GSD type V (McArdle disease) US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for GSD type V (McArdle disease). These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
GSD type V (McArdle disease) US Medical PG Question 1: A 6-month-old girl is brought to the emergency department by her father after he observed jerking movements of her arms and legs earlier in the day. She appears lethargic. Physical examination shows generalized hypotonia. The liver edge is palpable 3 cm below the right costophrenic angle. Her fingerstick glucose shows hypoglycemia. Serum levels of acetone, acetoacetate, and β-hydroxybutyrate are undetectable. Molecular genetic testing shows a mutation in the carnitine palmitoyltransferase II gene. This patient will most likely benefit from supplementation with which of the following?
- A. Thiamine
- B. Coenzyme A
- C. Methionine
- D. Tetrahydrobiopterin
- E. Medium-chain triglycerides (Correct Answer)
GSD type V (McArdle disease) Explanation: ***Medium-chain triglycerides***
- This patient presents with symptoms consistent with a **fatty acid oxidation disorder** (lethargy, hypotonia, hepatomegaly, hypoglycemia, and undetectable ketones in the setting of hypoglycemia). A **carnitine palmitoyltransferase II (CPT II) deficiency** is a specific fatty acid oxidation disorder.
- **Medium-chain triglycerides (MCTs)** can be directly used for energy in the mitochondria without requiring the carnitine shuttle system, bypassing the defective CPT II enzyme and providing an alternative energy source.
*Thiamine*
- **Thiamine (vitamin B1)** is a coenzyme important for carbohydrate metabolism (e.g., pyruvate dehydrogenase, alpha-ketoglutarate dehydrogenase) and can be deficient in conditions like Wernicke-Korsakoff syndrome.
- It is not directly involved in fatty acid oxidation or carnitine palmitoyltransferase II function.
*Coenzyme A*
- **Coenzyme A (CoA)** is a crucial cofactor in many metabolic pathways, including fatty acid oxidation, but its deficiency is not the primary issue in CPT II deficiency.
- Supplementation with CoA would not address the specific defect in the carnitine shuttle system, which prevents long-chain fatty acids from entering the mitochondria.
*Methionine*
- **Methionine** is an essential amino acid involved in protein synthesis and as a precursor for other molecules like S-adenosylmethionine (SAM).
- It is not directly involved in fatty acid oxidation or CPT II function, and its supplementation would not alleviate the metabolic crisis caused by CPT II deficiency.
*Tetrahydrobiopterin*
- **Tetrahydrobiopterin (BH4)** is a cofactor for several enzymes, including phenylalanine hydroxylase (deficient in PKU) and tyrosine hydroxylase.
- It is not involved in fatty acid metabolism, and its deficiency would not explain the symptoms or the underlying genetic defect in CPT II.
GSD type V (McArdle disease) US Medical PG Question 2: A 12-year-old male presents to the pediatrician after two days of tea-colored urine which appeared to coincide with the first day of junior high football. He explains that he refused to go back to practice because he was humiliated by the other players due to his quick and excessive fatigue after a set of drills accompanied by pain in his muscles. A blood test revealed elevated creatine kinase and myoglobulin levels. A muscle biopsy was performed revealing large glycogen deposits and an enzyme histochemistry showed a lack of myophosphorylase activity. Which of the following reactions is not occurring in this individual?
- A. Cleaving alpha-1,6 glycosidic bonds from glycogen
- B. Creating alpha-1,6 glycosidic bonds in glycogen
- C. Breaking down glycogen to glucose-1-phosphate (Correct Answer)
- D. Converting glucose-6-phosphate to glucose
- E. Converting galactose to galactose-1-phosphate
GSD type V (McArdle disease) Explanation: ***Breaking down glycogen to glucose-1-phosphate***
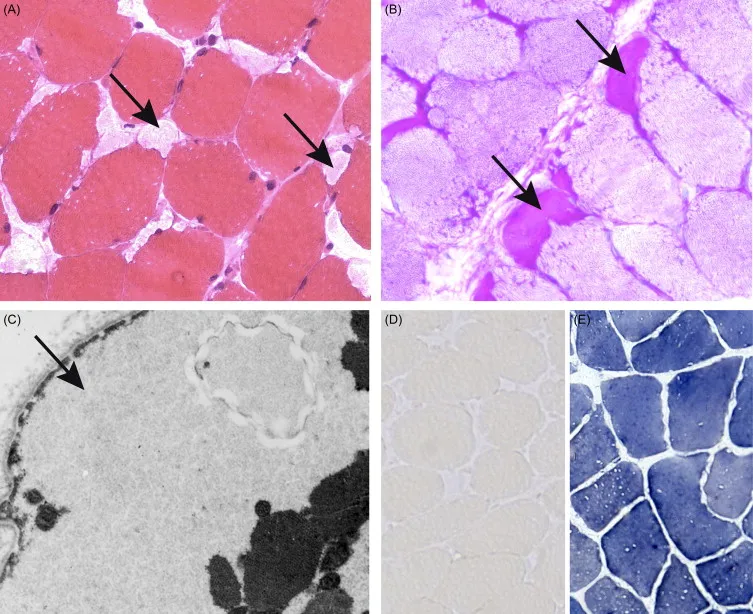
- The patient's symptoms (muscle pain, quick fatigue during exercise, tea-colored urine indicating **rhabdomyolysis**) and laboratory findings (**elevated creatine kinase and myoglobin**, **large glycogen deposits** in muscle, and **lack of myophosphorylase activity**) are classic for **McArdle disease (Glycogen Storage Disease Type V).**
- **Myophosphorylase** (also known as **glycogen phosphorylase**) is the enzyme responsible for breaking down glycogen into **glucose-1-phosphate** in muscle, so this reaction is severely impaired.
