GSD type VI (Hers disease) US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for GSD type VI (Hers disease). These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
GSD type VI (Hers disease) US Medical PG Question 1: A 67-year-old man with hypertension comes to the emergency department because of progressively worsening abdominal pain that started 1 week ago. The pain is localized to the right upper quadrant. He has also noticed yellowing of his eyes and skin during this time period. Physical examination shows jaundice, a distended abdomen, and tender hepatomegaly. There is no jugular venous distention. Laboratory studies show a hemoglobin concentration of 19.2 g/dL, aspartate aminotransferase of 420 U/L, alanine aminotransferase of 318 U/L, and total bilirubin of 2.2 mg/dL. Which of the following is the most likely cause of this patient's symptoms?
- A. Thickened pericardium
- B. Hepatic steatosis
- C. Hepatotropic viral infection
- D. Increased iron absorption
- E. Hepatic vein obstruction (Correct Answer)
GSD type VI (Hers disease) Explanation: ***Hepatic vein obstruction***
- The patient presents with **jaundice**, **tender hepatomegaly**, and **elevated transaminases and bilirubin** in the setting of rapidly progressive abdominal pain, suggestive of **Budd-Chiari syndrome** due to hepatic vein obstruction.
- The high **hemoglobin (19.2 g/dL)** indicates **polycythemia**, a common predisposing factor for thrombotic events like hepatic vein obstruction.
*Thickened pericardium*
- A thickened pericardium would lead to **constrictive pericarditis**, presenting with signs of right-sided heart failure like **jugular venous distention** and peripheral edema, which are absent here.
- While it can cause hepatomegaly due to passive congestion, it typically does not cause the acute, severe liver enzyme elevations or the markedly elevated hemoglobin seen in this patient.
*Hepatic steatosis*
- **Hepatic steatosis** (fatty liver) is often asymptomatic or causes mild RUQ pain, typically without significant jaundice or such acutely elevated transaminases.
- It is not associated with polycythemia or a rapid onset of severe symptoms as described.
*Hepatotropic viral infection*
- While hepatotropic viral infections (e.g., hepatitis A, B, C) can cause **jaundice**, **hepatomegaly**, and elevated liver enzymes, they are generally not associated with **polycythemia**.
- The acute, progressive nature with tender hepatomegaly and relatively low bilirubin compared to transaminase elevation might suggest a more obstructive or vascular cause rather than typical viral hepatitis.
*Increased iron absorption*
- **Increased iron absorption** (e.g., in hemochromatosis) leads to iron deposition in the liver, which can cause hepatomegaly and eventually cirrhosis.
- However, it typically has a **chronic, insidious onset** and does not present with acute, severe pain, jaundice, and marked transaminase elevation. While polycythemia can occur in some chronic liver diseases, it's not a direct consequence of iron overload itself in the acute setting described.
GSD type VI (Hers disease) US Medical PG Question 2: A 3-month-old girl is brought to the emergency department by her parents after she appeared to have a seizure at home. On presentation, she no longer has convulsions though she is still noted to be lethargic. She was born through uncomplicated vaginal delivery and was not noted to have any abnormalities at the time of birth. Since then, she has been noted by her pediatrician to be falling behind in height and weight compared to similarly aged infants. Physical exam reveals an enlarged liver, and laboratory tests reveal a glucose of 38 mg/dL. Advanced testing shows that a storage molecule present in the cells of this patient has abnormally short outer chains. Which of the following enzymes is most likely defective in this patient?
- A. Debranching enzyme (Correct Answer)
- B. Hepatic phosphorylase
- C. Glucose-6-phosphatase
- D. Muscle phosphorylase
- E. Branching enzyme
GSD type VI (Hers disease) Explanation: ***Debranching enzyme***
- The presence of **abnormally short outer chains** in a storage molecule, along with **hypoglycemia** and **hepatomegaly**, strongly suggests a defect in the **debranching enzyme** (Type III Glycogen Storage Disease or Cori/Forbes disease). This enzyme is responsible for breaking down the α-1,6 glycosidic bonds at the branch points of glycogen.
- Deficiency leads to the accumulation of glycogen with **short branches**, affecting both liver and muscle.
