Overview and regulation of glycolysis US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Overview and regulation of glycolysis. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Overview and regulation of glycolysis US Medical PG Question 1: A 45-year-old man is brought to the emergency department by ambulance after vomiting blood. The patient reports that he only ate a small snack the morning before and had not eaten anything for over 24 hours. At the hospital, the patient is stabilized. He is admitted to a surgical floor and placed on NPO with a nasogastric tube set to intermittent suction. He has been previously diagnosed with liver cirrhosis. An esophagogastroduodenoscopy (EGD) has been planned for the next afternoon. At the time of endoscopy, some pathways were generating glucose to maintain serum glucose levels. Which of the following enzymes catalyzes the irreversible biochemical reaction of this process?
- A. Glucose-6-phosphate dehydrogenase
- B. Glycogen phosphorylase
- C. Enolase
- D. Glyceraldehyde-3-phosphate dehydrogenase
- E. Fructose-1,6-bisphosphatase (Correct Answer)
Overview and regulation of glycolysis Explanation: ***Fructose-1,6-bisphosphatase***
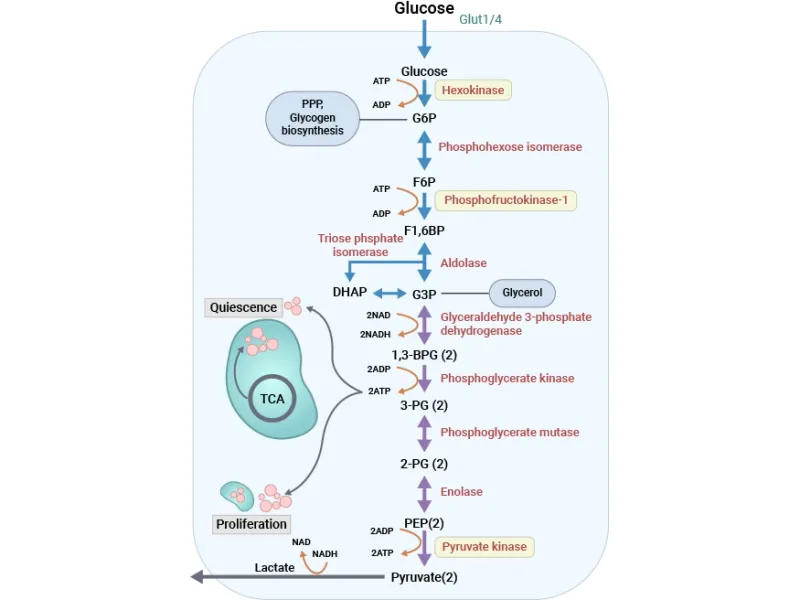
- The scenario describes a patient in a fasting state for over 24 hours, during which **gluconeogenesis** is crucial for maintaining blood glucose levels.
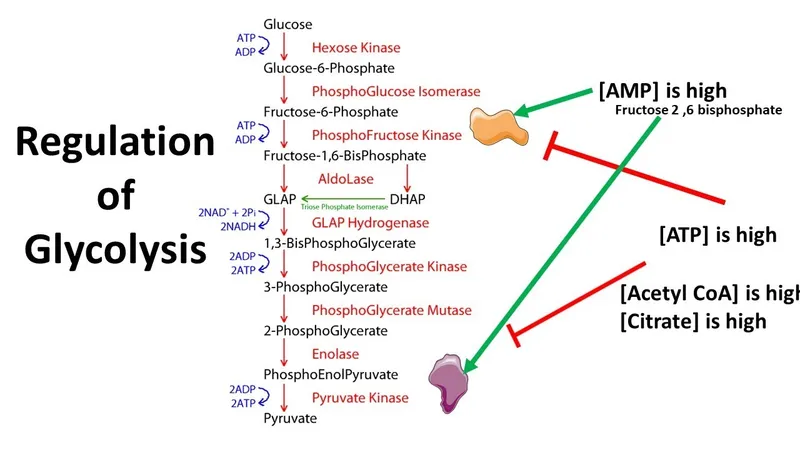
- **Fructose-1,6-bisphosphatase** is one of the key regulatory enzymes in gluconeogenesis, catalyzing an **irreversible reaction** that bypasses the phosphofructokinase-1 step of glycolysis.
