GSD type VII (Tarui disease) US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for GSD type VII (Tarui disease). These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
GSD type VII (Tarui disease) US Medical PG Question 1: A 4-month-old boy is brought to his pediatrician for a well-child visit. His parents have noticed that he has had poor growth compared to his older siblings. The boy was delivered vaginally after a normal pregnancy. His temperature is 98.8°F (37.1°C), blood pressure is 98/68 mmHg, pulse is 88/min, and respirations are 20/min. On exam, his abdomen appears protuberant, and the boy appears to have abnormally enlarged cheeks. A finger stick reveals that the patient’s fasting blood glucose is 50 mg/dL. On further laboratory testing, the patient is found to have elevated blood lactate levels, as well as no response to a glucagon stimulation test. What enzymatic defect is most likely present?
- A. Alpha-1,4-glucosidase
- B. Glycogen synthase
- C. Alpha-1,6-glucosidase
- D. Glucose-6-phosphatase (Correct Answer)
- E. Glycogen phosphorylase
GSD type VII (Tarui disease) Explanation: ***Glucose-6-phosphatase***
- The patient's symptoms, including **hypoglycemia**, **hepatomegaly** (implied by protuberant abdomen), **lactic acidosis** (elevated lactate), and lack of response to **glucagon stimulation**, are classic for **Type I glycogen storage disease (von Gierke disease)**, which is caused by a deficiency in **glucose-6-phosphatase**.
- This enzyme is crucial for the final step of both **glycogenolysis** and **gluconeogenesis**, and its deficiency prevents the liver from releasing glucose into the bloodstream, leading to severe hypoglycemia.
*Alpha-1,4-glucosidase*
- A deficiency in **alpha-1,4-glucosidase (acid maltase)** causes **Type II glycogen storage disease (Pompe disease)**, which primarily affects muscle (cardiac and skeletal).
- Symptoms include **cardiomyopathy**, **hypotonia**, and muscle weakness, and it does **not** typically present with hypoglycemia or lactic acidosis.
*Glycogen synthase*
- A deficiency in **glycogen synthase** would lead to an inability to synthesize glycogen, resulting in **hypoglycemia** but **low** (rather than high) glycogen levels.
- Patients typically experience fasting hypoglycemia, but **no hepatomegaly** or lactic acidosis would be expected.
*Alpha-1,6-glucosidase*
- A deficiency in **alpha-1,6-glucosidase (debranching enzyme)** causes **Type III glycogen storage disease (Cori disease)**.
- This condition presents with **hepatomegaly**, **hypoglycemia**, and sometimes muscle weakness, but patients typically **do respond to glucagon** and have less severe lactic acidosis compared to Type I.
*Glycogen phosphorylase*
- A deficiency in **glycogen phosphorylase (hepatic form, Type VI GSD or Hers disease)** primarily affects the liver's ability to break down glycogen.
- This typically causes **hepatomegaly** and **hypoglycemia**, but usually, the patients **respond to glucagon** because other pathways for glucose release (like gluconeogenesis) are intact.
GSD type VII (Tarui disease) US Medical PG Question 2: A 12-year-old male presents to the pediatrician after two days of tea-colored urine which appeared to coincide with the first day of junior high football. He explains that he refused to go back to practice because he was humiliated by the other players due to his quick and excessive fatigue after a set of drills accompanied by pain in his muscles. A blood test revealed elevated creatine kinase and myoglobulin levels. A muscle biopsy was performed revealing large glycogen deposits and an enzyme histochemistry showed a lack of myophosphorylase activity. Which of the following reactions is not occurring in this individual?
