Alcohol metabolism US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Alcohol metabolism. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Alcohol metabolism US Medical PG Question 1: A 72-year-old man presents to the emergency department with a 1 hour history of bruising and bleeding. He says that he fell and scraped his knee on the ground. Since then, he has been unable to stop the bleeding and has developed extensive bruising around the area. He has a history of gastroesophageal reflux disease, hypertension, and atrial fibrillation for which he is taking an oral medication. He says that he recently started taking omeprazole for reflux. Which of the following processes is most likely inhibited in this patient?
- A. Sulfation
- B. Oxidation (Correct Answer)
- C. Filtration
- D. Acetylation
- E. Glucuronidation
Alcohol metabolism Explanation: ***Oxidation***
- The patient is taking **omeprazole**, a proton pump inhibitor, which is a known **CYP450 inhibitor**.
- Since the patient is also on an **oral anticoagulant** for atrial fibrillation, inhibition of CYP450 enzymes can reduce the metabolism of the anticoagulant, leading to **increased anticoagulant effect** and subsequent bleeding and bruising.
*Sulfation*
- **Sulfation** is a phase II metabolic reaction that converts compounds into more polar and excretable forms, but omeprazole primarily affects phase I metabolism involving CYP450 enzymes.
- While sulfation can be important for the metabolism of some drugs, it is not the primary process inhibited by omeprazole to cause increased bleeding with oral anticoagulants.
*Filtration*
- **Filtration** is a renal process and not a metabolic enzyme pathway affected by omeprazole.
- Omeprazole's interaction with anticoagulants mainly occurs through hepatic metabolism, not renal filtration.
*Acetylation*
- **Acetylation** is a phase II metabolic reaction, primarily carried out by **N-acetyltransferases**.
- Omeprazole is primarily known to interact with **CYP450 enzymes** (phase I metabolism) rather than N-acetyltransferases.
*Glucuronidation*
- **Glucuronidation** is a phase II metabolic reaction involving **UGT enzymes** that typically inactivates and increases the excretion of drugs.
- While important for drug metabolism, omeprazole's primary drug interactions leading to increased anticoagulant effects are via **CYP450 inhibition** (phase I metabolism), not directly through glucuronidation.
Alcohol metabolism US Medical PG Question 2: A 45-year-old man is brought to the emergency department by ambulance after vomiting blood. The patient reports that he only ate a small snack the morning before and had not eaten anything for over 24 hours. At the hospital, the patient is stabilized. He is admitted to a surgical floor and placed on NPO with a nasogastric tube set to intermittent suction. He has been previously diagnosed with liver cirrhosis. An esophagogastroduodenoscopy (EGD) has been planned for the next afternoon. At the time of endoscopy, some pathways were generating glucose to maintain serum glucose levels. Which of the following enzymes catalyzes the irreversible biochemical reaction of this process?
- A. Glucose-6-phosphate dehydrogenase
- B. Glycogen phosphorylase
- C. Enolase
- D. Glyceraldehyde-3-phosphate dehydrogenase
- E. Fructose-1,6-bisphosphatase (Correct Answer)
Alcohol metabolism Explanation: ***Fructose-1,6-bisphosphatase***
- The scenario describes a patient in a fasting state for over 24 hours, during which **gluconeogenesis** is crucial for maintaining blood glucose levels.
- **Fructose-1,6-bisphosphatase** is one of the key regulatory enzymes in gluconeogenesis, catalyzing an **irreversible reaction** that bypasses the phosphofructokinase-1 step of glycolysis.
*Glucose-6-phosphate dehydrogenase*
- This enzyme is involved in the **pentose phosphate pathway**, which generates NADPH and precursors for nucleotide synthesis.
- It does not directly participate in gluconeogenesis to produce glucose from non-carbohydrate sources.
*Glycogen phosphorylase*
- This enzyme is involved in **glycogenolysis**, the breakdown of glycogen into glucose-1-phosphate.
