Adipose tissue metabolism US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Adipose tissue metabolism. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Adipose tissue metabolism US Medical PG Question 1: A 15-year-old boy is brought to the emergency department by his father 10 minutes after falling into a frozen lake during ice fishing. He was in the water for less than 1 minute before his father managed to pull him out. On arrival, his clothes are still wet and he appears scared. His body temperature is 36.2°C (97.1°F), pulse is 102/min, blood pressure is 133/88 mm Hg. Which of the following mechanisms contributes most to maintaining this patient's core body temperature?
- A. Inhibition of the thyroid axis
- B. Involuntary muscular contractions (Correct Answer)
- C. Activation of thermogenin
- D. Increase in hypothalamic set point
- E. Contraction of arrector pili muscles
Adipose tissue metabolism Explanation: ***Involuntary muscular contractions***
- **Shivering** is the body's primary mechanism for increasing heat production in response to cold stress, involving rapid, involuntary muscle contractions to generate heat.
- This process significantly increases the **metabolic rate** and heat output, crucial for maintaining core body temperature when exposed to cold environments.
*Inhibition of the thyroid axis*
- The **thyroid axis** is generally activated in response to chronic cold exposure to increase basal metabolic rate, not inhibited.
- Inhibition of thyroid hormones would lead to a decrease in metabolism and heat production, worsening hypothermia.
*Activation of thermogenin*
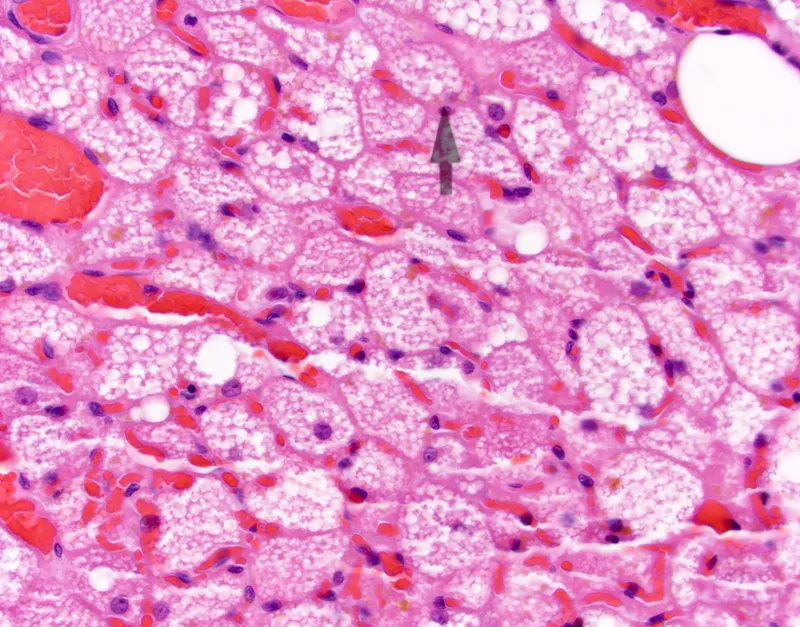
- **Thermogenin** (uncoupling protein 1) is found primarily in **brown adipose tissue** and its activation leads to non-shivering thermogenesis.
- While present in infants and some adults, shivering is a much more significant and rapid response to acute cold in a 15-year-old.
*Increase in hypothalamic set point*
- An increase in the **hypothalamic set point** is characteristic of **fever**, where the body aims to achieve a higher temperature.
- In this scenario, the body is trying to maintain its normal set point despite cold exposure, not raise it.
*Contraction of arrector pili muscles*
- **Contraction of arrector pili muscles** causes **piloerection** (goosebumps), which traps a layer of air close to the skin.
- While contributing to insulation, this mechanism is relatively minor in humans compared to the heat generated by shivering.
Adipose tissue metabolism US Medical PG Question 2: A 24-year-old man presents for an annual check-up. He is a bodybuilder and tells you he is on a protein-rich diet that only allows for minimal carbohydrate intake. His friend suggests he try exogenous glucagon to help him lose some excess weight before an upcoming competition. Which of the following effects of glucagon is he attempting to exploit?
