Disorders of glycolytic enzymes US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Disorders of glycolytic enzymes. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Disorders of glycolytic enzymes US Medical PG Question 1: A 3-year-old boy is brought to the physician because of a 1-week history of yellowish discoloration of his eyes and skin. He has had generalized fatigue and mild shortness of breath for the past month. Three weeks ago, he was treated for a urinary tract infection with antibiotics. His father underwent a splenectomy during childhood. Examination shows pale conjunctivae and jaundice. The abdomen is soft and nontender; there is nontender splenomegaly. Laboratory studies show:
Hemoglobin 9.1 g/dL
Mean corpuscular volume 89 μm3
Mean corpuscular hemoglobin 32 pg/cell
Mean corpuscular hemoglobin concentration 37.8% Hb/cell
Leukocyte count 7800/mm3
Platelet count 245,000/mm3
Red cell distribution width 22.8% (N=13%–15%)
Serum
Bilirubin
Total 13.8 mg/dL
Direct 1.9 mg/dL
Lactate dehydrogenase 450 U/L
Which of the following is the most likely pathophysiology of these findings?
- A. Deficient glucose-6 phosphate dehydrogenase
- B. Decreased synthesis of alpha chains of hemoglobin
- C. Increased hemoglobin S
- D. Decreased spectrin in the RBC membrane (Correct Answer)
- E. Deficiency of pyruvate kinase
Disorders of glycolytic enzymes Explanation: ***Decreased spectrin in the RBC membrane***
- This presentation is highly suggestive of **hereditary spherocytosis**, characterized by **defects in red blood cell membrane proteins** like **spectrin**, ankyrin, or band 3 protein.
- The patient's features—**jaundice**, **anemia**, **splenomegaly**, elevated **indirect bilirubin**, increased **LDH**, high **MCHC**, and a family history of splenectomy (often a treatment for hereditary spherocytosis)—point to this diagnosis.
*Deficient glucose-6 phosphate dehydrogenase*
- **G6PD deficiency** typically presents with **hemolytic anemia** following exposure to **oxidative stressors** (e.g., certain drugs, fava beans, infections).
- While an infection might trigger hemolysis, the chronic nature of the symptoms, **splenomegaly**, and high MCHC are less typical for G6PD deficiency.
*Decreased synthesis of alpha chains of hemoglobin*
- This describes **alpha thalassemia**, which would present with **microcytic hypochromic anemia** (low MCV, low MCH) rather than the normal MCV and high MCHC seen here.
- While chronic hemolysis can occur in severe forms, the specific lab values do not align with thalassemia.
*Increased hemoglobin S*
- **Sickle cell anemia** involves **hemoglobin S**, leading to sickling of red blood cells under hypoxic conditions.
- Patients typically experience **vaso-occlusive crises** and different RBC morphology (e.g., sickle cells, target cells) and usually a normocytic or macrocytic anemia, which is not fully consistent with the high MCHC seen here in isolation.
*Deficiency of pyruvate kinase*
- **Pyruvate kinase deficiency** causes **hemolytic anemia** due to impaired glycolysis, leading to insufficient ATP production in RBCs.
- While it presents with chronic hemolysis, **splenomegaly**, and jaundice, it typically does not cause the characteristic **high MCHC** seen in hereditary spherocytosis, nor does it typically present with a positive family history of splenectomy in father.
Disorders of glycolytic enzymes US Medical PG Question 2: A 4-month-old boy is brought to his pediatrician for a well-child visit. His parents have noticed that he has had poor growth compared to his older siblings. The boy was delivered vaginally after a normal pregnancy. His temperature is 98.8°F (37.1°C), blood pressure is 98/68 mmHg, pulse is 88/min, and respirations are 20/min. On exam, his abdomen appears protuberant, and the boy appears to have abnormally enlarged cheeks. A finger stick reveals that the patient’s fasting blood glucose is 50 mg/dL. On further laboratory testing, the patient is found to have elevated blood lactate levels, as well as no response to a glucagon stimulation test. What enzymatic defect is most likely present?
