Phospholipid metabolism US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Phospholipid metabolism. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Phospholipid metabolism US Medical PG Question 1: A newborn infant is resuscitated and transferred to the neonatal intensive care unit. The infant has notable limb deformities as well as low-set ears and a flattened nose. He was born at 34 weeks gestation to a healthy mother who received regular obstetric follow-up. Resuscitation was notable for difficulty maintaining oxygenation in the newborn. Despite appropriate interventions, the infant is still struggling to maintain adequate oxygenation. Which of the following is most likely the cause of this patient's symptoms?
- A. PKD1 gene mutation
- B. Cystic dilation of the collecting ducts in the kidney (Correct Answer)
- C. Chromosomal abnormality
- D. Maternal diabetes
- E. Failure to administer betamethasone
Phospholipid metabolism Explanation: ***Cystic dilation of the collecting ducts in the kidney***
- This finding is characteristic of **autosomal recessive polycystic kidney disease (ARPKD)**, which leads to **Potter sequence/Potter syndrome**.
- **Potter sequence** results from severe **oligohydramnios** (often due to bilateral renal disease causing inadequate urine production), leading to:
- **Pulmonary hypoplasia** (lungs cannot expand properly without adequate amniotic fluid)
- **Characteristic facial features** (Potter facies): low-set ears, flattened nose, recessed chin
- **Limb deformities** (positional abnormalities from mechanical compression in utero)
- The **persistent difficulty maintaining oxygenation despite appropriate interventions** is the key clinical clue - this indicates **structural pulmonary hypoplasia**, not simply respiratory distress from prematurity or other causes that would respond to treatment.
- Potter sequence is the most likely diagnosis given this specific constellation of findings.
*Chromosomal abnormality*
- While **trisomy 18 (Edwards syndrome)** or **trisomy 13 (Patau syndrome)** can present with multiple congenital anomalies including facial dysmorphisms and limb deformities, they typically have additional characteristic findings (cardiac defects, rocker-bottom feet, holoprosencephaly, etc.).
- The **specific triad** of Potter facies + limb deformities + **refractory respiratory distress due to pulmonary hypoplasia** is pathognomonic for Potter sequence, not chromosomal abnormalities.
- Chromosomal abnormalities would not typically cause the severe oligohydramnios that leads to pulmonary hypoplasia.
*Maternal diabetes*
- Maternal diabetes can cause **macrosomia**, **hypoglycemia**, **respiratory distress syndrome (RDS)**, and rarely congenital anomalies (cardiac, neural tube defects).
- It does not cause the specific pattern of **Potter facies** (low-set ears, flattened nose) and **limb deformities** seen in Potter sequence.
- The mother is described as healthy with regular obstetric follow-up, making uncontrolled diabetes unlikely.
*PKD1 gene mutation*
- **PKD1 mutation** causes **autosomal dominant polycystic kidney disease (ADPKD)**, which typically presents in **adulthood** with hypertension, flank pain, and progressive renal failure.
- While rare severe cases can present in utero, PKD1 mutation does not cause the **cystic dilation of collecting ducts** - that finding is specific to **ARPKD** (associated with PKHD1 gene mutation).
- ADPKD involves cysts throughout the cortex and medulla, not specifically in collecting ducts.
*Failure to administer betamethasone*
- **Betamethasone** is given to mothers at risk of preterm delivery (before 34 weeks) to accelerate **fetal lung maturity** and reduce the severity of **respiratory distress syndrome (RDS)**.
- While this infant is preterm (34 weeks) and has respiratory distress, betamethasone failure would cause RDS due to **surfactant deficiency**, which typically **responds to surfactant administration and respiratory support**.
- This does not explain the **structural pulmonary hypoplasia** (indicated by refractory oxygenation issues) or the **facial and limb deformities**.
- Betamethasone is typically given before 34 weeks; at 34 weeks, the benefit is limited.
