Eicosanoid synthesis and function US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Eicosanoid synthesis and function. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Eicosanoid synthesis and function US Medical PG Question 1: A 6-year-old boy is presented to a pediatric clinic by his mother with complaints of fever, malaise, and cough for the past 2 days. He frequently complains of a sore throat and has difficulty eating solid foods. The mother mentions that, initially, the boy’s fever was low-grade and intermittent but later became high grade and continuous. The boy was born at 39 weeks gestation via spontaneous vaginal delivery. He is up to date on all vaccines and is meeting all developmental milestones. The past medical history is noncontributory. The boy takes a multivitamin every day. The mother reports that he does well in school and is helpful around the house. The boy’s vital signs include blood pressure 110/65 mm Hg, heart rate 110/min, respiratory rate 32/min, and temperature 38.3°C (101.0°F). On physical examination, the boy appears uncomfortable and has difficulty breathing. His heart is mildly tachycardic with a regular rhythm and his lungs are clear to auscultation bilaterally. Oropharyngeal examination shows that his palatine tonsils are covered with pus and that there is erythema of the surrounding mucosa. Which of the following mediators is responsible for this patient’s elevated temperature?
- A. Leukotriene D4
- B. Prostaglandin F2
- C. Prostaglandin E2 (Correct Answer)
- D. Thromboxane A2
- E. Prostaglandin I2
Eicosanoid synthesis and function Explanation: ***Prostaglandin E2***
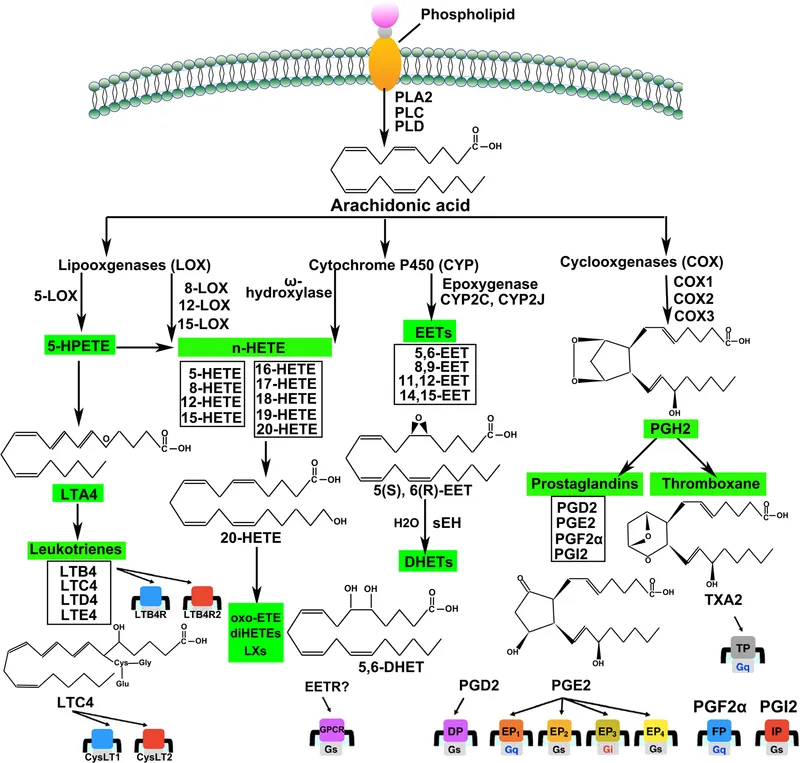
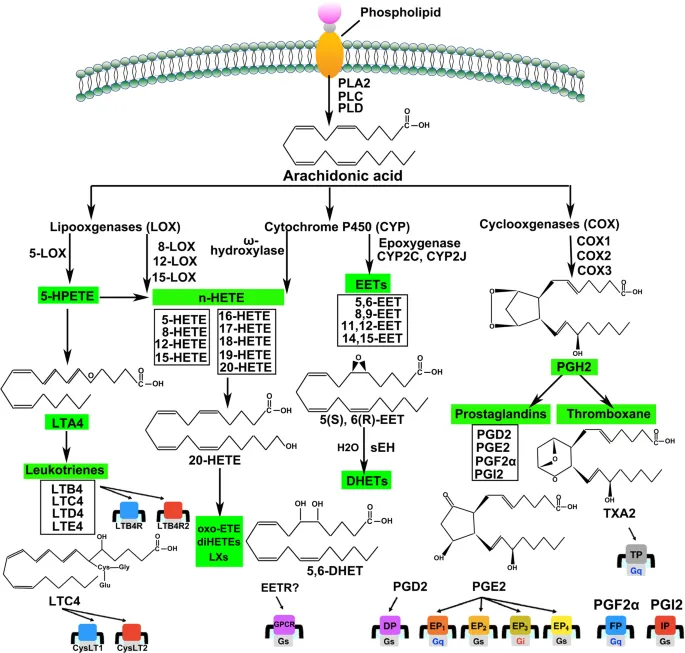
- **Prostaglandin E2 (PGE2)** is a key mediator of fever, acting directly on the **hypothalamus** to reset the body's thermoregulatory set point.
- In response to infection and inflammation, immune cells release **pyrogens** (like IL-1, TNF-alpha), which stimulate PGE2 synthesis in the brain, leading to increased body temperature.
*Leukotriene D4*
- **Leukotriene D4 (LTD4)** is a potent mediator of **bronchoconstriction** and increased **vascular permeability**, particularly in allergic reactions and asthma.