- A. Cleaving alpha-1,6 glycosidic bonds from glycogen
- B. Creating alpha-1,6 glycosidic bonds in glycogen
- C. Breaking down glycogen to glucose-1-phosphate (Correct Answer)
- D. Converting glucose-6-phosphate to glucose
- E. Converting galactose to galactose-1-phosphate
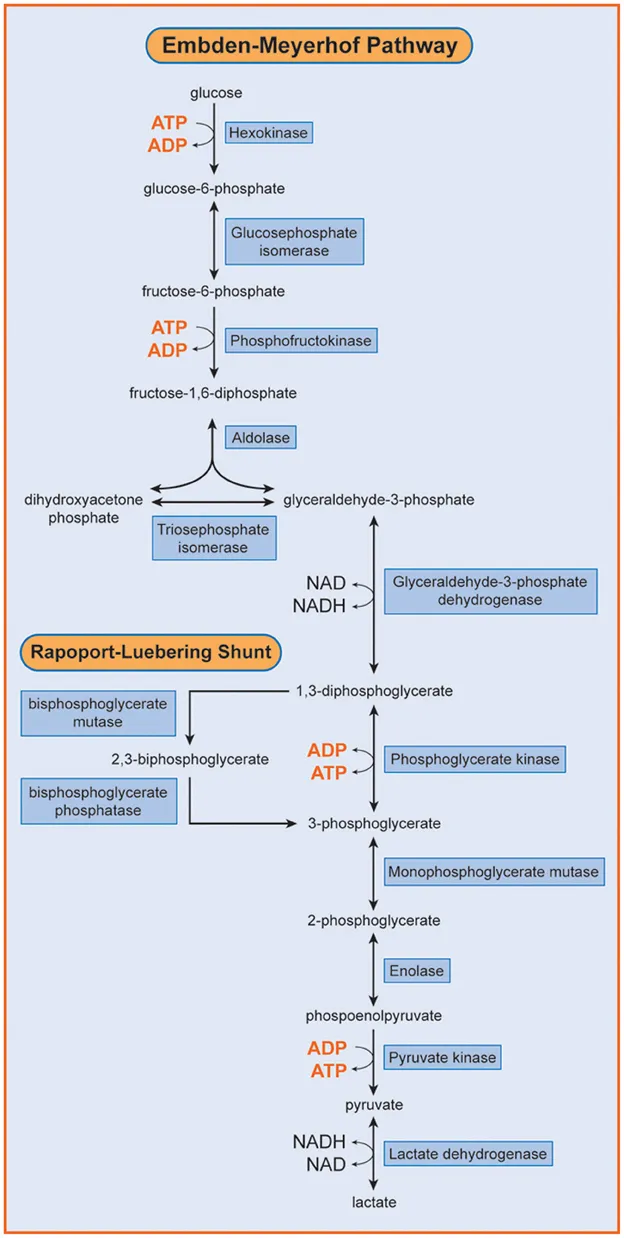
GSD type VII (Tarui disease) Explanation: ***Breaking down glycogen to glucose-1-phosphate***
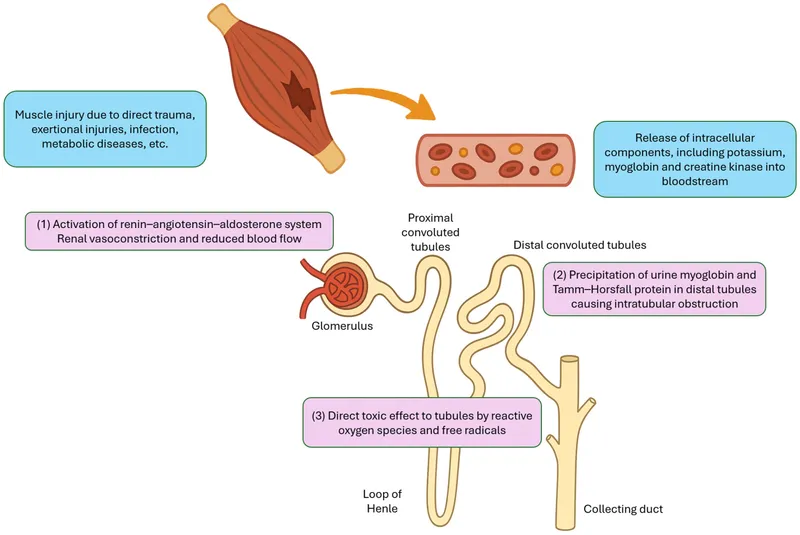
- The patient's symptoms (muscle pain, quick fatigue during exercise, tea-colored urine indicating **rhabdomyolysis**) and laboratory findings (**elevated creatine kinase and myoglobin**, **large glycogen deposits** in muscle, and **lack of myophosphorylase activity**) are classic for **McArdle disease (Glycogen Storage Disease Type V).**
- **Myophosphorylase** (also known as **glycogen phosphorylase**) is the enzyme responsible for breaking down glycogen into **glucose-1-phosphate** in muscle, so this reaction is severely impaired.
