Lipoprotein metabolism US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Lipoprotein metabolism. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Lipoprotein metabolism US Medical PG Question 1: A scientist is trying to design a drug to modulate cellular metabolism in the treatment of obesity. Specifically, he is interested in understanding how fats are processed in adipocytes in response to different energy states. His target is a protein within these cells that catalyzes catabolism of an energy source. The products of this reaction are subsequently used in gluconeogenesis or β-oxidation. Which of the following is true of the most likely protein that is being studied by this scientist?
- A. It is stimulated by epinephrine (Correct Answer)
- B. It is inhibited by glucagon
- C. It is inhibited by acetylcholine
- D. It is inhibited by cortisol
- E. It is stimulated by insulin
Lipoprotein metabolism Explanation: ***It is stimulated by epinephrine***
- The protein described is likely **hormone-sensitive lipase (HSL)**, which catabolizes **triglycerides** in adipocytes to **glycerol** and **fatty acids**.
- **Epinephrine** (and norepinephrine) stimulates HSL activity via a **cAMP-dependent protein kinase A (PKA)** pathway, leading to increased fatty acid release for energy.
*It is inhibited by glucagon*
- **Glucagon primarily acts on the liver** to promote gluconeogenesis and glycogenolysis, but it does **not directly inhibit HSL** in adipocytes.
- While glucagon has a lipolytic effect, it doesn't inhibit the enzyme that releases fatty acids.
*It is inhibited by acetylcholine*
- **Acetylcholine** is a neurotransmitter involved in the **parasympathetic nervous system**, which generally promotes energy storage.
- It does **not directly inhibit HSL**; its effects on lipid metabolism are indirect and typically involve other pathways.
*It is inhibited by cortisol*
- **Cortisol**, a glucocorticoid, generally **promotes lipolysis** (breakdown of fats) in certain contexts, particularly during stress to provide energy substrates.
- Therefore, it would **not inhibit HSL**; rather, it often enhances its activity or provides a permissive effect for other lipolytic hormones.
*It is stimulated by insulin*
- **Insulin** is an **anabolic hormone** that promotes energy storage, including **lipogenesis** (fat synthesis) and inhibits lipolysis.
- Insulin **inhibits HSL activity** by activating phosphodiesterase, which reduces cAMP levels, thus deactivating PKA and preventing HSL phosphorylation.
Lipoprotein metabolism US Medical PG Question 2: A previously healthy 22-year-old man comes to the physician because of multiple nodules on his hands that first appeared a few months ago. He works as a computer game programmer. His father died of a myocardial infarction at 37 years of age, and his mother has rheumatoid arthritis. A photograph of the lesions is shown. The nodules are firm, mobile, and nontender. Which of the following is the most likely mechanism underlying this patient's skin findings?
- A. Extravasation of lipoproteins (Correct Answer)
- B. Crystallization of monosodium urate
- C. Uncontrolled adipocyte growth
- D. Deposition of triglycerides
- E. Fibrinoid necrosis
Lipoprotein metabolism Explanation: ***Extravasation of lipoproteins***
- The description of firm, mobile, nontender nodules on the hands of a young man with a strong family history of early-onset **myocardial infarction** (father died at age 37) is highly suggestive of **tendinous xanthomas**