- A. Increased glucose utilization by tissues
- B. Decreased blood cholesterol level
- C. Increased hepatic gluconeogenesis
- D. Increased lipolysis in adipose tissues (Correct Answer)
- E. Increased hepatic glycogenolysis
Adipose tissue metabolism Explanation: ***Increased lipolysis in adipose tissues***
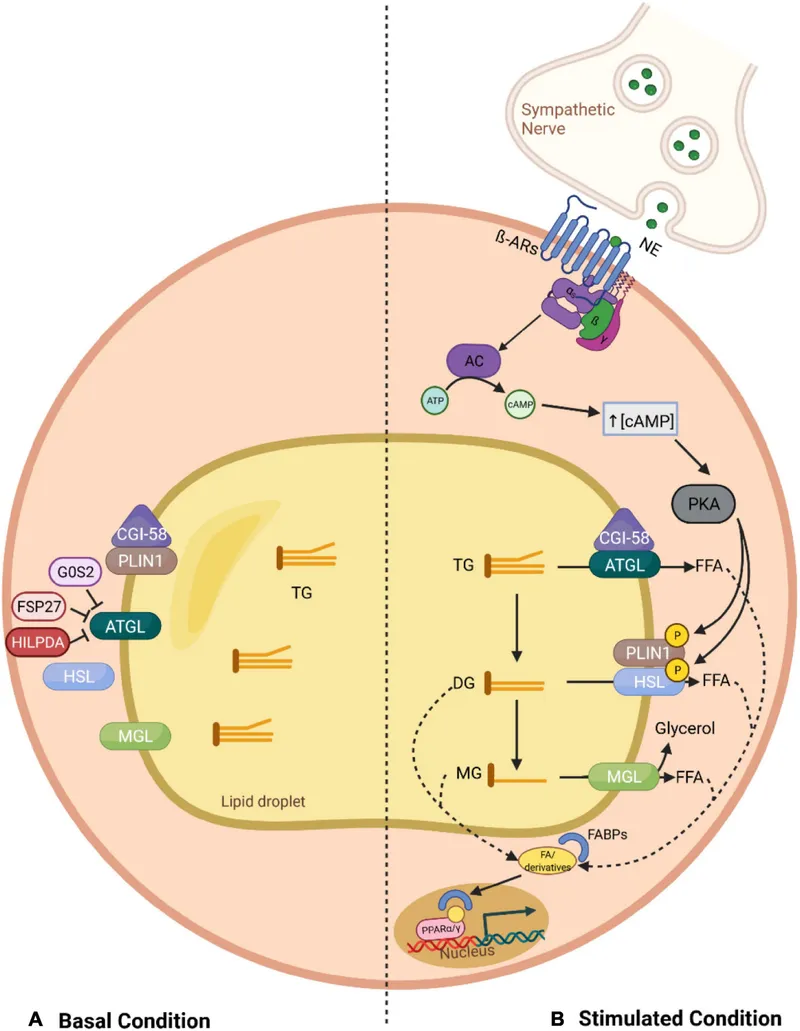
- While **glucagon's primary target is the liver**, it can have **modest lipolytic effects** on adipose tissue by opposing insulin's anti-lipolytic actions.
- Glucagon stimulates cAMP production, which can activate **hormone-sensitive lipase** to break down triglycerides into **fatty acids** and **glycerol**.
- However, **catecholamines (epinephrine/norepinephrine)** are far more potent direct stimulators of adipose tissue lipolysis than glucagon.
- The friend is attempting to exploit this lipolytic effect for fat loss, though **exogenous glucagon is not an evidence-based or safe weight-loss strategy**.
*Increased glucose utilization by tissues*
- This is **opposite** to glucagon's actual effect. **Glucagon raises blood glucose** levels; it does not promote glucose uptake by peripheral tissues.
- **Insulin** is the hormone responsible for promoting glucose uptake and utilization by muscle, adipose, and other tissues.
*Decreased blood cholesterol level*
- Glucagon does not have a direct, clinically significant effect on reducing blood cholesterol levels.
- While glucagon affects overall lipid metabolism through its catabolic actions, it is not used therapeutically for hypercholesterolemia.
*Increased hepatic gluconeogenesis*
- **Glucagon strongly stimulates hepatic gluconeogenesis**, which is the synthesis of glucose from non-carbohydrate precursors (amino acids, lactate, glycerol) in the liver.
- This action **raises blood glucose** levels and would not directly contribute to fat loss or weight reduction.