*Cleaving alpha-1,6 glycosidic bonds from glycogen*
- This reaction is catalyzed by the **debranching enzyme** (specifically, its **oligo-1,6-glucosidase** activity), not myophosphorylase.
- The debranching enzyme is crucial for completely breaking down glycogen, but its deficiency would lead to different clinical and histopathological findings (e.g., accumulation of **dextrin-like structures**).
*Creating alpha-1,6 glycosidic bonds in glycogen*
- This is the function of the **branching enzyme**, which introduces branches into the glycogen structure.
- This process is part of **glycogen synthesis**, not degradation, and is not directly affected by myophosphorylase deficiency.
*Converting glucose-6-phosphate to glucose*
- This reaction primarily occurs in the liver and kidneys, catalyzed by **glucose-6-phosphatase**, to release glucose into the bloodstream.
- While muscle cells can produce glucose-6-phosphate from glycogen, they lack glucose-6-phosphatase, so they cannot release free glucose into the blood. This reaction is irrelevant to the primary defect here.
*Converting galactose to galactose-1-phosphate*
- This is an initial step in **galactose metabolism**, catalyzed by **galactokinase**.
- This metabolic pathway is entirely separate from glycogen metabolism and is not implicated in McArdle disease.
GSD type VII (Tarui disease) US Medical PG Question 3: A 42-year-old man comes to the physician because of a 2-month history of fatigue and increased urination. The patient reports that he has been drinking more than usual because he is constantly thirsty. He has avoided driving for the past 8 weeks because of intermittent episodes of blurred vision. He had elevated blood pressure at his previous visit but is otherwise healthy. Because of his busy work schedule, his diet consists primarily of fast food. He does not smoke or drink alcohol. He is 178 cm (5 ft 10 in) tall and weighs 109 kg (240 lb); BMI is 34 kg/m2. His pulse is 75/min and his blood pressure is 148/95 mm Hg. Cardiopulmonary examination shows no abnormalities. Laboratory studies show:
Hemoglobin A1c 6.8%
Serum
Glucose 180 mg/dL
Creatinine 1.0 mg/dL
Total cholesterol 220 mg/dL
HDL cholesterol 50 mg/dL
Triglycerides 140 mg/dL
Urine
Blood negative
Glucose 2+
Protein 1+
Ketones negative
Which of the following is the most appropriate next step in management?
- A. Metformin therapy (Correct Answer)
- B. Low-carbohydrate diet
- C. Aspirin therapy
- D. ACE inhibitor therapy
- E. Insulin therapy
GSD type VII (Tarui disease) Explanation: ***Metformin therapy***
- This patient has **newly diagnosed type 2 diabetes mellitus** with classic symptoms (polyuria, polydipsia, blurred vision) and laboratory confirmation (HbA1c 6.8%, glucose 180 mg/dL, glucosuria).
- **Metformin is the first-line pharmacologic therapy** for type 2 diabetes according to current guidelines (ADA, AACE) due to its efficacy, safety profile, cardiovascular benefits, and low risk of hypoglycemia.
- The patient's creatinine is normal (1.0 mg/dL), so metformin is not contraindicated.
- Addressing the **symptomatic hyperglycemia** is the most appropriate next step in management.
*ACE inhibitor therapy*
- ACE inhibitors are indicated for diabetic patients with **hypertension and albuminuria** to provide renoprotection and slow progression of diabetic nephropathy.
- While this patient has both hypertension (148/95 mm Hg) and proteinuria (1+), ACE inhibitor therapy should be initiated **after or concurrent with diabetes management**, not as the sole initial intervention.
- The patient needs **glycemic control first** given symptomatic hyperglycemia, though ACE inhibitor would be an appropriate addition to the treatment regimen.
*Low-carbohydrate diet*
- **Lifestyle modifications** including medical nutrition therapy and exercise are foundational for managing type 2 diabetes and should be recommended.
- However, given the patient's **symptomatic hyperglycemia** (HbA1c 6.8%, glucose 180 mg/dL with classic symptoms), lifestyle changes alone are **insufficient as the initial management**.