- A. Alpha-1,4-glucosidase
- B. Glycogen synthase
- C. Alpha-1,6-glucosidase
- D. Glucose-6-phosphatase (Correct Answer)
- E. Glycogen phosphorylase
Disorders of glycolytic enzymes Explanation: ***Glucose-6-phosphatase***
- The patient's symptoms, including **hypoglycemia**, **hepatomegaly** (implied by protuberant abdomen), **lactic acidosis** (elevated lactate), and lack of response to **glucagon stimulation**, are classic for **Type I glycogen storage disease (von Gierke disease)**, which is caused by a deficiency in **glucose-6-phosphatase**.
- This enzyme is crucial for the final step of both **glycogenolysis** and **gluconeogenesis**, and its deficiency prevents the liver from releasing glucose into the bloodstream, leading to severe hypoglycemia.
*Alpha-1,4-glucosidase*
- A deficiency in **alpha-1,4-glucosidase (acid maltase)** causes **Type II glycogen storage disease (Pompe disease)**, which primarily affects muscle (cardiac and skeletal).
- Symptoms include **cardiomyopathy**, **hypotonia**, and muscle weakness, and it does **not** typically present with hypoglycemia or lactic acidosis.
*Glycogen synthase*
- A deficiency in **glycogen synthase** would lead to an inability to synthesize glycogen, resulting in **hypoglycemia** but **low** (rather than high) glycogen levels.
- Patients typically experience fasting hypoglycemia, but **no hepatomegaly** or lactic acidosis would be expected.
*Alpha-1,6-glucosidase*
- A deficiency in **alpha-1,6-glucosidase (debranching enzyme)** causes **Type III glycogen storage disease (Cori disease)**.
- This condition presents with **hepatomegaly**, **hypoglycemia**, and sometimes muscle weakness, but patients typically **do respond to glucagon** and have less severe lactic acidosis compared to Type I.
*Glycogen phosphorylase*
- A deficiency in **glycogen phosphorylase (hepatic form, Type VI GSD or Hers disease)** primarily affects the liver's ability to break down glycogen.
- This typically causes **hepatomegaly** and **hypoglycemia**, but usually, the patients **respond to glucagon** because other pathways for glucose release (like gluconeogenesis) are intact.
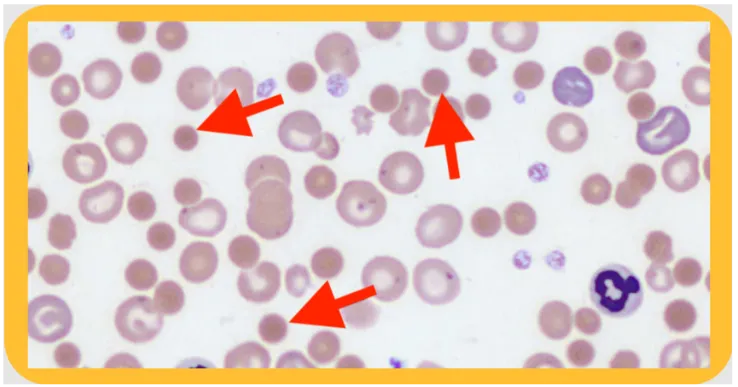
Disorders of glycolytic enzymes US Medical PG Question 3: An 11-year-old boy is brought to the emergency room with acute abdominal pain and hematuria. Past medical history is significant for malaria. On physical examination, he has jaundice and a generalized pallor. His hemoglobin is 5 g/dL, and his peripheral blood smear reveals fragmented RBC, microspherocytes, and eccentrocytes (bite cells). Which of the following reactions catalyzed by the enzyme is most likely deficient in this patient?
- A. Glucose-1-phosphate + UTP → UDP-glucose + pyrophosphate
- B. Glucose + ATP → Glucose-6-phosphate + ADP + H+
- C. D-glucose 6-phosphate → D-fructose-6-phosphate
- D. Glucose-6-phosphate + H2O → glucose + Pi
- E. D-glucose-6-phosphate + NADP+ → 6-phospho-D-glucono-1,5-lactone + NADPH + H+ (Correct Answer)
Disorders of glycolytic enzymes Explanation: ***D-glucose-6-phosphate + NADP+ → 6-phospho-D-glucono-1,5-lactone + NADPH + H+***
- This reaction is catalyzed by **glucose-6-phosphate dehydrogenase (G6PD)**, an enzyme critical for the production of **NADPH** in the **pentose phosphate pathway**.