- In the context of a low-carbohydrate diet, increased gluconeogenesis would maintain blood glucose but not promote the fat loss the bodybuilder seeks.
*Increased hepatic glycogenolysis*
- **Glucagon is a potent stimulator of hepatic glycogenolysis**, the breakdown of stored liver glycogen into glucose.
- This rapidly increases blood glucose levels during fasting or hypoglycemia.
- However, this does not directly target adipose tissue for fat loss; it mobilizes glucose stores rather than fat stores, so it's not the mechanism relevant to weight loss goals.
Adipose tissue metabolism US Medical PG Question 3: A 46-year-old man comes to the physician for a follow-up examination. He has type 2 diabetes mellitus and hypertension. Current medications include metformin and lisinopril. He reports that he has adhered to his diet and medication regimen. His hemoglobin A1c is 8.6%. Insulin glargine is added to his medication regimen. Which of the following sets of changes is most likely to occur in response to this new medication?
$$$ Glycolysis %%% Glycogenesis %%% Lipolysis %%% Gluconeogenesis $$$
- A. ↓ ↓ ↑ ↑
- B. ↑ ↓ ↑ ↓
- C. ↓ ↑ ↓ ↑
- D. ↑ ↑ ↓ ↓ (Correct Answer)
- E. ↑ ↓ ↑ ↑
Adipose tissue metabolism Explanation: ***↑ ↑ ↓ ↓***
- Insulin **increases glucose utilization** by promoting glycolysis and increases glucose storage by promoting glycogenesis.
- Insulin **inhibits glucose production** by decreasing lipolysis and gluconeogenesis.
*↓ ↓ ↑ ↑*
- This option incorrectly suggests that insulin would decrease glycolysis and glycogenesis, which are pathways for glucose utilization and storage.
- It also incorrectly suggests that insulin would increase lipolysis and gluconeogenesis, which are pathways for glucose production.
*↑ ↓ ↑ ↓*
- This option correctly indicates an increase in glycolysis and a decrease in gluconeogenesis, but incorrectly suggests a decrease in glycogenesis and an increase in lipolysis.
- Insulin's primary role is to lower blood glucose, which involves promoting both glucose utilization (glycolysis) and storage (glycogenesis).
*↓ ↑ ↓ ↑*
- This option incorrectly suggests a decrease in glycolysis and an increase in gluconeogenesis, which would lead to higher blood glucose.
- While it correctly shows an increase in glycogenesis and a decrease in lipolysis, the overall pattern does not match insulin's coordinated metabolic effects.
*↑ ↓ ↑ ↑*
- This option incorrectly suggests a decrease in glycogenesis and an increase in lipolysis and gluconeogenesis, which would lead to higher blood glucose.
- Insulin's main actions are to promote glucose uptake and storage and to inhibit glucose production.
Adipose tissue metabolism US Medical PG Question 4: A 10-month-old boy with a seizure disorder is brought to the physician by his mother because of a 2-day history of vomiting and lethargy. Laboratory studies show a decreased serum glucose concentration with low ketones. Further testing confirms a deficiency in an enzyme involved in fatty acid oxidation. Which of the following enzymes is most likely deficient in this patient?
- A. Acyl-CoA dehydrogenase (Correct Answer)
- B. HMG-CoA reductase
- C. Glycerol kinase
- D. Acetyl-CoA carboxylase
- E. Glycerol-3-phosphate dehydrogenase
Adipose tissue metabolism Explanation: ***Acyl-CoA dehydrogenase***
- The combination of **hypoglycemia** with **low ketones** in a setting of prolonged vomiting (stress) strongly suggests a **disorder of fatty acid oxidation**. These disorders impair the body's ability to produce ketones when glucose stores are low.
- **Acyl-CoA dehydrogenase** is a key enzyme in the mitochondrial β-oxidation of fatty acids. A deficiency prevents the breakdown of fatty acids into acetyl-CoA, which is necessary for ketogenesis and to fuel gluconeogenesis indirectly.
*HMG-CoA reductase*
- This enzyme is involved in **cholesterol synthesis**, not directly in fatty acid oxidation or ketone body formation from fatty acids.
- Deficiency would primarily affect cholesterol levels and not typically present with the described metabolic crisis of hypoglycemia and low ketones.
*Glycerol kinase*
- **Glycerol kinase** phosphorylates glycerol, a product of triglyceride hydrolysis, allowing it to enter glycolysis or gluconeogenesis.