Phospholipid metabolism US Medical PG Question 2: An 18-month-old boy is brought to the physician because of a 2-day history of cough, fever, and lethargy. He has been admitted to the hospital twice during the past year for pneumonia. He can stand without support but has not started to walk. He speaks in bisyllables. He is at the 3rd percentile for height and 4th percentile for weight. Examination shows diffuse crackles over bilateral lung fields. Abdominal examination shows hepatosplenomegaly. Fundoscopy shows bright red macular spots. Despite being given appropriate antibiotic therapy, the patient dies. A photomicrograph of a section of the spleen obtained during autopsy is shown. Accumulation of which of the following substances is the most likely cause of this patient's condition?
- A. Ceramide trihexoside
- B. Cerebroside sulfate
- C. Glucocerebroside
- D. Sphingomyelin (Correct Answer)
- E. Limit dextrin
Phospholipid metabolism Explanation: ***Sphingomyelin***
- The patient's history of **recurrent pneumonia**, **hepatosplenomegaly**, **developmental delay** (not walking, bisyllables at 18 months), **failure to thrive**, and **cherry-red macular spots** (on fundoscopy) are classic signs of **Niemann-Pick disease**.
- **Niemann-Pick disease** is an autosomal recessive lysosomal storage disorder caused by a deficiency of the enzyme **acid sphingomyelinase**, leading to the accumulation of **sphingomyelin** in various tissues.
*Ceramide trihexoside*
- Accumulation of **ceramide trihexoside** is characteristic of **Fabry disease**, an X-linked recessive lysosomal storage disorder.
- While Fabry disease can cause renal failure, angiokeratomas, and peripheral neuropathy, it does not typically present with **hepatosplenomegaly**, **recurrent pneumonia**, or **cherry-red macular spots** in infancy.
*Cerebroside sulfate*
- Accumulation of **cerebroside sulfate** (sulfatide) is characteristic of **metachromatic leukodystrophy**, an autosomal recessive lysosomal storage disorder.
- This condition primarily affects the **nervous system**, leading to demyelination and neurological deterioration, but it does not present with **hepatosplenomegaly** or **cherry-red macula**.
*Glucocerebroside*
- Accumulation of **glucocerebroside** is characteristic of **Gaucher disease**, an autosomal recessive lysosomal storage disorder.
- While Gaucher disease causes **hepatosplenomegaly** and can lead to bone crises, it does not typically present with **cherry-red macular spots**, severe early developmental delay, or recurrent pulmonary infections in the same manner as Niemann-Pick.
*Limit dextrin*
- Accumulation of **limit dextrin** is associated with **Cori disease** (Type III glycogen storage disease).
- This disorder primarily affects the **liver** and **muscles**, causing hepatomegaly, hypoglycemia, and myopathy, but it does not present with **cherry-red macular spots** or specific developmental delays and recurrent infections seen in this patient.
Phospholipid metabolism US Medical PG Question 3: A 61-year-old woman comes to the physician because of a 6-month history of left knee pain and stiffness. Examination of the left knee shows tenderness to palpation along the joint line; there is crepitus with full flexion and extension. An x-ray of the knee shows osteophytes with joint-space narrowing. Arthrocentesis of the knee joint yields clear fluid with a leukocyte count of 120/mm3. Treatment with ibuprofen during the next week significantly improves her condition. The beneficial effect of this drug is most likely due to inhibition of which of the following?
- A. Conversion of hypoxanthine to urate
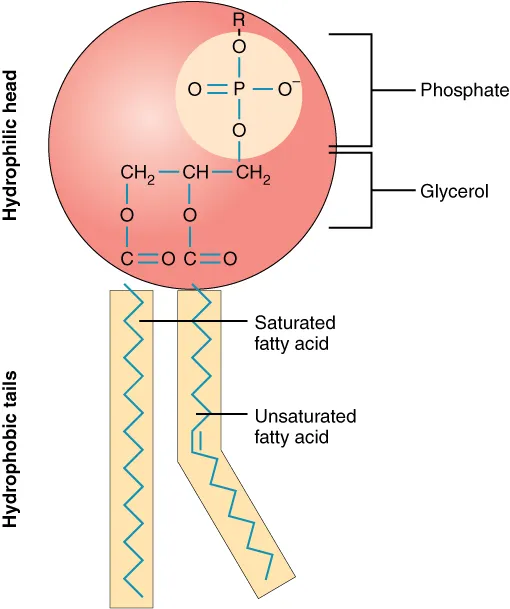
- B. Conversion of phospholipids to arachidonic acid
- C. Conversion of prostaglandin H2 to thromboxane A2
- D. Conversion of arachidonic acid to prostaglandin G2 (Correct Answer)
- E. Conversion of dihydroorotate to orotate
Phospholipid metabolism Explanation: ***Conversion of arachidonic acid to prostaglandin G2***
- This patient presents with symptoms and signs consistent with **osteoarthritis**, characterized by joint pain, stiffness, crepitus, and radiographic findings like **osteophytes** and **joint-space narrowing**.