- While it releases glucose, the body's glycogen stores would likely be depleted after over 24 hours of fasting, making gluconeogenesis the primary pathway for glucose production.
*Enolase*
- Enolase is an enzyme in the glycolytic pathway, catalyzing the reversible conversion of 2-phosphoglycerate to phosphoenolpyruvate.
- It is not an enzyme of gluconeogenesis, nor does it catalyze an irreversible step in the glucose production process during fasting.
*Glyceraldehyde-3-phosphate dehydrogenase*
- This enzyme is also part of glycolysis, catalyzing the reversible oxidation and phosphorylation of glyceraldehyde-3-phosphate to 1,3-bisphosphoglycerate.
- Like enolase, it is not an irreversible enzyme in gluconeogenesis that would be generating glucose under fasting conditions.
Alcohol metabolism US Medical PG Question 3: A 55-year-old man presents to his primary care physician for a wellness checkup. The patient has a past medical history of alcohol abuse and is currently attending alcoholics anonymous with little success. He is currently drinking roughly 1L of hard alcohol every day and does not take his disulfiram anymore. Which of the following findings is most likely to also be found in this patient?
- A. Dysdiadochokinesia (Correct Answer)
- B. Microcytic anemia
- C. Constipation
- D. Decreased CNS NMDA activity
- E. Increased transketolase activity
Alcohol metabolism Explanation: ***Dysdiadochokinesia***
- Chronic **alcohol abuse** can lead to cerebellar degeneration, a condition characterized by damage to the **cerebellum**.
- **Dysdiadochokinesia**, the impaired ability to perform rapidly alternating movements, is a classic sign of **cerebellar dysfunction**.
*Microcytic anemia*
- **Chronic alcohol abuse** typically causes **macrocytic anemia** due to folate deficiency, or less commonly, iron deficiency anemia from gastrointestinal bleeding.
- **Microcytic anemia** is usually associated with **iron deficiency** (often due to chronic blood loss) or **thalassemia**, neither of which are suggested here.
*Constipation*
- While various factors can cause constipation, **chronic alcohol abuse** is more commonly associated with **diarrhea** due to alterations in gut motility and malabsorption.
- Constipation is not a direct or prominent feature of **alcoholism**.
*Decreased CNS NMDA activity*
- **Chronic alcohol abuse** leads to an **upregulation of NMDA receptors** in the brain as a compensatory mechanism against alcohol's inhibitory effects on the central nervous system.
- When alcohol consumption ceases, this upregulated NMDA activity contributes to the **excitatory symptoms of alcohol withdrawal**, such as seizures and delirium tremens.
*Increased transketolase activity*
- **Transketolase activity** is usually **decreased** in chronic alcoholics due to **thiamine deficiency**, as thiamine (vitamin B1) is a critical cofactor for this enzyme.
- A **decrease** in transketolase activity is a key diagnostic indicator for thiamine deficiency, which contributes to conditions like **Wernicke-Korsakoff syndrome**.
Alcohol metabolism US Medical PG Question 4: A 65-year-old homeless man with a history of hospitalization for alcohol intoxication is brought in confused. His serum glucose is 39mg/dl. Which of the following best explains his hypoglycemia?
