Oligosaccharidoses US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Oligosaccharidoses. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Oligosaccharidoses US Medical PG Question 1: An 18-month-old girl is brought to the pediatrician’s office for failure to thrive and developmental delay. The patient’s mother says she has not started speaking and is just now starting to pull herself up to standing position. Furthermore, her movement appears to be restricted. Physical examination reveals coarse facial features and restricted joint mobility. Laboratory studies show increased plasma levels of several enzymes. Which of the following is the underlying biochemical defect in this patient?
- A. Congenital lack of lysosomal formation
- B. Inappropriate protein targeting to endoplasmic reticulum
- C. Failure of mannose phosphorylation (Correct Answer)
- D. Inappropriate degradation of lysosomal enzymes
- E. Misfolding of nuclear proteins
Oligosaccharidoses Explanation: ***Failure of mannose phosphorylation***
- The constellation of **failure to thrive**, **developmental delay**, **coarse facial features**, restricted joint mobility, and elevated plasma enzymes in an 18-month-old girl is highly suggestive of **I-cell disease** (mucolipidosis type II).
- **I-cell disease** is caused by the deficiency of **N-acetylglucosaminyl-1-phosphotransferase**, an enzyme responsible for phosphorylating mannose residues on lysosomal enzymes, which is crucial for proper targeting to the lysosome.
*Congenital lack of lysosomal formation*
- **Lysosomes** are present in this condition, but their enzymes are misdirected.
- A congenital lack of lysosomal formation would present with even more severe and widespread cellular dysfunction, possibly incompatible with life beyond early embryonic stages.
*Inappropriate protein targeting to endoplasmic reticulum*
- Proteins destined for the endoplasmic reticulum (ER) are typically targeted by an N-terminal signal peptide and then processed within the ER.
- While ER dysfunction can cause various disorders, the specific symptoms and enzyme elevations point away from a primary ER targeting defect related to lysosomal enzymes.
*Inappropriate degradation of lysosomal enzymes*
- In I-cell disease, lysosomal enzymes are synthesized but are **not properly targeted to the lysosomes**; instead, they are secreted into the bloodstream, leading to their elevated plasma levels.
- While some degradation might occur, the primary issue is mis-packaging and secretion, not increased degradation within the cell.
*Misfolding of nuclear proteins*
- Misfolding of nuclear proteins can lead to a variety of genetic disorders and cellular stress responses, but the clinical presentation, particularly the accumulation of undegraded material and elevated plasma lysosomal enzymes, is not characteristic of primary nuclear protein misfolding.
- The pathology in I-cell disease centers on lysosomal dysfunction rather than nuclear protein abnormalities.
Oligosaccharidoses US Medical PG Question 2: A 15-year-old boy is sent from gym class with a chief complaint of severe muscle aches. In class today he was competing with his friends and therefore engaged in weightlifting for the first time. A few hours later he was extremely sore and found that his urine was red when he went to urinate. This concerned him and he was sent to the emergency department for evaluation.
Upon further questioning, you learn that since childhood he has always had muscle cramps with exercise. Physical exam was unremarkable. Upon testing, his creatine kinase level was elevated and his urinalysis was negative for blood and positive for myoglobin.
Thinking back to biochemistry you suspect that he may be suffering from a hereditary glycogen disorder. Given this suspicion, what would you expect to find upon examination of his cells?
- A. Normal glycogen structure (Correct Answer)
- B. Short outer glycogen chains
- C. Accumulation of glycogen in lysosomes forming dense granules
- D. Glycogen without normal branching pattern
- E. Absence of glycogen in muscles
Oligosaccharidoses Explanation: ***Normal glycogen structure***
- The patient's symptoms (exercise-induced muscle cramps, myoglobinuria, and elevated CK) are classic for **McArdle disease** (Glycogen Storage Disease Type V), caused by a deficiency in **muscle glycogen phosphorylase**.
- In McArdle disease, the enzyme responsible for breaking down glycogen (glycogen phosphorylase) is deficient, but the enzymes involved in synthesizing glycogen are normal. Therefore, the **structure of glycogen is normal**, but it accumulates in muscle cells because it cannot be catabolized.