*Glucose-6-phosphate dehydrogenase*
- This enzyme is involved in the **pentose phosphate pathway**, which generates NADPH and precursors for nucleotide synthesis.
- It does not directly participate in gluconeogenesis to produce glucose from non-carbohydrate sources.
*Glycogen phosphorylase*
- This enzyme is involved in **glycogenolysis**, the breakdown of glycogen into glucose-1-phosphate.
- While it releases glucose, the body's glycogen stores would likely be depleted after over 24 hours of fasting, making gluconeogenesis the primary pathway for glucose production.
*Enolase*
- Enolase is an enzyme in the glycolytic pathway, catalyzing the reversible conversion of 2-phosphoglycerate to phosphoenolpyruvate.
- It is not an enzyme of gluconeogenesis, nor does it catalyze an irreversible step in the glucose production process during fasting.
*Glyceraldehyde-3-phosphate dehydrogenase*
- This enzyme is also part of glycolysis, catalyzing the reversible oxidation and phosphorylation of glyceraldehyde-3-phosphate to 1,3-bisphosphoglycerate.
- Like enolase, it is not an irreversible enzyme in gluconeogenesis that would be generating glucose under fasting conditions.
Overview and regulation of glycolysis US Medical PG Question 2: A 16-year-old boy presents with acute left-sided weakness. The patient is obtunded and can not provide any history other than his stomach hurts. The patient’s friend states that the patient has had episodes like this in the past and that “he has the same weird disease as his mom”. On physical examination, strength is 1 out of 5 in the left upper and lower extremities. A noncontrast CT scan of the head is normal. Laboratory tests reveal an anion gap metabolic acidosis. Which of the following is a normal function of the structure causing this patient’s condition?
- A. Regulation of blood glucose
- B. Synthesis of fatty acids
- C. Production of bile acids
- D. Metabolism of purines
- E. Conversion of ammonia to urea (Correct Answer)
Overview and regulation of glycolysis Explanation: ***Conversion of ammonia to urea***
- The patient's presentation with **acute neurological deficits**, **abdominal pain**, and **anion gap metabolic acidosis** with a normal head CT, along with family history, is highly suggestive of a **urea cycle disorder (UCD)**.
- The **urea cycle** primarily functions in the **liver** to convert **toxic ammonia** into less toxic urea for excretion.
*Regulation of blood glucose*
- While regulation of blood glucose is a vital **liver function**, it does not directly relate to the primary metabolic derangement (ammonia accumulation) seen in UCDs.
- **Hypoglycemia** can occur in some UCDs, but it's not the defining feature of the neurological crisis.
*Synthesis of fatty acids*
- **Fatty acid synthesis** primarily occurs in the liver and adipose tissue, but its dysfunction is not the direct cause of the patient's acute symptoms.
- While liver dysfunction can impact lipid metabolism, it is not the central pathological process in UCDs.
*Production of bile acids*
- **Bile acid production** is a critical function of the liver for fat digestion and absorption, but it is not directly impaired in urea cycle disorders.
- Bile acid synthesis disorders would present with different clinical features, such as **cholestasis** and fat malabsorption.
*Metabolism of purines*
- **Purine metabolism** occurs in various tissues, and its dysfunction can lead to conditions like **gout** or **Lesch-Nyhan syndrome**, which differ from the presented symptoms.
- Abnormalities in purine metabolism are not the core defect in urea cycle disorders.
Overview and regulation of glycolysis US Medical PG Question 3: A 25-year-old man is brought to the emergency department 6 hours after rescuing babies and puppies from a burning daycare center. He says that he has a severe headache, feels nauseous and dizzy. He is tachypneic. An arterial blood gas shows pH 7.3, PaCO2 49 mmHg, PaO2 80 mmHg. Serum lactate level is 6 mmol/L. What biochemical process explains these laboratory values?
