Amino acid metabolism US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Amino acid metabolism. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Amino acid metabolism US Medical PG Question 1: An 8-day-old boy is brought to the physician by his mother because of vomiting and poor feeding. The pregnancy was uncomplicated, and he was born at full term. He appears pale and lethargic. Physical examination shows diffusely increased muscle tone. His urine is noted to have a sweet odor. This patient's symptoms are most likely caused by the accumulation of which of the following?
- A. Phenylalanine
- B. Homogentisic acid
- C. Isoleucine (Correct Answer)
- D. Homocysteine
- E. Phytanic acid
Amino acid metabolism Explanation: ***Isoleucine***
- The combination of **vomiting**, poor feeding, lethargy, **increased muscle tone**, and a **sweet-smelling urine** (often described as maple syrup odor) in a neonate strongly points to **Maple Syrup Urine Disease (MSUD)**.
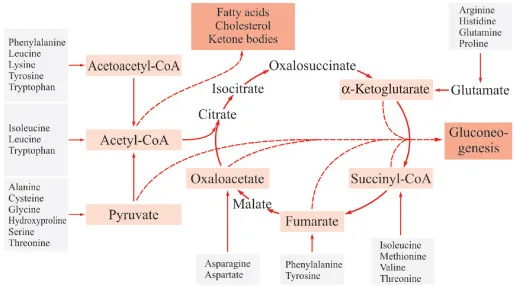
- MSUD is caused by a defect in the **branched-chain alpha-keto acid dehydrogenase complex**, leading to the accumulation of branched-chain amino acids (leucine, isoleucine, and valine) and their corresponding alpha-keto acids.
*Phenylalanine*
- Accumulation of **phenylalanine** is characteristic of **Phenylketonuria (PKU)**, which typically presents with intellectual disability, seizures, and an eczematous rash if untreated, but not a maple syrup odor in urine or acute neonatal crisis.
- The urine odor in PKU is often described as **mousy** or musty, distinctly different from a sweet or maple syrup odor.
*Homogentisic acid*
- Accumulation of **homogentisic acid** is seen in **Alkaptonuria**, an inborn error of metabolism that primarily causes dark urine upon standing (due to oxidation of homogentisic acid), ochronosis (blue-black pigmentation of cartilage and connective tissue later in life), and arthritis.
- It does not present with acute neonatal symptoms such as vomiting, lethargy, or a sweet urine odor.
*Homocysteine*
- Elevated levels of **homocysteine** are found in **Homocystinuria**, which can lead to intellectual disability, developmental delay, dislocation of the ocular lens (ectopia lentis), Marfanoid habitus, and thromboembolic events.
- It does not typically present in the neonatal period with a sweet urine odor or acute neurological symptoms like increased muscle tone.
*Phytanic acid*
- Accumulation of **phytanic acid** is characteristic of **Refsum disease**, a rare peroxisomal disorder that causes progressive neurological symptoms such as retinitis pigmentosa, peripheral neuropathy, ataxia, and deafness in childhood or adulthood.
- It does not present in the neonatal period with the described acute symptoms or unique urine odor.
Amino acid metabolism US Medical PG Question 2: A 36-year-old woman comes to the physician because of prolonged stiffness in the morning and progressive pain and swelling of her wrists and hands over the past 4 months. Examination shows bilateral swelling and mild tenderness of the wrists and the second, third, and fourth metacarpophalangeal joints. Her range of motion is limited by pain. Serum studies show elevated anti-cyclic citrullinated peptide antibodies. Treatment with methotrexate is begun. At a follow-up examination, her serum aspartate aminotransferase (AST) concentration is 75 U/L and her serum alanine aminotransferase (ALT) concentration is 81 U/L. Which of the following substances is essential for the function of these enzymes?