- While it plays a role in inflammation, it does not directly cause fever by altering the hypothalamic set point.
*Prostaglandin F2*
- **Prostaglandin F2 (PGF2)** has various physiological roles, including **uterine contraction** and **bronchoconstriction**, and is important for reproductive functions.
- It is not primarily involved in mediating the febrile response to infection.
*Thromboxane A2*
- **Thromboxane A2 (TXA2)** is predominantly involved in **platelet aggregation** and **vasoconstriction**, playing a crucial role in hemostasis and thrombosis.
- While it is a product of the arachidonic acid pathway, it does not directly contribute to fever.
*Prostaglandin I2*
- **Prostaglandin I2 (PGI2)**, also known as **prostacyclin**, is a potent **vasodilator** and inhibitor of **platelet aggregation**, protecting the vascular endothelium.
- It typically counteracts the effects of TXA2 and is not a mediator of fever.
Eicosanoid synthesis and function US Medical PG Question 2: A 53-year-old man is brought to the emergency department because of wheezing and shortness of breath that began 1 hour after he took a new medication. Earlier in the day he was diagnosed with stable angina pectoris and prescribed a drug that irreversibly inhibits cyclooxygenase-1 and 2. He has chronic rhinosinusitis and asthma treated with inhaled β-adrenergic agonists and corticosteroids. His respirations are 26/min. Examination shows multiple small, erythematous nasal mucosal lesions. After the patient is stabilized, therapy for primary prevention of coronary artery disease should be switched to a drug with which of the following mechanisms of action?
- A. Direct inhibition of Factor Xa
- B. Sequestration of Ca2+ ions
- C. Potentiation of antithrombin III
- D. Blockage of P2Y12 component of ADP receptors (Correct Answer)
- E. Inhibition of vitamin K epoxide reductase
Eicosanoid synthesis and function Explanation: ***Blockage of P2Y12 component of ADP receptors***
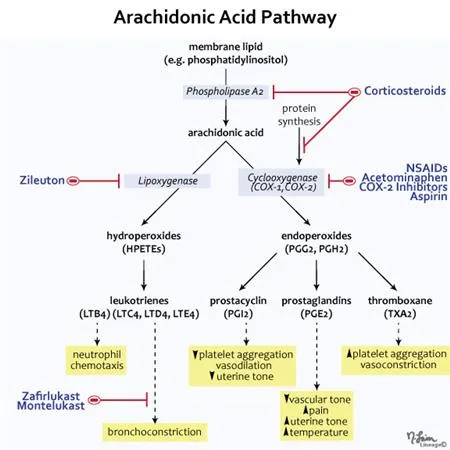
- The patient experienced an asthma exacerbation suspected to be due to **aspirin-exacerbated respiratory disease (AERD)**, which is triggered by **aspirin** (a non-selective COX inhibitor).