- A deficiency would impair glycerol utilization but would not directly impact fatty acid oxidation pathways that are critical for ketone production during hypoglycemia.
*Acetyl-CoA carboxylase*
- **Acetyl-CoA carboxylase** is the rate-limiting enzyme in **fatty acid synthesis**, not degradation.
- A deficiency would lead to impaired fatty acid synthesis, which is the opposite of the metabolic problem described (impaired breakdown of fatty acids).
*Glycerol-3-phosphate dehydrogenase*
- This enzyme is involved in the conversion of **dihydroxyacetone phosphate (DHAP)** to **glycerol-3-phosphate** in both triglyceride synthesis and the glycerol phosphate shuttle.
- While related to lipid metabolism, a deficiency would not directly cause the severe hypoglycemia and hypoketosis seen with a fatty acid oxidation defect.
Adipose tissue metabolism US Medical PG Question 5: A 22-year-old medical student decides to fast for 24 hours after reading about the possible health benefits of fasting. She read that blood glucose levels are maintained by metabolic processes such as hepatic glycogenolysis and hepatic gluconeogenesis during the initial 3 days of fasting. During the day, she did not suffer from the symptoms of hypoglycemia. Which of the following signaling molecules most likely stimulated the reaction which maintained her blood glucose after all her stored glucose was broken down and used up?
- A. Adenosine diphosphate
- B. Acetyl CoA (Correct Answer)
- C. Acetate
- D. Citrate
- E. Adenosine monophosphate
Adipose tissue metabolism Explanation: ***Acetyl CoA***
- **Acetyl CoA** is the key **allosteric activator of pyruvate carboxylase**, the first committed enzyme of gluconeogenesis that converts pyruvate to oxaloacetate.
- During prolonged fasting after glycogen stores are depleted, the body shifts to **fatty acid oxidation** (β-oxidation), which produces large amounts of **Acetyl CoA**.
- High **Acetyl CoA** levels signal that fat is being oxidized for energy, and simultaneously **activate gluconeogenesis** to maintain blood glucose for glucose-dependent tissues (brain, RBCs).
- This is the primary signaling mechanism that directly stimulates the gluconeogenic pathway after glycogen is exhausted.
*Adenosine monophosphate (AMP)*
- **AMP** levels rise during energy depletion and activate **AMP-activated protein kinase (AMPK)**.
- However, AMPK **inhibits gluconeogenesis** (not stimulates it) because gluconeogenesis is an **ATP-consuming** anabolic process (requires 6 ATP per glucose).
- AMPK promotes ATP-generating catabolic processes like fatty acid oxidation, but suppresses ATP-consuming processes like gluconeogenesis and fatty acid synthesis.
*Adenosine diphosphate (ADP)*
- **ADP** accumulates when ATP is hydrolyzed and signals moderate energy deficit.
- ADP is primarily a substrate for ATP regeneration via oxidative phosphorylation and does not directly regulate gluconeogenesis.
- Its role in metabolic regulation is less specific than allosteric activators like Acetyl CoA.
*Acetate*
- **Acetate** can be converted to Acetyl CoA but is not a direct signaling molecule for gluconeogenesis.
- It is a minor metabolite that may be produced in specific conditions (e.g., alcohol metabolism, ketoacidosis) but does not play a primary role in fasting-induced glucose homeostasis.
*Citrate*
- **Citrate** is a Krebs cycle intermediate that inhibits **phosphofructokinase-1 (PFK-1)** in glycolysis, thus reducing glucose breakdown.
- While citrate inhibition of glycolysis indirectly favors gluconeogenesis by preventing futile cycling, citrate does not **directly activate** gluconeogenic enzymes.
- Citrate primarily signals energy sufficiency and promotes fatty acid synthesis in the fed state, not fasting gluconeogenesis.