*Short outer glycogen chains*
- **Short outer glycogen chains** are characteristic of **Cori disease** (Glycogen Storage Disease Type III), caused by a deficiency in **debranching enzyme**.
- This condition also presents with hypoglycemia and hepatomegaly, which are not described in the patient's presentation.
*Accumulation of glycogen in lysosomes forming dense granules*
- **Accumulation of glycogen in lysosomes** and the formation of **dense granules** is characteristic of **Pompe disease** (Glycogen Storage Disease Type II), caused by a deficiency in **lysosomal alpha-glucosidase (acid maltase)**.
- Pompe disease typically presents as a severe infantile form with cardiomegaly and hypotonia, or a later-onset form with proximal muscle weakness, which differs from the patient's primary complaint of exercise intolerance and myoglobinuria.
*Glycogen without normal branching pattern*
- **Glycogen without a normal branching pattern** (very long unbranched chains) is characteristic of **Andersen disease** (Glycogen Storage Disease Type IV), caused by a deficiency in **branching enzyme**.
- This condition typically leads to cirrhosis and liver failure in infancy, which is not consistent with the patient's presentation.
*Absence of glycogen in muscles*
- While McArdle disease involves an inability to break down muscle glycogen, it does not result in the **absence of glycogen** in muscles; rather, there is an **over-accumulation** of normal-structured glycogen because it cannot be utilized.
- The defect is in **glycogenolysis**, not glycogen synthesis, so glycogen is formed but not broken down.
Oligosaccharidoses US Medical PG Question 3: A newborn undergoing the standard screening tests is found to have a positive test for reducing sugars. Further testing is performed and reveals that the patient does not have galactosemia, but rather is given a diagnosis of fructosuria. What levels of enzymatic activity are altered in this patient?
- A. Hexokinase decreased; fructokinase decreased
- B. Hexokinase unchanged; fructokinase unchanged
- C. Hexokinase increased; fructokinase increased
- D. Hexokinase increased; fructokinase decreased
- E. Hexokinase unchanged; fructokinase decreased (Correct Answer)
Oligosaccharidoses Explanation: ***Hexokinase unchanged; fructokinase decreased***
- **Essential fructosuria** is caused by a deficiency in **fructokinase**, the enzyme responsible for the first step of fructose metabolism (fructose → fructose-1-phosphate).
- This results in **decreased or absent fructokinase activity**, leading to fructose accumulation in blood and urine (positive reducing sugar test).
- **Hexokinase activity remains unchanged** - there is no upregulation or compensatory increase in hexokinase. The enzyme maintains its normal baseline activity.
- Essential fructosuria is a **benign, asymptomatic condition** with no metabolic stress, so no compensatory enzyme changes occur.
- The small amount of fructose that needs metabolism can be handled by normal baseline hexokinase activity (hexokinase has broad substrate specificity).
*Hexokinase decreased; fructokinase decreased*
- While **fructokinase is decreased** in essential fructosuria, hexokinase activity is not decreased.
- Hexokinase is a constitutively expressed glycolytic enzyme whose activity does not change in this benign condition.
*Hexokinase unchanged; fructokinase unchanged*
- This is incorrect because **fructokinase activity is specifically decreased** in essential fructosuria, which is the defining enzymatic defect of the condition.
- The decreased fructokinase activity causes fructose to accumulate and appear in the urine.
*Hexokinase increased; fructokinase increased*
- **Fructokinase is decreased, not increased** - an increase would prevent the fructose accumulation characteristic of this condition.
- Hexokinase activity does not increase as essential fructosuria causes no metabolic stress requiring compensation.
*Hexokinase increased; fructokinase decreased*
- While **fructokinase is decreased** in essential fructosuria, hexokinase activity does not increase.
- This is a benign condition with no compensatory enzyme upregulation - hexokinase maintains normal baseline activity levels.
Oligosaccharidoses US Medical PG Question 4: A deficiency in which of the following lysosomal enzymes is inherited in a pattern similar to a deficiency of iduronate sulfatase (Hunter syndrome)?