- Given the need for antiplatelet therapy for CAD, a **P2Y12 receptor antagonist** such as **clopidogrel** is a suitable alternative to aspirin in patients with AERD, as it does not interact with the cyclooxygenase pathway.
*Direct inhibition of Factor Xa*
- This mechanism of action describes drugs like **rivaroxaban** or **apixaban**, which are primarily used as anticoagulants for conditions like atrial fibrillation or venous thromboembolism.
- While they prevent clot formation, they are not typically used for primary prevention of **coronary artery disease (CAD)** in lieu of antiplatelet agents like aspirin or P2Y12 inhibitors.
*Sequestration of Ca2+ ions*
- This refers to **calcium channel blockers (CCBs)**, which are used to treat hypertension, angina, and certain arrhythmias.
- While CCBs can be used to manage angina symptoms, they do not provide the necessary **antiplatelet effect** for primary prevention of cardiovascular events in CAD.
*Potentiation of antithrombin III*
- This is the mechanism of action for **heparins** (e.g., unfractionated heparin, low molecular weight heparin) and related drugs like fondaparinux.
- **Heparins are anticoagulants** used for acute thrombosis or prophylaxis in specific situations, but they are not used for chronic **primary prevention of CAD** in stable patients.
*Inhibition of vitamin K epoxide reductase*
- This describes the mechanism of **warfarin**, a vitamin K antagonist used as an anticoagulant for conditions like atrial fibrillation, prosthetic heart valves, or venous thromboembolism.
- Warfarin is an anticoagulant, not an antiplatelet agent, and is not indicated for **primary prevention of CAD** in this context.
Eicosanoid synthesis and function US Medical PG Question 3: A 14-year-old boy is brought to the emergency department because of a 4-hour history of vomiting, lethargy, and confusion. Three days ago, he was treated with an over-the-counter medication for fever and runny nose. He is oriented only to person. His blood pressure is 100/70 mm Hg. Examination shows bilateral optic disc swelling and hepatomegaly. His blood glucose concentration is 65 mg/dL. Toxicology screening for serum acetaminophen is negative. The over-the-counter medication that was most likely used by this patient has which of the following additional effects?
- A. Increased partial thromboplastin time
- B. Decreased uric acid elimination
- C. Decreased expression of glycoprotein IIb/IIIa
- D. Irreversible inhibition of ATP synthase
- E. Irreversible inhibition of cyclooxygenase-1 (Correct Answer)
Eicosanoid synthesis and function Explanation: ***Irreversible inhibition of cyclooxygenase-1***
- The patient's presentation is classic for **Reye syndrome** (vomiting, lethargy, confusion, cerebral edema with optic disc swelling, hepatomegaly, hypoglycemia) following recent viral illness treated with OTC medication
- **Aspirin** is strongly associated with Reye syndrome in children with viral infections and should be avoided in this population
- The "additional effect" of aspirin is its mechanism of action: **irreversible acetylation and inhibition of COX-1 and COX-2**
- This irreversible COX inhibition also explains aspirin's antiplatelet effects (via inhibition of thromboxane A2 synthesis) and anti-inflammatory properties
*Increased partial thromboplastin time*
- PTT measures the intrinsic and common coagulation pathways and is prolonged by **heparin** or clotting factor deficiencies
- Aspirin affects **platelet function** (prolonging bleeding time), not the coagulation cascade measured by PTT
- While Reye syndrome can cause coagulopathy from liver dysfunction, increased PTT is not a direct pharmacologic effect of aspirin
*Decreased uric acid elimination*