- Pharmacologic therapy with metformin should be initiated immediately alongside lifestyle counseling.
*Insulin therapy*
- Insulin therapy is indicated for patients with **very high HbA1c** (typically >9-10%), **severe symptoms of hyperglycemia**, evidence of catabolism, or failure of oral agents.
- This patient's HbA1c of 6.8% represents **relatively mild hyperglycemia** that is appropriately managed with metformin as first-line therapy.
- Insulin is **not indicated** at this stage of disease.
*Aspirin therapy*
- **Aspirin for primary prevention** in diabetes is controversial; current guidelines suggest shared decision-making for patients at increased cardiovascular risk without high bleeding risk.
- While this patient has cardiovascular risk factors (diabetes, hypertension, obesity, dyslipidemia), aspirin would be a **secondary priority** after addressing the acute metabolic derangements.
- **Glycemic control takes precedence** over aspirin initiation in newly diagnosed diabetes.
GSD type VII (Tarui disease) US Medical PG Question 4: A 22-year-old man comes to the physician for a routine physical examination. He feels well. He has no history of major medical illness and takes no medications. His vital signs are within normal limits. Examination shows no abnormalities. Laboratory studies, including a complete blood count and a standard electrolyte panel, are within normal limits. Urine dipstick is negative for glucose; a reducing substance test result of the urine is positive. Which of the following is the most appropriate dietary recommendation for this patient?
- A. Eliminate galactose and lactose
- B. Eliminate fructose and sucrose
- C. Increase intake of ketogenic amino acids
- D. Decrease purine intake
- E. No changes needed (Correct Answer)
GSD type VII (Tarui disease) Explanation: ***No changes needed***
- The positive urine reducing substance test with negative urine glucose in an otherwise healthy individual often indicates **essential fructosuria**, a benign condition.
- Essential fructosuria is caused by a deficiency in **fructokinase** and does not require any dietary modifications.
*Eliminate galactose and lactose*
- This recommendation would be appropriate for **galactosemia**, a condition where the body cannot properly metabolize galactose.
- Galactosemia typically presents with more severe symptoms in infancy, such as **failure to thrive**, **jaundice**, and **cataracts**, which are not present here.
*Eliminate fructose and sucrose*
- This is the recommended diet for **hereditary fructose intolerance**, a more severe disorder involving a deficiency of **aldolase B**.
- Hereditary fructose intolerance would lead to symptoms like **hypoglycemia**, **vomiting**, and **liver damage** upon ingestion of fructose, which are absent in this case.
*Increase intake of ketogenic amino acids*
- This dietary approach is typically used for conditions like **pyruvate dehydrogenase complex deficiency** or **glucose transporter type 1 deficiency syndrome (Glut1 deficiency)**.
- These conditions involve metabolic crises or neurological symptoms that are not relevant to the patient's presentation.
*Decrease purine intake*
- A low-purine diet is recommended for conditions associated with **hyperuricemia**, such as **gout** or **Lesch-Nyhan syndrome**.
- There is no indication of elevated uric acid levels or symptoms related to purine metabolism in this patient.
GSD type VII (Tarui disease) US Medical PG Question 5: A 13-year-old boy is brought to the physician by his parents, who are concerned about recurrent muscle cramps he experiences while playing soccer. The boy has always loved sports and has been playing in a soccer league for the past 3 years. He now complains of severe cramping pain in his legs after intense practice sessions. He has no significant medical history. His physical examination is unremarkable. A battery of laboratory tests is ordered and they are all normal. Imaging studies yield no abnormalities as well. Which of the following is most likely deficient in this patient?
- A. Carnitine palmitoyltransferase I
- B. Medium-chain acyl-coenzyme A dehydrogenase
- C. Carnitine palmitoyltransferase II
- D. Phosphofructokinase
- E. Myophosphorylase (Correct Answer)
GSD type VII (Tarui disease) Explanation: ***Myophosphorylase***
- The patient's symptoms of **exercise-induced muscle cramps** and pain, specifically after intense activity, and normal lab findings, are classic for **McArdle disease** (glycogen storage disease type V).
- McArdle disease is caused by a deficiency in **myophosphorylase**, preventing the breakdown of glycogen for energy in muscles during exercise.