- A. Sphingomyelinase
- B. Glucocerebrosidase
- C. Galactocerebrosidase
- D. Alpha-L-iduronidase
- E. Alpha-galactosidase A (Correct Answer)
Oligosaccharidoses Explanation: ***Alpha-galactosidase A***
- A deficiency in **alpha-galactosidase A** causes **Fabry disease**, which, like Hunter syndrome (iduronate sulfatase deficiency), is inherited in an **X-linked recessive** pattern.
- Both conditions primarily affect males, with carrier females potentially exhibiting milder symptoms.
*Sphingomyelinase*
- A deficiency in sphingomyelinase leads to **Niemann-Pick disease types A and B**, which are inherited in an **autosomal recessive** pattern.
- This mode of inheritance differs from the X-linked pattern of Hunter syndrome.
*Glucocerebrosidase*
- A deficiency in glucocerebrosidase causes **Gaucher disease**, inherited in an **autosomal recessive** pattern.
- This is a common lysosomal storage disorder, but its inheritance pattern is distinct from X-linked disorders.
*Galactocerebrosidase*
- A deficiency in galactocerebrosidase causes **Krabbe disease (globoid cell leukodystrophy)**, which is inherited in an **autosomal recessive** pattern.
- Krabbe disease is a severe neurodegenerative disorder, but its genetic transmission is not X-linked.
*Alpha-L-iduronidase*
- A deficiency in **alpha-L-iduronidase** causes **Hurler syndrome (MPS I)**, which is inherited in an **autosomal recessive** pattern.
- While both Hunter and Hurler syndromes are mucopolysaccharidoses, their genetic inheritance patterns are different.
Oligosaccharidoses US Medical PG Question 5: A 22-year-old man presents to the physician due to a progressively worsening weakness and an increasingly large abdomen. He notes that he eats well and is fairly active; however, his abdomen has become increasingly protuberant. He also complains of easy bruisability. His medical history is not significant and he takes no medications. Physical examination reveals hepatomegaly and splenomegaly. Several bruises can be seen on the inside of his arms and legs. His skin has a yellowish tinge to it. Laboratory testing shows the following:
Hematocrit 25%
Erythrocyte count 2.5 x 106/mm3
Thrombocyte count 25,000/mm3
A bone marrow biopsy shows a crinkled-paper appearance to the macrophages. Which of the following enzymes is most likely deficient in this patient?
- A. Arylsulfatase A
- B. Sphingomyelinase
- C. α-galactosidase
- D. Hexosaminidase
- E. β-glucosidase (Correct Answer)
Oligosaccharidoses Explanation: ***β-glucosidase***
- The patient's symptoms (hepatosplenomegaly, easy bruisability, anemia, thrombocytopenia) and the characteristic **crinkled-paper appearance of macrophages** on bone marrow biopsy are pathognomonic for **Gaucher disease**.
- **Gaucher disease** is an autosomal recessive lysosomal storage disorder caused by a deficiency of the enzyme **β-glucosidase** (also known as glucocerebrosidase), leading to the accumulation of glucocerebroside.
*Arylsulfatase A*
- Deficiency of **arylsulfatase A** causes **metachromatic leukodystrophy**, characterized by progressive demyelination and neurological symptoms, not the hematological and visceral findings seen here.
- While it is also a lysosomal storage disorder, the clinical presentation and specific cell morphology are distinct.
*Sphingomyelinase*
- Deficiency of **sphingomyelinase** leads to **Niemann-Pick disease**, which shares some features with Gaucher disease, such as hepatosplenomegaly.
- However, the characteristic cell found in Niemann-Pick disease is a lipid-laden macrophage with a **foamy appearance**, not a "crinkled-paper" appearance.
*α-galactosidase*
- Deficiency of **α-galactosidase A** causes **Fabry disease**, an X-linked lysosomal storage disorder.
- Symptoms include episodic pain, acroparesthesias, angiokeratomas, and renal/cardiac involvement, which are not described in this patient.