- **Tendinous xanthomas** result from deposition of **cholesterol-rich lipoproteins** in tendons, characteristically seen in **familial hypercholesterolemia (FH)**
- FH is an autosomal dominant disorder causing defective **LDL receptor function**, leading to markedly elevated **LDL cholesterol** levels and premature **cardiovascular disease**
- The **extravasation and accumulation of lipoproteins** in tendons creates these firm nodules, most commonly affecting the **Achilles tendons** and **extensor tendons of the hands**
*Crystallization of monosodium urate*
- This mechanism describes the formation of **tophi** in **chronic gout**, composed of **monosodium urate crystals**
- Tophi can present as firm nodules but typically occur in patients with **longstanding hyperuricemia** and often have a history of **gouty arthritis attacks**
- The strong family history of early MI and absence of gout history makes this unlikely
*Uncontrolled adipocyte growth*
- This mechanism describes **lipomas**, which are benign tumors of **adipocytes (fat cells)**
- Lipomas are typically **soft, pliable, and rubbery** (not firm), and are usually **solitary rather than multiple**
- They are not associated with **hyperlipidemia** or **premature cardiovascular disease**
*Deposition of triglycerides*
- While **triglycerides** are lipids, the primary component of **tendinous xanthomas** is **cholesterol** (not triglycerides) deposited within **lipoproteins**
- **Eruptive xanthomas** (associated with severe **hypertriglyceridemia**) present differently as small, yellow papules on **extensor surfaces** and **buttocks**, not firm tendon nodules
- The clinical presentation and family history point to **cholesterol accumulation**, not triglyceride deposition
*Fibrinoid necrosis*
- **Fibrinoid necrosis** is a pattern of tissue injury involving deposition of **fibrin-like material** in vessel walls, seen in **immune-mediated vasculitis** and **malignant hypertension**
- This process does not produce the firm, mobile, nontender tendon nodules described
- Not associated with **familial hyperlipidemia** or **premature atherosclerotic disease**
Lipoprotein metabolism US Medical PG Question 3: A 1-year-old girl is brought to the pediatrician because of a 6-month history of diarrhea. She has not received recommended well-child examinations. Her stools are foul-smelling and nonbloody. There is no family history of serious illness. She is at the 15th percentile for height and 5th percentile for weight. Physical examination shows abdominal distension. Her serum triglyceride concentration is 5 mg/dL. Genetic analysis shows a mutation in the gene that encodes microsomal triglyceride transfer protein. Which of the following is the most appropriate treatment for this patient's condition?
- A. Nicotinic acid supplementation
- B. Pancreatic enzyme replacement
- C. Long-term antibiotic therapy
- D. Restriction of long-chain fatty acids (Correct Answer)
- E. Avoidance of dietary gluten
Lipoprotein metabolism Explanation: ***Restriction of long-chain fatty acids***
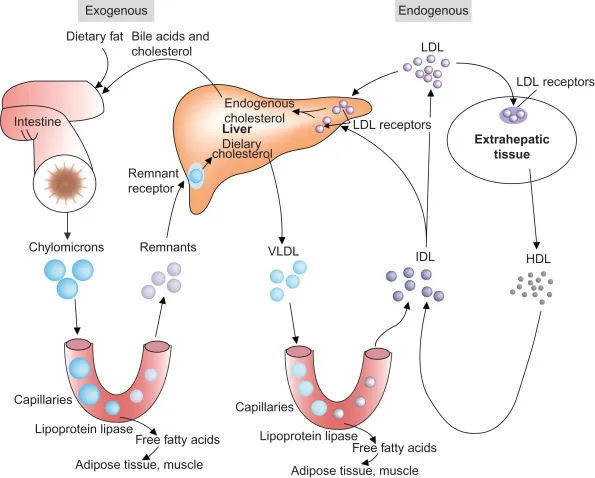
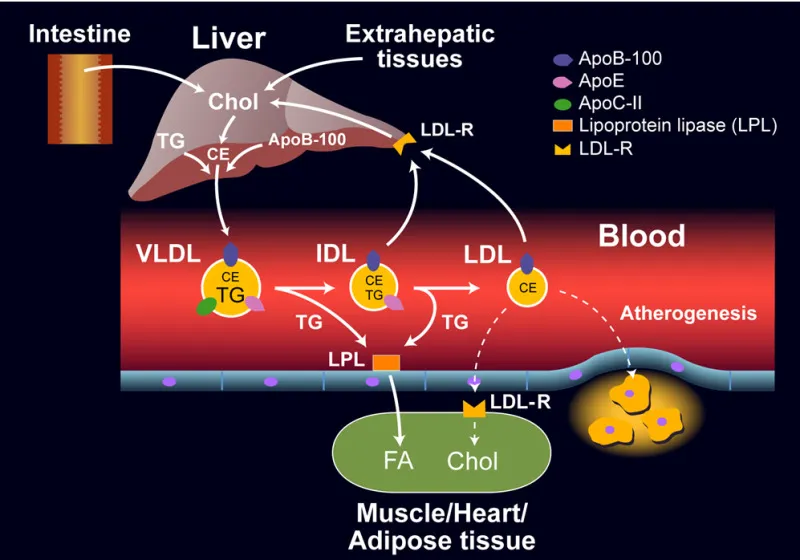
- This patient has **abetalipoproteinemia** due to the mutation in the **microsomal triglyceride transfer protein (MTP)**, causing defective chylomicron formation and severe fat malabsorption. Restricting **long-chain fatty acids (LCFAs)** minimizes the substrate for chylomicron synthesis, reducing gastrointestinal symptoms.