- **Low-dose aspirin** (<2 g/day) can decrease renal uric acid excretion and may precipitate gout
- While this is true, it is not the primary or most clinically relevant "additional effect" in this context
- High-dose aspirin actually increases uric acid excretion (uricosuric effect)
*Decreased expression of glycoprotein IIb/IIIa*
- This is the mechanism of **GP IIb/IIIa inhibitors** (abciximab, eptifibatide, tirofiban), not aspirin
- Aspirin inhibits platelet aggregation by preventing thromboxane A2 synthesis, not by affecting GP IIb/IIIa expression
- These are IV antiplatelet agents used in acute coronary syndromes, not OTC medications
*Irreversible inhibition of ATP synthase*
- This is not a mechanism of aspirin or other common OTC fever/cold medications
- While Reye syndrome involves mitochondrial dysfunction, aspirin does not directly inhibit ATP synthase
- The mitochondrial injury in Reye syndrome is likely multifactorial
Eicosanoid synthesis and function US Medical PG Question 4: A 54-year-old man comes to the physician for a follow-up examination. One week ago, he was treated in the emergency department for chest pain, palpitations, and dyspnea. As part of his regimen, he was started on a medication that irreversibly inhibits the synthesis of thromboxane A2 and prostaglandins. Which of the following is the most likely adverse effect of this medication?
- A. Tinnitus
- B. Gout attack
- C. Chronic rhinosinusitis
- D. Acute interstitial nephritis
- E. Gastrointestinal hemorrhage (Correct Answer)
Eicosanoid synthesis and function Explanation: ***Gastrointestinal hemorrhage***
- The medication described, which **irreversibly inhibits thromboxane A2 and prostaglandins**, is **aspirin**. Aspirin's inhibition of **prostaglandin synthesis** in the stomach reduces the protective mucous barrier, leading to an increased risk of **gastric ulcers** and **hemorrhage**.
- **Thromboxane A2 inhibition** by aspirin also impairs platelet aggregation, thereby increasing the risk of bleeding, including **gastrointestinal hemorrhage**.
- This is the **most common serious adverse effect** of chronic aspirin therapy, occurring in approximately 2-4% of patients on long-term low-dose aspirin for cardiovascular prophylaxis.
*Tinnitus*
- **Tinnitus** is a known adverse effect of **salicylate toxicity**, which usually occurs with higher doses of aspirin (>3-4 g/day). While possible, it's **uncommon with standard prophylactic doses** (81-325 mg/day) used for cardiovascular events.
- The question describes a regimen for a cardiac patient, implying a therapeutic dose rather than an overdose scenario.
*Gout attack*
- Aspirin's effect on **uric acid excretion** is dose-dependent: low doses (<1-2 g/day) can **decrease uric acid excretion**, potentially precipitating a gout attack, while high doses increase excretion.
- However, this effect is **less common** than GI complications, and aspirin is generally avoided in patients with known gout due to this complex effect and the availability of safer alternatives.
*Chronic rhinosinusitis*
- **Chronic rhinosinusitis** is not a direct adverse effect of aspirin. However, **aspirin-exacerbated respiratory disease (AERD)**, a condition involving asthma, nasal polyps, and chronic rhinosinusitis, can be triggered by aspirin in susceptible individuals.
- This is a **rare, specific syndrome** affecting approximately 7% of adults with asthma, not a general adverse effect for all patients on aspirin.
*Acute interstitial nephritis*
- **Acute interstitial nephritis** is more commonly associated with **non-steroidal anti-inflammatory drugs (NSAIDs)**, which also inhibit prostaglandin synthesis, but their effect on cyclooxygenase (COX) enzymes is typically reversible, unlike aspirin.