*Hexosaminidase*
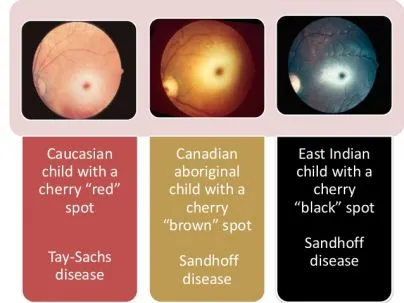
- Deficiency of **hexosaminidase A** causes **Tay-Sachs disease**, a lysosomal storage disorder primarily affecting the central nervous system.
- It is characterized by progressive neurodegeneration, developmental delay, and a **cherry-red spot** on the retina, without the hepatosplenomegaly or characteristic macrophages seen in this case.
Oligosaccharidoses US Medical PG Question 6: A pathologist receives a patient sample for analysis. Cells in the sample are first labeled with fluorescent antibodies and then passed across a laser beam in a single file of particles. The light scatter and fluorescent intensity of the particles are plotted on a graph; this information is used to characterize the sample. This laboratory method would be most useful to establish the diagnosis of a patient with which of the following?
- A. Ventricular septal defect and facial dysmorphism with low T-lymphocyte count
- B. Painless generalized lymphadenopathy with monomorphic cells and interspersed benign histiocytes on histology
- C. Pancytopenia and deep vein thrombosis with intermittent hemoglobinuria (Correct Answer)
- D. Multiple opportunistic infections with decreased CD4 counts
- E. Vesicular lesions with dermatomal distribution and dendritic corneal ulcers
Oligosaccharidoses Explanation: ***Pancytopenia and deep vein thrombosis with intermittent hemoglobinuria***
- The described laboratory method is **flow cytometry**, which is the **gold standard for diagnosing paroxysmal nocturnal hemoglobinuria (PNH)** by detecting the absence of **CD55** and **CD59** on red blood cells due to impaired GPI anchor synthesis.
- PNH classically presents with **pancytopenia**, **hemolytic anemia** (leading to hemoglobinuria), and a high risk of **thrombosis** (e.g., deep vein thrombosis).
*Ventricular septal defect and facial dysmorphism with low T-lymphocyte count*
- This clinical picture suggests **DiGeorge syndrome**, which involves a developmental defect of the **third and fourth pharyngeal pouches**, leading to thymic hypoplasia and **T-cell deficiency**.
- While flow cytometry is used to quantify T-lymphocyte subsets (e.g., CD3, CD4, CD8), the primary method for diagnosing DiGeorge syndrome is **fluorescent in situ hybridization (FISH)** for a **22q11 deletion**, making it less ideal for flow cytometry diagnosis.
*Painless generalized lymphadenopathy with monomorphic cells and interspersed benign histiocytes on histology*
- This description with "**monomorphic cells**" is more consistent with certain **non-Hodgkin lymphomas** (e.g., Burkitt lymphoma) rather than Hodgkin lymphoma, which typically shows a **polymorphic** cellular infiltrate.
- While flow cytometry can be useful in characterizing lymphomas by identifying cell surface markers, the diagnosis is primarily established by **lymph node biopsy and histopathology** with **immunohistochemistry**, making flow cytometry a supplementary rather than primary diagnostic tool.
*Multiple opportunistic infections with decreased CD4 counts*
- This presentation is highly suggestive of **HIV infection leading to AIDS**. The "decreased CD4 counts" are a key diagnostic and prognostic marker.
- While flow cytometry is used to **monitor CD4 cell counts** in HIV patients, the initial diagnosis of HIV is established via **antibody/antigen combination tests** and confirmed by **Western blot** or **PCR for viral load**, not by flow cytometry.
*Vesicular lesions with dermatomal distribution and dendritic corneal ulcers*
- This clinical presentation points to **herpes zoster ophthalmicus** (shingles affecting the eye due to **varicella-zoster virus** reactivation).
- Diagnosis is primarily **clinical** based on the characteristic rash and eye findings, although **PCR** of vesicular fluid can confirm VZV infection. Flow cytometry has no role in this diagnosis.