- **Medium-chain triglycerides (MCTs)** can be supplemented as they do not require chylomicron formation for absorption, bypassing the defective MTP pathway and providing a source of energy.
- Additional treatment includes **fat-soluble vitamin supplementation** (vitamins A, D, E, K) since fat malabsorption leads to deficiency of these vitamins.
*Nicotinic acid supplementation*
- **Nicotinic acid (niacin)** is typically used to lower **LDL cholesterol** and **triglyceride** levels in patients with **hyperlipidemia**.
- It would not address the underlying issue of fat malabsorption or the inability to form chylomicrons in abetalipoproteinemia.
*Pancreatic enzyme replacement*
- **Pancreatic enzyme replacement therapy** is used for conditions like **cystic fibrosis** or **chronic pancreatitis**, where there is insufficient production of lipase and other digestive enzymes.
- In this case, the issue is not enzyme deficiency but rather the inability to package absorbed fats into chylomicrons for transport.
*Long-term antibiotic therapy*
- Long-term antibiotics are primarily used to treat **chronic bacterial infections** or **small intestinal bacterial overgrowth (SIBO)**.
- The patient's symptoms are due to a genetic metabolic defect, not an infection, making antibiotics ineffective for the primary condition.
*Avoidance of dietary gluten*
- **Gluten-free diets** are prescribed for **celiac disease**, an autoimmune condition triggered by gluten, leading to villous atrophy and malabsorption.
- The patient's symptoms, low triglyceride levels, and genetic mutation point to abetalipoproteinemia, not celiac disease.
Lipoprotein metabolism US Medical PG Question 4: A 33-year-old man presents with his recent laboratory results. He has no symptoms currently, but he underwent a medical evaluation as a requirement for taking up a new job. His medical history is not significant. His laboratory reports are as follows:
Blood hemoglobin 13.7 g/dL
Leukocyte count 8,000/mm3
Platelet count 350,000/mm3
Serum creatinine 0.8 mg/dL
Serum alanine aminotransferase 16 U/L
Serum aspartate aminotransferase 14 U/L
Serum cholesterol 450 mg/dL
Serum triglyceride 790 mg/dL
Serum LDL cholesterol 150 mg/dL
Serum HDL cholesterol 55 mg/dL
Which of the following findings is most likely to be present on physical examination of this patient?
- A. Eruptive xanthomas over back
- B. Xanthelasma
- C. Palmar xanthomas in flexor creases (Correct Answer)
- D. Achilles tendon xanthoma
- E. Metacarpophalangeal extensor tendon xanthoma
Lipoprotein metabolism Explanation: ***Palmar xanthomas in flexor creases***
- This patient presents with significantly elevated **triglycerides (790 mg/dL)** and **total cholesterol (450 mg/dL)** with relatively normal **LDL (150 mg/dL)** and **HDL (55 mg/dL)**.
- This lipid profile pattern—**combined elevation of cholesterol and triglycerides with disproportionately normal/low LDL**—is characteristic of **familial dysbetalipoproteinemia (Type III hyperlipoproteinemia)**.
- **Palmar xanthomas** appearing in the palmar creases are **pathognomonic** for Type III hyperlipoproteinemia, caused by accumulation of chylomicron and VLDL remnants due to defective apolipoprotein E.