- A. Thiamine
- B. Pyridoxine (Correct Answer)
- C. Folic acid
- D. Riboflavin
- E. Niacin
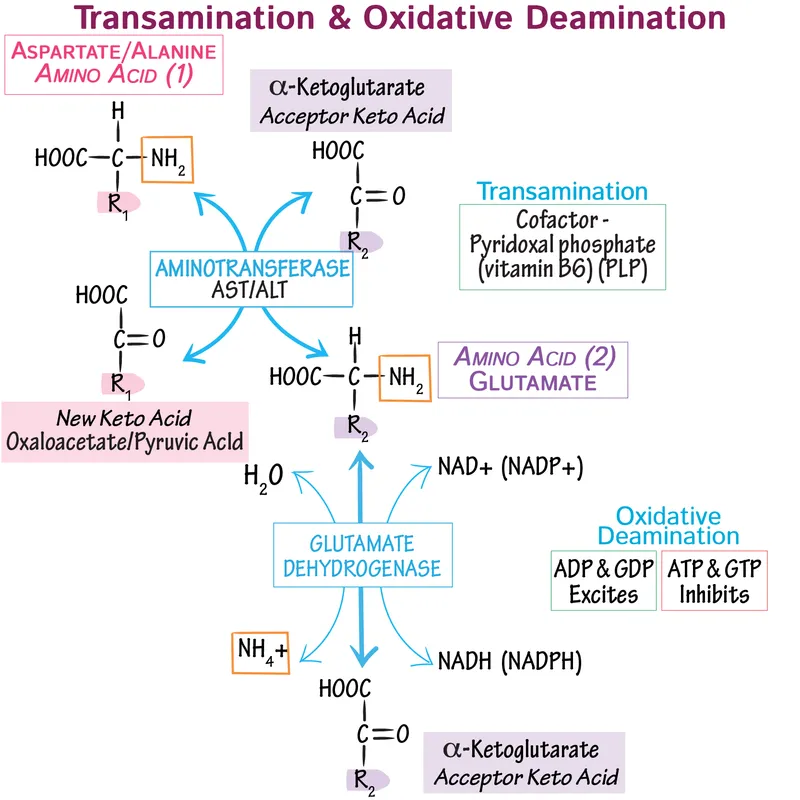
Amino acid metabolism Explanation: ***Pyridoxine***
- **Pyridoxine (Vitamin B6)** is a crucial **cofactor** for **aminotransferase enzymes** like AST and ALT, functioning as **pyridoxal phosphate (PLP)**.
- In the context of **methotrexate treatment**, monitoring liver enzymes is essential due to potential **hepatotoxicity**, and disturbances in pyridoxine metabolism can impact enzyme activity.
*Thiamine*
- **Thiamine (Vitamin B1)** is essential for enzymes involved in **carbohydrate metabolism**, particularly in the form of **thiamine pyrophosphate (TPP)**.
- It plays a primary role in reactions such as those catalyzed by **pyruvate dehydrogenase** and **alpha-ketoglutarate dehydrogenase**, not aminotransferases.
*Folic acid*
- **Folic acid (Vitamin B9)** is primarily involved in **one-carbon metabolism**, including **DNA synthesis** and repair.
- It is not a cofactor for AST or ALT; however, **leucovorin (folinic acid)** is often co-administered with methotrexate to mitigate its side effects.
*Riboflavin*
- **Riboflavin (Vitamin B2)** is a precursor for **flavin adenine dinucleotide (FAD)** and **flavin mononucleotide (FMN)**, which are cofactors for **redox reactions**.
- Enzymes like **succinate dehydrogenase** and **acyl-CoA dehydrogenase** require riboflavin, but not AST or ALT.
*Niacin*
- **Niacin (Vitamin B3)** is a precursor for **nicotinamide adenine dinucleotide (NAD+)** and **nicotinamide adenine dinucleotide phosphate (NADP+)**, which are vital for many **dehydrogenase reactions**.
- These coenzymes are crucial for **energy metabolism**, but not directly for the catalytic activity of aminotransferases.
