Rate-limiting enzymes and control points US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Rate-limiting enzymes and control points. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Rate-limiting enzymes and control points US Medical PG Question 1: A 20-year-old male with no significant medical history comes to you with a urine positive for fructose. He does not have diabetes mellitus. Which enzyme is most likely to be deficient in this patient?
- A. Pyruvate kinase
- B. Lactase
- C. Fructokinase (Correct Answer)
- D. Aldolase B
Rate-limiting enzymes and control points Explanation: ***Fructokinase***
- A urine positive for **fructose** without symptoms of diabetes mellitus (i.e., **benign fructosuria**) is characteristic of a **fructokinase deficiency**.
- **Fructokinase** is the enzyme responsible for the first step in fructose metabolism, converting **fructose to fructose-1-phosphate**.
*Pyruvate kinase*
- Deficiency of **pyruvate kinase** primarily affects **glycolysis** in red blood cells and leads to **hemolytic anemia**, not fructosuria.
- This enzyme converts **phosphoenolpyruvate to pyruvate**.
*Lactase*
- **Lactase** is an enzyme that digests **lactose** (milk sugar) into glucose and galactose.
- A deficiency in lactase causes **lactose intolerance**, presenting with gastrointestinal symptoms like bloating and diarrhea after consuming dairy products, not fructose in the urine.
*Aldolase B*
- A deficiency in **aldolase B** leads to **hereditary fructose intolerance**, a severe condition where **fructose-1-phosphate accumulates** after fructose ingestion.
- This typically presents with symptoms such as **hypoglycemia**, vomiting, jaundice, and liver damage, which are not described in this benign case of fructosuria.
Rate-limiting enzymes and control points US Medical PG Question 2: A 45-year-old woman with type 1 diabetes mellitus is brought to the emergency department by her husband because of polyuria, nausea, vomiting, and altered mental status for 4 hours. On arrival, she is unconscious. Treatment with a drug is begun that increases glucose transport to skeletal muscle and adipose tissue. Which of the following cellular events is most likely to also occur in response to this drug?
- A. Dephosphorylation of fructose-1,6-bisphosphatase (Correct Answer)
- B. Increased activity of acyl-CoA dehydrogenases
- C. Cleavage of UDP from UDP-glucose
- D. Upregulation of glucose transporter type 3 expression
- E. Phosphorylation of glycogen phosphorylase kinase
Rate-limiting enzymes and control points Explanation: ***Dephosphorylation of fructose-1,6-bisphosphatase***
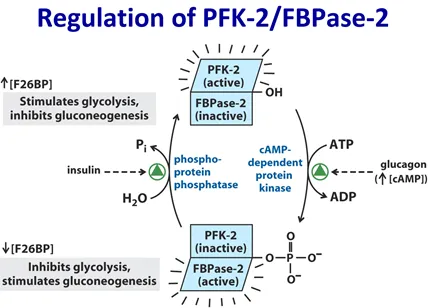
- The patient is in diabetic ketoacidosis (DKA), and the drug administered is insulin
- Insulin promotes glucose utilization and storage, which involves inhibiting gluconeogenesis through the dephosphorylation and inactivation of fructose-1,6-bisphosphatase
- This is a key regulatory mechanism by which insulin suppresses hepatic glucose production
*Increased activity of acyl-CoA dehydrogenases*
- This enzyme is crucial for fatty acid oxidation, a process that is inhibited by insulin
- In DKA, fatty acid oxidation is elevated, leading to ketone body production, but insulin treatment reduces this activity
*Cleavage of UDP from UDP-glucose*
- This reaction occurs in the synthesis of glycogen from UDP-glucose by glycogen synthase, which is activated by insulin
- While insulin stimulates glycogen synthesis, the direct cleavage of UDP from UDP-glucose is part of the synthetic process, not a primary regulatory cellular event caused by insulin in the context of DKA treatment
*Upregulation of glucose transporter type 3 expression*
- Glucose transporter type 3 (GLUT3) is primarily found in neurons and has a high affinity for glucose, with its expression generally not significantly regulated by insulin
- Insulin primarily promotes GLUT4 translocation to the cell membrane in muscle and adipose tissue to increase glucose uptake
*Phosphorylation of glycogen phosphorylase kinase*
- Phosphorylation of glycogen phosphorylase kinase activates it, subsequently activating glycogen phosphorylase and promoting glycogen breakdown (glycogenolysis)
- Insulin inhibits glycogenolysis and promotes glycogen synthesis, meaning insulin would deactivate glycogen phosphorylase kinase through dephosphorylation
Rate-limiting enzymes and control points US Medical PG Question 3: A 12-year-old boy and his siblings are referred to a geneticist for evaluation of a mild but chronic hemolytic anemia that has presented with fatigue, splenomegaly, and scleral icterus. Coombs test is negative and blood smear does not show any abnormal findings. An enzymatic panel is assayed, and pyruvate kinase is found to be mutated on both alleles. The geneticist explains that pyruvate kinase functions in glycolysis and is involved in a classic example of feed-forward regulation. Which of the following metabolites is able to activate pyruvate kinase?