*Carnitine palmitoyltransferase I*
- Deficiency in CPT I primarily affects the liver and causes a hypoketotic hypoglycemia, not isolated exercise-induced muscle cramps.
- This enzyme is crucial for the transport of long-chain fatty acids into the mitochondria for beta-oxidation.
*Medium-chain acyl-coenzyme A dehydrogenase*
- MCAD deficiency is characterized by **hypoketotic hypoglycemia** and liver dysfunction, especially during fasting or illness, due to impaired fatty acid oxidation.
- It does not typically present with isolated exercise-induced muscle cramps in an otherwise healthy active adolescent.
*Carnitine palmitoyltransferase II*
- CPT II deficiency can cause **recurrent myoglobinuria** and acute muscle pain precipitated by prolonged exercise, fasting, or cold exposure, which might resemble the patient's symptoms.
- However, the presentation of "severe cramping pain in his legs after intense practice sessions" with normal lab tests points more directly to an issue with carbohydrate metabolism in muscle, making myophosphorylase deficiency a more likely primary diagnosis given the typical onset with intense, high-energy demand activities rather than prolonged exercise or fasting.
*Phosphofructokinase*
- PFK deficiency (Tarui disease) also presents with exercise intolerance, muscle pain, and cramps, and is a type of glycogen storage disease.
- It would typically result in **hemolytic anemia** and elevated bilirubin, which are not mentioned in this patient, and would also lead to an accumulation of glycolytic intermediates, which is not indicated by the normal lab results.
GSD type VII (Tarui disease) US Medical PG Question 6: A 7-year-old boy is brought to his pediatrician by his mother who is worried about his clumsiness. She states that over the past 3 months she has noticed progressive weakness. He used to climb trees and run outside with his cousins, but now he says he gets “too tired.” She’s recently noticed him starting to “walk funny,” despite having “muscular legs.” Upon physical examination, the patient has calf muscle hypertrophy. He uses his arms to rise out of the chair. Labs are obtained that show an elevated creatine kinase. Genetic analysis detects a dystropin gene mutation. A muscle biopsy is performed that reveals reduced dystrophin. Which of the following is the most likely diagnosis?
- A. Fragile X syndrome
- B. Pompe disease
- C. Duchenne muscular dystrophy (Correct Answer)
- D. Spinal muscular atrophy
- E. Becker muscular dystrophy
GSD type VII (Tarui disease) Explanation: ***Duchenne muscular dystrophy***
- This 7-year-old presents with classic features of **Duchenne muscular dystrophy (DMD)**: **progressive proximal muscle weakness**, **calf pseudohypertrophy**, **Gowers' sign** (using arms to rise from a chair), and **markedly elevated creatine kinase**.
- Genetic analysis confirms a **dystrophin gene mutation**, and muscle biopsy shows **reduced dystrophin**, consistent with DMD where dystrophin is absent or severely reduced (<3% of normal).
- The **age of presentation (7 years)** is typical for DMD, as many boys are diagnosed between ages 3-7 when motor delays become apparent in school settings; the recent 3-month history of rapid decline is characteristic of DMD's progressive course.
- Boys with DMD typically lose ambulation by age 12 and require wheelchair assistance, distinguishing it from the milder Becker variant.
*Becker muscular dystrophy*
- While also caused by a **dystrophin gene mutation**, Becker muscular dystrophy (BMD) presents **later** (typically age 8-25) with a **much milder and slower progression**.
- In BMD, dystrophin is **reduced but functional** (3-20% or more of normal, often abnormal in size), not severely deficient as in this case.
- Patients with BMD remain ambulatory into their 20s-30s or beyond, which contrasts with this patient's relatively early onset and rapid 3-month decline.
- The clinical tempo and age of onset in this case are more consistent with Duchenne than Becker.
*Fragile X syndrome*
- This is a genetic disorder primarily characterized by **intellectual disability**, **developmental delays**, **autism spectrum features**, and distinct physical features (long face, large ears, macroorchidism).
- It does not present with **progressive muscle weakness**, **calf pseudohypertrophy**, **elevated CK**, or **dystrophin gene mutations**.
*Pompe disease*
- This is a **lysosomal storage disorder** caused by deficiency of **acid alpha-glucosidase (GAA)**, leading to glycogen accumulation in lysosomes.