Amino acid metabolism US Medical PG Question 3: A 30-year-old African American G1P0 mother gives birth to a male infant at 33 weeks' gestation. The mother had no prenatal care and took no prenatal vitamins. The child’s postnatal period was complicated by neonatal sepsis due to group B Streptococcus. He required a two week stay in the neonatal intensive care unit to receive antibiotics, cardiopulmonary support, and intravenous nutrition. He eventually recovered and was discharged. At a normal follow-up visit to the pediatrician’s office one month later, the mother asks about the child’s skin color and hair color. On examination, the child has white hair and diffusely pale skin. The child’s irises appear translucent. Further questioning of the mother reveals that there is a distant family history of blindness. This child most likely has a defect in an enzyme involved in the metabolism of which of the following molecules?
- A. Leucine
- B. Homocysteine
- C. Phenylalanine
- D. Homogentisic acid
- E. DOPA (Correct Answer)
Amino acid metabolism Explanation: ***DOPA***
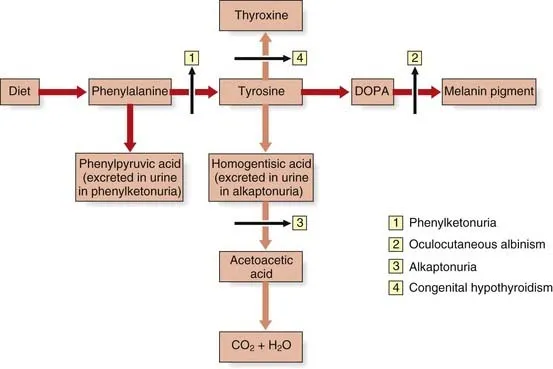
- The symptoms of **white hair**, **pale skin**, and **translucent irises**, along with a family history of **blindness**, are classic signs of **oculocutaneous albinism**.
- **Oculocutaneous albinism** results from a defect in **tyrosinase**, an enzyme responsible for converting **DOPA** (3,4-dihydroxyphenylalanine) into **melanin**.
*Leucine*
- Defects in **leucine** metabolism are associated with **Maple Syrup Urine Disease**, characterized by sweet-smelling urine and neurological complications, not albinism.
- This condition involves impaired **branched-chain alpha-keto acid dehydrogenase** complex activity, leading to an accumulation of branched-chain amino acids.
*Homocysteine*
- Problems with **homocysteine** metabolism are seen in conditions like **homocystinuria**, which can cause developmental delay, skeletal abnormalities, and vascular issues, but not hypopigmentation.
- This is often due to deficiencies in **cystathionine beta-synthase** or other enzymes involved in folate and vitamin B12 metabolism.
*Phenylalanine*
- A defect in **phenylalanine** metabolism, specifically **phenylalanine hydroxylase**, leads to **phenylketonuria (PKU)**, which causes intellectual disability, seizures, and a musty odor, but not the specific ocular and cutaneous features described for albinism.
- While PKU can cause milder hypopigmentation due to reduced tyrosine availability, the described translucent irises and severe white hair are more indicative of albinism.
*Homogentisic acid*
- A defect in **homogentisic acid** metabolism causes **alkaptonuria**, characterized by dark urine upon standing, blue-black discoloration of cartilage (ochronosis), and early-onset arthritis, which are not present in this case.
- This condition results from a deficiency of **homogentisate 1,2-dioxygenase**.
Amino acid metabolism US Medical PG Question 4: A 2-year-old boy is brought to the emergency department by his mother 30 minutes after having a generalized tonic-clonic seizure. He was born at home and has not attended any well-child visits. He is not yet able to walk and does not use recognizable words. His paternal uncle has a severe intellectual disability and has been living in an assisted-living facility all of his life. The boy's urine phenylacetate level is markedly elevated. Which of the following amino acids is most likely nutritionally essential for this patient because of his underlying condition?
- A. Alanine
- B. Glutamate
- C. Phenylalanine
- D. Cysteine
- E. Tyrosine (Correct Answer)
Amino acid metabolism Explanation: ***Tyrosine***
- The patient's presentation with seizures, developmental delay, and elevated **phenylacetate (a phenylalanine metabolite)** strongly suggest **phenylketonuria (PKU)**.