- While uncommon even in Type III, palmar xanthomas are the most specific physical finding for this diagnosis.
*Eruptive xanthomas over back*
- **Eruptive xanthomas** typically occur with **very high triglycerides (>1000 mg/dL)**, presenting as sudden crops of small, yellowish-red papules with erythematous halos.
- This patient's triglycerides at 790 mg/dL are elevated but below the threshold that typically produces eruptive xanthomas.
- Eruptive xanthomas are more commonly seen in **Type I or Type V hyperlipoproteinemia** with severe hypertriglyceridemia.
*Xanthelasma*
- **Xanthelasma** are yellowish plaques on the eyelids, the most common type of xanthoma overall.
- Can occur with **any lipid disorder** or even with normal lipid levels in some cases.
- While possible in this patient, xanthelasma lack the diagnostic specificity of palmar xanthomas for Type III hyperlipoproteinemia.
*Achilles tendon xanthoma*
- **Achilles tendon xanthomas** are characteristic of **familial hypercholesterolemia (Type IIa)**, which features markedly elevated **LDL cholesterol (typically >190 mg/dL)** due to defective LDL receptors.
- This patient's LDL is only 150 mg/dL, making familial hypercholesterolemia unlikely.
- The combined cholesterol and triglyceride elevation points away from pure LDL elevation.
*Metacarpophalangeal extensor tendon xanthoma*
- **Tendon xanthomas** on the extensor tendons are also associated with **familial hypercholesterolemia (Type IIa)**.
- Like Achilles tendon xanthomas, these require very high **LDL cholesterol**, which is not the primary abnormality here.
- The patient's lipid profile does not support this diagnosis.
Lipoprotein metabolism US Medical PG Question 5: A 14-year-old boy comes to the physician for a follow-up after a blood test showed a serum triglyceride level of 821 mg/dL. Several of his family members have familial hypertriglyceridemia. The patient is prescribed a fibrate medication that increases his risk of gallstone disease. The expected beneficial effect of this drug is most likely due to which of the following actions?
- A. Increased PPAR-gamma activity
- B. Increased bile acid sequestration
- C. Increased lipoprotein lipase activity (Correct Answer)
- D. Decreased HMG-CoA reductase activity
- E. Decreased lipolysis in adipose tissue
Lipoprotein metabolism Explanation: **Increased lipoprotein lipase activity**
- Fibrates, such as **gemfibrozil** and **fenofibrate**, are agonists of **peroxisome proliferator-activated receptor alpha (PPAR-alpha)**, which upregulates the expression of **lipoprotein lipase (LPL)**.
- Increased LPL activity leads to enhanced catabolism of **triglyceride-rich lipoproteins** (VLDL and chylomicrons), thereby lowering serum triglyceride levels.
*Increased PPAR-gamma activity*
- This is the primary mechanism of action for **thiazolidinediones (glitazones)**, used in the treatment of **type 2 diabetes mellitus**.
- PPAR-gamma activation primarily improves **insulin sensitivity** and promotes **adipogenesis**, with a less direct effect on triglyceride clearance compared to PPAR-alpha activation.
*Increased bile acid sequestration*
- This is the mechanism of action for **bile acid resins** (e.g., cholestyramine, colestipol), which bind bile acids in the intestine, preventing their reabsorption.
- This leads to increased synthesis of **new bile acids** from cholesterol in the liver, thereby lowering **LDL cholesterol** levels, but not directly targeting triglycerides.
*Decreased HMG-CoA reductase activity*
- This describes the mechanism of action of **statins** (e.g., atorvastatin, simvastatin), which are potent inhibitors of **HMG-CoA reductase**, the rate-limiting enzyme in **cholesterol biosynthesis**.
- Statins primarily reduce **LDL cholesterol** levels, with a secondary, less pronounced effect on triglycerides.
*Decreased lipolysis in adipose tissue*
- **Niacin (vitamin B3)** primarily works by inhibiting **hormone-sensitive lipase** in adipose tissue, which reduces the release of **free fatty acids** into circulation.