- A. Increased oxidation of NADH
- B. Low lactate dehydrogenase activity
- C. Low pyruvate dehydrogenase activity (Correct Answer)
- D. High pyruvate dehydrogenase activity
- E. Increased decarboxylation of pyruvate
Overview and regulation of glycolysis Explanation: ***Low pyruvate dehydrogenase activity***
- The patient's symptoms (headache, nausea, dizziness, tachypnea) after smoke exposure, combined with a **high serum lactate (6 mmol/L)** and signs of acidosis (pH 7.3, PaCO2 49 mmHg indicating respiratory compensation for metabolic acidosis), are highly suggestive of **carbon monoxide (CO) poisoning**.
- **CO binds to cytochrome C oxidase**, inhibiting the electron transport chain and **oxidative phosphorylation**. This leads to a buildup of NADH and a shift to **anaerobic metabolism**, where pyruvate is converted to **lactate** instead of entering the **Krebs cycle** via **pyruvate dehydrogenase (PDH)**. Therefore, the effective activity of PDH is reduced because its substrate (pyruvate) is shunted to lactate production.
*Increased oxidation of NADH*
- In CO poisoning, **oxidative phosphorylation is inhibited**, leading to a *decrease* in NADH oxidation as the electron transport chain cannot efficiently accept electrons from NADH.
- Instead, NADH *accumulates*, favoring the conversion of pyruvate to lactate to regenerate NAD+ for glycolysis.
*Low lactate dehydrogenase activity*
- **Lactate dehydrogenase (LDH)** activity would likely be *increased* or normal in this scenario, as it is responsible for converting pyruvate to lactate during anaerobic metabolism, which is elevated as indicated by the high serum lactate.
- Low LDH activity would *reduce* lactate production, counteracting the observed elevated lactate levels.
*High pyruvate dehydrogenase activity*
- **Pyruvate dehydrogenase (PDH)** converts pyruvate to acetyl-CoA for entry into the Krebs cycle, a key step in *aerobic* metabolism.
- In the setting of **CO poisoning**, aerobic metabolism is compromised, leading to a *reduction* in the flow through PDH as pyruvate is shunted towards **lactate production**.
*Increased decarboxylation of pyruvate*
- **Decarboxylation of pyruvate** is catalyzed by **pyruvate dehydrogenase (PDH)**, converting pyruvate to acetyl-CoA and releasing CO2.
- With compromised oxidative phosphorylation due to CO poisoning, the cell shifts to anaerobic metabolism, which *reduces* the processing of pyruvate through PDH, thus *decreasing* its decarboxylation, leading to lactate build-up.
Overview and regulation of glycolysis US Medical PG Question 4: A 52-year-old man with a history of Type 1 diabetes mellitus presents to the emergency room with increasing fatigue. Two days ago, he ran out of insulin and has not had time to obtain a new prescription. He denies fevers or chills. His temperature is 37.2 degrees Celsius, blood pressure 84/56 mmHg, heart rate 100/min, respiratory rate 20/min, and SpO2 97% on room air. His physical exam is otherwise within normal limits. An arterial blood gas analysis shows the following:
pH 7.25, PCO2 29, PO2 95, HCO3- 15.
Which of the following acid-base disorders is present?
- A. Respiratory alkalosis with appropriate metabolic compensation
- B. Respiratory acidosis with appropriate metabolic compensation
- C. Mixed metabolic and respiratory acidosis
- D. Metabolic acidosis with appropriate respiratory compensation (Correct Answer)
- E. Metabolic alkalosis with appropriate respiratory compensation
Overview and regulation of glycolysis Explanation: ***Metabolic acidosis with appropriate respiratory compensation***
- The patient's pH of 7.25 and HCO3- of 15 indicate **metabolic acidosis**, while the PCO2 of 29 indicates **respiratory compensation**.
- The compensation is **appropriate** as suggested by Winter's formula [Expected PCO2 = (1.5 x HCO3-) + 8 +/- 2; (1.5 x 15) + 8 = 30.5, which is close to 29].
*Respiratory alkalosis with appropriate metabolic compensation*
- This would involve a **pH > 7.45** and **low PCO2** with a secondary drop in HCO3-, which is not seen here.