- A. Fructose-1,6-bisphosphate (Correct Answer)
- B. Alanine
- C. ATP
- D. Glucose-6-phosphate
- E. Glyceraldehyde-3-phosphate
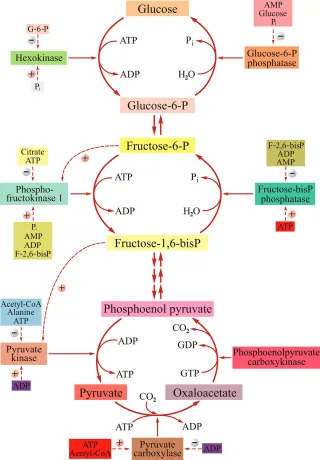
Rate-limiting enzymes and control points Explanation: ***Fructose-1,6-bisphosphate***
- **Fructose-1,6-bisphosphate** is a potent **allosteric activator** of pyruvate kinase. This is an example of **feed-forward activation**, where a product of an early irreversible step in glycolysis (catalyzed by phosphofructokinase-1) activates a later enzyme (pyruvate kinase) in the pathway.
- This activation ensures that substrates for the later steps of glycolysis are rapidly utilized when earlier steps are highly active, matching the rate of metabolite flow and increasing the overall efficiency of glycolysis for energy production.
*Alanine*
- **Alanine** is an **inhibitor** of pyruvate kinase, not an activator. It serves as an indicator of a high cellular energy state and ample amino acid supply.
- High levels of alanine signal the cell that there is sufficient energy and building blocks, thus **shutting down** glycolysis at the pyruvate kinase step to conserve glucose for other needs like glycogen synthesis.
*ATP*
- **ATP** (adenosine triphosphate) is an **allosteric inhibitor** of pyruvate kinase. High ATP levels signal a high energy state in the cell.
- When the cell has sufficient energy, ATP binds to a regulatory site on pyruvate kinase, reducing its activity and **slowing down glycolysis** to prevent overproduction of ATP.
*Glucose-6-phosphate*
- **Glucose-6-phosphate** is an intermediate in glycolysis but does not directly activate pyruvate kinase. It can act as an allosteric inhibitor of hexokinase, the first enzyme in glycolysis, but not pyruvate kinase.
- Its accumulation typically signifies a **backup** in the glycolytic pathway (e.g., due to downstream inhibition), leading to a *reduction* in overall glucose flux rather than a direct activation of pyruvate kinase.
*Glyceraldehyde-3-phosphate*
- **Glyceraldehyde-3-phosphate** is an intermediate in glycolysis, but it does not directly activate pyruvate kinase. It is a substrate for glyceraldehyde-3-phosphate dehydrogenase.
- While its presence indicates active glycolysis, it does not exert a specific allosteric regulatory effect on pyruvate kinase in the way fructose-1,6-bisphosphate does.
Rate-limiting enzymes and control points US Medical PG Question 4: A 22-year-old medical student decides to fast for 24 hours after reading about the possible health benefits of fasting. She read that blood glucose levels are maintained by metabolic processes such as hepatic glycogenolysis and hepatic gluconeogenesis during the initial 3 days of fasting. During the day, she did not suffer from the symptoms of hypoglycemia. Which of the following signaling molecules most likely stimulated the reaction which maintained her blood glucose after all her stored glucose was broken down and used up?
- A. Adenosine diphosphate
- B. Acetyl CoA (Correct Answer)
- C. Acetate
- D. Citrate
- E. Adenosine monophosphate
Rate-limiting enzymes and control points Explanation: ***Acetyl CoA***
- **Acetyl CoA** is the key **allosteric activator of pyruvate carboxylase**, the first committed enzyme of gluconeogenesis that converts pyruvate to oxaloacetate.