*Hepatic phosphorylase*
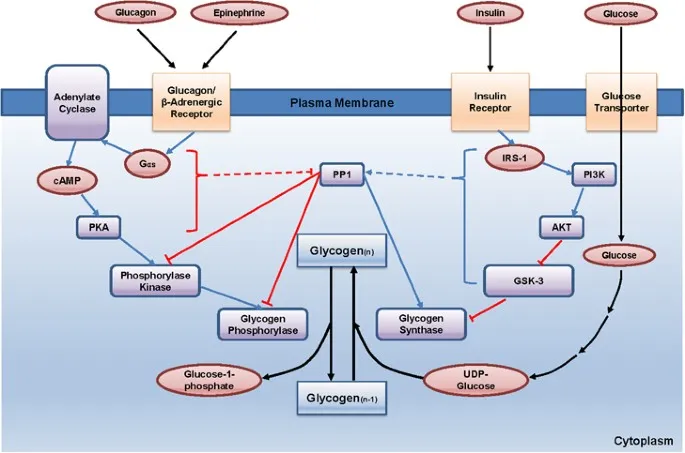
- A defect in **hepatic phosphorylase** (Type VI Glycogen Storage Disease or Hers' disease) leads to similar symptoms like **hepatomegaly** and **hypoglycemia**.
- However, the glycogen structure would be normal, not characterized by abnormally short outer chains.
*Glucose-6-phosphatase*
- A deficiency in **glucose-6-phosphatase** (Type I Glycogen Storage Disease or Von Gierke's disease) leads to severe **hypoglycemia**, **hepatomegaly**, and often **renal enlargement**.
- Glycogen structure in this condition is typically normal, with **increased hepatic glycogen stores**.
*Muscle phosphorylase*
- A deficiency in **muscle phosphorylase** (Type V Glycogen Storage Disease or McArdle's disease) primarily affects skeletal muscle function, causing **muscle cramping**, pain, and **fatigue during exercise**.
- It does not typically present with severe **hypoglycemia** or **hepatomegaly** because the liver enzyme is unaffected.
*Branching enzyme*
- A defect in the **branching enzyme** (Type IV Glycogen Storage Disease or Andersen's disease) results in glycogen with **abnormally long unbranched chains** and fewer branch points.
- This typically leads to **cirrhosis** and liver failure, and while hypoglycemia can occur, the characteristic glycogen structure is the opposite of what is described in the patient.
GSD type VI (Hers disease) US Medical PG Question 3: A 10-year-old boy is brought to the emergency department due to vomiting and weakness. He is attending a summer camp and was on a hike with the other kids and a camp counselor. His friends say that the boy skipped breakfast, and the counselor says he forgot to pack snacks for the kids during the hike. The child’s parents are contacted and report that the child has been completely healthy since birth. They also say there is an uncle who would have to eat regularly or he would have similar symptoms. At the hospital, his heart rate is 90/min, respiratory rate is 17/min, blood pressure is 110/65 mm Hg, and temperature is 37.0°C (98.6°F). Physical examination reveals a visibly lethargic child with slight disorientation to time and place. Mild hepatosplenomegaly is observed but no signs of dehydration are noted. A blood sample is drawn, and fluids are started via an intravenous line.
Lab report
Serum glucose 44 mg/dL
Serum ketones absent
Serum creatinine 1.0 mg/dL
Blood urea nitrogen 32 mg/dL
Alanine aminotransferase (ALT) 425 U/L
Aspartate aminotransferase (AST) 372 U/L
Hemoglobin (Hb%) 12.5 g/dL
Mean corpuscular volume (MCV) 80 fl
Reticulocyte count 1%
Erythrocyte count 5.1 million/mm3
Which of the following is most likely deficient in this patient?
- A. Acyl-CoA dehydrogenase (Correct Answer)
- B. α-glucosidase
- C. Glucose-6-phosphatase
- D. Acetyl-CoA carboxylase
- E. Nicotinic acid
GSD type VI (Hers disease) Explanation: ***Acyl-CoA dehydrogenase***
- This patient presents with **hypoglycemia** (44 mg/dL) and **absent ketone bodies** after prolonged fasting, along with elevated **liver transaminases** and **hepatosplenomegaly**, which are classic signs of a **fatty acid oxidation disorder**.
- A deficiency in **acyl-CoA dehydrogenase**, particularly **medium-chain acyl-CoA dehydrogenase (MCAD)**, prevents adequate fatty acid breakdown for energy and ketone production, leading to **hypoketotic hypoglycemia** during periods of fasting.
