the well-documented side effect of red-orange body fluids. For which of the following is this drug used as monotherapy?
- A. Brucellosis
- B. Tuberculosis
- C. Methicillin-resistant staphylococcus aureus infection
- D. Mycobacterium avium intracellulare infection
- E. Neisseria meningitidis prophylaxis (Correct Answer)
Electron transport chain and oxidative phosphorylation Explanation: ***Neisseria meningitidis prophylaxis***
- The drug described is **rifampin**, which inhibits bacterial **DNA-dependent RNA polymerase**, thereby blocking **mRNA synthesis** and causes characteristic **red-orange discoloration of body fluids** (tears, urine, sweat).
- Rifampin is used as **monotherapy** for **prophylaxis** against **Neisseria meningitidis** infection in close contacts of infected patients.
- This is the **only indication** where rifampin monotherapy is appropriate, as prophylaxis requires short-term use where resistance development is not a concern.
*Tuberculosis*
- Rifampin is a **first-line agent** for tuberculosis treatment and a cornerstone of all TB regimens.
- However, it is **never used as monotherapy** for TB due to rapid development of resistance.
- Standard TB treatment requires **multidrug therapy** with rifampin, isoniazid, pyrazinamide, and ethambutol (RIPE) for initial phase.
*Methicillin-resistant Staphylococcus aureus infection*
- Rifampin is sometimes used in **combination** with other antibiotics (e.g., vancomycin, daptomycin) to treat **MRSA infections**, especially those involving **prosthetic devices** or **biofilms**.
- It is **not used as monotherapy** for active MRSA infections due to extremely high rates of spontaneous resistance.
*Mycobacterium avium intracellulare infection*
- **Mycobacterium avium complex (MAC)** infections require a multidrug regimen, typically including **macrolides (azithromycin or clarithromycin)**, **ethambutol**, and sometimes **rifabutin** (a rifamycin derivative preferred over rifampin).
- **Monotherapy is never appropriate** for MAC infections due to resistance concerns and treatment failure.
*Brucellosis*
- **Brucellosis** treatment requires **combination therapy**, typically **doxycycline plus rifampin** for 6 weeks or longer.
- **Rifampin monotherapy** is inadequate for eradicating Brucella infection and leads to treatment failure and resistance development.
Electron transport chain and oxidative phosphorylation US Medical PG Question 8: A 13-year-old girl is brought to the physician by her mother because of a 1-month history of abnormal movements of her muscles that she cannot control. She has a younger brother with cognitive disabilities and epilepsy. Examination shows frequent, brief, involuntary contractions of the muscle groups of the upper arms, legs, and face that can be triggered by touch. An EEG shows generalized epileptiform activity. A trichrome stain of a skeletal muscle biopsy specimen shows muscle fibers with peripheral red inclusions that disrupt the normal fiber contour. Which of the following is the most likely underlying mechanism of the patient's symptoms?
- A. CTG trinucleotide repeat expansion
- B. Mutation of the methyl-CpG binding protein 2 gene
- C. Truncated dystrophin protein
- D. Autoimmune endomysial destruction
- E. Defective oxidative phosphorylation (Correct Answer)
Electron transport chain and oxidative phosphorylation Explanation: ***Defective oxidative phosphorylation***
- The constellation of **uncontrolled muscle movements (myoclonus)**, **epilepsy**, and the brother's **cognitive disabilities** strongly suggests a **mitochondrial disorder**.
- **Ragged red fibers** on trichrome stain of skeletal muscle biopsy are pathognomonic for **mitochondrial myopathies**, indicating defective oxidative phosphorylation due to abnormal mitochondrial aggregates.
*CTG trinucleotide repeat expansion*
- This is characteristic of **Myotonic Dystrophy**, which primarily presents with **myotonia** (delayed muscle relaxation), progressive muscle weakness, and often cataracts, rather than prominent myoclonus and seizures.
- While muscle weakness can occur, the specific biopsy findings and prominent myoclonus point away from this diagnosis.
*Mutation of the methyl-CpG binding protein 2 gene*
- A mutation in the **MECP2 gene** causes **Rett Syndrome**, an X-linked dominant disorder seen almost exclusively in girls.
- It involves normal development for 6-18 months followed by regression, loss of purposeful hand movements, **stereotypical hand-wringing**, and microcephaly, which are not described here.
*Truncated dystrophin protein*
- A truncated dystrophin protein causes **Duchenne Muscular Dystrophy**, an X-linked recessive disorder leading to progressive muscle weakness, **Gowers' sign**, and elevated creatine kinase.
- This condition does not typically present with myoclonus or the characteristic ragged red fibers, nor does it typically involve the sibling's intellectual disability and epilepsy in this manner.
*Autoimmune endomysial destruction*
- This mechanism is characteristic of **celiac disease**, which can have neurological symptoms like ataxia or peripheral neuropathy, but not typically the severe myoclonus, epilepsy, or muscle biopsy findings seen here.
- **Inflammatory myopathies** like polymyositis may show endomysial inflammation, but the clinical picture and specific biopsy findings (ragged red fibers) are not consistent.