- During prolonged fasting after glycogen stores are depleted, the body shifts to **fatty acid oxidation** (β-oxidation), which produces large amounts of **Acetyl CoA**.
- High **Acetyl CoA** levels signal that fat is being oxidized for energy, and simultaneously **activate gluconeogenesis** to maintain blood glucose for glucose-dependent tissues (brain, RBCs).
- This is the primary signaling mechanism that directly stimulates the gluconeogenic pathway after glycogen is exhausted.
*Adenosine monophosphate (AMP)*
- **AMP** levels rise during energy depletion and activate **AMP-activated protein kinase (AMPK)**.
- However, AMPK **inhibits gluconeogenesis** (not stimulates it) because gluconeogenesis is an **ATP-consuming** anabolic process (requires 6 ATP per glucose).
- AMPK promotes ATP-generating catabolic processes like fatty acid oxidation, but suppresses ATP-consuming processes like gluconeogenesis and fatty acid synthesis.
*Adenosine diphosphate (ADP)*
- **ADP** accumulates when ATP is hydrolyzed and signals moderate energy deficit.
- ADP is primarily a substrate for ATP regeneration via oxidative phosphorylation and does not directly regulate gluconeogenesis.
- Its role in metabolic regulation is less specific than allosteric activators like Acetyl CoA.
*Acetate*
- **Acetate** can be converted to Acetyl CoA but is not a direct signaling molecule for gluconeogenesis.
- It is a minor metabolite that may be produced in specific conditions (e.g., alcohol metabolism, ketoacidosis) but does not play a primary role in fasting-induced glucose homeostasis.
*Citrate*
- **Citrate** is a Krebs cycle intermediate that inhibits **phosphofructokinase-1 (PFK-1)** in glycolysis, thus reducing glucose breakdown.
- While citrate inhibition of glycolysis indirectly favors gluconeogenesis by preventing futile cycling, citrate does not **directly activate** gluconeogenic enzymes.
- Citrate primarily signals energy sufficiency and promotes fatty acid synthesis in the fed state, not fasting gluconeogenesis.
Rate-limiting enzymes and control points US Medical PG Question 5: You have been asked to deliver a lecture to medical students about the effects of various body hormones and neurotransmitters on the metabolism of glucose. Which of the following statements best describes the effects of sympathetic stimulation on glucose metabolism?
- A. Norepinephrine causes increased glucose absorption within the intestines.
- B. Without epinephrine, insulin cannot act on the liver.
- C. Peripheral tissues require epinephrine to take up glucose.
- D. Epinephrine increases liver glycogenolysis. (Correct Answer)
- E. Sympathetic stimulation to alpha receptors of the pancreas increases insulin release.
Rate-limiting enzymes and control points Explanation: ***Epinephrine increases liver glycogenolysis.***
- **Epinephrine**, released during sympathetic stimulation, primarily acts to increase **glucose availability** for immediate energy.
- It achieves this by stimulating **glycogenolysis** (breakdown of glycogen into glucose) in the liver via **beta-adrenergic receptors**.
*Norepinephrine causes increased glucose absorption within the intestines.*
- **Norepinephrine** primarily causes **vasoconstriction** and can *decrease* **intestinal motility** and nutrient absorption due to shunting blood away from the digestive tract during stress.
- Glucose absorption is mainly regulated by digestive enzymes and transport proteins, not directly increased by norepinephrine.
*Without epinephrine, insulin cannot act on the liver.*
- **Insulin** acts on the liver independent of epinephrine to promote **glucose uptake**, **glycogenesis**, and **lipid synthesis**.
- Epinephrine and insulin have **antagonistic effects** on liver glucose metabolism; epinephrine increases glucose output, while insulin decreases it.
*Peripheral tissues require epinephrine to take up glucose.*
- **Insulin** is the primary hormone required for **glucose uptake** by most peripheral tissues, especially **muscle** and **adipose tissue**, via **GLUT4 transporters**.
- Epinephrine generally *reduces* glucose uptake by peripheral tissues to preserve glucose for the brain during stress.
*Sympathetic stimulation to alpha receptors of the pancreas increases insulin release.*
- Sympathetic stimulation, primarily acting through **alpha-2 adrenergic receptors** on pancreatic beta cells, actually **inhibits** **insulin secretion**.
- This inhibition helps to increase blood glucose levels by reducing insulin's glucose-lowering effects.