- While it can cause **muscle weakness** and elevated CK, infantile-onset Pompe presents with **cardiomyopathy** and **hypotonia** ("floppy infant"), and late-onset Pompe presents with limb-girdle weakness and respiratory failure.
- Pompe does **not involve dystrophin mutations** or **calf pseudohypertrophy**.
*Spinal muscular atrophy*
- This disorder results from **loss of motor neurons** in the spinal cord due to **SMN1 gene mutations**, causing muscle weakness and atrophy.
- SMA presents with **hypotonia**, **areflexia**, and **muscle atrophy** (not hypertrophy), with **fasciculations** of the tongue in some cases.
- It does **not involve dystrophin mutations**, **calf pseudohypertrophy**, or markedly elevated CK levels.
GSD type VII (Tarui disease) US Medical PG Question 7: A 5-month-old boy presents with increasing weakness for the past 3 months. The patient’s mother says that the weakness is accompanied by dizziness, sweating, and vertigo early in the morning. Physical examination shows hepatomegaly. Laboratory findings show an increased amount of lactate, uric acid, and elevated triglyceride levels. Which of the following enzymes is most likely deficient in this patient?
- A. Hepatic glycogen phosphorylase
- B. Debranching enzyme
- C. Glucose-6-phosphatase (Correct Answer)
- D. Muscle glycogen phosphorylase
- E. Lysosomal α-1,4-glucosidase
GSD type VII (Tarui disease) Explanation: ***Glucose-6-phosphatase***
- The constellation of **hypoglycemia** (weakness, dizziness, sweating, vertigo, especially early morning), **hepatomegaly**, **lactic acidosis**, **hyperuricemia**, and **hypertriglyceridemia** are classic features of **Type I glycogen storage disease (von Gierke disease)**, which is caused by a deficiency of **glucose-6-phosphatase**.
- This enzyme is crucial for the final step of both **glycogenolysis** and **gluconeogenesis**, releasing free glucose into the bloodstream; its deficiency leads to an inability to maintain normal blood glucose levels during fasting and accumulation of glucose-6-phosphate, which shunts into other metabolic pathways.
*Hepatic glycogen phosphorylase*
- Deficiency in **hepatic glycogen phosphorylase** (Type VI glycogen storage disease, Hers disease) would cause **hepatomegaly** and **hypoglycemia**, but typically does not present with severe **lactic acidosis**, **hyperuricemia**, or **hypertriglyceridemia** to the same degree as von Gierke disease.
- The primary defect is in breaking down glycogen, leading to its accumulation in the liver, but the products of glycolysis can still exit the liver via gluconeogenesis.
*Debranching enzyme*
- Deficiency in **debranching enzyme** (Type III glycogen storage disease, Cori or Forbes disease) causes **hepatomegaly** and **hypoglycemia**, but usually presents with milder symptoms and less severe **lactic acidosis**, **hyperuricemia**, and **hypertriglyceridemia**.
- Patients often present with symptoms similar to Type I, but muscle involvement is also common, and **glycogen structures with short outer branches** are characteristic.
*Muscle glycogen phosphorylase*
- Deficiency in **muscle glycogen phosphorylase** (Type V glycogen storage disease, McArdle disease) primarily affects **skeletal muscle**, leading to exercise intolerance, muscle pain, and myoglobinuria.
- It does not typically cause **hypoglycemia** or **hepatomegaly**, as the liver enzyme is functional, and the symptoms described are systemic rather than muscle-specific.
*Lysosomal α-1,4-glucosidase*
- Deficiency in **lysosomal α-1,4-glucosidase** (Type II glycogen storage disease, Pompe disease) primarily affects the **heart, muscle, and liver**, causing severe **cardiomyopathy**, hypotonia, and **hepatomegaly**.
- While it involves glycogen accumulation, it typically does not present with **hypoglycemia** (as cytoplasmic glycogen metabolism is intact), **lactic acidosis**, or the specific metabolic derangements seen in this patient.