- The patient's primary problem is a metabolic disturbance due to insulin deficiency.
*Respiratory acidosis with appropriate metabolic compensation*
- This disorder is characterized by a **low pH** and a **high PCO2**, with a secondary rise in HCO3-.
- The patient's PCO2 is low, indicating a compensatory response rather than a primary respiratory acidosis.
*Mixed metabolic and respiratory acidosis*
- A mixed disorder would show a **low pH** due to both **low HCO3-** and **high PCO2**.
- The patient's PCO2 is low, indicating a compensatory response to metabolic acidosis, not an additional respiratory acidosis.
*Metabolic alkalosis with appropriate respiratory compensation*
- This would present with a **high pH (>7.45)** and **high HCO3-**, with compensatory **elevated PCO2**.
- The patient's pH and HCO3- are low, indicating acidosis, not alkalosis.
Overview and regulation of glycolysis US Medical PG Question 5: A 22-year-old medical student decides to fast for 24 hours after reading about the possible health benefits of fasting. She read that blood glucose levels are maintained by metabolic processes such as hepatic glycogenolysis and hepatic gluconeogenesis during the initial 3 days of fasting. During the day, she did not suffer from the symptoms of hypoglycemia. Which of the following signaling molecules most likely stimulated the reaction which maintained her blood glucose after all her stored glucose was broken down and used up?
- A. Adenosine diphosphate
- B. Acetyl CoA (Correct Answer)
- C. Acetate
- D. Citrate
- E. Adenosine monophosphate
Overview and regulation of glycolysis Explanation: ***Acetyl CoA***
- **Acetyl CoA** is the key **allosteric activator of pyruvate carboxylase**, the first committed enzyme of gluconeogenesis that converts pyruvate to oxaloacetate.
- During prolonged fasting after glycogen stores are depleted, the body shifts to **fatty acid oxidation** (β-oxidation), which produces large amounts of **Acetyl CoA**.
- High **Acetyl CoA** levels signal that fat is being oxidized for energy, and simultaneously **activate gluconeogenesis** to maintain blood glucose for glucose-dependent tissues (brain, RBCs).
- This is the primary signaling mechanism that directly stimulates the gluconeogenic pathway after glycogen is exhausted.
*Adenosine monophosphate (AMP)*
- **AMP** levels rise during energy depletion and activate **AMP-activated protein kinase (AMPK)**.
- However, AMPK **inhibits gluconeogenesis** (not stimulates it) because gluconeogenesis is an **ATP-consuming** anabolic process (requires 6 ATP per glucose).
- AMPK promotes ATP-generating catabolic processes like fatty acid oxidation, but suppresses ATP-consuming processes like gluconeogenesis and fatty acid synthesis.
*Adenosine diphosphate (ADP)*
- **ADP** accumulates when ATP is hydrolyzed and signals moderate energy deficit.
- ADP is primarily a substrate for ATP regeneration via oxidative phosphorylation and does not directly regulate gluconeogenesis.
- Its role in metabolic regulation is less specific than allosteric activators like Acetyl CoA.
*Acetate*
- **Acetate** can be converted to Acetyl CoA but is not a direct signaling molecule for gluconeogenesis.
- It is a minor metabolite that may be produced in specific conditions (e.g., alcohol metabolism, ketoacidosis) but does not play a primary role in fasting-induced glucose homeostasis.
*Citrate*
- **Citrate** is a Krebs cycle intermediate that inhibits **phosphofructokinase-1 (PFK-1)** in glycolysis, thus reducing glucose breakdown.
- While citrate inhibition of glycolysis indirectly favors gluconeogenesis by preventing futile cycling, citrate does not **directly activate** gluconeogenic enzymes.
- Citrate primarily signals energy sufficiency and promotes fatty acid synthesis in the fed state, not fasting gluconeogenesis.
Overview and regulation of glycolysis US Medical PG Question 6: A 24-year-old man is running a marathon. Upon reaching the finish line, his serum lactate levels were measured and were significantly increased as compared to his baseline. Which of the following pathways converts the lactate produced by muscles into glucose and transports it back to the muscles?