Oligosaccharidoses US Medical PG Question 7: A 3-month-old boy presents for routine health maintenance. The patient has coarse facial features and stiff joint movements with restricted passive and active range of motion. He also has problems following objects with his eyes and seems not to focus on anything. On physical examination, the corneas are clouded, and the patient fails to meet any 3-month developmental milestones. Genetic testing and histopathology are performed and reveal failure of a cellular structure to phosphorylate mannose residues on glycoproteins. An electron microscopy image of one of this patient’s cells is shown. Which of the following is the most likely diagnosis in this patient?
- A. Adrenoleukodystrophy
- B. Kartagener syndrome
- C. Tay-Sachs disease
- D. Inclusion cell disease (Correct Answer)
- E. Diamond-Blackfan anemia
Oligosaccharidoses Explanation: ***Inclusion cell disease***
- This condition is characterized by a **failure to phosphorylate mannose residues** on glycoproteins due to a defective **N-acetylglucosaminyl-1-phosphotransferase** enzyme.
- The clinical presentation of **coarse facial features, stiff joint movements**, clouded corneas, and developmental delay is classical for **I-cell disease** (mucolipidosis II), where lysosomal enzymes are **mistargeted and secreted from cells** instead of being properly delivered to lysosomes, resulting in **lysosomes that lack hydrolytic enzymes** and accumulate undigested substrates (visible as inclusions on electron microscopy).
*Adrenoleukodystrophy*
- This is an **X-linked disorder** affecting very long chain fatty acid metabolism, leading to their accumulation in the **adrenal glands** and **white matter of the brain**.
- While it causes **neurological dysfunction** and adrenal insufficiency, it does not typically present with the coarse facial features, corneal clouding, and skeletal abnormalities seen in this patient.
*Kartagener syndrome*
- This is a form of **primary ciliary dyskinesia** characterized by impaired ciliary movement due to structural defects in **dynein arms**.
- It presents with **recurrent respiratory infections** (sinusitis, bronchitis, bronchiectasis), **situs inversus** (in about 50% of cases), and infertility, which are unrelated to the patient's symptoms.
*Tay-Sachs disease*
- This is a **lysosomal storage disorder** caused by a deficiency of **hexosaminidase A**, leading to the accumulation of **GM2 ganglioside**.
- It causes **progressive neurological deterioration**, motor weakness, and a **cherry-red spot** on the macula, but not the coarse facial features or skeletal abnormalities described.
*Diamond-Blackfan anemia*
- This is a **congenital hypoplastic anemia** characterized by a defect in **erythroid progenitor cells**, leading to severe macrocytic anemia.
- It can be associated with various congenital anomalies, but the primary presentation is **anemia** and it does not involve the lysosomal storage defects or the characteristic facial and joint features seen in this case.
Oligosaccharidoses US Medical PG Question 8: An 8-month-old female infant from a first-degree consanguineous couple was brought to the physician because the mother noticed abnormalities in the growth of her child as well as the different lengths of her child's legs. The infant had gingival hyperplasia, restricted movement in both shoulders, a prominent, pointed forehead, and enophthalmos with a slight opacity in both corneas. A blood test revealed 10 fold higher than normal levels of the following enzymes: N-acetyl-ß-glucosaminidase, ß-glucuronidase, ß-hexosaminidase A, and alkaline phosphatase. Which of the following is most likely deficient in this patient?
- A. Lysosomal alpha-1,4-glucosidase
- B. Glucose-6-phosphate dehydrogenase
- C. N-acetyl-glucosamine-1-phosphotransferase (Correct Answer)
- D. Glucocerebrosidase
- E. Alpha-galactosidase A
Oligosaccharidoses Explanation: ***N-acetyl-glucosamine-1-phosphotransferase***
- The clinical presentation with **gingival hyperplasia**, **restricted joint movement**, **skeletal abnormalities** (growth abnormalities, leg length discrepancy, prominent forehead), and **corneal opacity** with elevated lysosomal enzymes (N-acetyl-ß-glucosaminidase, ß-glucuronidase, ß-hexosaminidase A) is highly characteristic of **I-cell disease** (mucolipidosis II).