- **Ibuprofen is a non-selective NSAID** that inhibits **cyclooxygenase (COX-1 and COX-2) enzymes**, which catalyze the conversion of **arachidonic acid to prostaglandin G2 (PGG2)**, the first committed step in prostaglandin synthesis.
- By blocking prostaglandin production, ibuprofen reduces inflammation and pain associated with osteoarthritis.
*Conversion of hypoxanthine to urate*
- This process is catalyzed by **xanthine oxidase** and is inhibited by medications like **allopurinol**, used in the treatment of **gout** to reduce uric acid levels.
- Gout typically presents with acute, severe joint pain with signs of inflammation and monosodium urate crystals on joint aspiration, which are not characteristic of this patient's presentation.
*Conversion of phospholipids to arachidonic acid*
- This step is catalyzed by **phospholipase A2**, which is inhibited by **glucocorticoids** (via lipocortin induction).
- While glucocorticoids have potent anti-inflammatory effects by working upstream of the arachidonic acid cascade, ibuprofen has a different mechanism targeting the COX enzymes downstream.
*Conversion of prostaglandin H2 to thromboxane A2*
- This reaction is catalyzed by **thromboxane synthase**, primarily important in platelet aggregation and vasoconstriction.
- NSAIDs like ibuprofen do not specifically inhibit thromboxane synthase; rather, they inhibit COX enzymes upstream, which reduces production of both prostaglandins and thromboxanes.
- Low-dose aspirin preferentially inhibits COX-1 in platelets, reducing thromboxane A2 for cardioprotection, but this is not ibuprofen's primary therapeutic mechanism in osteoarthritis.
*Conversion of dihydroorotate to orotate*
- This is a step in **pyrimidine synthesis**, inhibited by **leflunomide**, a disease-modifying antirheumatic drug (DMARD) used in rheumatoid arthritis.
- This mechanism is unrelated to the action of NSAIDs or the treatment of osteoarthritis.
Phospholipid metabolism US Medical PG Question 4: A 12-year-old boy is brought to the emergency department because of acute onset abdominal pain. On arrival, he also complains of nausea and shortness of breath in addition to epigastric pain. He has previously been admitted to the hospital several times for respiratory infections with Pseudomonas species and uses a nebulizer and a chest wall oscillation vest at home. The patient's acute condition is found to be due to premature activation of an enzyme that normally interacts with the brush border. Which of the following describes the activity of this enzyme?
- A. Activates pancreatic enzyme precursors (Correct Answer)
- B. Breaks down elastin molecules
- C. Hydrolyzes phospholipids
- D. Digests triglycerides
- E. Activates phospholipase A2
Phospholipid metabolism Explanation: ***Activates pancreatic enzyme precursors***
- The patient's history of **recurrent respiratory infections with Pseudomonas** and use of a **nebulizer/chest wall oscillation vest** strongly suggests **cystic fibrosis (CF)**.
- In cystic fibrosis, **thickened secretions** can obstruct the pancreatic ducts, leading to **autodigestion of the pancreas** due to obstruction preventing the release of pancreatic enzymes. The enzyme being referred to is **trypsin**, which, when prematurely activated, activates other pancreatic enzyme precursors, leading to **pancreatitis**.
*Breaks down elastin molecules*
- This activity is characteristic of **elastase**, an enzyme produced by the pancreas. While elastase is involved in the overall digestive process and can be prematurely activated, its primary role is not the one alluded to in the clinical presentation, which points to **pancreatitis** from premature activation of the cascade.