- A. Citric acid cycle
- B. Glycolysis
- C. Glycogenesis
- D. Pentose phosphate pathway
- E. Cori cycle (Correct Answer)
Overview and regulation of glycolysis Explanation: ***Cori cycle***
- The **Cori cycle** is the metabolic pathway that converts **lactate** produced by anaerobic glycolysis in muscles (especially during intense exercise) back to **glucose in the liver** via gluconeogenesis.
- During strenuous exercise, muscles rely on anaerobic glycolysis when oxygen supply is insufficient, producing lactate and 2 ATP per glucose.
- The lactate is transported via bloodstream to the liver, where it is converted back to glucose (requiring 6 ATP), which then returns to muscles for energy or glycogen storage.
- This cycle allows muscles to continue generating ATP anaerobically while the liver handles lactate clearance.
*Citric acid cycle*
- The **citric acid cycle** (Krebs cycle) oxidizes **acetyl-CoA** to generate ATP, NADH, and FADH₂ in the mitochondrial matrix under aerobic conditions.
- It does not convert lactate to glucose; rather, pyruvate can be converted to acetyl-CoA to enter this cycle for complete oxidation.
- This is an aerobic process and does not involve the liver-muscle lactate-glucose exchange.
*Glycolysis*
- **Glycolysis** is the metabolic pathway that breaks down **glucose into pyruvate**, generating 2 ATP and 2 NADH per glucose molecule.
- Under anaerobic conditions, pyruvate is converted to lactate to regenerate NAD⁺ for continued glycolysis.
- This is the opposite of what the question asks—glycolysis produces lactate from glucose, not glucose from lactate.
*Glycogenesis*
- **Glycogenesis** is the process of synthesizing **glycogen from glucose** for storage, primarily in liver and muscle tissue.
- While it involves glucose storage, it does not convert lactate back to glucose or involve the metabolic exchange between muscles and liver described in the question.
*Pentose phosphate pathway*
- The **pentose phosphate pathway** (hexose monophosphate shunt) produces **NADPH** for reductive biosynthesis and **ribose-5-phosphate** for nucleotide synthesis.
- It branches from glycolysis but is not involved in lactate metabolism or the muscle-liver glucose-lactate exchange.
Overview and regulation of glycolysis US Medical PG Question 7: A 16-year-old teenager is brought to the emergency department after having slipped on ice while walking to school. She hit her head on the side of the pavement and retained consciousness. She was brought to the closest ER within an hour of the incident. The ER physician sends her immediately to get a CT scan and also orders routine blood work. The physician understands that in cases of stress, such as in this patient, the concentration of certain hormones will be increased, while others will be decreased. Considering allosteric regulation by hormones, which of the following enzymes will most likely be inhibited in this patient?
- A. Glucose-6-phosphatase
- B. Fructose 1,6-bisphosphatase
- C. Pyruvate carboxylase
- D. Phosphofructokinase (Correct Answer)
- E. Glycogen phosphorylase
Overview and regulation of glycolysis Explanation: ***Phosphofructokinase***
- In a stress state, **cortisol** and **epinephrine** levels are elevated, leading to increased **gluconeogenesis** and **glycogenolysis** to provide rapid energy.
- **Allosteric inhibition** of PFK-1 occurs through multiple mechanisms:
- **ATP** and **citrate** (high energy signals) act as direct **allosteric inhibitors** of PFK-1
- **Glucagon** (elevated during stress) indirectly inhibits PFK-1 by reducing levels of **fructose-2,6-bisphosphate**, a potent allosteric activator
- This inhibition of glycolysis spares glucose for critical organs like the brain and heart.
*Glucose-6-phosphatase*
- This enzyme catalyzes the final step of **gluconeogenesis** and **glycogenolysis**, converting G6P to free glucose.
- During stress, its activity is **stimulated** to increase blood glucose levels, not inhibited.
*Fructose 1,6-bisphosphatase*
- This enzyme plays a key role in **gluconeogenesis**, a process vital for maintaining glucose homeostasis during stress.
- Its activity would be **upregulated** to produce glucose, rather than inhibited.