- This, in turn, decreases hepatic synthesis of **triglycerides** and **VLDL**, thus lowering triglyceride levels.
Lipoprotein metabolism US Medical PG Question 6: A 10-month-old boy with a seizure disorder is brought to the physician by his mother because of a 2-day history of vomiting and lethargy. Laboratory studies show a decreased serum glucose concentration with low ketones. Further testing confirms a deficiency in an enzyme involved in fatty acid oxidation. Which of the following enzymes is most likely deficient in this patient?
- A. Acyl-CoA dehydrogenase (Correct Answer)
- B. HMG-CoA reductase
- C. Glycerol kinase
- D. Acetyl-CoA carboxylase
- E. Glycerol-3-phosphate dehydrogenase
Lipoprotein metabolism Explanation: ***Acyl-CoA dehydrogenase***
- The combination of **hypoglycemia** with **low ketones** in a setting of prolonged vomiting (stress) strongly suggests a **disorder of fatty acid oxidation**. These disorders impair the body's ability to produce ketones when glucose stores are low.
- **Acyl-CoA dehydrogenase** is a key enzyme in the mitochondrial β-oxidation of fatty acids. A deficiency prevents the breakdown of fatty acids into acetyl-CoA, which is necessary for ketogenesis and to fuel gluconeogenesis indirectly.
*HMG-CoA reductase*
- This enzyme is involved in **cholesterol synthesis**, not directly in fatty acid oxidation or ketone body formation from fatty acids.
- Deficiency would primarily affect cholesterol levels and not typically present with the described metabolic crisis of hypoglycemia and low ketones.
*Glycerol kinase*
- **Glycerol kinase** phosphorylates glycerol, a product of triglyceride hydrolysis, allowing it to enter glycolysis or gluconeogenesis.
- A deficiency would impair glycerol utilization but would not directly impact fatty acid oxidation pathways that are critical for ketone production during hypoglycemia.
*Acetyl-CoA carboxylase*
- **Acetyl-CoA carboxylase** is the rate-limiting enzyme in **fatty acid synthesis**, not degradation.
- A deficiency would lead to impaired fatty acid synthesis, which is the opposite of the metabolic problem described (impaired breakdown of fatty acids).
*Glycerol-3-phosphate dehydrogenase*
- This enzyme is involved in the conversion of **dihydroxyacetone phosphate (DHAP)** to **glycerol-3-phosphate** in both triglyceride synthesis and the glycerol phosphate shuttle.
- While related to lipid metabolism, a deficiency would not directly cause the severe hypoglycemia and hypoketosis seen with a fatty acid oxidation defect.
Lipoprotein metabolism US Medical PG Question 7: A 57-year-old woman comes to the physician for a routine examination. She takes no medications. She swims 3 times weekly and jogs several miles with her dog on most mornings. Her diet consists primarily of vegetables, fish, and whole grains; she avoids processed foods and carbohydrates. She drinks one glass of red wine with dinner on most evenings. There is no family history of serious medical illness or cardiovascular disease. Physical examination shows no abnormalities. This patient is most likely to have an increase in which of the following laboratory markers?
- A. Low density lipoprotein
- B. Apolipoprotein B-100
- C. Very low density lipoprotein
- D. Triglyceride
- E. High density lipoprotein (Correct Answer)
Lipoprotein metabolism Explanation: ***High density lipoprotein***
- This patient's lifestyle, characterized by **regular exercise**, a **diet rich in good fats** (fish, whole grains), and **moderate alcohol consumption** (one glass of red wine), are all factors known to increase **HDL levels**.
- **HDL** is often referred to as "good cholesterol" and plays a vital role in reverse cholesterol transport, removing cholesterol from peripheral tissues and transporting it to the liver for excretion.
*Low density lipoprotein*
- A diet high in fruits, vegetables, fish, and whole grains, along with regular exercise, would typically lead to a **decrease in LDL** ("bad cholesterol").
- The absence of processed foods and carbohydrates further supports a **lower, not higher, LDL level**.