Electron transport chain and oxidative phosphorylation US Medical PG Question 9: A 25-year-old woman comes to the emergency department because of a mild headache, dizziness, fatigue, and nausea over the past several hours. She has no history of serious illness and takes no medications. She lives in a basement apartment and uses a wood stove for heating. Her temperature is 36°C (96.8°F) and pulse is 120/min. Arterial blood gas analysis shows a carboxyhemoglobin level of 11% (N = < 1.5). Which of the following mechanisms is the underlying cause of this patient's symptoms?
- A. Formation of carboxyhemoglobin reducing oxygen transport capacity (Correct Answer)
- B. Inhibition of hemoglobin synthesis in bone marrow
- C. Direct cellular toxicity from carbon monoxide metabolites
- D. Competitive inhibition of oxygen at tissue level
- E. Decreased hemoglobin-oxygen binding affinity
Electron transport chain and oxidative phosphorylation Explanation: ***Formation of carboxyhemoglobin reducing oxygen transport capacity***
- Carbon monoxide binds to hemoglobin with **200-250 times greater affinity** than oxygen, forming **carboxyhemoglobin (COHb)**.
- This patient's **carboxyhemoglobin level of 11%** (normal <1.5%) confirms CO poisoning from the **wood stove** in her basement apartment.
- COHb formation **reduces oxygen-carrying capacity** of blood, leading to **tissue hypoxia** and symptoms of headache, dizziness, fatigue, and nausea.
- CO also **shifts the oxygen-hemoglobin dissociation curve leftward**, impairing oxygen release to tissues.
*Inhibition of hemoglobin synthesis in bone marrow*
- Carbon monoxide does **not** inhibit hemoglobin synthesis.
- This mechanism would be seen in conditions like **iron deficiency anemia**, **anemia of chronic disease**, or exposure to toxins like **lead**.
- CO poisoning is an **acute** problem of oxygen transport, not a chronic problem of hemoglobin production.
*Direct cellular toxicity from carbon monoxide metabolites*
- Carbon monoxide is **not significantly metabolized** in the human body.
- CO is eliminated unchanged through the **lungs** when the patient breathes fresh air or receives oxygen therapy.
- The toxicity is from **CO itself** binding to hemoglobin, myoglobin, and cytochrome enzymes, not from any metabolites.
*Competitive inhibition of oxygen at tissue level*
- While CO does bind to **myoglobin** and **mitochondrial cytochrome oxidase** at the tissue level, this is a **secondary mechanism**.
- The **primary and most significant mechanism** is carboxyhemoglobin formation, which reduces oxygen delivery to tissues.
- Tissue-level effects contribute to toxicity but don't explain the elevated **carboxyhemoglobin level** seen in this patient.
*Decreased hemoglobin-oxygen binding affinity*
- This is **incorrect**; CO actually causes hemoglobin to bind oxygen **more tightly**, not less.
- CO shifts the **oxygen-hemoglobin dissociation curve to the left**, increasing hemoglobin's affinity for oxygen and impairing oxygen release to tissues.
- The primary problem is **reduced oxygen-carrying capacity** from CO occupying hemoglobin binding sites, not decreased affinity.
Electron transport chain and oxidative phosphorylation US Medical PG Question 10: A 24-year-old man comes to the physician because his vision has worsened rapidly over the last 2 months. His maternal uncle lost his vision suddenly over a period of 3 months at 26 years of age. The patient's wife and 1-year-old son have normal vision. Funduscopic examination of the patient shows bilateral circumpapillary telangiectasia. Genetic testing shows a missense mutation in one of the genes of the electron transport chain complexes. The probability that this patient's son will be affected by the same disease is closest to which of the following?
- A. 33%
- B. 100%
- C. 0% (Correct Answer)
- D. 25%
- E. 50%
Electron transport chain and oxidative phosphorylation Explanation: ***0%***
- This condition, **Leber's Hereditary Optic Neuropathy (LHON)**, is caused by a mutation in **mitochondrial DNA**.
- **Mitochondrial DNA** is exclusively inherited from the mother, meaning the father cannot pass it on to his children.
*33%*
- This percentage does not align with any known pattern of Mendelian inheritance or mitochondrial inheritance.
- It would be too low for a dominant mitochondrial disorder and too high for a recessive one if the mother were a carrier.
*100%*
- While all children of an affected mother would inherit the disease, the patient is a male, and mitochondria are inherited maternally.
- Therefore, the father cannot pass on his **mitochondrial DNA** to his son.
*25%*
- This percentage is typically associated with **autosomal recessive inheritance**, where both parents are carriers.
- LHON follows a **mitochondrial inheritance pattern**, which is distinct from autosomal inheritance.
*50%*
- This percentage is characteristic of **autosomal dominant inheritance** or X-linked recessive inheritance where the mother is a carrier.
- Since this is a **mitochondrial disorder**, the father's genes are not involved in transmission to his son.
More Electron transport chain and oxidative phosphorylation US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.