- A. He has decreased activity of alcohol dehydrogenase
- B. Hepatic gluconeogenesis is elevated
- C. His hepatic NADH/NAD+ ratio is high (Correct Answer)
- D. He has also been using cocaine
- E. His hepatic glycogen stores are depleted
Alcohol metabolism Explanation: ***His hepatic NADH/NAD+ ratio is high***
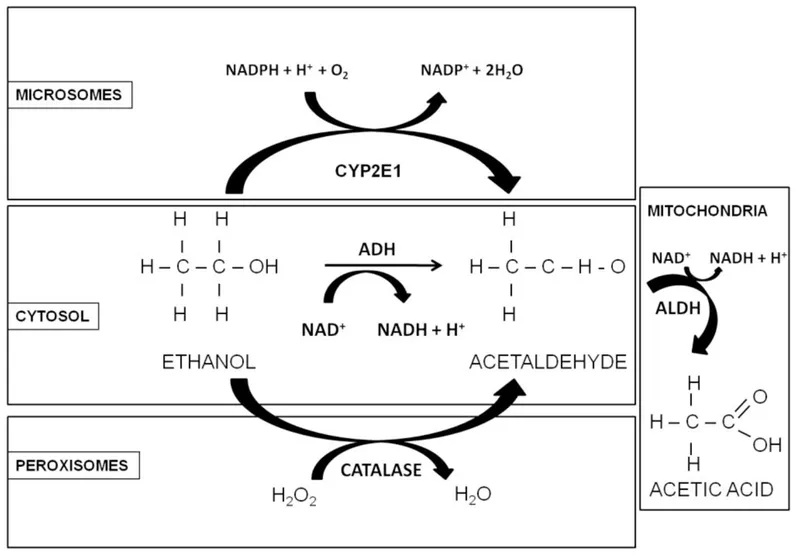
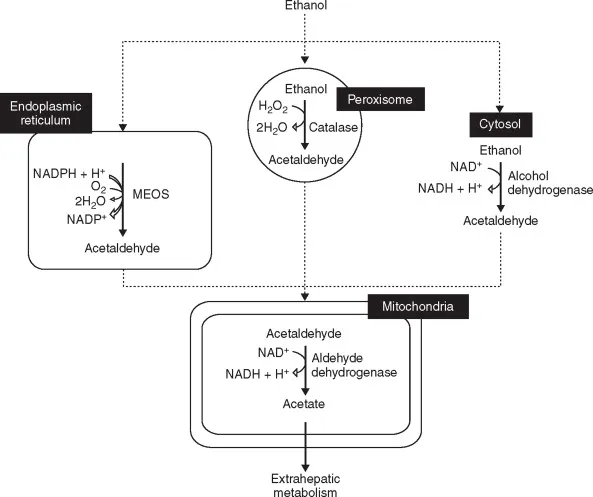
- **Ethanol metabolism** by **alcohol dehydrogenase** and **aldehyde dehydrogenase** generates a large amount of **NADH**, significantly increasing the hepatic NADH/NAD+ ratio.
- This high NADH/NAD+ ratio inhibits several key enzymes in **gluconeogenesis** (e.g., pyruvate carboxylase, malate dehydrogenase), leading to **hypoglycemia** in malnourished individuals, especially after alcohol consumption.
*He has decreased activity of alcohol dehydrogenase*
- **Decreased alcohol dehydrogenase activity** would lead to a slower metabolism of alcohol, potentially prolonging its effects but not directly causing severe hypoglycemia in this manner.
- Individuals with decreased activity metabolize alcohol less efficiently, typically resulting in a **delayed rise in NADH** and potentially less severe metabolic derangements related to ethanol.
*Hepatic gluconeogenesis is elevated*
- The elevated **NADH/NAD+ ratio** due to alcohol metabolism actually **inhibits hepatic gluconeogenesis**, rather than elevating it.
- This **inhibition** contributes to the observed **hypoglycemia**, especially in a patient with likely **depleted glycogen stores** due to malnourishment or chronic alcohol use.
*He has also been using cocaine*
- While possible, the clinical picture of **confusion** and **hypoglycemia** in a chronic alcoholic is most directly explained by the metabolic effects of alcohol itself, particularly its impact on **glucose metabolism**.
- **Cocaine use** would typically present with different symptoms such as **tachycardia**, **hypertension**, or agitation, and is not the most likely explanation for severe hypoglycemia.
*His hepatic glycogen stores are depleted*
- While it is very likely that a homeless, alcoholic individual would have **depleted hepatic glycogen stores** due to poor nutrition, this option alone does not fully explain the **acute hypoglycemia** precipitated by alcohol.