*Apolipoprotein B-100*
- **Apolipoprotein B-100** is the primary protein component of LDL and VLDL, and its levels generally **correlate directly with LDL levels**.
- Given the patient's healthy lifestyle, an increase in LDL is unlikely, making an increase in **ApoB-100** also unlikely.
*Very low density lipoprotein*
- VLDL levels are strongly influenced by dietary intake, particularly of **saturated fats and refined carbohydrates**.
- This patient's diet explicitly avoids processed foods and carbohydrates, making an **increase in VLDL unlikely**.
*Triglyceride*
- This patient's **healthy diet**, including lean proteins and whole grains, combined with regular exercise and limited saturated fats, would typically result in **lower triglyceride levels**.
- **Moderate alcohol intake** may temporarily increase triglycerides in some individuals, but the overall lifestyle factors strongly point towards reduced levels.
Lipoprotein metabolism US Medical PG Question 8: Steroid hormone synthesis, lipid synthesis, and chemical detoxification are activities of which of the following?
- A. Peroxisomes
- B. Nucleolus
- C. Rough Endoplasmic Reticulum
- D. Smooth Endoplasmic Reticulum (Correct Answer)
- E. Golgi bodies
Lipoprotein metabolism Explanation: ***Smooth Endoplasmic Reticulum***
- The **smooth endoplasmic reticulum (SER)** is rich in enzymes that catalyze the synthesis of **lipids**, including steroid hormones, and is crucial for the detoxification of drugs and poisons, particularly in liver cells.
- Its tubular structure, devoid of ribosomes, differentiates its functions from the rough ER, focusing on metabolic processes like **calcium ion storage** and carbohydrate metabolism.
*Peroxisomes*
- Peroxisomes are primarily involved in the breakdown of **fatty acids** and amino acids, producing hydrogen peroxide as a byproduct.
- They also play a role in detoxification but are not the primary site for steroid hormone or general lipid synthesis.
*Nucleolus*
- The **nucleolus** is a dense structure within the nucleus responsible for synthesizing **ribosomal RNA (rRNA)** and assembling ribosomes.
- It has no direct role in steroid hormone synthesis, lipid metabolism, or chemical detoxification.
*Rough Endoplasmic Reticulum*
- The **rough endoplasmic reticulum (RER)** is studded with **ribosomes** and is primarily involved in the synthesis and modification of **proteins** destined for secretion or insertion into membranes.
- While it's part of the endomembrane system, it does not directly perform lipid synthesis or chemical detoxification as its main functions.
*Golgi bodies*
- **Golgi bodies (or Golgi apparatus)** are responsible for modifying, sorting, and packaging **proteins and lipids** synthesized in the ER into vesicles for secretion or delivery to other organelles.
- They do not perform the initial synthesis of steroid hormones or lipids, nor are they the primary site for chemical detoxification.
Lipoprotein metabolism US Medical PG Question 9: A 35-year-old man comes to the physician because of fatigue and generalized weakness for the past year. He has noticed he has been having fewer bowel movements. He has had pain with defecation and small amounts of blood when wiping. He has not lost weight despite increased efforts to diet and exercise. He has had no fever, throat pain, or difficulty swallowing. His temperature is 36.5°C (97.7°F), pulse is 50/min, blood pressure is 120/90 mm Hg, and BMI is 35 kg/m2. Physical examination shows dry skin and a distended abdomen. There is 1+ pitting edema in the lower extremities. On neurological examination, deep tendon reflexes are 1+. Further evaluation of this patient is most likely to show which of the following findings?
- A. Hyperglycemia
- B. Decreased serum creatinine
- C. Elevated serum low-density lipoprotein (Correct Answer)
- D. Decreased plasma homocysteine concentrations
- E. Decreased serum creatine kinase
Lipoprotein metabolism Explanation: ***Elevated serum low-density lipoprotein***
- The patient's symptoms (fatigue, generalized weakness, constipation, weight gain despite efforts, cold intolerance implied by dry skin, bradycardia, and edema) are highly suggestive of **hypothyroidism**.