*α-glucosidase*
- A deficiency in **α-glucosidase** (Pompe disease) leads to the accumulation of **glycogen** in lysosomes, primarily affecting muscles, heart, and liver.
- While it can cause hepatomegaly and muscle weakness, it typically presents with **cardiomyopathy** and does not directly cause hypoketotic hypoglycemia.
*Glucose-6-phosphatase*
- A deficiency in **glucose-6-phosphatase** (Von Gierke disease) is a type of **glycogen storage disease** characterized by severe **fasting hypoglycemia with lactic acidosis**, **massive hepatomegaly**, and **hyperlipidemia**.
- Unlike fatty acid oxidation disorders, Von Gierke disease typically presents with **lactic acidosis** as the predominant metabolic derangement, and patients often have a **doll-like face** and **growth retardation** from chronic presentation.
*Acetyl-CoA carboxylase*
- **Acetyl-CoA carboxylase** is a key enzyme in **fatty acid synthesis**, not fatty acid oxidation.
- A deficiency would primarily impair the body's ability to synthesize fatty acids, which is not consistent with the hypoketotic hypoglycemia observed here.
*Nicotinic acid*
- **Nicotinic acid** (niacin or vitamin B3) is a precursor to **NAD+** and **NADP+**, coenzymes involved in various metabolic reactions, including fatty acid synthesis and breakdown.
- While a deficiency (pellagra) can cause dermatitis, diarrhea, and dementia, it does not directly lead to **hypoketotic hypoglycemia** or fatty liver disease.
GSD type VI (Hers disease) US Medical PG Question 4: A 48-year-old homeless male presents to the ED because he hasn’t felt well recently. He states that he has been feeling nauseous and extremely weak over the past few days. He has several previous admissions for alcohol intoxication and uses heroin occasionally. His temperature is 100.9°F (38.3°C), blood pressure is 127/89 mmHg, and pulse is 101/min. His physical examination is notable for palmar erythema, tender hepatomegaly, and gynecomastia. His laboratory findings are notable for:
AST: 170 U/L
ALT: 60 U/L
GGT: 400 (normal range: 0-45 U/L)
Alkaline phosphatase: 150 IU/L
Direct bilirubin: 0.2 mg/dL
Total bilirubin: 0.8 mg/dL
WBC: 10,500
Serum iron: 100 µg/dL
TIBC: 300 µg/dL (normal range: 250–370 µg/dL)
Serum acetaminophen screen: Negative
Serum AFP: 6 ng/mL (normal range: < 10ng/mL)
Which of the following is the most likely cause of this patient’s symptoms?
- A. Acute viral hepatitis
- B. Acute cholangitis
- C. Hereditary hemochromatosis
- D. Hepatocellular carcinoma
- E. Alcoholic hepatitis (Correct Answer)
GSD type VI (Hers disease) Explanation: ***Alcoholic hepatitis***
- The patient's history of **heavy alcohol use**, along with symptoms such as **nausea**, **weakness**, **palmar erythema**, **tender hepatomegaly**, and **gynecomastia**, strongly points to alcoholic hepatitis.
- Laboratory findings of **AST:ALT ratio > 2:1** (170:60), **elevated GGT** (400 U/L), and **mildly elevated WBC** are characteristic of alcoholic liver injury.
*Acute viral hepatitis*
- While acute viral hepatitis can cause similar symptoms and elevated transaminases, the **AST:ALT ratio being significantly greater than 1** (specifically >2) is highly suggestive of alcoholic liver disease, whereas viral hepatitis typically shows ALT > AST.
- The elevated GGT is also more indicative of chronic alcohol use rather than acute viral infection.
*Acute cholangitis*
- Acute cholangitis typically presents with **Charcot's triad** (fever, right upper quadrant pain, jaundice) or **Reynolds' pentad** (Charcot's triad plus altered mental status and hypotension), along with **elevated alkaline phosphatase** and **direct bilirubin**.
- This patient's symptoms do not align with a classic presentation of cholangitis, and his direct bilirubin is normal.
*Hereditary hemochromatosis*
- Hereditary hemochromatosis is characterized by **iron overload**, which would manifest as **elevated serum iron** and **transferrin saturation**, along with a **decreased TIBC**.
- This patient's serum iron is normal, and his TIBC is within the normal range, ruling out iron overload as the primary cause.
*Hepatocellular carcinoma*
- HCC is a form of **liver cancer** that often develops in the setting of chronic liver disease (e.g., cirrhosis). While his history of alcohol use puts him at risk for cirrhosis, his **alpha-fetoprotein (AFP)** level is normal.