GSD type VII (Tarui disease) US Medical PG Question 8: A 9-month-old girl is brought to the physician because of a 1-month history of poor feeding and irritability. She is at the 15th percentile for height and 5th percentile for weight. Examination shows hypotonia and wasting of skeletal muscles. Cardiopulmonary examination shows no abnormalities. There is hepatomegaly. Her serum glucose is 61 mg/dL, creatinine kinase is 100 U/L, and lactic acid is within the reference range. Urine ketone bodies are elevated. Which of the following enzymes is most likely deficient in this patient?
- A. Glucose-6-phosphatase
- B. Muscle phosphorylase
- C. Acid alpha-glucosidase
- D. Glycogen debrancher (Correct Answer)
- E. Glucocerebrosidase
GSD type VII (Tarui disease) Explanation: ***Glycogen debrancher***
- The patient's symptoms of **hepatomegaly**, **hypoglycemia**, **poor feeding**, **growth failure**, and **elevated urine ketones** in the presence of normal lactic acid suggest Type III glycogen storage disease (Cori disease), caused by a deficiency in **glycogen debrancher enzyme**.
- **Muscle wasting** and **hypotonia** are also consistent with Type III GSD, as the debranching enzyme is present in both liver and muscle.
*Glucose-6-phosphatase*
- Deficiency in **glucose-6-phosphatase** (Type I GSD, Von Gierke disease) also presents with **hepatomegaly** and **hypoglycemia**.
- However, Type I GSD is characterized by **lactic acidosis**, which is explicitly stated as normal in this patient, and **hyperlipidemia**, which is not mentioned.
*Muscle phosphorylase*
- Deficiency in **muscle phosphorylase** (Type V GSD, McArdle disease) primarily affects skeletal muscle, causing **exercise intolerance** and **muscle pain**.
- It does not typically present with **hypoglycemia**, **hepatomegaly**, or **growth failure** in infancy.
*Acid alpha-glucosidase*
- Deficiency in **acid alpha-glucosidase** (Type II GSD, Pompe disease) causes accumulation of glycogen in lysosomes, leading to severe **cardiomyopathy**, **hypotonia**, and **muscle weakness**.
- While hypotonia is present, the absence of **cardiomegaly** and significant **liver involvement** makes this diagnosis less likely.
*Glucocerebrosidase*
- Deficiency in **glucocerebrosidase** causes Gaucher disease, a lysosomal storage disorder, not a glycogen storage disorder.
- Symptoms include **hepatosplenomegaly**, **bone crises**, and neurological symptoms, but not **hypoglycemia** or isolated muscle wasting directly related to glycogen metabolism.
GSD type VII (Tarui disease) US Medical PG Question 9: A 2-month-old boy is brought to the emergency department 25 minutes after having a seizure. He has had multiple seizures during the past week. His mother has noticed that he has become lethargic and has had a weak cry for the past month. He was born at 37 weeks' gestation. He is at the 20th percentile for height and 15th percentile for weight. His temperature is 36.7°C (98°F), respirations are 50/min, and pulse is 140/min. Examination shows a soft and nontender abdomen. The liver is palpated 4 cm below the right costal margin; there is no splenomegaly. Serum studies show:
Na+ 137 mEq/L
Cl- 103 mEq/L
K+ 3.9 mEq/L
Glucose 32 mg/dL
Calcium 9.6 mg/dL
Total cholesterol 202 mg/dL
Triglycerides 260 mg/dL
Lactate 4.2 mEq/L (N = 0.5 - 2.2 mEq/L)
A deficiency of which of the following enzymes is the most likely cause of this infant's symptoms?
- A. Galactose 1-phosphate uridyltransferase
- B. Glycogen branching enzyme
- C. Glucose 6-phosphatase (Correct Answer)
- D. Fructokinase
- E. Acid maltase
GSD type VII (Tarui disease) Explanation: ***Glucose 6-phosphatase***
- The constellation of **hypoglycemia**, **lactic acidosis**, **hepatomegaly**, and **hyperlipidemia** in an infant is characteristic of **Type I glycogen storage disease (von Gierke's disease)**, which is caused by a deficiency of glucose 6-phosphatase.
- Seizures and lethargy are common manifestations of severe hypoglycemia in infants.
*Galactose 1-phosphate uridyltransferase*
- Deficiency of this enzyme causes **classic galactosemia**, which typically presents with **jaundice**, **cataracts**, **vomiting**, and **failure to thrive**, usually after initiation of milk feeds.