- In PKU, the enzyme **phenylalanine hydroxylase (PAH)** is deficient, preventing the conversion of **phenylalanine** to **tyrosine**, making **tyrosine** a **nutritionally essential** amino acid.
*Alanine*
- **Alanine** is a **non-essential** amino acid synthesized from pyruvate and other amino acids, and its synthesis is not impaired in PKU.
- It plays a role in **gluconeogenesis** but is not directly related to the metabolic defect in PKU.
*Glutamate*
- **Glutamate** is a **non-essential** amino acid, crucial for neurotransmission and protein synthesis, and is not affected by PKU.
- It can be synthesized from various metabolic intermediates, and its status is not altered in patients with PKU.
*Phenylalanine*
- **Phenylalanine** is an **essential amino acid** that becomes **toxic** when accumulated due to PKU, making it necessary to restrict it in the diet.
- It is the precursor to **tyrosine**, but its inability to be metabolized is the core problem in PKU, not a nutritional essentiality related to the disease.
*Cysteine*
- **Cysteine** is a **conditionally essential** amino acid, often synthesized from methionine, and its synthesis is not directly impacted by PKU.
- While potentially essential in certain conditions, it is not the primary amino acid that becomes essential due to the specific enzymatic defect in PKU.
Amino acid metabolism US Medical PG Question 5: A 4-day-old male newborn delivered at 39 weeks' gestation is evaluated because of poor feeding, recurrent vomiting, and lethargy. Physical examination shows tachypnea with subcostal retractions. An enzyme assay performed on a liver biopsy specimen shows decreased activity of carbamoyl phosphate synthetase I. This enzyme plays an important role in the breakdown and excretion of amino groups that result from protein digestion. Which of the following is an immediate substrate for the synthesis of the molecule needed for the excretion of amino groups?
- A. N-acetylglutamate
- B. Homocysteine
- C. Phenylalanine
- D. Valine
- E. Aspartate (Correct Answer)
Amino acid metabolism Explanation: ***Aspartate***
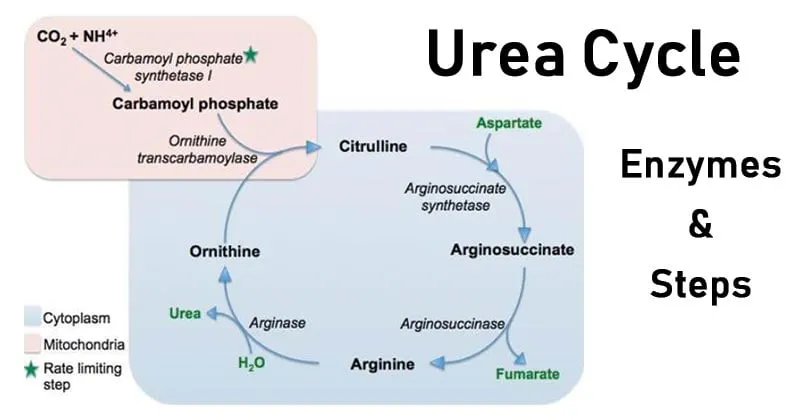
- The question describes a case of **carbamoyl phosphate synthetase I (CPS I)** deficiency, which leads to **hyperammonemia** due to impaired urea cycle function.
- The urea cycle is responsible for excreting **amino groups** as urea; one of the key molecules directly incorporated into the urea molecule is **aspartate**, which donates an amino group to form **argininosuccinate**.
*N-acetylglutamate*
- **N-acetylglutamate** is an essential activator of **carbamoyl phosphate synthetase I (CPS I)**, the enzyme deficient in this patient.
- While crucial for the urea cycle's regulation, it is an **allosteric activator** rather than a direct substrate for the synthesis of molecules needed for amino group excretion.
*Homocysteine*
- **Homocysteine** is an intermediate in **methionine metabolism** and is primarily associated with cardiovascular disease and neurological issues when elevated.
- It plays no direct role as a substrate in the urea cycle for the excretion of amino groups.