- The combination of **depleted glycogen** and **inhibited gluconeogenesis** (due to the high NADH/NAD+ ratio) is what leads to severe hypoglycemia in this scenario.
Alcohol metabolism US Medical PG Question 5: A 35-year-old woman presents to the emergency department after ingesting approximately 50 tablets of acetaminophen 4 hours ago in a suicide attempt. Her acetaminophen level is 200 µg/mL. Which of the following best describes the mechanism of toxicity in this case?
- A. Depletion of glutathione stores (Correct Answer)
- B. Blockade of calcium channels
- C. Direct cellular necrosis
- D. Inhibition of cytochrome oxidase
Alcohol metabolism Explanation: ***Depletion of glutathione stores***
- In acetaminophen overdose, the normal metabolic pathways become saturated, leading to the accumulation of a toxic metabolite called **N-acetyl-p-benzoquinone imine (NAPQI)**.
- **NAPQI** is normally detoxified by conjugation with **glutathione**, but in overdose, glutathione stores are depleted, allowing NAPQI to bind covalently to hepatocyte macromolecules, causing damage.
*Blockade of calcium channels*
- This mechanism is characteristic of **calcium channel blocker toxicity**, leading to cardiovascular depression (bradycardia, hypotension) and is not relevant to acetaminophen overdose.
- Acetaminophen toxicity primarily affects the liver via a different pathway, not directly interfering with calcium channels.
*Direct cellular necrosis*
- While acetaminophen overdose ultimately leads to **hepatocellular necrosis**, this is the *result* of the toxicity, not the primary mechanism by which the drug initiates cellular damage.
- The necrosis is mediated by the accumulation of the toxic metabolite **NAPQI** and the subsequent oxidative stress and cellular injury, not by direct cellular destruction without prior steps.
*Inhibition of cytochrome oxidase*
- This mechanism is associated with toxins like **cyanide** and **carbon monoxide**, which impair mitochondrial respiration and cellular energy production.
- Acetaminophen toxicity does not directly involve the inhibition of cytochrome oxidase as its primary mechanism of hepatotoxicity.
Alcohol metabolism US Medical PG Question 6: A 45-year-old female with a history of gastroesophageal reflux disease presents to her family physician with symptoms of epigastric pain right after a meal. The physician performs a urea breath test which is positive and the patient is started on appropriate medical therapy. Three days later at a restaurant, she experienced severe flushing, tachycardia, hypotension, and vomiting after her first glass of wine. Which of the following is the mechanism of action of the medication causing this side effect?
- A. Binds to the 30S ribosomal subunit preventing attachment of the aminoacyl-tRNA
- B. Blocks protein synthesis by binding to the 50S ribosomal subunit inhibiting protein translocation
- C. Blocks the synthesis of the peptidoglycan layer
- D. Inhibits the H+/K+ ATPase
- E. Forms toxic metabolites that damage bacterial DNA (Correct Answer)
Alcohol metabolism Explanation: ***Forms toxic metabolites that damage bacterial DNA***
- The patient likely has a **_H. pylori_ infection** causing epigastric pain, diagnosed by a **positive urea breath test**.
- **Metronidazole**, a common treatment for _H. pylori_, causes a **disulfiram-like reaction** with alcohol, leading to flushing, tachycardia, hypotension, and vomiting. Metronidazole's mechanism involves forming **toxic free radicals** that damage bacterial DNA.
*Binds to the 30S ribosomal subunit preventing attachment of the aminoacyl-tRNA*
- This is the mechanism of action for **tetracyclines** (e.g., doxycycline) and **aminoglycosides** (e.g., gentamicin), which are sometimes used in _H. pylori_ regimens but do not typically cause this severe alcohol interaction.
- While tetracyclines are part of some _H. pylori_ treatment regimens, they are not primarily associated with a disulfiram-like reaction.