- Damage to elastin is more classically associated with conditions like **emphysema** (due to alpha-1 antitrypsin deficiency) rather than acute abdominal pain secondary to autodigestion.
*Hydrolyzes phospholipids*
- This is the function of **phospholipase**, another pancreatic enzyme. While also capable of contributing to pancreatic autodigestion if prematurely activated, it is typically activated by **trypsin**, making trypsin the primary enzyme responsible for initiating the cascade of activation.
- **Phospholipase A2** acts on phospholipids, but the question describes an enzyme that *normally interacts with the brush border* before activation of the precursors begins.
*Digests triglycerides*
- This is the function of **pancreatic lipase**. Premature activation of lipase can contribute to the fat necrosis seen in pancreatitis.
- However, lipase, like many other pancreatic enzymes, is activated by **trypsin**, which is the initial enzyme in the cascade of activation leading to autodigestion.
*Activates phospholipase A2*
- This describes the action of **trypsinogen turning into trypsin**, which then activates other proenzymes like **prophospholipase A2**.
- While correct that trypsin activates phospholipase A2, the question asks about the primary enzyme whose *premature activation* causes the issue, which is **trypsin** itself, as it activates *multiple* pancreatic enzyme precursors, initiating a cascade.
Phospholipid metabolism US Medical PG Question 5: A P2G1 diabetic woman is at risk of delivering at 29 weeks gestation. Her obstetrician counsels her that there is a risk the baby could have significant pulmonary distress after it is born. However, she states she will give the mother corticosteroids, which will help prevent this from occurring. Additionally, the obstetrician states she will perform a test on the amniotic fluid which will indicate the likelihood of the infant being affected by this syndrome. Which of the following ratios would be most predictive of the infant having pulmonary distress?
- A. lecithin:phosphatidylserine < 1.5
- B. lecithin:sphingomyelin < 1.5 (Correct Answer)
- C. lecithin:sphingomyelin > 1.5
- D. lecithin:phosphatidylserine > 3.0
- E. lecithin:sphingomyelin > 3.0
Phospholipid metabolism Explanation: ***lecithin:sphingomyelin < 1.5***
- A lecithin:sphingomyelin (L:S) ratio less than 2:1 (or 1.5 in some clinical contexts) indicates **fetal lung immaturity** and a **high risk for respiratory distress syndrome (RDS)**.
- The **lecithin level increases** significantly in the amniotic fluid during the third trimester as fetal lungs mature, while **sphingomyelin levels remain relatively constant**.
*lecithin:phosphatidylserine < 1.5*
- While **phosphatidylserine** is a component of surfactant, the **Lecithin:Sphingomyelin (L:S) ratio** is the established and most commonly used marker for fetal lung maturity.
- There is **no widely recognized or clinically validated threshold** for a lecithin:phosphatidylserine ratio in predicting respiratory distress syndrome.
*lecithin:sphingomyelin > 1.5*
- An L:S ratio **greater than 2:1 (or 1.5, in some labs)** generally indicates **fetal lung maturity** and a low risk for respiratory distress syndrome.
- Therefore, this ratio would suggest a **lower likelihood of pulmonary distress**, which contradicts the aim of identifying risk.
*lecithin:phosphatidylserine > 3.0*
- As with an L:S ratio, a higher ratio would generally indicate **lung maturity**, not increased risk for pulmonary distress.
- There is **no clinical standard for lecithin:phosphatidylserine ratio** to assess lung maturity for preventing RDS.
*lecithin:sphingomyelin > 3.0*
- An L:S ratio of **greater than 2:1 (or 3.0 in certain clinical scenarios)** is a strong indicator of **fetal lung maturity**, meaning the risk of respiratory distress syndrome is low.
- The question asks for a ratio that would be **predictive of pulmonary distress**, whereas this ratio indicates the opposite.
Phospholipid metabolism US Medical PG Question 6: A P1G0 diabetic woman is at risk of delivering at 30 weeks gestation. Her obstetrician counsels her that there is a risk the baby could have significant pulmonary distress after it is born. However, she states she will administer a drug to the mother to help prevent this from occurring. By what action will this drug prevent respiratory distress in the premature infant?