*Pyruvate carboxylase*
- This enzyme initiates **gluconeogenesis** by converting pyruvate to oxaloacetate in the mitochondria.
- During stress, its activity is **stimulated** by elevated acetyl-CoA (an allosteric activator), not inhibited.
*Glycogen phosphorylase*
- This enzyme is responsible for **glycogenolysis**, the breakdown of glycogen into glucose-1-phosphate.
- Its activity is **stimulated** by stress hormones (epinephrine and glucagon) through cAMP-mediated phosphorylation, ensuring rapid glucose availability.
Overview and regulation of glycolysis US Medical PG Question 8: A 12-year-old boy and his siblings are referred to a geneticist for evaluation of a mild but chronic hemolytic anemia that has presented with fatigue, splenomegaly, and scleral icterus. Coombs test is negative and blood smear does not show any abnormal findings. An enzymatic panel is assayed, and pyruvate kinase is found to be mutated on both alleles. The geneticist explains that pyruvate kinase functions in glycolysis and is involved in a classic example of feed-forward regulation. Which of the following metabolites is able to activate pyruvate kinase?
- A. Fructose-1,6-bisphosphate (Correct Answer)
- B. Alanine
- C. ATP
- D. Glucose-6-phosphate
- E. Glyceraldehyde-3-phosphate
Overview and regulation of glycolysis Explanation: ***Fructose-1,6-bisphosphate***
- **Fructose-1,6-bisphosphate** is a potent **allosteric activator** of pyruvate kinase. This is an example of **feed-forward activation**, where a product of an early irreversible step in glycolysis (catalyzed by phosphofructokinase-1) activates a later enzyme (pyruvate kinase) in the pathway.
- This activation ensures that substrates for the later steps of glycolysis are rapidly utilized when earlier steps are highly active, matching the rate of metabolite flow and increasing the overall efficiency of glycolysis for energy production.
*Alanine*
- **Alanine** is an **inhibitor** of pyruvate kinase, not an activator. It serves as an indicator of a high cellular energy state and ample amino acid supply.
- High levels of alanine signal the cell that there is sufficient energy and building blocks, thus **shutting down** glycolysis at the pyruvate kinase step to conserve glucose for other needs like glycogen synthesis.
*ATP*
- **ATP** (adenosine triphosphate) is an **allosteric inhibitor** of pyruvate kinase. High ATP levels signal a high energy state in the cell.
- When the cell has sufficient energy, ATP binds to a regulatory site on pyruvate kinase, reducing its activity and **slowing down glycolysis** to prevent overproduction of ATP.
*Glucose-6-phosphate*
- **Glucose-6-phosphate** is an intermediate in glycolysis but does not directly activate pyruvate kinase. It can act as an allosteric inhibitor of hexokinase, the first enzyme in glycolysis, but not pyruvate kinase.
- Its accumulation typically signifies a **backup** in the glycolytic pathway (e.g., due to downstream inhibition), leading to a *reduction* in overall glucose flux rather than a direct activation of pyruvate kinase.
*Glyceraldehyde-3-phosphate*
- **Glyceraldehyde-3-phosphate** is an intermediate in glycolysis, but it does not directly activate pyruvate kinase. It is a substrate for glyceraldehyde-3-phosphate dehydrogenase.
- While its presence indicates active glycolysis, it does not exert a specific allosteric regulatory effect on pyruvate kinase in the way fructose-1,6-bisphosphate does.
Overview and regulation of glycolysis US Medical PG Question 9: To maintain blood glucose levels even after glycogen stores have been depleted, the body, mainly the liver, is able to synthesize glucose in a process called gluconeogenesis. Which of the following reactions of gluconeogenesis requires an enzyme different from glycolysis?
- A. Fructose 1,6-bisphosphate --> Fructose-6-phosphate (Correct Answer)
- B. Glyceraldehyde 3-phosphate --> 1,3-bisphosphoglycerate
- C. 2-phosphoglycerate --> 3-phosphoglycerate
- D. Dihydroxyacetone phosphate --> Glyceraldehyde 3-phosphate
- E. Phosphoenolpyruvate --> 2-phosphoglycerate
Overview and regulation of glycolysis Explanation: ***Fructose 1,6-bisphosphate --> Fructose-6-phosphate***
- This reaction in gluconeogenesis is catalyzed by **fructose 1,6-bisphosphatase**, which is distinct from **phosphofructokinase-1** that catalyzes the reverse reaction in glycolysis.