- I-cell disease is caused by a deficiency in **N-acetyl-glucosamine-1-phosphotransferase**, an enzyme crucial for phosphorylating mannose residues on lysosomal enzymes, tagging them for delivery to lysosomes. Without this tag, lysosomal enzymes are secreted extracellularly, leading to their accumulation in the blood and their deficiency within lysosomes, causing the clinical features.
*Lysosomal alpha-1,4-glucosidase*
- Deficiency of **lysosomal alpha-1,4-glucosidase** causes **Pompe disease (glycogen storage disease type II)**, which is characterized by **cardiomegaly**, hypotonia, and liver involvement, but typically does not present with the skeletal dysplasias, gingival hyperplasia, or corneal clouding seen in this patient.
- While it is a lysosomal storage disorder, the specific clinical features and panel of elevated enzymes differ significantly from this case.
*Glucose-6-phosphate dehydrogenase*
- Deficiency of **glucose-6-phosphate dehydrogenase (G6PD)** causes **G6PD deficiency**, an X-linked disorder leading to **hemolytic anemia** in response to oxidative stress (e.g., fava beans, certain drugs, infections).
- It does not present with the systemic skeletal, connective tissue, and corneal abnormalities described, nor does it involve elevated lysosomal enzyme levels.
*Glucocerebrosidase*
- Deficiency of **glucocerebrosidase** causes **Gaucher disease**, which presents with **hepatosplenomegaly**, bone crises, pancytopenia, and sometimes neurological involvement.
- While it is a lysosomal storage disorder, the clinical features (e.g., absence of gingival hyperplasia, corneal opacity, or specific skeletal dysplasias like restricted joint movement) and the pattern of elevated enzymes do not match the patient's presentation.
*Alpha-galactosidase A*
- Deficiency of **alpha-galactosidase A** causes **Fabry disease**, an X-linked lysosomal storage disorder characterized by **neuropathic pain**, **angiokeratomas**, renal failure, and cardiac involvement.
- The clinical picture of Fabry disease does not include gingival hyperplasia, prominent skeletal abnormalities, or the specific pattern of elevated lysosomal enzymes observed in this patient.
Oligosaccharidoses US Medical PG Question 9: A 13-year-old girl is brought to the physician by her mother because of a 1-month history of abnormal movements of her muscles that she cannot control. She has a younger brother with cognitive disabilities and epilepsy. Examination shows frequent, brief, involuntary contractions of the muscle groups of the upper arms, legs, and face that can be triggered by touch. An EEG shows generalized epileptiform activity. A trichrome stain of a skeletal muscle biopsy specimen shows muscle fibers with peripheral red inclusions that disrupt the normal fiber contour. Which of the following is the most likely underlying mechanism of the patient's symptoms?
- A. CTG trinucleotide repeat expansion
- B. Mutation of the methyl-CpG binding protein 2 gene
- C. Truncated dystrophin protein
- D. Autoimmune endomysial destruction
- E. Defective oxidative phosphorylation (Correct Answer)
Oligosaccharidoses Explanation: ***Defective oxidative phosphorylation***
- The constellation of **uncontrolled muscle movements (myoclonus)**, **epilepsy**, and the brother's **cognitive disabilities** strongly suggests a **mitochondrial disorder**.
- **Ragged red fibers** on trichrome stain of skeletal muscle biopsy are pathognomonic for **mitochondrial myopathies**, indicating defective oxidative phosphorylation due to abnormal mitochondrial aggregates.
*CTG trinucleotide repeat expansion*
- This is characteristic of **Myotonic Dystrophy**, which primarily presents with **myotonia** (delayed muscle relaxation), progressive muscle weakness, and often cataracts, rather than prominent myoclonus and seizures.
- While muscle weakness can occur, the specific biopsy findings and prominent myoclonus point away from this diagnosis.
*Mutation of the methyl-CpG binding protein 2 gene*
- A mutation in the **MECP2 gene** causes **Rett Syndrome**, an X-linked dominant disorder seen almost exclusively in girls.
- It involves normal development for 6-18 months followed by regression, loss of purposeful hand movements, **stereotypical hand-wringing**, and microcephaly, which are not described here.