*Cleaving alpha-1,6 glycosidic bonds from glycogen*
- This reaction is catalyzed by the **debranching enzyme** (specifically, its **oligo-1,6-glucosidase** activity), not myophosphorylase.
- The debranching enzyme is crucial for completely breaking down glycogen, but its deficiency would lead to different clinical and histopathological findings (e.g., accumulation of **dextrin-like structures**).
*Creating alpha-1,6 glycosidic bonds in glycogen*
- This is the function of the **branching enzyme**, which introduces branches into the glycogen structure.
- This process is part of **glycogen synthesis**, not degradation, and is not directly affected by myophosphorylase deficiency.
*Converting glucose-6-phosphate to glucose*
- This reaction primarily occurs in the liver and kidneys, catalyzed by **glucose-6-phosphatase**, to release glucose into the bloodstream.
- While muscle cells can produce glucose-6-phosphate from glycogen, they lack glucose-6-phosphatase, so they cannot release free glucose into the blood. This reaction is irrelevant to the primary defect here.
*Converting galactose to galactose-1-phosphate*
- This is an initial step in **galactose metabolism**, catalyzed by **galactokinase**.
- This metabolic pathway is entirely separate from glycogen metabolism and is not implicated in McArdle disease.
GSD type V (McArdle disease) US Medical PG Question 3: A 48-year-old woman comes to the physician because of a 6-month history of muscle stiffness, myalgia, and a 7-kg (15-lb) weight gain. Her last menstrual period was 4 months ago. Physical examination shows cold, dry skin, and proximal muscle weakness. Deep tendon reflexes are 2+ bilaterally, with delayed relaxation. The creatine kinase level is 2,940 U/L. Which of the following is the most appropriate next step in diagnosis?
- A. Thyroid function tests (Correct Answer)
- B. Repetitive nerve stimulation
- C. Serum electrolytes
- D. Muscle biopsy
- E. Serum assay for muscle specific tyrosine kinase antibody
GSD type V (McArdle disease) Explanation: ***Thyroid function tests***
- The patient's symptoms (muscle stiffness, myalgia, weight gain, cold/dry skin, proximal muscle weakness, delayed deep tendon reflex relaxation, and elevated CK) are highly suggestive of **hypothyroidism**.
- Measuring **TSH** and **free T4** is crucial to confirm or rule out this diagnosis and it is the most appropriate next step in the diagnostic workup.
*Repetitive nerve stimulation*
- This test is primarily used to diagnose disorders of the **neuromuscular junction**, such as **myasthenia gravis** or **Lambert-Eaton syndrome**.
- The patient's clinical picture, particularly the delayed deep tendon reflex relaxation and muscle stiffness, is not typical for these conditions.
*Serum electrolytes*
- While electrolytes can be abnormal in various conditions, they are unlikely to directly explain the constellation of symptoms (muscle stiffness, weight gain, cold/dry skin, delayed reflexes) and the high **creatine kinase** level in this patient.
- While a basic metabolic panel is often part of a general workup, it is not the most specific or appropriate *next step* for this clinical presentation.
*Muscle biopsy*
- A muscle biopsy is an **invasive procedure** typically reserved for diagnosing specific **myopathies** (e.g., inflammatory myopathies, muscular dystrophies) when less invasive tests have not yielded a diagnosis.
- Given the strong indicators for hypothyroidism, a muscle biopsy would be premature before evaluating thyroid function.
*Serum assay for muscle specific tyrosine kinase antibody*
- This antibody is a marker for a subtype of **myasthenia gravis** (**MuSK-associated myasthenia gravis**), a disorder of the neuromuscular junction.
- As with repetitive nerve stimulation, the patient's symptoms, especially the delayed deep tendon reflexes and myxedema-like features, do not primarily point towards myasthenia gravis.
GSD type V (McArdle disease) US Medical PG Question 4: A 25-year-old man comes to the physician for severe back pain. He describes the pain as shooting and stabbing. On a 10-point scale, he rates the pain as a 9 to 10. The pain started after he lifted a heavy box at work; he works at a supermarket and recently switched from being a cashier to a storekeeper. The patient appears to be in severe distress. Vital signs are within normal limits. On physical examination, the spine is nontender without paravertebral muscle spasms. Range of motion is normal. A straight-leg raise test is negative. After the physical examination has been completed, the patient asks for a letter to his employer attesting to his inability to work as a storekeeper. Which of the following is the most appropriate response?