- A. Increasing the secretory product of type II alveolar cells (Correct Answer)
- B. Promoting increased surface tension of alveoli
- C. Suppressing the neonatal immune system
- D. Preventing infection of immature lungs
- E. Reducing the secretory product of type II alveolar cells
Phospholipid metabolism Explanation: ***Increasing the secretory product of type II alveolar cells***
- The drug administered is likely a **corticosteroid**, which **accelerates fetal lung maturation** by stimulating the production and release of **surfactant** from **type II alveolar cells**.
- **Surfactant** is crucial for reducing surface tension within the alveoli, preventing their collapse and ensuring proper lung function in premature infants.
*Promoting increased surface tension of alveoli*
- This option is incorrect because premature infants suffer from **respiratory distress syndrome (RDS)** due to **insufficient surfactant**, which leads to **high surface tension** and alveolar collapse.
- The goal of treatment is to **reduce surface tension**, not increase it.
*Suppressing the neonatal immune system*
- While corticosteroids do have **immunosuppressive effects**, this is not the primary mechanism by which they prevent **respiratory distress syndrome (RDS)** in premature infants.
- The main goal in this context is lung maturation, not immune modulation.
*Preventing infection of immature lungs*
- Although premature infants are susceptible to infections, the primary purpose of administering corticosteroids in this scenario is to promote **lung maturation** and prevent **respiratory distress syndrome (RDS)** due to **surfactant deficiency**, not to directly prevent infection.
- Antibiotics would be used for infection prevention or treatment.
*Reducing the secretory product of type II alveolar cells*
- This statement is incorrect because the problem in premature infants is a **deficiency of surfactant**, the secretory product of **type II alveolar cells**.
- The treatment aims to **increase** this secretory product to facilitate lung function.
Phospholipid metabolism US Medical PG Question 7: Steroid hormone synthesis, lipid synthesis, and chemical detoxification are activities of which of the following?
- A. Peroxisomes
- B. Nucleolus
- C. Rough Endoplasmic Reticulum
- D. Smooth Endoplasmic Reticulum (Correct Answer)
- E. Golgi bodies
Phospholipid metabolism Explanation: ***Smooth Endoplasmic Reticulum***
- The **smooth endoplasmic reticulum (SER)** is rich in enzymes that catalyze the synthesis of **lipids**, including steroid hormones, and is crucial for the detoxification of drugs and poisons, particularly in liver cells.
- Its tubular structure, devoid of ribosomes, differentiates its functions from the rough ER, focusing on metabolic processes like **calcium ion storage** and carbohydrate metabolism.
*Peroxisomes*
- Peroxisomes are primarily involved in the breakdown of **fatty acids** and amino acids, producing hydrogen peroxide as a byproduct.
- They also play a role in detoxification but are not the primary site for steroid hormone or general lipid synthesis.
*Nucleolus*
- The **nucleolus** is a dense structure within the nucleus responsible for synthesizing **ribosomal RNA (rRNA)** and assembling ribosomes.
- It has no direct role in steroid hormone synthesis, lipid metabolism, or chemical detoxification.
*Rough Endoplasmic Reticulum*
- The **rough endoplasmic reticulum (RER)** is studded with **ribosomes** and is primarily involved in the synthesis and modification of **proteins** destined for secretion or insertion into membranes.
- While it's part of the endomembrane system, it does not directly perform lipid synthesis or chemical detoxification as its main functions.
*Golgi bodies*
- **Golgi bodies (or Golgi apparatus)** are responsible for modifying, sorting, and packaging **proteins and lipids** synthesized in the ER into vesicles for secretion or delivery to other organelles.
- They do not perform the initial synthesis of steroid hormones or lipids, nor are they the primary site for chemical detoxification.
Phospholipid metabolism US Medical PG Question 8: A 16-year-old boy presents with shortness of breath after prolonged exposure to cold air during a recent hike with his friends. Past medical history is significant for asthma, untreated because he doesn't like using medications. The patient says he is a non-smoker and occasionally drinks alcohol. On physical examination, his temperature is 37.0°C (98.6°F), pulse rate is 120/min, blood pressure is 114/76 mm Hg, and respiratory rate is 32/min. Auscultation of the chest reveals bilateral wheezing. Nebulized ipratropium bromide results in significant clinical improvement. Which of the following second messenger systems is affected by this drug?