- The acute presentation with elevated transaminases and inflammatory markers is more consistent with acute hepatitis rather than carcinoma, which typically presents insidiously.
GSD type VI (Hers disease) US Medical PG Question 5: A 12-year-old girl comes to the clinic with a grossly enlarged abdomen. She has a history of frequent episodes of weakness, sweating, and pallor that are eliminated by eating. Her development has been slow. She started to walk unassisted at 2 years and was not performing well at school. Physical examination reveals a blood pressure of 100/60 mm Hg, heart rate of 80/min, and temperature of 36.9°C (98.4℉). On physical examination, the liver is enlarged, firm, and palpable up to the pelvis. The spleen and kidney are not palpable. Laboratory investigation reveals low blood glucose and pH with high lactate, triglycerides, ketones, and free fatty acids. The liver biopsy revealed high glycogen content. Hepatic glycogen structure was normal. The enzyme assay performed on the biopsy tissue revealed very low glucose-6-phosphatase levels. What is the most likely diagnosis?
- A. Pompe's disease
- B. Cori's disease
- C. Hereditary hemochromatosis
- D. Von-Gierke's disease (Correct Answer)
- E. McArdle disease
GSD type VI (Hers disease) Explanation: ***Von-Gierke's disease***
- The combination of **hepatomegaly**, **hypoglycemia** (causing weakness, sweating, pallor), **lactic acidosis**, **hyperlipidemia**, and elevated ketones points to a severe defect in glucose metabolism.
- **Very low glucose-6-phosphatase levels** on liver biopsy and normal hepatic glycogen structure are pathognomonic for Von-Gierke's disease (Glycogen Storage Disease Type I).
*Pompe's disease*
- This is a **lysosomal storage disease** affecting **alpha-1,4-glucosidase**, leading to glycogen accumulation in lysosomes.
- It primarily affects the **heart** and skeletal muscles and would not present with severe lactic acidosis and hyperlipidemia.
*Cori's disease*
- This is **Glycogen Storage Disease Type III**, caused by a deficiency in the **debranching enzyme** (amylo-alpha-1,6-glucosidase).
- While it can cause hepatomegaly and hypoglycemia, the hepatic glycogen structure would be abnormal due to incompletely debranched glycogen, and glucose-6-phosphatase levels would be normal.
*Hereditary hemochromatosis*
- This is an **iron overload disorder** leading to iron deposition in organs like the liver, heart, and pancreas.
- It would present with symptoms related to organ damage from iron accumulation, such as liver cirrhosis and diabetes, not the metabolic derangements seen here.
*McArdle disease*
- This is **Glycogen Storage Disease Type V**, due to a deficiency in **muscle glycogen phosphorylase**.
- It primarily causes exercise-induced muscle pain, cramping, and fatigue due to an inability to break down muscle glycogen for energy, not systemic metabolic disturbances or hepatomegaly.
GSD type VI (Hers disease) US Medical PG Question 6: A previously healthy 14-year-old girl is brought to the emergency department by her mother because of abdominal pain, nausea, and vomiting for 6 hours. Over the past 6 weeks, she has also had increased frequency of urination, and she has been drinking more water than usual. She has lost 6 kg (13 lb) over the same time period despite having a good appetite. Her temperature is 37.1°C (98.8°F), pulse is 125/min, respirations are 32/min, and blood pressure is 94/58 mm Hg. She appears lethargic. Physical examination shows deep and labored breathing and dry mucous membranes. The abdomen is soft, and there is diffuse tenderness to palpation with no guarding or rebound. Urine dipstick is positive for ketones and glucose. Further evaluation is most likely to show which of the following findings?
- A. Excess water retention
- B. Serum glucose concentration > 800 mg/dL
- C. Increased arterial pCO2
- D. Increased arterial blood pH
- E. Decreased total body potassium (Correct Answer)
GSD type VI (Hers disease) Explanation: ***Decreased total body potassium***
- This is the correct answer. In **diabetic ketoacidosis (DKA)**, patients have **significant total body potassium depletion** due to osmotic diuresis and urinary losses.
- **Serum potassium may initially appear normal or even elevated** due to acidosis-induced extracellular shift of potassium from cells.
- However, **total body potassium stores are markedly depleted**, and during treatment with insulin and fluids, severe hypokalemia can develop as potassium shifts back intracellularly.