- While patients can develop hepatomegaly and hypoglycemia, the prominent lactic acidosis and hyperlipidemia seen here are less typical.
*Glycogen branching enzyme*
- Deficiency causes **Type IV glycogen storage disease (Andersen's disease)**, characterized by **hepatosplenomegaly**, **failure to thrive**, and progressive cirrhosis.
- Hypoglycemia is generally less severe, and lactic acidosis and hyperlipidemia are not primary features in the same way as Type I GSD.
*Fructokinase*
- Deficiency causes **essential fructosuria**, a benign condition where fructose accumulates in the urine.
- It is typically asymptomatic and does not lead to hypoglycemia, lactic acidosis, or hepatomegaly.
*Acid maltase*
- Deficiency (alpha-1,4-glucosidase) causes **Type II glycogen storage disease (Pompe's disease)**, which primarily affects skeletal and cardiac muscle.
- The infantile form presents with **severe hypotonia** ("floppy baby"), **cardiomyopathy**, and **macroglossia**. Hepatomegaly, hypoglycemia, and lactic acidosis are not prominent features.
GSD type VII (Tarui disease) US Medical PG Question 10: A 2-day-old newborn boy is brought to the emergency department because of apnea, cyanosis, and seizures. He is severely hypoglycemic and does not improve with glucagon administration. His blood pressure is 100/62 mm Hg and heart rate is 75/min. Blood tests show high lactate levels. Physical examination is notable for hepatomegaly. Which of the following enzymes is most likely to be deficient in this baby?
- A. α-ketoacid dehydrogenase
- B. Phenylalanine hydroxylase
- C. Glucose-6-phosphatase (Correct Answer)
- D. Glucocerebrosidase
- E. Sphingomyelinase
GSD type VII (Tarui disease) Explanation: ***Correct: Glucose-6-phosphatase***
- The presentation of severe **hypoglycemia** not responsive to glucagon, coupled with **hepatomegaly** and **lactic acidosis** in a neonate, is highly suggestive of **Type I glycogen storage disease (von Gierke disease)**.
- Deficiency of **glucose-6-phosphatase** prevents the liver from releasing glucose into the bloodstream (the final step of both gluconeogenesis and glycogenolysis), leading to profound hypoglycemia.
- **Key diagnostic clue**: Lack of response to glucagon occurs because glucagon stimulates glycogenolysis, but without functional glucose-6-phosphatase, glucose-6-phosphate cannot be converted to free glucose for release.
- Accumulated glucose-6-phosphate shunts to glycolysis, producing **lactate** (lactic acidosis), and to glycogen synthesis, causing **hepatomegaly**.
*Incorrect: α-ketoacid dehydrogenase*
- Deficiency of **branched-chain α-ketoacid dehydrogenase** causes **maple syrup urine disease (MSUD)**, which presents with poor feeding, vomiting, lethargy, and a characteristic maple syrup odor in urine.
- While MSUD can cause neurological symptoms and seizures, **severe hypoglycemia unresponsive to glucagon** and **hepatomegaly** as primary features are not typical.
*Incorrect: Phenylalanine hydroxylase*
- Deficiency in **phenylalanine hydroxylase** causes **phenylketonuria (PKU)**, which is primarily characterized by intellectual disability, seizures (if untreated), and a musty odor, usually manifesting later in infancy.
- PKU does not present with acute neonatal hypoglycemia, lactic acidosis, or hepatomegaly.
*Incorrect: Glucocerebrosidase*
- Deficiency in **glucocerebrosidase** leads to **Gaucher disease**, a lysosomal storage disorder characterized by hepatosplenomegaly, bone crises, and neurological symptoms in severe infantile forms.
- While hepatomegaly may be present, Gaucher disease does not cause acute, severe neonatal hypoglycemia, lactic acidosis, or lack of response to glucagon.
*Incorrect: Sphingomyelinase*
- Deficiency in **sphingomyelinase** causes **Niemann-Pick disease**, another lysosomal storage disorder, which typically presents with hepatosplenomegaly, neurological deterioration, and "cherry-red spots" in the retina.
- This condition does not cause acute neonatal hypoglycemia, lactic acidosis, or glucagon unresponsiveness.
More GSD type VII (Tarui disease) US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.