- While NSAIDs can cause AIN by acting as haptens and triggering an immune response, aspirin is **less frequently implicated** in this specific renal pathology compared to other NSAIDs.
Eicosanoid synthesis and function US Medical PG Question 5: A 61-year-old woman comes to the physician because of a 6-month history of left knee pain and stiffness. Examination of the left knee shows tenderness to palpation along the joint line; there is crepitus with full flexion and extension. An x-ray of the knee shows osteophytes with joint-space narrowing. Arthrocentesis of the knee joint yields clear fluid with a leukocyte count of 120/mm3. Treatment with ibuprofen during the next week significantly improves her condition. The beneficial effect of this drug is most likely due to inhibition of which of the following?
- A. Conversion of hypoxanthine to urate
- B. Conversion of phospholipids to arachidonic acid
- C. Conversion of prostaglandin H2 to thromboxane A2
- D. Conversion of arachidonic acid to prostaglandin G2 (Correct Answer)
- E. Conversion of dihydroorotate to orotate
Eicosanoid synthesis and function Explanation: ***Conversion of arachidonic acid to prostaglandin G2***
- This patient presents with symptoms and signs consistent with **osteoarthritis**, characterized by joint pain, stiffness, crepitus, and radiographic findings like **osteophytes** and **joint-space narrowing**.
- **Ibuprofen is a non-selective NSAID** that inhibits **cyclooxygenase (COX-1 and COX-2) enzymes**, which catalyze the conversion of **arachidonic acid to prostaglandin G2 (PGG2)**, the first committed step in prostaglandin synthesis.
- By blocking prostaglandin production, ibuprofen reduces inflammation and pain associated with osteoarthritis.
*Conversion of hypoxanthine to urate*
- This process is catalyzed by **xanthine oxidase** and is inhibited by medications like **allopurinol**, used in the treatment of **gout** to reduce uric acid levels.
- Gout typically presents with acute, severe joint pain with signs of inflammation and monosodium urate crystals on joint aspiration, which are not characteristic of this patient's presentation.
*Conversion of phospholipids to arachidonic acid*
- This step is catalyzed by **phospholipase A2**, which is inhibited by **glucocorticoids** (via lipocortin induction).
- While glucocorticoids have potent anti-inflammatory effects by working upstream of the arachidonic acid cascade, ibuprofen has a different mechanism targeting the COX enzymes downstream.
*Conversion of prostaglandin H2 to thromboxane A2*
- This reaction is catalyzed by **thromboxane synthase**, primarily important in platelet aggregation and vasoconstriction.
- NSAIDs like ibuprofen do not specifically inhibit thromboxane synthase; rather, they inhibit COX enzymes upstream, which reduces production of both prostaglandins and thromboxanes.
- Low-dose aspirin preferentially inhibits COX-1 in platelets, reducing thromboxane A2 for cardioprotection, but this is not ibuprofen's primary therapeutic mechanism in osteoarthritis.
*Conversion of dihydroorotate to orotate*
- This is a step in **pyrimidine synthesis**, inhibited by **leflunomide**, a disease-modifying antirheumatic drug (DMARD) used in rheumatoid arthritis.
- This mechanism is unrelated to the action of NSAIDs or the treatment of osteoarthritis.
Eicosanoid synthesis and function US Medical PG Question 6: A 48-year-old woman presents to the emergency room because of severe back pain after a fall. She says that she was walking home from work when she slipped on a patch of ice on the sidewalk. Since she did not have anything to hold onto, she fell backwards and landed on her posterior iliac crests bilaterally. Immediately after the fall, she started experiencing back pain and tenderness that concerned her enough to call for an ambulance. Her past medical history is significant for arthritis, diabetes, and hypertension. On arrival, her temperature is 99°F (37.2°C), blood pressure is 129/86 mmHg, pulse is 112/min, respirations are 19/min. Physical exam reveals tenderness to palpation over the middle of her lower back. A drug that may have predisposed this patient to this outcome most likely has which of the following mechanisms?