*Excess water retention*
- The patient's symptoms, including **polydipsia**, **polyuria**, and **dry mucous membranes**, indicate **dehydration**, not excessive water retention.
- Her blood pressure of 94/58 mm Hg also suggests **volume depletion**.
*Serum glucose concentration > 800 mg/dL*
- While the patient has significant hyperglycemia (indicated by glucose in urine), **DKA** typically presents with glucose levels between **250-600 mg/dL**.
- Glucose levels >800 mg/dL are more characteristic of **hyperosmolar hyperglycemic state (HHS)**, which is less common in children and usually lacks significant ketosis.
*Increased arterial pCO2*
- The patient exhibits **Kussmaul respirations** (deep and labored breathing) and an increased respiratory rate (32/min), which are compensatory mechanisms for **metabolic acidosis**.
- This compensation leads to **decreased arterial pCO2** as the body tries to blow off CO2 to raise pH.
*Increased arterial blood pH*
- The symptoms, particularly **Kussmaul respirations** and the presence of **ketones** in the urine, strongly suggest **diabetic ketoacidosis (DKA)**.
- DKA is characterized by **severe metabolic acidosis**, meaning the arterial blood pH would be **decreased**, not increased.
GSD type VI (Hers disease) US Medical PG Question 7: A 9-month-old girl is brought to the physician because of a 1-month history of poor feeding and irritability. She is at the 15th percentile for height and 5th percentile for weight. Examination shows hypotonia and wasting of skeletal muscles. Cardiopulmonary examination shows no abnormalities. There is hepatomegaly. Her serum glucose is 61 mg/dL, creatinine kinase is 100 U/L, and lactic acid is within the reference range. Urine ketone bodies are elevated. Which of the following enzymes is most likely deficient in this patient?
- A. Glucose-6-phosphatase
- B. Muscle phosphorylase
- C. Acid alpha-glucosidase
- D. Glycogen debrancher (Correct Answer)
- E. Glucocerebrosidase
GSD type VI (Hers disease) Explanation: ***Glycogen debrancher***
- The patient's symptoms of **hepatomegaly**, **hypoglycemia**, **poor feeding**, **growth failure**, and **elevated urine ketones** in the presence of normal lactic acid suggest Type III glycogen storage disease (Cori disease), caused by a deficiency in **glycogen debrancher enzyme**.
- **Muscle wasting** and **hypotonia** are also consistent with Type III GSD, as the debranching enzyme is present in both liver and muscle.
*Glucose-6-phosphatase*
- Deficiency in **glucose-6-phosphatase** (Type I GSD, Von Gierke disease) also presents with **hepatomegaly** and **hypoglycemia**.
- However, Type I GSD is characterized by **lactic acidosis**, which is explicitly stated as normal in this patient, and **hyperlipidemia**, which is not mentioned.
*Muscle phosphorylase*
- Deficiency in **muscle phosphorylase** (Type V GSD, McArdle disease) primarily affects skeletal muscle, causing **exercise intolerance** and **muscle pain**.
- It does not typically present with **hypoglycemia**, **hepatomegaly**, or **growth failure** in infancy.
*Acid alpha-glucosidase*
- Deficiency in **acid alpha-glucosidase** (Type II GSD, Pompe disease) causes accumulation of glycogen in lysosomes, leading to severe **cardiomyopathy**, **hypotonia**, and **muscle weakness**.
- While hypotonia is present, the absence of **cardiomegaly** and significant **liver involvement** makes this diagnosis less likely.
*Glucocerebrosidase*
- Deficiency in **glucocerebrosidase** causes Gaucher disease, a lysosomal storage disorder, not a glycogen storage disorder.
- Symptoms include **hepatosplenomegaly**, **bone crises**, and neurological symptoms, but not **hypoglycemia** or isolated muscle wasting directly related to glycogen metabolism.
GSD type VI (Hers disease) US Medical PG Question 8: A 2-day-old newborn boy is brought to the emergency department because of apnea, cyanosis, and seizures. He is severely hypoglycemic and does not improve with glucagon administration. His blood pressure is 100/62 mm Hg and heart rate is 75/min. Blood tests show high lactate levels. Physical examination is notable for hepatomegaly. Which of the following enzymes is most likely to be deficient in this baby?