Rate-limiting enzymes and control points US Medical PG Question 6: What is the primary mechanism for glucose uptake in neurons?
- A. GLUT1
- B. GLUT2
- C. GLUT3 (Correct Answer)
- D. GLUT4
Rate-limiting enzymes and control points Explanation: ***GLUT3***
- **GLUT3** is the primary glucose transporter in **neurons** and has a **high affinity** for glucose.
- This high affinity ensures that neurons can continuously take up glucose, even when blood glucose levels are relatively low, to meet their significant energy demands.
*GLUT1*
- **GLUT1** is abundant in **red blood cells** and at the **blood-brain barrier**, where it provides basal glucose transport to many cell types.
- While present in the brain, it is primarily responsible for glucose transport across the **blood-brain barrier** into the interstitial fluid, not directly into neurons as the main mechanism.
*GLUT2*
- **GLUT2** has a **low affinity** and **high capacity** for glucose, primarily found in the **liver, pancreatic beta cells, kidney, and intestine**.
- Its role is to sense high glucose levels and transport large amounts of glucose accordingly, which is not characteristic of neuronal glucose uptake.
*GLUT4*
- **GLUT4** is the **insulin-sensitive** glucose transporter, predominantly found in **adipose tissue** and **skeletal muscle**.
- Its translocation to the cell membrane is stimulated by insulin, a mechanism not central to neuronal glucose uptake.
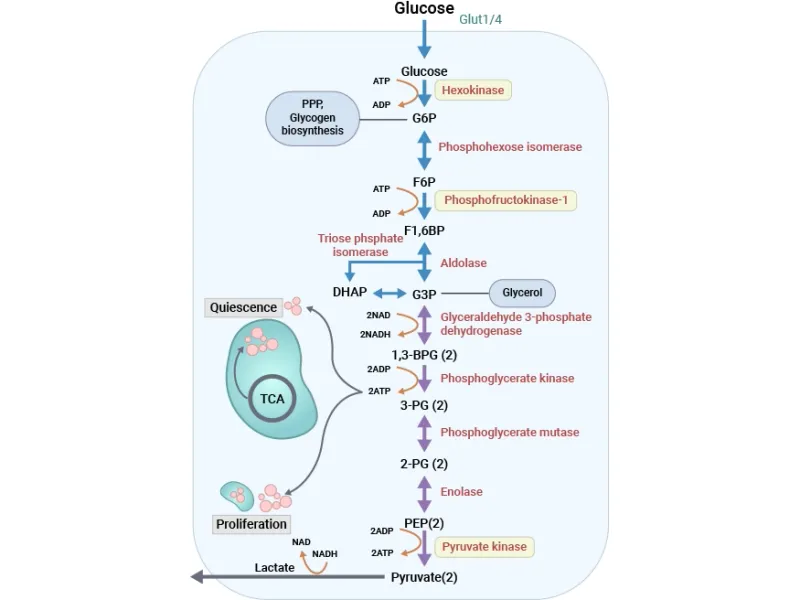
Rate-limiting enzymes and control points US Medical PG Question 7: To maintain blood glucose levels even after glycogen stores have been depleted, the body, mainly the liver, is able to synthesize glucose in a process called gluconeogenesis. Which of the following reactions of gluconeogenesis requires an enzyme different from glycolysis?
- A. Fructose 1,6-bisphosphate --> Fructose-6-phosphate (Correct Answer)
- B. Glyceraldehyde 3-phosphate --> 1,3-bisphosphoglycerate
- C. 2-phosphoglycerate --> 3-phosphoglycerate
- D. Dihydroxyacetone phosphate --> Glyceraldehyde 3-phosphate
- E. Phosphoenolpyruvate --> 2-phosphoglycerate
Rate-limiting enzymes and control points Explanation: ***Fructose 1,6-bisphosphate --> Fructose-6-phosphate***
- This reaction in gluconeogenesis is catalyzed by **fructose 1,6-bisphosphatase**, which is distinct from **phosphofructokinase-1** that catalyzes the reverse reaction in glycolysis.
- This step is one of the three **irreversible steps** in glycolysis that must be bypassed by different enzymes in gluconeogenesis to ensure the unidirectional flow of the pathway.
*Glyceraldehyde 3-phosphate --> 1,3-bisphosphoglycerate*
- This reaction is catalyzed by **Glyceraldehyde 3-phosphate dehydrogenase** in both glycolysis and gluconeogenesis, as it is a **reversible step**.