*Truncated dystrophin protein*
- A truncated dystrophin protein causes **Duchenne Muscular Dystrophy**, an X-linked recessive disorder leading to progressive muscle weakness, **Gowers' sign**, and elevated creatine kinase.
- This condition does not typically present with myoclonus or the characteristic ragged red fibers, nor does it typically involve the sibling's intellectual disability and epilepsy in this manner.
*Autoimmune endomysial destruction*
- This mechanism is characteristic of **celiac disease**, which can have neurological symptoms like ataxia or peripheral neuropathy, but not typically the severe myoclonus, epilepsy, or muscle biopsy findings seen here.
- **Inflammatory myopathies** like polymyositis may show endomysial inflammation, but the clinical picture and specific biopsy findings (ragged red fibers) are not consistent.
Oligosaccharidoses US Medical PG Question 10: A 22-year-old man comes to the physician because of a fall associated with a 6-month history of increasing difficulty walking. Over the last year, his friends have also noticed his speech becoming slower. During this period, he also gave up his hobby of playing video games because he has become clumsy with his hands. His father died of esophageal varices at the age of 40 years. The patient does not smoke or drink alcohol. He takes no medications. He appears sad. His temperature is 37°C (98.6°F), pulse is 70/min, and blood pressure is 120/80 mm Hg. He is alert and oriented to person, place, and time. His speech is slurred and monotonous; his gait is unsteady. Examination shows scleral icterus and some drooling. The liver is palpated 2 to 3 cm below the right costal margin, and the spleen is palpated 1 to 2 cm below the left costal margin. Further evaluation of this patient is most likely to show which of the following findings?
- A. Increased number of CAG repeats
- B. Oligoclonal bands on CSF analysis
- C. Low serum ceruloplasmin concentration (Correct Answer)
- D. Ventriculomegaly on CT scan of the brain
- E. Increased transferrin saturation
Oligosaccharidoses Explanation: ***Low serum ceruloplasmin concentration***
- This patient presents with a constellation of symptoms including neurological (difficulty walking, clumsy hands, slurred speech, unsteady gait), hepatic (father died of esophageal varices at an early age, hepatosplenomegaly, scleral icterus), and psychiatric (sadness, slurred and monotonous speech) manifestations, all suggestive of **Wilson's disease**.
- **Wilson's disease** is an autosomal recessive disorder of copper metabolism leading to copper accumulation in various organs, predominantly the **liver**, **brain**, and **cornea**. **Low serum ceruloplasmin** is a hallmark biochemical finding, as ceruloplasmin is a copper-carrying protein, and its synthesis or copper incorporation is defective.
*Increased number of CAG repeats*
- An increased number of **CAG trinucleotide repeats** is characteristic of **Huntington's disease**.
- While Huntington's disease causes neurological and psychiatric symptoms, it does not typically involve significant **liver disease** or scleral icterus, which are prominent features in this patient's presentation.
*Oligoclonal bands on CSF analysis*
- **Oligoclonal bands** in the **cerebrospinal fluid (CSF)** are a key diagnostic finding for **multiple sclerosis**.
- Multiple sclerosis presents with neurological deficits, but it does not account for the prominent liver involvement (scleral icterus, hepatosplenomegaly, family history of varices) seen in this case.
*Ventriculomegaly on CT scan of the brain*
- **Ventriculomegaly** on a CT scan of the brain can be seen in various conditions, including **hydrocephalus** or **cerebral atrophy**.
- While some neurological degenerative diseases can lead to cerebral atrophy and resulting ventriculomegaly, it's a non-specific finding and doesn't explain the patient's severe **hepatic involvement** with scleral icterus and hepatosplenomegaly.
*Increased transferrin saturation*
- **Increased transferrin saturation** is a laboratory finding indicative of **hemochromatosis**, a disorder of iron metabolism leading to iron overload.
- While hemochromatosis can cause liver disease and neurological symptoms, the combination of **scleral icterus**, the specific neurological presentation, and the strong family history of early liver disease in this context points much more strongly towards **Wilson's disease** rather than hemochromatosis.
More Oligosaccharidoses US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.