Adipose tissue metabolism US Medical PG Question 6: A 42-year-old woman comes to the physician for a routine health maintenance examination. She has generalized fatigue and has had difficulties doing her household duties for the past 3 months. She has eczema and gastroesophageal reflux disease. She has a history of using intravenous methamphetamine in her youth but has not used illicit drugs in 23 years. Her medications include topical clobetasol and pantoprazole. She is 160 cm (5 ft 3 in) tall and weighs 105 kg (231 lb); BMI is 42 kg/m2. Her temperature is 37°C (98.6°F), pulse is 95/min, and blood pressure is 145/90 mm Hg. The lungs are clear to auscultation. Cardiac examination shows no abnormalities. Pelvic examination shows a normal vagina and cervix. Laboratory studies show:
Hemoglobin 13.1 g/dL
Leukocyte count 7,800/mm3
Platelet count 312,000/mm3
Serum
Na+ 141 mEq/L
K+ 4.6 mEq/L
Cl- 98 mEq/L
Urea nitrogen 12 mg/dL
Fasting glucose 110 mg/dL
Creatinine 0.8 mg/dL
Total cholesterol 269 mg/dL
HDL-cholesterol 55 mg/dL
LDL-cholesterol 160 mg/dL
Triglycerides 320 mg/dL
Urinalysis is within normal limits. An x-ray of the chest shows no abnormalities. She has not lost any weight over the past year despite following supervised weight loss programs, including various diets and exercise regimens. Which of the following is the most appropriate next step in management of this patient?
- A. Phentermine and topiramate therapy and follow-up in 3 months
- B. Bariatric surgery (Correct Answer)
- C. Liposuction
- D. Behavioral therapy
- E. Metformin and statin therapy and follow-up in 3 months
Adipose tissue metabolism Explanation: ***Bariatric surgery***
- This patient has **severe obesity** (BMI of 42 kg/m²) with obesity-related comorbidities including **hypertension** (BP 145/90 mm Hg), **dyslipidemia** (elevated cholesterol and triglycerides), and **pre-diabetes** (fasting glucose 110 mg/dL), and has failed multiple supervised weight loss programs. **Bariatric surgery** is indicated for patients with BMI ≥ 40 kg/m² or BMI ≥ 35 kg/m² with obesity-related comorbidities who have failed at least 6 months of supervised weight loss.
- It is the most effective treatment for sustained weight loss in patients with **severe obesity**, leading to significant improvement or resolution of comorbidities.
*Phentermine and topiramate therapy and follow-up in 3 months*
- While medication can aid weight loss, this patient's **BMI of 42 kg/m²** signifies severe obesity, where medication alone is often insufficient for sustained and significant weight reduction.
- **Pharmacotherapy** is typically considered for BMI ≥ 30 kg/m² or BMI ≥ 27 kg/m² with comorbidities, but for class III obesity (BMI ≥ 40 kg/m²), bariatric surgery generally provides superior and more lasting outcomes.
*Liposuction*
- **Liposuction** is primarily a cosmetic procedure for localized fat removal and is not an effective treatment for generalized severe obesity or weight loss, nor does it address the metabolic complications of obesity.
- It does not lead to sustained weight loss or improvement in obesity-related comorbidities like **hypertension** and **dyslipidemia**.
*Behavioral therapy*
- The patient has already attempted multiple supervised weight loss programs, including various diets and exercise regimens, suggesting that **behavioral therapy** alone has not been effective for sustained weight loss in her case.
- While beneficial as part of a comprehensive approach, it is unlikely to achieve the significant and sustained weight loss required for a patient with **severe obesity** that has failed prior conventional methods.
*Metformin and statin therapy and follow-up in 3 months*
- **Metformin** and **statin therapy** target specific comorbidities (pre-diabetes/insulin resistance and dyslipidemia, respectively) but do not address the underlying **severe obesity**.
- While these medications are important for managing aspects of her metabolic syndrome, they are not a primary treatment for weight loss and will not lead to significant weight reduction in a patient with a **BMI of 42 kg/m²**.
Adipose tissue metabolism US Medical PG Question 7: A startup is working on a novel project in which they claim they can replicate the organelle that is defective in MELAS syndrome. Which of the following metabolic processes must they be able to replicate if their project is to mimic the metabolic processes of this organelle?
- A. Hexose monophosphate shunt
- B. Cholesterol synthesis
- C. Glycolysis
- D. Fatty acid (beta) oxidation (Correct Answer)
- E. Fatty acid synthesis
Adipose tissue metabolism Explanation: ***Fatty acid (beta) oxidation***
- **MELAS syndrome** (Mitochondrial Encephalomyopathy, Lactic Acidosis, and Stroke-like episodes) is caused by defects in **mitochondrial function**.
- **Beta-oxidation of fatty acids** is a crucial metabolic process that occurs within the mitochondria, generating ATP.