- A. Tyrosine kinase system
- B. Phosphoinositol system (Correct Answer)
- C. Arachidonic acid system
- D. Cyclic guanosine monophosphate (cGMP) system
- E. Cyclic adenosine monophosphate (cAMP) system
Phospholipid metabolism Explanation: ***Phosphoinositol system***
- **Ipratropium bromide** is an **anticholinergic drug** that blocks **muscarinic M3 receptors** on bronchial smooth muscle.
- M3 receptors are **Gq protein-coupled receptors** that activate the **phosphoinositol (PIP2) pathway**.
- When activated, Gq proteins stimulate **phospholipase C (PLC)**, which cleaves **PIP2** into **IP3** (inositol trisphosphate) and **DAG** (diacylglycerol).
- IP3 increases **intracellular calcium**, causing **bronchoconstriction**; ipratropium **blocks this pathway**, resulting in **bronchodilation**.
- This is the primary second messenger system affected by ipratropium.
*Cyclic adenosine monophosphate (cAMP) system*
- The **cAMP system** is associated with **β2-adrenergic receptors** (Gs-coupled), not muscarinic M3 receptors.
- **Beta-agonists** like albuterol work through cAMP to cause bronchodilation, but ipratropium does not directly affect this pathway.
- While there may be indirect effects, M3 receptors primarily signal through the phosphoinositol system, not cAMP.
*Tyrosine kinase system*
- The **tyrosine kinase system** is activated by **growth factors** (e.g., insulin, EGF, PDGF) through receptor tyrosine kinases.
- This pathway involves autophosphorylation and activation of downstream signaling cascades like **MAPK** and **PI3K/Akt**.
- Muscarinic receptors are **G protein-coupled receptors (GPCRs)**, not tyrosine kinase receptors.
*Arachidonic acid system*
- The **arachidonic acid pathway** produces **prostaglandins, leukotrienes**, and **thromboxanes** via **cyclooxygenase** and **lipoxygenase** enzymes.
- This system is targeted by **NSAIDs** (block COX) and **leukotriene modifiers** (e.g., montelukast), not by anticholinergics.
- While inflammation plays a role in asthma, ipratropium's mechanism does not primarily involve this pathway.
*Cyclic guanosine monophosphate (cGMP) system*
- The **cGMP system** is primarily associated with **nitric oxide (NO) signaling** and **atrial natriuretic peptide (ANP)**.
- NO activates **guanylyl cyclase**, increasing cGMP levels and causing **smooth muscle relaxation** and **vasodilation**.
- M3 muscarinic receptors do not primarily signal through the cGMP pathway.
Phospholipid metabolism US Medical PG Question 9: A 12-year-old boy is brought to the physician because of difficulty in walking for 5 months. His mother reports that he has trouble keeping his balance and walking without support. Over the past year, he has started to have difficulty seeing in the dark and his hearing has been impaired. Examination shows marked scaling of the skin on the face and feet and a shortened 4th toe. Muscle strength is 3/5 in the lower extremities and 4/5 in the upper extremities. Sensation to pinprick is symmetrically decreased over the legs. Fundoscopy shows peripheral pigment deposits and retinal atrophy. His serum phytanic acid concentration is markedly elevated. The patient's condition is most likely caused by a defect in which of the following cellular structures?
- A. Proteasomes
- B. Peroxisomes (Correct Answer)
- C. Smooth endoplasmic reticulum
- D. Mitochondria
- E. Myofilaments
Phospholipid metabolism Explanation: ***Peroxisomes***
- The constellation of symptoms including **difficulty walking and maintaining balance**, **impaired night vision and hearing**, **scaling skin**, **distal muscle weakness**, **ataxia**, **peripheral neuropathy**, **pigmentary retinopathy**, and **markedly elevated serum phytanic acid** is characteristic of **Refsum disease**.
- **Refsum disease** is an autosomal recessive disorder caused by a defect in **peroxisomal alpha-oxidation** (specifically phytanoyl-CoA hydroxylase deficiency), leading to the accumulation of phytanic acid in tissues.