- **NADPH** is essential for reducing **oxidative stress** in red blood cells. A deficiency in G6PD leads to increased susceptibility to hemolysis, especially under oxidative triggers like malaria, resulting in symptoms such as **acute hemolytic anemia**, jaundice, and specific morphological changes (e.g., **fragmented RBCs**, **microspherocytes**, and **eccentrocytes**, also known as **bite cells**).
*Glucose-1-phosphate + UTP → UDP-glucose + pyrophosphate*
- This reaction is catalyzed by **UDP-glucose pyrophosphorylase** and is important for **glycogen synthesis**.
- A deficiency in this enzyme would primarily affect glycogen metabolism and would not explain the **hemolytic anemia** or the characteristic red blood cell morphology seen in the patient.
*Glucose + ATP → Glucose-6-phosphate + ADP + H+*
- This reaction is catalyzed by **hexokinase**, the first committed step in **glycolysis**.
- While hexokinase deficiency can cause **hemolytic anemia**, it generally presents with chronic, moderate anemia and does not typically involve the specific red blood cell morphology (eccentrocytes/bite cells) associated with oxidative damage found in G6PD deficiency.
*D-glucose 6-phosphate → D-fructose-6-phosphate*
- This reaction is catalyzed by **phosphoglucose isomerase** (also known as phosphohexose isomerase) and is part of **glycolysis**.
- A deficiency in this enzyme would impair glycolysis and lead to **hemolytic anemia**, but its clinical presentation and RBC morphology differ from what is typically seen in G6PD deficiency, particularly the absence of oxidative stress markers like bite cells.
*Glucose-6-phosphate + H2O → glucose + Pi*
- This reaction is catalyzed by **glucose-6-phosphatase**, an enzyme found primarily in the liver and kidney, responsible for the final step in **gluconeogenesis** and glycogenolysis to release free glucose into the bloodstream.
- A deficiency in glucose-6-phosphatase leads to **glycogen storage disease type I (Von Gierke's disease)**, characterized by **hypoglycemia**, **lactic acidosis**, and hepatomegaly, not hemolytic anemia.
Disorders of glycolytic enzymes US Medical PG Question 4: A 5-month-old boy presents with increasing weakness for the past 3 months. The patient’s mother says that the weakness is accompanied by dizziness, sweating, and vertigo early in the morning. Physical examination shows hepatomegaly. Laboratory findings show an increased amount of lactate, uric acid, and elevated triglyceride levels. Which of the following enzymes is most likely deficient in this patient?
- A. Hepatic glycogen phosphorylase
- B. Debranching enzyme
- C. Glucose-6-phosphatase (Correct Answer)
- D. Muscle glycogen phosphorylase
- E. Lysosomal α-1,4-glucosidase
Disorders of glycolytic enzymes Explanation: ***Glucose-6-phosphatase***
- The constellation of **hypoglycemia** (weakness, dizziness, sweating, vertigo, especially early morning), **hepatomegaly**, **lactic acidosis**, **hyperuricemia**, and **hypertriglyceridemia** are classic features of **Type I glycogen storage disease (von Gierke disease)**, which is caused by a deficiency of **glucose-6-phosphatase**.
- This enzyme is crucial for the final step of both **glycogenolysis** and **gluconeogenesis**, releasing free glucose into the bloodstream; its deficiency leads to an inability to maintain normal blood glucose levels during fasting and accumulation of glucose-6-phosphate, which shunts into other metabolic pathways.
*Hepatic glycogen phosphorylase*
- Deficiency in **hepatic glycogen phosphorylase** (Type VI glycogen storage disease, Hers disease) would cause **hepatomegaly** and **hypoglycemia**, but typically does not present with severe **lactic acidosis**, **hyperuricemia**, or **hypertriglyceridemia** to the same degree as von Gierke disease.
- The primary defect is in breaking down glycogen, leading to its accumulation in the liver, but the products of glycolysis can still exit the liver via gluconeogenesis.
*Debranching enzyme*
- Deficiency in **debranching enzyme** (Type III glycogen storage disease, Cori or Forbes disease) causes **hepatomegaly** and **hypoglycemia**, but usually presents with milder symptoms and less severe **lactic acidosis**, **hyperuricemia**, and **hypertriglyceridemia**.
- Patients often present with symptoms similar to Type I, but muscle involvement is also common, and **glycogen structures with short outer branches** are characteristic.