- In gluconeogenesis, the equilibrium is shifted towards the formation of glyceraldehyde 3-phosphate due to the low concentration of products.
*2-phosphoglycerate --> 3-phosphoglycerate*
- This is a reversible isomerization reaction catalyzed by **phosphoglycerate mutase** in both glycolysis and gluconeogenesis.
- No unique enzyme is required for gluconeogenesis at this step.
*Dihydroxyacetone phosphate --> Glyceraldehyde 3-phosphate*
- This reversible interconversion between these two triose phosphates is catalyzed by **triose phosphate isomerase** in both pathways.
- These molecules are in equilibrium and can be readily converted from one to the other.
*Phosphoenolpyruvate --> 2-phosphoglycerate*
- This is a reversible reaction catalyzed by **enolase** in both glycolysis and gluconeogenesis.
- No distinct enzyme is needed for this step in gluconeogenesis.
Rate-limiting enzymes and control points US Medical PG Question 8: Maturity Onset Diabetes of the Young (MODY) type 2 is a consequence of a defective pancreatic enzyme, which normally acts as a glucose sensor, resulting in a mild hyperglycemia. The hyperglycemia is especially exacerbated during pregnancy. Which of the following pathways is controlled by this enzyme?
- A. Fructose-6-phosphate --> fructose-1,6-bisphosphate
- B. Phosphoenolpyruvate --> pyruvate
- C. Glucose --> glucose-6-phosphate (Correct Answer)
- D. Glucose-6-phosphate --> fructose-6-phosphate
- E. Glyceraldehyde-3-phosphate --> 1,3-bisphosphoglycerate
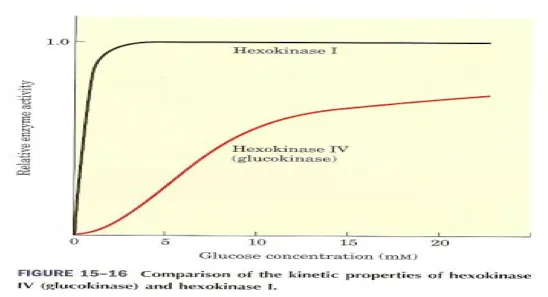
Rate-limiting enzymes and control points Explanation: ***Glucose --> glucose-6-phosphate***
- This reaction is catalyzed by **glucokinase** in the pancreatic beta cells, which serves as a **glucose sensor** by controlling the rate-limiting step of glycolysis.
- MODY type 2 is caused by mutations in the **glucokinase gene (GCK)**, leading to a higher threshold for insulin secretion and mild hyperglycemia, particularly exacerbated during pregnancy.
*Fructose-6-phosphate --> fructose-1,6-bisphosphate*
- This step is catalyzed by **phosphofructokinase-1 (PFK-1)**, a key regulatory enzyme in glycolysis, but it is not the primary glucose sensor in pancreatic beta cells.
- While important for glycolysis, defects in PFK-1 are associated with glycolytic enzyme deficiencies (e.g., Tarui's disease), not MODY type 2.
*Phosphoenolpyruvate --> pyruvate*
- This final step of glycolysis is catalyzed by **pyruvate kinase**, an enzyme that is regulated but does not act as the primary glucose sensor.
- Pyruvate kinase deficiency leads to hemolytic anemia and is not associated with MODY type 2.
*Glucose-6-phosphate --> fructose-6-phosphate*
- This reversible isomerization step is catalyzed by **phosphoglucose isomerase**, and while part of glycolysis, it is not the rate-limiting step or the primary glucose sensing mechanism in pancreatic beta cells.
- Defects in this enzyme are rare and not linked to MODY type 2.
*Glyceraldehyde-3-phosphate --> 1,3-bisphosphoglycerate*
- This step is catalyzed by **glyceraldehyde-3-phosphate dehydrogenase (GAPDH)**, an important enzyme in glycolysis.
- GAPDH is involved in energy production but is not considered the glucose sensor for insulin release, and its defects are not associated with MODY type 2.
Rate-limiting enzymes and control points US Medical PG Question 9: A newborn undergoing the standard screening tests is found to have a positive test for reducing sugars. Further testing is performed and reveals that the patient does not have galactosemia, but rather is given a diagnosis of fructosuria. What levels of enzymatic activity are altered in this patient?