*Blocks protein synthesis by binding to the 50S ribosomal subunit inhibiting protein translocation*
- This describes the mechanism of action of **macrolide antibiotics** (e.g., clarithromycin), which are commonly used in _H. pylori_ treatment protocols.
- Although clarithromycin can cause gastrointestinal upset, it does not typically induce the severe disulfiram-like reaction described with alcohol.
*Blocks the synthesis of the peptidoglycan layer*
- This is the mechanism of action of **beta-lactam antibiotics** (e.g., amoxicillin), frequently included in _H. pylori_ eradication regimens.
- Amoxicillin does not cause a disulfiram-like reaction when combined with alcohol.
*Inhibits the H+/K+ ATPase*
- This describes **proton pump inhibitors (PPIs)** like omeprazole or pantoprazole, which are part of nearly all _H. pylori_ treatment regimens to reduce acid production.
- PPIs do not have a direct interaction with alcohol that causes this specific constellation of symptoms; their primary role is acid suppression, not antibacterial action leading to disulfiram effects.
Alcohol metabolism US Medical PG Question 7: A 20-year-old male is brought by ambulance to the emergency room in extremis. He is minimally conscious, hypotensive, and tachypneic, and his breath gives off a "fruity" odor. An arterial blood gas and metabolic panel show anion gap metabolic acidosis. This patient is most likely deficient in which of the following metabolic actions?
- A. Glucagon production
- B. Cortisol secretion
- C. Formation of ketone bodies
- D. Glucose production
- E. Cellular uptake of glucose (Correct Answer)
Alcohol metabolism Explanation: ***Cellular uptake of glucose***
- The patient's symptoms, including **fruity odor breath**, **anion gap metabolic acidosis**, and being found in extremis, are classic signs of **diabetic ketoacidosis (DKA)**.
- DKA results from a profound lack of **insulin**, which is essential for cells (especially muscle and adipose tissue) to take up glucose from the bloodstream, leading to hyperglycemia and a shift to fat metabolism.
*Glucagon production*
- **Glucagon** is a counter-regulatory hormone that *raises* blood glucose levels, and its production is often *increased* in DKA as the body attempts to provide fuel to cells in the absence of insulin's effect.
- A deficiency in glucagon production would more likely lead to **hypoglycemia**, not the profound hyperglycemia seen in DKA.
*Cortisol secretion*
- **Cortisol** is another counter-regulatory hormone that *increases* blood glucose, and its secretion is typically *elevated* in stress states like DKA.
- A deficiency in cortisol (e.g., in adrenal insufficiency) would present with different symptoms such as **hypoglycemia**, **hyponatremia**, and **hyperkalemia**, without the classic DKA picture.
*Formation of ketone bodies*
- The patient's **fruity odor breath** and **anion gap metabolic acidosis** are direct consequences of the *overproduction* of **ketone bodies**.
- This overproduction occurs when the body, lacking glucose for fuel due to insulin deficiency, switches to **fat metabolism**, leading to excessive formation of acetoacetate, beta-hydroxybutyrate, and acetone.
*Glucose production*
- **Glucose production** (gluconeogenesis and glycogenolysis) is typically *increased* in DKA as the liver tries to supply glucose to the body due to perceived cellular starvation (despite high blood glucose).
- A deficiency in glucose production, such as in certain glycogen storage diseases or severe liver failure, would lead to **hypoglycemia**, not the hyperglycemia characteristic of DKA.