- **Hypothyroidism** classically leads to **hyperlipidemia**, specifically elevated **LDL cholesterol**, due to decreased catabolism of cholesterol.
*Decreased serum creatine kinase*
- **Hypothyroidism** typically causes **myopathy**, which can manifest as elevated, not decreased, serum **creatine kinase** levels.
- Muscle weakness and fatigue in hypothyroidism are often associated with muscle damage and elevated CK.
*Hyperglycemia*
- While hypothyroidism can impact glucose metabolism, it more commonly leads to **insulin resistance** and can contribute to **hyperglycemia**, but it is not a direct or consistent consequence, and other factors are often more significant.
- However, hypothyroidism is not primarily characterized by hyperglycemia as a direct pathognomonic finding.
*Decreased serum creatinine*
- **Hypothyroidism** is typically associated with **decreased glomerular filtration rate (GFR)**, which can lead to **increased serum creatinine**, not decreased.
- A decreased GFR would imply reduced clearance of creatinine, thus elevating its serum concentration.
*Decreased plasma homocysteine concentrations*
- **Hypothyroidism** is linked to **elevated plasma homocysteine** concentrations, likely due to impaired metabolism (e.g., reduced activity of methionine synthase).
- High homocysteine levels are a risk factor for cardiovascular disease.
Lipoprotein metabolism US Medical PG Question 10: A 24-year-old man presents for an annual check-up. He is a bodybuilder and tells you he is on a protein-rich diet that only allows for minimal carbohydrate intake. His friend suggests he try exogenous glucagon to help him lose some excess weight before an upcoming competition. Which of the following effects of glucagon is he attempting to exploit?
- A. Increased glucose utilization by tissues
- B. Decreased blood cholesterol level
- C. Increased hepatic gluconeogenesis
- D. Increased lipolysis in adipose tissues (Correct Answer)
- E. Increased hepatic glycogenolysis
Lipoprotein metabolism Explanation: ***Increased lipolysis in adipose tissues***
- While **glucagon's primary target is the liver**, it can have **modest lipolytic effects** on adipose tissue by opposing insulin's anti-lipolytic actions.
- Glucagon stimulates cAMP production, which can activate **hormone-sensitive lipase** to break down triglycerides into **fatty acids** and **glycerol**.
- However, **catecholamines (epinephrine/norepinephrine)** are far more potent direct stimulators of adipose tissue lipolysis than glucagon.
- The friend is attempting to exploit this lipolytic effect for fat loss, though **exogenous glucagon is not an evidence-based or safe weight-loss strategy**.
*Increased glucose utilization by tissues*
- This is **opposite** to glucagon's actual effect. **Glucagon raises blood glucose** levels; it does not promote glucose uptake by peripheral tissues.
- **Insulin** is the hormone responsible for promoting glucose uptake and utilization by muscle, adipose, and other tissues.
*Decreased blood cholesterol level*
- Glucagon does not have a direct, clinically significant effect on reducing blood cholesterol levels.
- While glucagon affects overall lipid metabolism through its catabolic actions, it is not used therapeutically for hypercholesterolemia.
*Increased hepatic gluconeogenesis*
- **Glucagon strongly stimulates hepatic gluconeogenesis**, which is the synthesis of glucose from non-carbohydrate precursors (amino acids, lactate, glycerol) in the liver.
- This action **raises blood glucose** levels and would not directly contribute to fat loss or weight reduction.
- In the context of a low-carbohydrate diet, increased gluconeogenesis would maintain blood glucose but not promote the fat loss the bodybuilder seeks.
*Increased hepatic glycogenolysis*
- **Glucagon is a potent stimulator of hepatic glycogenolysis**, the breakdown of stored liver glycogen into glucose.
- This rapidly increases blood glucose levels during fasting or hypoglycemia.
- However, this does not directly target adipose tissue for fat loss; it mobilizes glucose stores rather than fat stores, so it's not the mechanism relevant to weight loss goals.
More Lipoprotein metabolism US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.