- A. Hexokinase decreased; fructokinase decreased
- B. Hexokinase unchanged; fructokinase unchanged
- C. Hexokinase increased; fructokinase increased
- D. Hexokinase increased; fructokinase decreased
- E. Hexokinase unchanged; fructokinase decreased (Correct Answer)
Rate-limiting enzymes and control points Explanation: ***Hexokinase unchanged; fructokinase decreased***
- **Essential fructosuria** is caused by a deficiency in **fructokinase**, the enzyme responsible for the first step of fructose metabolism (fructose → fructose-1-phosphate).
- This results in **decreased or absent fructokinase activity**, leading to fructose accumulation in blood and urine (positive reducing sugar test).
- **Hexokinase activity remains unchanged** - there is no upregulation or compensatory increase in hexokinase. The enzyme maintains its normal baseline activity.
- Essential fructosuria is a **benign, asymptomatic condition** with no metabolic stress, so no compensatory enzyme changes occur.
- The small amount of fructose that needs metabolism can be handled by normal baseline hexokinase activity (hexokinase has broad substrate specificity).
*Hexokinase decreased; fructokinase decreased*
- While **fructokinase is decreased** in essential fructosuria, hexokinase activity is not decreased.
- Hexokinase is a constitutively expressed glycolytic enzyme whose activity does not change in this benign condition.
*Hexokinase unchanged; fructokinase unchanged*
- This is incorrect because **fructokinase activity is specifically decreased** in essential fructosuria, which is the defining enzymatic defect of the condition.
- The decreased fructokinase activity causes fructose to accumulate and appear in the urine.
*Hexokinase increased; fructokinase increased*
- **Fructokinase is decreased, not increased** - an increase would prevent the fructose accumulation characteristic of this condition.
- Hexokinase activity does not increase as essential fructosuria causes no metabolic stress requiring compensation.
*Hexokinase increased; fructokinase decreased*
- While **fructokinase is decreased** in essential fructosuria, hexokinase activity does not increase.
- This is a benign condition with no compensatory enzyme upregulation - hexokinase maintains normal baseline activity levels.
Rate-limiting enzymes and control points US Medical PG Question 10: An investigator is conducting an experiment to study different pathways of glucose metabolism. He obtains cells cultured from various tissues to study the effect of increased extracellular glucose concentration. Following the incubation of these cells in 5% dextrose, he measures the intracellular fructose concentration. The concentration of fructose is expected to be highest in cells obtained from which of the following tissues?
- A. Ovary
- B. Retina
- C. Myelin sheath
- D. Kidney
- E. Lens (Correct Answer)
Rate-limiting enzymes and control points Explanation: ***Lens***
- The **lens** is rich in the enzyme **aldose reductase**, which converts glucose to sorbitol, and then **sorbitol dehydrogenase** converts sorbitol to fructose via the **polyol pathway**.
- In a high-glucose environment, this pathway becomes highly active in the lens, leading to an increased production and accumulation of **fructose**, which can contribute to osmotic stress and cataract formation.
*Ovary*
- While other reproductive tissues can metabolize glucose, the **ovary** is not a primary site for significant fructose accumulation through the **polyol pathway** in response to elevated glucose.
- Its metabolic activity is more geared towards steroidogenesis and oocyte development rather than high fructose production from glucose.
*Retina*
- The **retina** contains some aldose reductase activity, and increased glucose can activate the **polyol pathway**, leading to sorbitol and fructose accumulation.
- However, the lens typically shows a more pronounced increase in fructose concentration due to its higher metabolic flux through this pathway and its susceptibility to osmotic damage.
*Myelin sheath*
- The **myelin sheath**, primarily composed of lipids, is part of the nervous system and is not known for significant **fructose production** via the **polyol pathway** in response to high glucose.
- Damage to myelin in diabetic conditions is often linked to other mechanisms like glycation and oxidative stress rather than direct fructose accumulation.
*Kidney*
- The **kidney** can utilize the **polyol pathway**, and conditions like **diabetic nephropathy** involve increased sorbitol and fructose production.
- However, the magnitude of fructose accumulation and its direct pathogenic role differ from that in the lens, where osmotic effects of polyols are particularly critical.
More Rate-limiting enzymes and control points US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.
 These three irreversible enzymes are the key control points. 📌 Mnemonic: Hungry People Prefer Pie.
These three irreversible enzymes are the key control points. 📌 Mnemonic: Hungry People Prefer Pie.