- Phytanic acid is a branched-chain fatty acid derived from dietary sources (dairy products, ruminant fats) that cannot undergo beta-oxidation and requires alpha-oxidation in peroxisomes.
*Proteasomes*
- **Proteasomes** are responsible for the degradation of ubiquitinated proteins, important for cellular protein homeostasis.
- Defects in proteasomes are associated with various conditions like **neurodegenerative diseases** (e.g., Parkinson's), but not with the specific symptoms of phytanic acid accumulation.
*Smooth endoplasmic reticulum*
- The **smooth endoplasmic reticulum** is involved in **lipid synthesis**, detoxification, and calcium storage.
- While lipid metabolism is affected in Refsum disease, the primary defect is in the degradation of branched-chain fatty acids like phytanic acid, which occurs in **peroxisomes**, not the smooth ER.
*Mitochondria*
- **Mitochondria** are the primary sites of **ATP production** through oxidative phosphorylation and are involved in fatty acid beta-oxidation.
- While some metabolic disorders affect mitochondria, **phytanic acid accumulation** specifically points to a peroxisomal defect because phytanic acid cannot undergo beta-oxidation due to its 3-methyl branch and requires alpha-oxidation, which is a peroxisomal process.
*Myofilaments*
- **Myofilaments** (actin and myosin) are the contractile proteins within muscle cells.
- While muscle weakness is a symptom, the underlying cause is not a primary defect in myofilaments themselves, but rather the **neurological and systemic effects** of phytanic acid accumulation affecting peripheral nerves and muscle innervation.
Phospholipid metabolism US Medical PG Question 10: A 35-year-old man comes to the physician because of fatigue and generalized weakness for the past year. He has noticed he has been having fewer bowel movements. He has had pain with defecation and small amounts of blood when wiping. He has not lost weight despite increased efforts to diet and exercise. He has had no fever, throat pain, or difficulty swallowing. His temperature is 36.5°C (97.7°F), pulse is 50/min, blood pressure is 120/90 mm Hg, and BMI is 35 kg/m2. Physical examination shows dry skin and a distended abdomen. There is 1+ pitting edema in the lower extremities. On neurological examination, deep tendon reflexes are 1+. Further evaluation of this patient is most likely to show which of the following findings?
- A. Hyperglycemia
- B. Decreased serum creatinine
- C. Elevated serum low-density lipoprotein (Correct Answer)
- D. Decreased plasma homocysteine concentrations
- E. Decreased serum creatine kinase
Phospholipid metabolism Explanation: ***Elevated serum low-density lipoprotein***
- The patient's symptoms (fatigue, generalized weakness, constipation, weight gain despite efforts, cold intolerance implied by dry skin, bradycardia, and edema) are highly suggestive of **hypothyroidism**.
- **Hypothyroidism** classically leads to **hyperlipidemia**, specifically elevated **LDL cholesterol**, due to decreased catabolism of cholesterol.
*Decreased serum creatine kinase*
- **Hypothyroidism** typically causes **myopathy**, which can manifest as elevated, not decreased, serum **creatine kinase** levels.
- Muscle weakness and fatigue in hypothyroidism are often associated with muscle damage and elevated CK.
*Hyperglycemia*
- While hypothyroidism can impact glucose metabolism, it more commonly leads to **insulin resistance** and can contribute to **hyperglycemia**, but it is not a direct or consistent consequence, and other factors are often more significant.
- However, hypothyroidism is not primarily characterized by hyperglycemia as a direct pathognomonic finding.
*Decreased serum creatinine*
- **Hypothyroidism** is typically associated with **decreased glomerular filtration rate (GFR)**, which can lead to **increased serum creatinine**, not decreased.
- A decreased GFR would imply reduced clearance of creatinine, thus elevating its serum concentration.
*Decreased plasma homocysteine concentrations*
- **Hypothyroidism** is linked to **elevated plasma homocysteine** concentrations, likely due to impaired metabolism (e.g., reduced activity of methionine synthase).
- High homocysteine levels are a risk factor for cardiovascular disease.
More Phospholipid metabolism US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.