- A. Inhibition of leukotriene and prostaglandin production
- B. Inhibition of circulating cytokine
- C. Inhibition of folate processing
- D. Stimulation of adipocyte transcription factor (Correct Answer)
- E. Inhibition of prostaglandin production alone
Eicosanoid synthesis and function Explanation: ***Stimulation of adipocyte transcription factor***
- The patient's presentation with a **vertebral fracture** after a minor fall, combined with a history of **arthritis**, strongly suggests **osteoporosis** as a predisposing factor.
- **Glucocorticoids** are commonly used to treat arthritis and stimulate **adipocyte transcription factors** (like PPAR-γ), leading to **reduced bone formation** and increased bone resorption, causing osteoporosis.
*Inhibition of leukotriene and prostaglandin production*
- This mechanism describes **NSAIDs**, which are used for pain and inflammation but do not typically cause osteoporosis or increase fracture risk through this specific mechanism.
- While NSAIDs can have gastrointestinal side effects, they are not directly linked to the bone fragility seen in this case.
*Inhibition of circulating cytokine*
- This mechanism is characteristic of **biologic agents** used in immunosuppression, such as TNF-α inhibitors.
- These drugs are not typically associated with increased fracture risk or osteoporosis in the same way glucocorticoids are.
*Inhibition of folate processing*
- This mechanism is characteristic of **methotrexate**, a disease-modifying antirheumatic drug (DMARD) used in arthritis.
- While methotrexate has side effects, it is not primarily known to induce osteoporosis or increase fracture risk as seen with glucocorticoids.
*Inhibition of prostaglandin production alone*
- This mechanism broadly refers to drugs like **NSAIDs** (non-selective COX inhibitors) or selective COX-2 inhibitors.
- As mentioned, these drugs do not typically cause the bone fragility leading to spontaneous fractures seen with long-term glucocorticoid use.
Eicosanoid synthesis and function US Medical PG Question 7: A 19-year-old woman with a history of poorly controlled asthma presents to her pulmonologist for a follow-up visit. She was recently hospitalized for an asthma exacerbation. It is her third hospitalization in the past five years. She currently takes inhaled salmeterol and medium-dose inhaled budesonide. Her past medical history is also notable for psoriasis. She does not smoke and does not drink alcohol. Her temperature is 98.6°F (37°C), blood pressure is 110/65 mmHg, pulse is 75/min, and respirations are 20/min. Physical examination reveals bilateral wheezes that are loudest at the bases. The patient’s physician decides to start the patient on zileuton. Which of the following is the most immediate downstream effect of initiating zileuton?
- A. Decreased signaling via the leukotriene receptor
- B. Decreased signaling via the muscarinic receptor
- C. Decreased mast cell degranulation
- D. Decreased production of leukotrienes (Correct Answer)
- E. Decreased IgE-mediated pro-inflammatory activity
Eicosanoid synthesis and function Explanation: ***Decreased production of leukotrienes***
- **Zileuton** is a **5-lipoxygenase inhibitor**. This enzyme is crucial for the synthesis of **leukotrienes** from arachidonic acid.
- By inhibiting 5-lipoxygenase, zileuton directly reduces the overall production of all types of leukotrienes, including LTB4, LTC4, LTD4, and LTE4.
*Decreased signaling via the leukotriene receptor*
- This describes the mechanism of action for **leukotriene receptor antagonists** (LTRAs) like montelukast and zafirlukast, which block leukotriene receptors.
- While zileuton ultimately reduces leukotriene effects, its direct and immediate action is on leukotriene synthesis, not receptor blockade.
*Decreased signaling via the muscarinic receptor*
- This is the mechanism of action for **anticholinergic bronchodilators** (e.g., ipratropium, tiotropium), which block the action of acetylcholine at muscarinic receptors.
- Zileuton does not act on the muscarinic receptor system.