- A. α-ketoacid dehydrogenase
- B. Phenylalanine hydroxylase
- C. Glucose-6-phosphatase (Correct Answer)
- D. Glucocerebrosidase
- E. Sphingomyelinase
GSD type VI (Hers disease) Explanation: ***Correct: Glucose-6-phosphatase***
- The presentation of severe **hypoglycemia** not responsive to glucagon, coupled with **hepatomegaly** and **lactic acidosis** in a neonate, is highly suggestive of **Type I glycogen storage disease (von Gierke disease)**.
- Deficiency of **glucose-6-phosphatase** prevents the liver from releasing glucose into the bloodstream (the final step of both gluconeogenesis and glycogenolysis), leading to profound hypoglycemia.
- **Key diagnostic clue**: Lack of response to glucagon occurs because glucagon stimulates glycogenolysis, but without functional glucose-6-phosphatase, glucose-6-phosphate cannot be converted to free glucose for release.
- Accumulated glucose-6-phosphate shunts to glycolysis, producing **lactate** (lactic acidosis), and to glycogen synthesis, causing **hepatomegaly**.
*Incorrect: α-ketoacid dehydrogenase*
- Deficiency of **branched-chain α-ketoacid dehydrogenase** causes **maple syrup urine disease (MSUD)**, which presents with poor feeding, vomiting, lethargy, and a characteristic maple syrup odor in urine.
- While MSUD can cause neurological symptoms and seizures, **severe hypoglycemia unresponsive to glucagon** and **hepatomegaly** as primary features are not typical.
*Incorrect: Phenylalanine hydroxylase*
- Deficiency in **phenylalanine hydroxylase** causes **phenylketonuria (PKU)**, which is primarily characterized by intellectual disability, seizures (if untreated), and a musty odor, usually manifesting later in infancy.
- PKU does not present with acute neonatal hypoglycemia, lactic acidosis, or hepatomegaly.
*Incorrect: Glucocerebrosidase*
- Deficiency in **glucocerebrosidase** leads to **Gaucher disease**, a lysosomal storage disorder characterized by hepatosplenomegaly, bone crises, and neurological symptoms in severe infantile forms.
- While hepatomegaly may be present, Gaucher disease does not cause acute, severe neonatal hypoglycemia, lactic acidosis, or lack of response to glucagon.
*Incorrect: Sphingomyelinase*
- Deficiency in **sphingomyelinase** causes **Niemann-Pick disease**, another lysosomal storage disorder, which typically presents with hepatosplenomegaly, neurological deterioration, and "cherry-red spots" in the retina.
- This condition does not cause acute neonatal hypoglycemia, lactic acidosis, or glucagon unresponsiveness.
GSD type VI (Hers disease) US Medical PG Question 9: A 2-month-old boy is brought to the emergency department 25 minutes after having a seizure. He has had multiple seizures during the past week. His mother has noticed that he has become lethargic and has had a weak cry for the past month. He was born at 37 weeks' gestation. He is at the 20th percentile for height and 15th percentile for weight. His temperature is 36.7°C (98°F), respirations are 50/min, and pulse is 140/min. Examination shows a soft and nontender abdomen. The liver is palpated 4 cm below the right costal margin; there is no splenomegaly. Serum studies show:
Na+ 137 mEq/L
Cl- 103 mEq/L
K+ 3.9 mEq/L
Glucose 32 mg/dL
Calcium 9.6 mg/dL
Total cholesterol 202 mg/dL
Triglycerides 260 mg/dL
Lactate 4.2 mEq/L (N = 0.5 - 2.2 mEq/L)
A deficiency of which of the following enzymes is the most likely cause of this infant's symptoms?
- A. Galactose 1-phosphate uridyltransferase
- B. Glycogen branching enzyme
- C. Glucose 6-phosphatase (Correct Answer)
- D. Fructokinase
- E. Acid maltase
GSD type VI (Hers disease) Explanation: ***Glucose 6-phosphatase***
- The constellation of **hypoglycemia**, **lactic acidosis**, **hepatomegaly**, and **hyperlipidemia** in an infant is characteristic of **Type I glycogen storage disease (von Gierke's disease)**, which is caused by a deficiency of glucose 6-phosphatase.
- Seizures and lethargy are common manifestations of severe hypoglycemia in infants.
*Galactose 1-phosphate uridyltransferase*
- Deficiency of this enzyme causes **classic galactosemia**, which typically presents with **jaundice**, **cataracts**, **vomiting**, and **failure to thrive**, usually after initiation of milk feeds.