*Muscle glycogen phosphorylase*
- Deficiency in **muscle glycogen phosphorylase** (Type V glycogen storage disease, McArdle disease) primarily affects **skeletal muscle**, leading to exercise intolerance, muscle pain, and myoglobinuria.
- It does not typically cause **hypoglycemia** or **hepatomegaly**, as the liver enzyme is functional, and the symptoms described are systemic rather than muscle-specific.
*Lysosomal α-1,4-glucosidase*
- Deficiency in **lysosomal α-1,4-glucosidase** (Type II glycogen storage disease, Pompe disease) primarily affects the **heart, muscle, and liver**, causing severe **cardiomyopathy**, hypotonia, and **hepatomegaly**.
- While it involves glycogen accumulation, it typically does not present with **hypoglycemia** (as cytoplasmic glycogen metabolism is intact), **lactic acidosis**, or the specific metabolic derangements seen in this patient.
Disorders of glycolytic enzymes US Medical PG Question 5: A 9-month-old girl is brought to the physician because of a 1-month history of poor feeding and irritability. She is at the 15th percentile for height and 5th percentile for weight. Examination shows hypotonia and wasting of skeletal muscles. Cardiopulmonary examination shows no abnormalities. There is hepatomegaly. Her serum glucose is 61 mg/dL, creatinine kinase is 100 U/L, and lactic acid is within the reference range. Urine ketone bodies are elevated. Which of the following enzymes is most likely deficient in this patient?
- A. Glucose-6-phosphatase
- B. Muscle phosphorylase
- C. Acid alpha-glucosidase
- D. Glycogen debrancher (Correct Answer)
- E. Glucocerebrosidase
Disorders of glycolytic enzymes Explanation: ***Glycogen debrancher***
- The patient's symptoms of **hepatomegaly**, **hypoglycemia**, **poor feeding**, **growth failure**, and **elevated urine ketones** in the presence of normal lactic acid suggest Type III glycogen storage disease (Cori disease), caused by a deficiency in **glycogen debrancher enzyme**.
- **Muscle wasting** and **hypotonia** are also consistent with Type III GSD, as the debranching enzyme is present in both liver and muscle.
*Glucose-6-phosphatase*
- Deficiency in **glucose-6-phosphatase** (Type I GSD, Von Gierke disease) also presents with **hepatomegaly** and **hypoglycemia**.
- However, Type I GSD is characterized by **lactic acidosis**, which is explicitly stated as normal in this patient, and **hyperlipidemia**, which is not mentioned.
*Muscle phosphorylase*
- Deficiency in **muscle phosphorylase** (Type V GSD, McArdle disease) primarily affects skeletal muscle, causing **exercise intolerance** and **muscle pain**.
- It does not typically present with **hypoglycemia**, **hepatomegaly**, or **growth failure** in infancy.
*Acid alpha-glucosidase*
- Deficiency in **acid alpha-glucosidase** (Type II GSD, Pompe disease) causes accumulation of glycogen in lysosomes, leading to severe **cardiomyopathy**, **hypotonia**, and **muscle weakness**.
- While hypotonia is present, the absence of **cardiomegaly** and significant **liver involvement** makes this diagnosis less likely.
*Glucocerebrosidase*
- Deficiency in **glucocerebrosidase** causes Gaucher disease, a lysosomal storage disorder, not a glycogen storage disorder.
- Symptoms include **hepatosplenomegaly**, **bone crises**, and neurological symptoms, but not **hypoglycemia** or isolated muscle wasting directly related to glycogen metabolism.
Disorders of glycolytic enzymes US Medical PG Question 6: To maintain blood glucose levels even after glycogen stores have been depleted, the body, mainly the liver, is able to synthesize glucose in a process called gluconeogenesis. Which of the following reactions of gluconeogenesis requires an enzyme different from glycolysis?