Alcohol metabolism US Medical PG Question 8: A 60-year-old man is rushed to the emergency room after he was found unconscious in bed that afternoon. The patient’s wife says he has been confused and irritable for the past several days. She says he has a history of chronic daily alcohol abuse and has been hospitalized multiple times with similar symptoms His temperature is 37°C (98.6°F), the blood pressure is 110/80 mm Hg, the pulse is 90/min, and the respiratory rate is 14/min. On physical examination, the patient is minimally responsive to painful stimuli. His abdomen is distended with positive shifting dullness. Laboratory results are as follows:
Complete blood count
Hematocrit 35%
Platelets 100,000/mm3
White blood cells 5000/mm3
Liver function studies
Serum Albumin 2 g/dL
Alkaline phosphatase (ALP) 200 IU/L
Aspartate aminotransferase (AST) 106 IU/L
Alanine aminotransferase (ALT) 56 IU/L
The patient is admitted to the hospital and started on the appropriate treatment to improve his mental status. Which of the following best describes the mechanism of action of the drug that is most likely used to treat this patient’s symptoms?
- A. Prevents the conversion of ammonia into ammonium
- B. Increases ammonia production and absorption
- C. Increases pH in the gastrointestinal lumen
- D. Decreases pH in the gastrointestinal lumen (Correct Answer)
- E. Decreases the colonic concentration of bacteria
Alcohol metabolism Explanation: ***Decreases pH in the gastrointestinal lumen***
- The patient's presentation with altered mental status, chronic alcohol abuse, distended abdomen with shifting dullness (*ascites*), and abnormal liver function tests (low *albumin*, elevated *AST/ALT*) is highly suggestive of **hepatic encephalopathy**.
- **Lactulose** is the mainstay treatment for hepatic encephalopathy, and its mechanism involves lowering the colonic pH, which converts ammonia (NH3) into poorly absorbed ammonium (NH4+), thereby reducing systemic ammonia levels.
*Prevents the conversion of ammonia into ammonium*
- This statement is incorrect; the goal of treatment for hepatic encephalopathy is to **promote** the conversion of ammonia to ammonium to prevent its absorption.
- Ammonia (NH3) is lipophilic and readily crosses the blood-brain barrier, while ammonium (NH4+) is hydrophilic and poorly absorbed from the gut.
*Increases ammonia production and absorption*
- This is incorrect and would exacerbate hepatic encephalopathy by increasing the toxic ammonia load.
- The primary aim of treatment is to **reduce** ammonia production and enhance its excretion or conversion into a non-absorbable form.
*Increases pH in the gastrointestinal lumen*
- Elevating the pH in the colon would favor the production of **ammonia (NH3)** from ammonium (NH4+), leading to increased systemic ammonia absorption and worsening hepatic encephalopathy.
- Therefore, this mechanism would be detrimental to a patient with hepatic encephalopathy.
*Decreases the colonic concentration of bacteria*
- While **rifaximin** (a non-absorbable antibiotic) does decrease ammonia-producing bacteria in the gut and is used in conjunction with lactulose, this option describes the mechanism of an antibiotic, not the primary action of lactulose.
- Lactulose itself does not primarily decrease the overall concentration of gut bacteria, but rather modifies the *metabolic activity* of the existing bacteria.
Alcohol metabolism US Medical PG Question 9: A 38-year-old man presents to his physician with double vision persisting for a week. When he enters the exam room, the physician notes that the patient has a broad-based gait. The man’s wife informs the doctor that he has been an alcoholic for the last 5 years and his consumption of alcohol has increased significantly over the past few months. She also reports that he has become indifferent to his family members over time and is frequently agitated. She also says that his memory has been affected significantly, and when asked about a particular detail, he often recollects it incorrectly, though he insists that his version is the true one. On physical examination, his vital signs are stable, but when the doctor asks him where he is, he seems to be confused. His neurological examination also shows nystagmus. Which of the following options describes the earliest change in the pathophysiology of the central nervous system in this man?
- A. Increased astrocyte lactate
- B. Increased extracellular concentration of glutamate
- C. Increased fragmentation of deoxyribonucleic acid within the neurons
- D. Breakdown of the blood-brain barrier
- E. Decreased α-ketoglutarate dehydrogenase activity in astrocytes (Correct Answer)
Alcohol metabolism Explanation: ***Decreased α-ketoglutarate dehydrogenase activity in astrocytes***
- Chronic **alcoholism** leads to **thiamine deficiency**, which impairs the activity of **α-ketoglutarate dehydrogenase** in the **Krebs cycle**.