- While patients can develop hepatomegaly and hypoglycemia, the prominent lactic acidosis and hyperlipidemia seen here are less typical.
*Glycogen branching enzyme*
- Deficiency causes **Type IV glycogen storage disease (Andersen's disease)**, characterized by **hepatosplenomegaly**, **failure to thrive**, and progressive cirrhosis.
- Hypoglycemia is generally less severe, and lactic acidosis and hyperlipidemia are not primary features in the same way as Type I GSD.
*Fructokinase*
- Deficiency causes **essential fructosuria**, a benign condition where fructose accumulates in the urine.
- It is typically asymptomatic and does not lead to hypoglycemia, lactic acidosis, or hepatomegaly.
*Acid maltase*
- Deficiency (alpha-1,4-glucosidase) causes **Type II glycogen storage disease (Pompe's disease)**, which primarily affects skeletal and cardiac muscle.
- The infantile form presents with **severe hypotonia** ("floppy baby"), **cardiomyopathy**, and **macroglossia**. Hepatomegaly, hypoglycemia, and lactic acidosis are not prominent features.
GSD type VI (Hers disease) US Medical PG Question 10: A 5-month-old boy presents with increasing weakness for the past 3 months. The patient’s mother says that the weakness is accompanied by dizziness, sweating, and vertigo early in the morning. Physical examination shows hepatomegaly. Laboratory findings show an increased amount of lactate, uric acid, and elevated triglyceride levels. Which of the following enzymes is most likely deficient in this patient?
- A. Hepatic glycogen phosphorylase
- B. Debranching enzyme
- C. Glucose-6-phosphatase (Correct Answer)
- D. Muscle glycogen phosphorylase
- E. Lysosomal α-1,4-glucosidase
GSD type VI (Hers disease) Explanation: ***Glucose-6-phosphatase***
- The constellation of **hypoglycemia** (weakness, dizziness, sweating, vertigo, especially early morning), **hepatomegaly**, **lactic acidosis**, **hyperuricemia**, and **hypertriglyceridemia** are classic features of **Type I glycogen storage disease (von Gierke disease)**, which is caused by a deficiency of **glucose-6-phosphatase**.
- This enzyme is crucial for the final step of both **glycogenolysis** and **gluconeogenesis**, releasing free glucose into the bloodstream; its deficiency leads to an inability to maintain normal blood glucose levels during fasting and accumulation of glucose-6-phosphate, which shunts into other metabolic pathways.
*Hepatic glycogen phosphorylase*
- Deficiency in **hepatic glycogen phosphorylase** (Type VI glycogen storage disease, Hers disease) would cause **hepatomegaly** and **hypoglycemia**, but typically does not present with severe **lactic acidosis**, **hyperuricemia**, or **hypertriglyceridemia** to the same degree as von Gierke disease.
- The primary defect is in breaking down glycogen, leading to its accumulation in the liver, but the products of glycolysis can still exit the liver via gluconeogenesis.
*Debranching enzyme*
- Deficiency in **debranching enzyme** (Type III glycogen storage disease, Cori or Forbes disease) causes **hepatomegaly** and **hypoglycemia**, but usually presents with milder symptoms and less severe **lactic acidosis**, **hyperuricemia**, and **hypertriglyceridemia**.
- Patients often present with symptoms similar to Type I, but muscle involvement is also common, and **glycogen structures with short outer branches** are characteristic.
*Muscle glycogen phosphorylase*
- Deficiency in **muscle glycogen phosphorylase** (Type V glycogen storage disease, McArdle disease) primarily affects **skeletal muscle**, leading to exercise intolerance, muscle pain, and myoglobinuria.
- It does not typically cause **hypoglycemia** or **hepatomegaly**, as the liver enzyme is functional, and the symptoms described are systemic rather than muscle-specific.
*Lysosomal α-1,4-glucosidase*
- Deficiency in **lysosomal α-1,4-glucosidase** (Type II glycogen storage disease, Pompe disease) primarily affects the **heart, muscle, and liver**, causing severe **cardiomyopathy**, hypotonia, and **hepatomegaly**.
- While it involves glycogen accumulation, it typically does not present with **hypoglycemia** (as cytoplasmic glycogen metabolism is intact), **lactic acidosis**, or the specific metabolic derangements seen in this patient.
More GSD type VI (Hers disease) US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.