*Phenylalanine*
- **Phenylalanine** is an **essential amino acid** that is a precursor to tyrosine and neurotransmitters.
- Its metabolism is separate from the urea cycle, and it is not a direct substrate for ammonia excretion in this pathway.
*Valine*
- **Valine** is a **branched-chain amino acid (BCAA)** primarily catabolized in muscles and used for energy.
- It is not a direct substrate in the urea cycle, which processes nitrogen from various amino acids into urea for excretion.
Amino acid metabolism US Medical PG Question 6: A 2-day-old male infant is brought to the emergency department by ambulance after his parents noticed that he was convulsing and unresponsive. He was born at home and appeared well initially; however, within 24 hours he became increasingly irritable and lethargic. Furthermore, he stopped feeding and began to experience worsening tachypnea. This continued for about 6 hours, at which point his parents noticed the convulsions and called for an ambulance. Laboratories are obtained with the following results:
Orotic acid: 9.2 mmol/mol creatinine (normal: 1.4-5.3 mmol/mol creatinine)
Ammonia: 135 µmol/L (normal: < 50 µmol/L)
Citrulline: 2 µmol/L (normal: 10-45 µmol/L)
Which of the following treatments would most likely be beneficial to this patient?
- A. Galactose avoidance
- B. Aspartame avoidance
- C. Benzoate administration (Correct Answer)
- D. Uridine administration
- E. Fructose avoidance
Amino acid metabolism Explanation: ***Benzoate administration***
- This patient presents with hyperammonemia (135 µmol/L), elevated orotic acid (9.2 mmol/mol creatinine), and **low citrulline (2 µmol/L)**, which is the classic triad for **ornithine transcarbamylase (OTC) deficiency**.
- The low citrulline distinguishes OTC deficiency from other urea cycle defects, while elevated orotic acid results from accumulation of carbamoyl phosphate that gets shunted into pyrimidine synthesis.
- **Sodium benzoate** is a nitrogen scavenger that conjugates with glycine to form hippurate, which is excreted renally, providing an alternative pathway for nitrogen disposal and reducing toxic ammonia levels.
- This is a life-saving acute treatment for hyperammonemia in urea cycle disorders.
*Galactose avoidance*
- This is the treatment for **galactosemia**, a disorder of galactose metabolism caused by galactose-1-phosphate uridyltransferase deficiency.
- Galactosemia presents with hepatomegaly, jaundice, cataracts, intellectual disability, and hypoglycemia after milk feeding.
- The patient's hyperammonemia and elevated orotic acid pattern is incompatible with galactosemia.
*Aspartame avoidance*
- This is relevant for **phenylketonuria (PKU)** dietary management, as aspartame contains phenylalanine.
- PKU presents with developmental delay, intellectual disability, musty odor, and eczema, with elevated phenylalanine levels.
- Ammonia and orotic acid are normal in PKU, making this diagnosis inconsistent with the lab findings.
*Uridine administration*
- **Uridine** treats **hereditary orotic aciduria** (UMP synthase deficiency), which presents with megaloblastic anemia, growth retardation, and developmental delays.
- While orotic acid is elevated in both conditions, hereditary orotic aciduria has **normal ammonia** and the primary pathology is impaired pyrimidine synthesis, not ammonia disposal.
- This patient's life-threatening hyperammonemia requires immediate nitrogen scavenging, which uridine does not provide.
*Fructose avoidance*
- This treats **hereditary fructose intolerance** (aldolase B deficiency), which causes hypoglycemia, vomiting, hepatomegaly, and jaundice after fructose ingestion.
- The presentation is triggered by dietary fructose exposure and does not cause hyperammonemia or elevated orotic acid.
- The patient's metabolic profile is inconsistent with a fructose metabolism disorder.
Amino acid metabolism US Medical PG Question 7: A 29-year-old female presents to the family physician concerned over the blue-black discoloration of her sclera and skin. She notes that at the end of her day, there are black stains in her underwear. The incomplete breakdown of which of the following amino acids is responsible for this presentation?