- This step is one of the three **irreversible steps** in glycolysis that must be bypassed by different enzymes in gluconeogenesis to ensure the unidirectional flow of the pathway.
*Glyceraldehyde 3-phosphate --> 1,3-bisphosphoglycerate*
- This reaction is catalyzed by **Glyceraldehyde 3-phosphate dehydrogenase** in both glycolysis and gluconeogenesis, as it is a **reversible step**.
- In gluconeogenesis, the equilibrium is shifted towards the formation of glyceraldehyde 3-phosphate due to the low concentration of products.
*2-phosphoglycerate --> 3-phosphoglycerate*
- This is a reversible isomerization reaction catalyzed by **phosphoglycerate mutase** in both glycolysis and gluconeogenesis.
- No unique enzyme is required for gluconeogenesis at this step.
*Dihydroxyacetone phosphate --> Glyceraldehyde 3-phosphate*
- This reversible interconversion between these two triose phosphates is catalyzed by **triose phosphate isomerase** in both pathways.
- These molecules are in equilibrium and can be readily converted from one to the other.
*Phosphoenolpyruvate --> 2-phosphoglycerate*
- This is a reversible reaction catalyzed by **enolase** in both glycolysis and gluconeogenesis.
- No distinct enzyme is needed for this step in gluconeogenesis.
Overview and regulation of glycolysis US Medical PG Question 10: A newborn undergoing the standard screening tests is found to have a positive test for reducing sugars. Further testing is performed and reveals that the patient does not have galactosemia, but rather is given a diagnosis of fructosuria. What levels of enzymatic activity are altered in this patient?
- A. Hexokinase decreased; fructokinase decreased
- B. Hexokinase unchanged; fructokinase unchanged
- C. Hexokinase increased; fructokinase increased
- D. Hexokinase increased; fructokinase decreased
- E. Hexokinase unchanged; fructokinase decreased (Correct Answer)
Overview and regulation of glycolysis Explanation: ***Hexokinase unchanged; fructokinase decreased***
- **Essential fructosuria** is caused by a deficiency in **fructokinase**, the enzyme responsible for the first step of fructose metabolism (fructose → fructose-1-phosphate).
- This results in **decreased or absent fructokinase activity**, leading to fructose accumulation in blood and urine (positive reducing sugar test).
- **Hexokinase activity remains unchanged** - there is no upregulation or compensatory increase in hexokinase. The enzyme maintains its normal baseline activity.
- Essential fructosuria is a **benign, asymptomatic condition** with no metabolic stress, so no compensatory enzyme changes occur.
- The small amount of fructose that needs metabolism can be handled by normal baseline hexokinase activity (hexokinase has broad substrate specificity).
*Hexokinase decreased; fructokinase decreased*
- While **fructokinase is decreased** in essential fructosuria, hexokinase activity is not decreased.
- Hexokinase is a constitutively expressed glycolytic enzyme whose activity does not change in this benign condition.
*Hexokinase unchanged; fructokinase unchanged*
- This is incorrect because **fructokinase activity is specifically decreased** in essential fructosuria, which is the defining enzymatic defect of the condition.
- The decreased fructokinase activity causes fructose to accumulate and appear in the urine.
*Hexokinase increased; fructokinase increased*
- **Fructokinase is decreased, not increased** - an increase would prevent the fructose accumulation characteristic of this condition.
- Hexokinase activity does not increase as essential fructosuria causes no metabolic stress requiring compensation.
*Hexokinase increased; fructokinase decreased*
- While **fructokinase is decreased** in essential fructosuria, hexokinase activity does not increase.
- This is a benign condition with no compensatory enzyme upregulation - hexokinase maintains normal baseline activity levels.
More Overview and regulation of glycolysis US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.