*Decreased mast cell degranulation*
- This is the primary action of **mast cell stabilizers** like cromolyn and nedocromil, which prevent the release of inflammatory mediators from mast cells.
- While leukotrienes are involved in inflammation, zileuton's direct action is not on preventing mast cell degranulation itself but rather on blocking a pathway downstream from initial triggers.
*Decreased IgE-mediated pro-inflammatory activity*
- This describes the mechanism of action for **omalizumab**, a monoclonal antibody that targets IgE, preventing its binding to mast cells and basophils.
- Zileuton acts on the leukotriene synthesis pathway, independent of IgE-mediated processes.
Eicosanoid synthesis and function US Medical PG Question 8: A 59-year-old male with a 1-year history of bilateral knee arthritis presents with epigastric pain that intensifies with meals. He has been self-medicating with aspirin, taking up to 2,000 mg per day for the past six months. Which of the following medications, if taken instead of aspirin, could have minimized his risk of experiencing this epigastric pain?
- A. Naproxen
- B. Celecoxib (Correct Answer)
- C. Indomethacin
- D. Ibuprofen
- E. Ketorolac
Eicosanoid synthesis and function Explanation: ***Celecoxib***
- **Celecoxib** is a selective **COX-2 inhibitor**, which preferentially inhibits the COX-2 enzyme responsible for inflammation and pain, while largely sparing COX-1.
- Sparing **COX-1** reduces the inhibition of **prostaglandins** that protect the gastric mucosa, thereby lowering the risk of GI side effects like epigastric pain and ulcers compared to non-selective NSAIDs.
*Naproxen*
- **Naproxen** is a **non-selective NSAID** that inhibits both COX-1 and COX-2 enzymes.
- Inhibition of **COX-1** interferes with the production of protective prostaglandins in the stomach, increasing the risk of gastrointestinal adverse effects such as epigastric pain, ulcers, and bleeding, similar to aspirin.
*Indomethacin*
- **Indomethacin** is a potent **non-selective NSAID** with significant inhibition of both COX-1 and COX-2.
- Its strong **COX-1 inhibition** makes it particularly prone to causing gastrointestinal side effects including severe epigastric pain, nausea, and dyspepsia.
*Ibuprofen*
- **Ibuprofen** is a **non-selective NSAID** commonly used for pain and inflammation that inhibits both COX-1 and COX-2 enzymes.
- Although generally better tolerated than indomethacin or high-dose aspirin, it still carries a dose-dependent risk of **GI adverse effects** due to COX-1 inhibition.
*Ketorolac*
- **Ketorolac** is a potent **non-selective NSAID** primarily used for short-term management of acute moderate to severe pain.
- It has a high risk of **gastrointestinal complications**, including gastric ulcers and bleeding, making it unsuitable for long-term use and not a safer alternative to aspirin in terms of GI risk.
Eicosanoid synthesis and function US Medical PG Question 9: A researcher is studying how arachidonic acid metabolites mediate the inflammatory response in rats. She has developed multiple enzyme inhibitors that specifically target individual proteins in the arachidonic acid pathway. She injects these inhibitors in rats who have been exposed to common bacterial pathogens and analyzes their downstream effects. In one of her experiments, she injects a leukotriene B4 inhibitor into a rat and observes an abnormal cell response. Which of the following interleukins would most closely restore the function of one of the missing products?
- A. Interleukin 2
- B. Interleukin 4
- C. Interleukin 1
- D. Interleukin 5
- E. Interleukin 8 (Correct Answer)
Eicosanoid synthesis and function Explanation: ***Interleukin 8***
- **Leukotriene B4 (LTB4)** is a potent **chemoattractant** and activator of neutrophils.
- **Interleukin 8 (IL-8)**, also known as **CXCL8**, is a primary **chemoattractant** for neutrophils, functionally mimicking the role of LTB4 in recruiting these inflammatory cells to the site of infection.