- A. Leucine
- B. Valine
- C. Tyrosine (Correct Answer)
- D. Methionine
- E. Isoleucine
Amino acid metabolism Explanation: ***Tyrosine***
- The symptoms described (blue-black **scleral and skin discoloration**, and dark urine staining underwear) are classic for **alkaptonuria**.
- Alkaptonuria results from a deficiency of **homogentisate oxidase**, an enzyme in the catabolic pathway of **tyrosine**, which leads to the accumulation of **homogentisic acid**.
*Leucine*
- Leucine is a **branched-chain amino acid**; disorders in its metabolism are typically associated with conditions like **Maple Syrup Urine Disease**.
- **Maple Syrup Urine Disease** presents with neurological symptoms, poor feeding, and a characteristic odor, not blue-black discoloration.
*Valine*
- Valine is another **branched-chain amino acid**, and its metabolic defects are also associated with conditions like **Maple Syrup Urine Disease**.
- Its accumulation does not lead to the specific pigmentary changes seen in alkaptonuria.
*Methionine*
- Methionine metabolism disorders include conditions such as **homocystinuria**.
- **Homocystinuria** is characterized by skeletal abnormalities, ocular problems, and intellectual disability, not blue-black discoloration.
*Isoleucine*
- Isoleucine is the third **branched-chain amino acid** and is also implicated in **Maple Syrup Urine Disease** when its metabolism is impaired.
- Clinical features of isoleucine metabolism defects do not include the blue-black pigmentation described.
Amino acid metabolism US Medical PG Question 8: On a medical trip to Nicaragua, you observe a sweet odor in the cerumen of a 12-hour-old female newborn. Within 48 hours, the newborn develops ketonuria, poor feeding, and a sweet odor is also noticed in the urine. By 96 hours, the newborn is extremely lethargic and opisthotonus is observed. In order to prevent a coma and subsequent death, which of the following amino acids is one of those that should be withheld from this newborn's diet?
- A. Methionine
- B. Valine (Correct Answer)
- C. Phenylalanine
- D. Threonine
- E. Tyrosine
Amino acid metabolism Explanation: ***Valine***
- The clinical presentation with a **sweet odor in cerumen** and urine, followed by **ketonuria**, poor feeding, lethargy, and opisthotonus, is highly characteristic of **Maple Syrup Urine Disease (MSUD)**.
- MSUD is an autosomal recessive disorder caused by a deficiency in the **branched-chain alpha-keto acid dehydrogenase complex (BCKDC)**, which is responsible for the metabolism of the branched-chain amino acids (BCAAs): **leucine, isoleucine, and valine**. Therefore, restricting these amino acids from the diet is crucial.
*Methionine*
- **Methionine** is an essential amino acid, but its dietary restriction is primarily associated with conditions like **homocystinuria**, not MSUD.
- The deficiency in MSUD specifically impacts the branched-chain amino acid pathway, not the methionine metabolism pathway.
*Phenylalanine*
- **Phenylalanine** is restricted in the diet of individuals with **phenylketonuria (PKU)**, a different inborn error of metabolism.
- PKU is characterized by the inability to metabolize phenylalanine to tyrosine, leading to its accumulation and neurotoxicity, with different clinical features than described.
*Threonine*
- **Threonine** is a different essential amino acid and is not one of the branched-chain amino acids whose catabolism is impaired in MSUD.
- Restricting threonine would not directly address the metabolic defect seen in MSUD.
*Tyrosine*
- **Tyrosine** is a non-essential amino acid that becomes essential in conditions like **phenylketonuria (PKU)**, where it cannot be synthesized from phenylalanine.
- It is not directly implicated in the pathogenesis or dietary management of MSUD.
Amino acid metabolism US Medical PG Question 9: A 4-day-old boy is brought to the physician because of somnolence, poor feeding, and vomiting after his first few breast feedings. He appears lethargic. His respiratory rate is 73/min. Serum ammonia is markedly increased. Genetic analysis shows deficiency in N-acetylglutamate synthase. The activity of which of the following enzymes is most likely directly affected by this genetic defect?