- A. Fructose 1,6-bisphosphate --> Fructose-6-phosphate (Correct Answer)
- B. Glyceraldehyde 3-phosphate --> 1,3-bisphosphoglycerate
- C. 2-phosphoglycerate --> 3-phosphoglycerate
- D. Dihydroxyacetone phosphate --> Glyceraldehyde 3-phosphate
- E. Phosphoenolpyruvate --> 2-phosphoglycerate
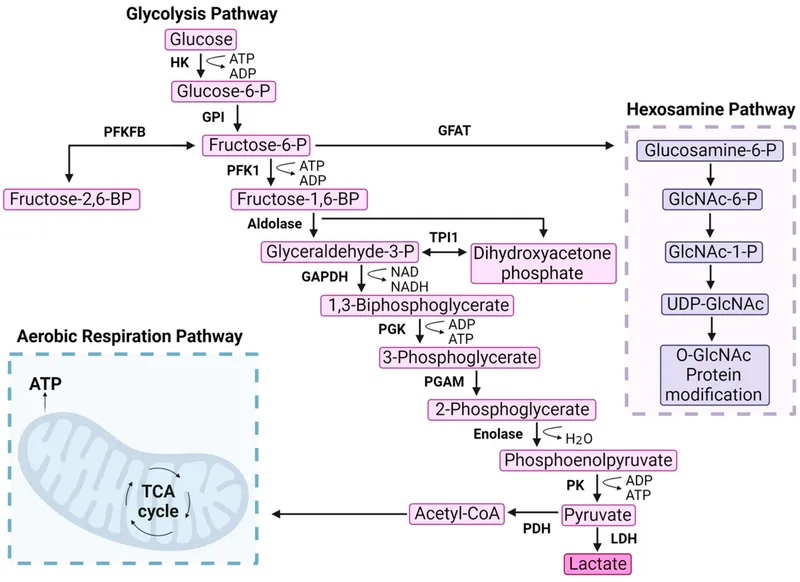
Disorders of glycolytic enzymes Explanation: ***Fructose 1,6-bisphosphate --> Fructose-6-phosphate***
- This reaction in gluconeogenesis is catalyzed by **fructose 1,6-bisphosphatase**, which is distinct from **phosphofructokinase-1** that catalyzes the reverse reaction in glycolysis.
- This step is one of the three **irreversible steps** in glycolysis that must be bypassed by different enzymes in gluconeogenesis to ensure the unidirectional flow of the pathway.
*Glyceraldehyde 3-phosphate --> 1,3-bisphosphoglycerate*
- This reaction is catalyzed by **Glyceraldehyde 3-phosphate dehydrogenase** in both glycolysis and gluconeogenesis, as it is a **reversible step**.
- In gluconeogenesis, the equilibrium is shifted towards the formation of glyceraldehyde 3-phosphate due to the low concentration of products.
*2-phosphoglycerate --> 3-phosphoglycerate*
- This is a reversible isomerization reaction catalyzed by **phosphoglycerate mutase** in both glycolysis and gluconeogenesis.
- No unique enzyme is required for gluconeogenesis at this step.
*Dihydroxyacetone phosphate --> Glyceraldehyde 3-phosphate*
- This reversible interconversion between these two triose phosphates is catalyzed by **triose phosphate isomerase** in both pathways.
- These molecules are in equilibrium and can be readily converted from one to the other.
*Phosphoenolpyruvate --> 2-phosphoglycerate*
- This is a reversible reaction catalyzed by **enolase** in both glycolysis and gluconeogenesis.
- No distinct enzyme is needed for this step in gluconeogenesis.
Disorders of glycolytic enzymes US Medical PG Question 7: A 16-year-old teenager is brought to the emergency department after having slipped on ice while walking to school. She hit her head on the side of the pavement and retained consciousness. She was brought to the closest ER within an hour of the incident. The ER physician sends her immediately to get a CT scan and also orders routine blood work. The physician understands that in cases of stress, such as in this patient, the concentration of certain hormones will be increased, while others will be decreased. Considering allosteric regulation by hormones, which of the following enzymes will most likely be inhibited in this patient?
- A. Glucose-6-phosphatase
- B. Fructose 1,6-bisphosphatase
- C. Pyruvate carboxylase
- D. Phosphofructokinase (Correct Answer)
- E. Glycogen phosphorylase
Disorders of glycolytic enzymes Explanation: ***Phosphofructokinase***
- In a stress state, **cortisol** and **epinephrine** levels are elevated, leading to increased **gluconeogenesis** and **glycogenolysis** to provide rapid energy.
- **Allosteric inhibition** of PFK-1 occurs through multiple mechanisms:
- **ATP** and **citrate** (high energy signals) act as direct **allosteric inhibitors** of PFK-1
- **Glucagon** (elevated during stress) indirectly inhibits PFK-1 by reducing levels of **fructose-2,6-bisphosphate**, a potent allosteric activator
- This inhibition of glycolysis spares glucose for critical organs like the brain and heart.