*Interleukin 2*
- **IL-2** is primarily involved in the **growth, proliferation, and differentiation of T cells**, as well as the activation of B cells and natural killer cells.
- It does not have a significant role in **neutrophil chemotaxis**, which is the main function of LTB4.
*Interleukin 4*
- **IL-4** is crucial for **B cell activation** and class switching to IgE, and it's a key cytokine in the **Th2 immune response**.
- Its functions are related to **allergic reactions** and **parasitic infections**, not neutrophil recruitment.
*Interleukin 1*
- **IL-1** is a pro-inflammatory cytokine that mediates a wide range of immune responses, including **fever** and the activation of other immune cells.
- While it contributes to inflammation, it does not directly act as a **chemoattractant for neutrophils** in the same manner as LTB4 or IL-8.
*Interleukin 5*
- **IL-5** is primarily involved in the **growth and differentiation of eosinophils** and B cell IgA production.
- It plays a significant role in **allergic reactions** and defense against parasites, not neutrophil chemotaxis.
Eicosanoid synthesis and function US Medical PG Question 10: A 42-year-old woman comes to her primary care physician because of an irritating sensation in her nose. She noticed recently that there seems to be a lump in her nose. Her past medical history is significant for pain that seems to migrate around her body and is refractory to treatment. She has intermittently been taking a medication for the pain and recently increased the dose of the drug. Which of the following processes was most likely responsible for development of this patient's complaint?
- A. Decreased lipoxygenase pathway activity
- B. Increased mucous viscosity
- C. Increased lipoxygenase pathway activity (Correct Answer)
- D. Decreased prostaglandin activity
- E. Increased allergic reaction in mucosa
Eicosanoid synthesis and function Explanation: ***Increased lipoxygenase pathway activity***
- This patient likely has **aspirin-exacerbated respiratory disease (AERD)**, characterized by a triad of **asthma, aspirin sensitivity, and chronic rhinosinusitis with nasal polyposis**. The history of "pain that seems to migrate around her body and is refractory to treatment" suggests a chronic pain condition, for which she is taking a medication that exacerbates her nasal symptoms. This medication is likely a **NSAID**.
- **NSAIDs** inhibit **cyclooxygenase (COX) enzymes**, shunting arachidonic acid metabolism towards the **lipoxygenase pathway**. This leads to an overproduction of **leukotrienes**, which are potent bronchoconstrictors and promoters of inflammation and nasal polyp formation.
*Decreased lipoxygenase pathway activity*
- A decrease in lipoxygenase pathway activity would generally lead to **reduced leukotriene production**, which would typically *alleviate* symptoms like nasal irritation and polyp formation, not cause them.
- This scenario would likely improve rather than worsen respiratory and allergic symptoms, making it inconsistent with the patient's presentation.
*Increased mucous viscosity*
- While increased mucous viscosity can contribute to nasal congestion and discomfort, it is a **symptom or consequence** of underlying inflammation, not the primary pathophysiological cause in AERD.
- It does not explain the specific link to aspirin/NSAID use and the formation of **nasal polyps**.
*Decreased prostaglandin activity*
- **Decreased prostaglandin activity** is caused by **NSAID inhibition of COX enzymes**. While this is a crucial step in AERD, it is the *consequence* (shunting to lipoxygenase pathway) rather than the direct cause of the nasal polyps.
- The direct cause of the patient's nasal obstruction and pain from the ASA is the **overproduction of leukotrienes**, not merely the absence of prostaglandins.
*Increased allergic reaction in mucosa*
- While AERD involves mast cell activation and eosinophilic inflammation, it is not primarily an **IgE-mediated allergic reaction** in the classical sense.
- The trigger is **pharmacological (NSAIDs)**, not an environmental allergen, and the underlying mechanism is an imbalance in arachidonic acid metabolism rather than a specific antigen-antibody interaction.
More Eicosanoid synthesis and function US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.