- A. Ornithine translocase
- B. Carbamoyl phosphate synthetase I (Correct Answer)
- C. Argininosuccinase
- D. Argininosuccinate synthetase
- E. Arginase
Amino acid metabolism Explanation: ***Carbamoyl phosphate synthetase I***
- **N-acetylglutamate** (NAG) is an essential allosteric activator of **carbamoyl phosphate synthetase I (CPS I)**, the rate-limiting enzyme of the urea cycle.
- A deficiency in **N-acetylglutamate synthase** directly leads to a lack of NAG, significantly impairing CPS I activity and causing severe hyperammonemia.
*Ornithine translocase*
- This enzyme is responsible for transporting **ornithine** into the mitochondria for the urea cycle.
- While a defect in **ornithine translocase** also causes hyperammonemia, it is due to accumulation of ornithine and upstream substrates, not a defect in N-acetylglutamate synthase.
*Argininosuccinase*
- Also known as **argininosuccinate lyase**, this enzyme cleaves argininosuccinate into arginine and fumarate.
- A deficiency would lead to accumulation of **argininosuccinate**, and while it is a urea cycle disorder, it is not directly affected by N-acetylglutamate synthase deficiency.
*Argininosuccinate synthetase*
- This enzyme catalyzes the condensation of **citrulline** and **aspartate** to form argininosuccinate.
- A defect in **argininosuccinate synthetase** causes citrullinemia but is not directly regulated by N-acetylglutamate.
*Arginase*
- **Arginase** is the final enzyme in the urea cycle, hydrolyzing arginine to form urea and ornithine.
- A deficiency would lead to hyperargininemia, which typically presents later in childhood and is not directly affected by N-acetylglutamate.
Amino acid metabolism US Medical PG Question 10: A 5 year old child was brought to the physician with a history of black urine. There is no history of fever or any other complaints. There is no growth retardation and all the developmental milestones are normal. The child is suspected to have an enzyme defect for metabolism of an aromatic amino acid. What is the enzyme deficient
- A. Homogentisate dehydrogenase
- B. Homogentistae oxidase (Correct Answer)
- C. Tyrosine Transaminase
- D. Tryptophan Hydroxylase
- E. Phenylalanine Hydroxylase
Amino acid metabolism Explanation: ***Homogentistae oxidase***
- The presentation of a child with **black urine** (alkaptonuria) in the absence of other symptoms is characteristic of a deficiency in **homogentisate oxidase**.
- This enzyme is crucial in the catabolism of **tyrosine**, and its deficiency leads to the accumulation of **homogentisic acid**, which oxidizes upon exposure to air, turning urine black.
*Homogentisate dehydrogenase*
- This enzyme is not a recognized component of the **tyrosine degradation pathway** in humans.
- The correct enzyme involved in the breakdown of **homogentisate** is an oxidase, not a dehydrogenase, in this context.
*Tyrosine Transaminase*
- A deficiency in **tyrosine transaminase** (tyrosinemia type II) would lead to elevated tyrosine levels and typically presents with symptoms affecting the eyes, skin, and intellectual disability, not primarily black urine.
- This condition is characterized by **ocular findings** (corneal ulcers), **skin lesions**, and **neurological symptoms**.
*Tryptophan Hydroxylase*
- This enzyme is involved in the synthesis of **serotonin** and **melatonin** from tryptophan, a different amino acid pathway.
- A deficiency or abnormality in **tryptophan hydroxylase** would not cause black urine but could lead to neurological or mood disorders.
*Phenylalanine Hydroxylase*
- A deficiency in **phenylalanine hydroxylase** causes **phenylketonuria (PKU)**, which affects phenylalanine metabolism, not tyrosine metabolism directly.
- PKU typically presents with **intellectual disability**, **musty odor**, **fair skin**, and **seizures** if untreated, not black urine.
More Amino acid metabolism US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.