*Glucose-6-phosphatase*
- This enzyme catalyzes the final step of **gluconeogenesis** and **glycogenolysis**, converting G6P to free glucose.
- During stress, its activity is **stimulated** to increase blood glucose levels, not inhibited.
*Fructose 1,6-bisphosphatase*
- This enzyme plays a key role in **gluconeogenesis**, a process vital for maintaining glucose homeostasis during stress.
- Its activity would be **upregulated** to produce glucose, rather than inhibited.
*Pyruvate carboxylase*
- This enzyme initiates **gluconeogenesis** by converting pyruvate to oxaloacetate in the mitochondria.
- During stress, its activity is **stimulated** by elevated acetyl-CoA (an allosteric activator), not inhibited.
*Glycogen phosphorylase*
- This enzyme is responsible for **glycogenolysis**, the breakdown of glycogen into glucose-1-phosphate.
- Its activity is **stimulated** by stress hormones (epinephrine and glucagon) through cAMP-mediated phosphorylation, ensuring rapid glucose availability.
Disorders of glycolytic enzymes US Medical PG Question 8: An investigator is studying the changes that occur in the oxygen-hemoglobin dissociation curve of different types of hemoglobin under various conditions. The blood obtained from a male infant shows decreased affinity for 2,3-bisphosphoglyceric acid. Which of the following is the most likely composition of the hemoglobin molecule in this sample?
- A. α2βS2
- B. α2β2
- C. α2δ2
- D. α2γ2 (Correct Answer)
- E. β4
Disorders of glycolytic enzymes Explanation: ***α2γ2***
- This formula represents **fetal hemoglobin (HbF)**, which is the predominant hemoglobin in infants.
- HbF has **decreased affinity for 2,3-bisphosphoglyceric acid (2,3-BPG)** compared to adult hemoglobin (HbA) because 2,3-BPG binds less avidly to the gamma chains.
- This decreased 2,3-BPG binding results in HbF having **higher oxygen affinity** than HbA (left-shifted oxygen-hemoglobin dissociation curve).
- The higher oxygen affinity allows fetal blood to efficiently extract oxygen from maternal blood across the placenta.
*α2βS2*
- This represents **hemoglobin S (HbS)**, found in **sickle cell disease**.
- HbS has similar 2,3-BPG binding to HbA, not decreased affinity.
- Its primary characteristic is polymerization and red blood cell sickling under deoxygenated conditions.
*α2β2*
- This represents **adult hemoglobin (HbA)**, the most common type of hemoglobin in adults.
- HbA has **higher affinity for 2,3-BPG** compared to HbF because 2,3-BPG binds strongly to the beta chains.
- The binding of 2,3-BPG to HbA decreases oxygen affinity, facilitating oxygen release to tissues.
*α2δ2*
- This represents **hemoglobin A2 (HbA2)**, a minor component of adult hemoglobin (typically <3.5%).
- HbA2 has normal 2,3-BPG binding similar to HbA, not decreased affinity.
- This doesn't fit the clinical description of an infant with decreased 2,3-BPG affinity.
*β4*
- This represents **hemoglobin H (HbH)**, which occurs in **alpha-thalassemia** where there is an excess of beta chains that form tetramers.
- HbH has **extremely high oxygen affinity** and does not release oxygen well to tissues.
- While HbH also has decreased 2,3-BPG binding, it is not found in healthy infants and represents a pathological condition.
Disorders of glycolytic enzymes US Medical PG Question 9: A 16-year-old boy comes to the physician because of muscle weakness and cramps for 5 months. He becomes easily fatigued and has severe muscle pain and swelling after 15 minutes of playing basketball with his friends. The symptoms improve after a brief period of rest. After playing, he sometimes also has episodes of reddish-brown urine. There is no family history of serious illness. Serum creatine kinase concentration is 950 U/L. Urinalysis shows:
Blood 2+
Protein negative
Glucose negative
RBC negative
WBC 1–2/hpf
Which of the following is the most likely underlying cause of this patient's symptoms?