*Hexose monophosphate shunt*
- The **hexose monophosphate shunt** (pentose phosphate pathway) occurs in the **cytosol** and is primarily involved in producing NADPH and synthesizing nucleotides, not a primary mitochondrial function.
- Its dysfunction is not directly linked to the core metabolic defects seen in MELAS syndrome.
*Cholesterol synthesis*
- **Cholesterol synthesis** primarily occurs in the **cytosol** and the **endoplasmic reticulum**, not within the mitochondria.
- While cholesterol metabolism can be indirectly affected by mitochondrial health, it is not a direct mitochondrial metabolic pathway.
*Glycolysis*
- **Glycolysis** is the metabolic pathway that converts glucose into pyruvate, occurring in the **cytosol**.
- Although it precedes mitochondrial oxidative phosphorylation, glycolysis itself does not occur within the mitochondria.
*Fatty acid synthesis*
- **Fatty acid synthesis** primarily takes place in the **cytosol** and endoplasmic reticulum, utilizing NADPH from the hexose monophosphate shunt.
- It is an anabolic process, while MELAS typically involves defects in catabolic/energy-producing mitochondrial pathways.
Adipose tissue metabolism US Medical PG Question 8: You have been asked to deliver a lecture to medical students about the effects of various body hormones and neurotransmitters on the metabolism of glucose. Which of the following statements best describes the effects of sympathetic stimulation on glucose metabolism?
- A. Norepinephrine causes increased glucose absorption within the intestines.
- B. Without epinephrine, insulin cannot act on the liver.
- C. Peripheral tissues require epinephrine to take up glucose.
- D. Epinephrine increases liver glycogenolysis. (Correct Answer)
- E. Sympathetic stimulation to alpha receptors of the pancreas increases insulin release.
Adipose tissue metabolism Explanation: ***Epinephrine increases liver glycogenolysis.***
- **Epinephrine**, released during sympathetic stimulation, primarily acts to increase **glucose availability** for immediate energy.
- It achieves this by stimulating **glycogenolysis** (breakdown of glycogen into glucose) in the liver via **beta-adrenergic receptors**.
*Norepinephrine causes increased glucose absorption within the intestines.*
- **Norepinephrine** primarily causes **vasoconstriction** and can *decrease* **intestinal motility** and nutrient absorption due to shunting blood away from the digestive tract during stress.
- Glucose absorption is mainly regulated by digestive enzymes and transport proteins, not directly increased by norepinephrine.
*Without epinephrine, insulin cannot act on the liver.*
- **Insulin** acts on the liver independent of epinephrine to promote **glucose uptake**, **glycogenesis**, and **lipid synthesis**.
- Epinephrine and insulin have **antagonistic effects** on liver glucose metabolism; epinephrine increases glucose output, while insulin decreases it.
*Peripheral tissues require epinephrine to take up glucose.*
- **Insulin** is the primary hormone required for **glucose uptake** by most peripheral tissues, especially **muscle** and **adipose tissue**, via **GLUT4 transporters**.
- Epinephrine generally *reduces* glucose uptake by peripheral tissues to preserve glucose for the brain during stress.
*Sympathetic stimulation to alpha receptors of the pancreas increases insulin release.*
- Sympathetic stimulation, primarily acting through **alpha-2 adrenergic receptors** on pancreatic beta cells, actually **inhibits** **insulin secretion**.
- This inhibition helps to increase blood glucose levels by reducing insulin's glucose-lowering effects.
Adipose tissue metabolism US Medical PG Question 9: A 35-year-old man comes to the physician because of fatigue and generalized weakness for the past year. He has noticed he has been having fewer bowel movements. He has had pain with defecation and small amounts of blood when wiping. He has not lost weight despite increased efforts to diet and exercise. He has had no fever, throat pain, or difficulty swallowing. His temperature is 36.5°C (97.7°F), pulse is 50/min, blood pressure is 120/90 mm Hg, and BMI is 35 kg/m2. Physical examination shows dry skin and a distended abdomen. There is 1+ pitting edema in the lower extremities. On neurological examination, deep tendon reflexes are 1+. Further evaluation of this patient is most likely to show which of the following findings?