- This enzyme is crucial for **neuronal energy metabolism** and its deficiency contributes to the earliest **neuropathological changes** observed in Wernicke-Korsakoff syndrome.
*Increased astrocyte lactate*
- While chronic alcoholism and thiamine deficiency can lead to metabolic dysfunction, increased **astrocyte lactate** is typically a response to **hypoxia** or **ischemia**, not the primary initiating event of thiamine deficiency.
- Lactate accumulation can be a downstream effect of impaired glucose metabolism, but not the earliest or most direct consequence of **α-ketoglutarate dehydrogenase** inhibition.
*Increased extracellular concentration of glutamate*
- **Glutamate excitotoxicity** can occur in chronic alcoholism, particularly during withdrawal, leading to neuronal damage.
- However, the primary insult in Wernicke-Korsakoff syndrome, which this patient's symptoms suggest, is **thiamine deficiency**, impacting the **Krebs cycle** before widespread glutamate release.
*Increased fragmentation of deoxyribonucleic acid within the neurons*
- **DNA fragmentation** indicates significant **neuronal damage** and **apoptosis**, which are later consequences of prolonged metabolic stress and oxidative injury.
- It is not the earliest pathophysiological change but rather a result of the progression of metabolic dysfunction caused by **thiamine deficiency**.
*Breakdown of the blood-brain barrier*
- **Blood-brain barrier (BBB) disruption** can occur in various neurological conditions, including chronic alcoholism, leading to inflammation and edema.
- While BBB dysfunction might contribute to the pathology, the initial and most direct effect of thiamine deficiency is on **cellular energy metabolism** within neurons and astrocytes, preceding widespread BBB breakdown.
Alcohol metabolism US Medical PG Question 10: A 4-year-old boy presents to the ophthalmologist for a down- and inward dislocation of the lens in his left eye. On physical exam, the boy has a marfanoid habitus and intellectual disability. Biochemical tests were performed to locate the exact defect in this boy. It was found that there was a significant deficiency in cystathionine beta-synthase activity with elevated homocysteine levels. Which of the following is the diagnosis?
- A. Marfan syndrome
- B. Homocystinuria (Correct Answer)
- C. Alkaptonuria
- D. Phenylketonuria
- E. Maple syrup urine disease
Alcohol metabolism Explanation: ***Homocystinuria***
- The combination of **ectopia lentis** (lens dislocation), **marfanoid habitus**, and **intellectual disability** is characteristic of homocystinuria.
- The **deficiency in cystathionine beta-synthase** leading to **elevated homocysteine levels** is the biochemical hallmark of this disorder.
*Marfan syndrome*
- While it presents with **marfanoid habitus** and **ectopia lentis**, the lens dislocation is typically **upward and outward**, unlike the down- and inward dislocation seen here.
- Marfan syndrome is caused by a defect in **fibrillin-1**, and biochemical tests would not show elevated homocysteine.
*Alkaptonuria*
- This disorder is characterized by **dark urine** upon standing, **ochronosis** (darkening of cartilage and connective tissue), and **arthropathy**.
- It results from a deficiency in **homogentisate oxidase** and does not present with lens dislocation or intellectual disability.
*Phenylketonuria*
- PKU is caused by a deficiency in **phenylalanine hydroxylase**, leading to an accumulation of phenylalanine.
- It primarily causes **severe intellectual disability**, seizures, and a musty odor, but not ectopia lentis or marfanoid habitus.
*Maple syrup urine disease*
- This is a metabolic disorder affecting the metabolism of **branched-chain amino acids** (leucine, isoleucine, valine).
- It presents with a characteristic **maple syrup odor** in urine, poor feeding, lethargy, and developmental delay, but not the specific features seen in this case.
More Alcohol metabolism US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.