- A. Medium-chain acyl-CoA dehydrogenase deficiency
- B. Myophosphorylase deficiency (Correct Answer)
- C. Low levels of triiodothyronine and thyroxine
- D. Acid maltase deficiency
- E. CTG repeat in the DMPK gene
Disorders of glycolytic enzymes Explanation: ***Myophosphorylase deficiency***
- This condition (McArdle disease) is an **autosomal recessive disorder** of glycogen metabolism characterized by a defect in **glycogenolysis**, specifically the breakdown of muscle glycogen. This leads to impaired energy production during exercise.
- The classic presentation includes **exercise-induced muscle pain, stiffness, cramps, fatigue**, and sometimes **myoglobinuria** (reddish-brown urine due to myoglobin release from damaged muscle), which is consistent with the patient's symptoms and elevated **creatine kinase**.
*Medium-chain acyl-CoA dehydrogenase deficiency*
- This is a disorder of **fatty acid oxidation** that primarily affects the liver, leading to episodes of **hypoketotic hypoglycemia** during fasting or illness.
- It does not typically present with isolated exercise-induced muscle pain and myoglobinuria.
*Low levels of triiodothyronine and thyroxine*
- **Hypothyroidism** can cause generalized muscle weakness, fatigue, and muscle cramps, but it is usually associated with other systemic symptoms like weight gain, cold intolerance, and constipation.
- While it can cause elevated CK, it generally does not present with acute, exercise-induced muscle pain and myoglobinuria in the manner described.
*Acid maltase deficiency*
- This (Pompe disease) is a lysosomal storage disorder affecting glycogen metabolism, but it results from a deficiency of **acid alpha-glucosidase (acid maltase)**.
- The infantile form presents with severe hypotonia and cardiomyopathy, while the juvenile and adult forms typically cause **proximal muscle weakness** and respiratory insufficiency, rather than exercise-induced muscle pain and myoglobinuria.
*CTG repeat in the DMPK gene*
- This genetic defect is associated with **myotonic dystrophy type 1 (Steinert disease)**, an autosomal dominant disorder.
- Key features include **myotonia** (delayed relaxation of muscles), muscle weakness, cataracts, and cardiac conduction abnormalities, which are distinct from the patient's presentation of exercise-induced cramps and myoglobinuria without myotonia.
Disorders of glycolytic enzymes US Medical PG Question 10: A 3-month-old African American infant presents to the hospital with 2 days of fever, "coke"-colored urine, and jaundice. The pregnancy was uneventful except the infant was found to have hyperbilirubinemia that was treated with phototherapy. The mother explains that she breastfeeds her child and recently was treated herself for a UTI with trimethoprim-sulfamethoxazole (TMP-SMX). Which of the following diseases is similarly inherited as the disease experienced by the child?
- A. Hemophilia A (Correct Answer)
- B. Rett syndrome
- C. Beta thalassemia
- D. Sickle cell anemia
- E. Marfan syndrome
Disorders of glycolytic enzymes Explanation: ***Hemophilia A***
- The infant's symptoms (**fever**, **coke-colored urine**, **jaundice**, and history of **hyperbilirubinemia**) following exposure to **trimethoprim-sulfamethoxazole (TMP-SMX)** suggest **glucose-6-phosphate dehydrogenase (G6PD) deficiency**, an X-linked recessive condition.
- **Hemophilia A** is also an **X-linked recessive disorder**, making its inheritance pattern similar to G6PD deficiency.
*Rett syndrome*
- **Rett syndrome** is an **X-linked dominant** neurodevelopmental disorder, primarily affecting females severely and often embryonically lethal in males.
- Its inheritance pattern differs significantly from the X-linked recessive inheritance of G6PD deficiency.
*Beta thalassemia*
- **Beta thalassemia** is an **autosomal recessive** blood disorder, meaning it is inherited through genes located on non-sex chromosomes.
- This inheritance pattern is distinct from the X-linked recessive pattern of G6PD deficiency.
*Sickle cell anemia*
- **Sickle cell anemia** is an **autosomal recessive** hereditary blood disorder, with the gene located on chromosome 11.
- Its inheritance pathway is different from the X-linked recessive genetic inheritance seen in G6PD deficiency.
*Marfan syndrome*
- **Marfan syndrome** is an **autosomal dominant** disorder affecting connective tissue, the gene for which is located on chromosome 15.
- This mode of inheritance is distinctly different from the X-linked recessive pattern of inheritance.
More Disorders of glycolytic enzymes US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.