- A. Hyperglycemia
- B. Decreased serum creatinine
- C. Elevated serum low-density lipoprotein (Correct Answer)
- D. Decreased plasma homocysteine concentrations
- E. Decreased serum creatine kinase
Adipose tissue metabolism Explanation: ***Elevated serum low-density lipoprotein***
- The patient's symptoms (fatigue, generalized weakness, constipation, weight gain despite efforts, cold intolerance implied by dry skin, bradycardia, and edema) are highly suggestive of **hypothyroidism**.
- **Hypothyroidism** classically leads to **hyperlipidemia**, specifically elevated **LDL cholesterol**, due to decreased catabolism of cholesterol.
*Decreased serum creatine kinase*
- **Hypothyroidism** typically causes **myopathy**, which can manifest as elevated, not decreased, serum **creatine kinase** levels.
- Muscle weakness and fatigue in hypothyroidism are often associated with muscle damage and elevated CK.
*Hyperglycemia*
- While hypothyroidism can impact glucose metabolism, it more commonly leads to **insulin resistance** and can contribute to **hyperglycemia**, but it is not a direct or consistent consequence, and other factors are often more significant.
- However, hypothyroidism is not primarily characterized by hyperglycemia as a direct pathognomonic finding.
*Decreased serum creatinine*
- **Hypothyroidism** is typically associated with **decreased glomerular filtration rate (GFR)**, which can lead to **increased serum creatinine**, not decreased.
- A decreased GFR would imply reduced clearance of creatinine, thus elevating its serum concentration.
*Decreased plasma homocysteine concentrations*
- **Hypothyroidism** is linked to **elevated plasma homocysteine** concentrations, likely due to impaired metabolism (e.g., reduced activity of methionine synthase).
- High homocysteine levels are a risk factor for cardiovascular disease.
Adipose tissue metabolism US Medical PG Question 10: A 55-year-old woman presents to a primary care clinic for a physical evaluation. She works as a software engineer, travels frequently, is married with 2 kids, and drinks alcohol occasionally. She does not exercise regularly. She currently does not take any medications except for occasional ibuprofen or acetaminophen. She is currently undergoing menopause. Her initial vital signs reveal that her blood pressure is 140/95 mmHg and heart rate is 75/min. She weighs 65 kg (143 lb) and is 160 cm (63 in) tall. Her physical exam is unremarkable. A repeat measurement of her blood pressure is the same as before. Among various laboratory tests for hypertension evaluation, the physician requests fasting glucose and hemoglobin A1c levels. Which of the following is the greatest risk factor for type 2 diabetes mellitus?
- A. Menopause
- B. Occupation
- C. Age
- D. Body mass index (Correct Answer)
- E. Hypertension
Adipose tissue metabolism Explanation: ***Body mass index***
- The patient's **BMI** is 25.4 kg/m², which falls into the **overweight** category (BMI 25-29.9 kg/m²). **Obesity** (BMI ≥ 30 kg/m²) and overweight status are significant and modifiable risk factors for **insulin resistance** and type 2 diabetes mellitus.
- Excess body fat, particularly **visceral fat**, leads to increased free fatty acid release and inflammation, impairing insulin signaling in target tissues.
*Menopause*
- While menopause can lead to changes in **body fat distribution** and increase the risk of metabolic syndrome components, it is not as strong a direct risk factor for type 2 diabetes as BMI.
- The hormonal shifts during menopause may contribute to **insulin resistance** but do not independently confer as high a risk as overweight or obesity.
*Occupation*
- The patient's occupation as a **software engineer** and frequent travel may contribute to a sedentary lifestyle, which is an indirect risk factor for obesity and diabetes. However, occupation itself is not a direct or primary biological risk factor.
- A sedentary lifestyle decreases **metabolic demand** and can lead to weight gain if not balanced with regular physical activity.
*Age*
- **Advancing age** is a known risk factor for type 2 diabetes due to a gradual decline in pancreatic beta-cell function and increased insulin resistance over time.
- While the patient's age (55) is a risk factor, her elevated **BMI** represents a more immediate and modifiable risk for developing the disease.
*Hypertension*
- **Hypertension** is often a comorbidity of type 2 diabetes and part of the **metabolic syndrome**, but it is generally considered a consequence or co-existing condition rather than the primary risk factor for the development of diabetes itself.
- Both hypertension and type 2 diabetes share common pathophysiological mechanisms such as **insulin resistance** and inflammation.
More Adipose tissue metabolism US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.