- A. “Yes. Since work may worsen your condition, I would prefer that you stay home a few days. I will write a letter to your employer to explain the situation.”
- B. You say you are in severe pain. However, the physical examination findings do not suggest a physical problem that can be addressed with medications or surgery. I'd like to meet on a regular basis to see how you're doing.
- C. I understand that you are uncomfortable, but the findings do not match the severity of your symptoms. Let's talk about the recent changes at your job. (Correct Answer)
- D. The physical exam findings do not match your symptoms, which suggests a psychological problem. I would be happy to refer you to a mental health professional.
- E. The physical exam findings suggest a psychological rather than a physical problem. But there is a good chance that we can address it with cognitive-behavioral therapy.
GSD type V (McArdle disease) Explanation: ***"I understand that you are uncomfortable, but the findings do not match the severity of your symptoms. Let's talk about the recent changes at your job."***
- This response acknowledges the patient's reported discomfort while gently highlighting the **discrepancy between symptoms and objective findings**, which is crucial in cases of suspected **somatoform or functional pain**.
- It also opens communication about potential **psychosocial stressors** related to his job change, which could be contributing to his symptoms, without dismissing his pain or making a premature diagnosis.
*"You say you are in severe pain. However, the physical examination findings do not suggest a physical problem that can be addressed with medications or surgery. I'd like to meet on a regular basis to see how you're doing."*
- While this option correctly identifies the lack of physical findings, it can be perceived as dismissive of the patient's pain, potentially damaging the **physician-patient relationship**.
- Suggesting regular meetings without a clear plan for addressing his immediate concerns or exploring underlying issues might not be the most effective initial approach.
*“Yes. Since work may worsen your condition, I would prefer that you stay home a few days. I will write a letter to your employer to explain the situation.”*
- This response would **validate the patient's claim of severe pain** without objective evidence, potentially reinforcing illness behavior and avoiding addressing the underlying issue.
- Providing a doctor's note for inability to work without a clear diagnostic basis or understanding of the pain's origin is **medically inappropriate** and could set a precedent for future such requests.
*"The physical exam findings do not match your symptoms, which suggests a psychological problem. I would be happy to refer you to a mental health professional."*
- Directly labeling the problem as "psychological" can be **stigmatizing and alienating** to the patient, leading to distrust and resistance to care.
- While a psychological component might be present, immediately referring to mental health without further exploration of the patient's situation or current stressors is premature and lacks empathy.
*"The physical exam findings suggest a psychological rather than a physical problem. But there is a good chance that we can address it with cognitive-behavioral therapy."*
- Similar to the previous option, explicitly stating a "psychological problem" can be **stigmatizing**.
- Jumping directly to recommending **cognitive-behavioral therapy (CBT)** without a comprehensive discussion and patient buy-in is premature and may lead to non-compliance.
GSD type V (McArdle disease) US Medical PG Question 5: A 5-year-old boy presents to the pediatrician after his parents noted that he could not sustain physical exertion and would experience muscle cramping. It was noted that after physical exertion the boy experienced severe muscle pain. After a series of biochemical and genetic tests, it was discovered that the boy had a nonsense mutation in the gene encoding the muscle glycogen phosphorylase. Thus he was diagnosed with McArdle's disease. Which of the following mRNA changes would be expected to cause this mutation?
- A. UGU -> CGC
- B. CUG -> AUG
- C. UAU -> UAA (Correct Answer)
- D. UGA -> UAG
- E. AUG -> UCA
GSD type V (McArdle disease) Explanation: ***UAU -> UAA***
- A **nonsense mutation** results in a prematurely truncated protein due to the introduction of a **stop codon** where a coding codon previously existed.
- Changing UAU (tyrosine) to UAA creates a **stop codon**, leading to premature termination and a dysfunctional muscle glycogen phosphorylase, consistent with **McArdle's disease**.
*UGU -> CGC*
- This change from UGU (cysteine) to CGC (arginine) is a **missense mutation**, where one amino acid is substituted for another.
- While it could potentially affect protein function, it does not introduce a **stop codon** and therefore is not a nonsense mutation.
*CUG -> AUG*
- This change from CUG (leucine) to AUG (methionine) is a **missense mutation**.
- Although AUG functions as a start codon at the beginning of mRNA, within the coding sequence it simply codes for methionine.
- This does not create a **stop codon** and therefore is not a nonsense mutation.
*UGA -> UAG*
- Both UGA and UAG are **stop codons** (UGA = opal, UAG = amber).
- Since both codons already terminate translation, this change would not create a **new** nonsense mutation in a coding sequence.
- A nonsense mutation requires changing a **coding codon** to a **stop codon**.
*AUG -> UCA*
- This change from AUG (methionine) to UCA (serine) is a **missense mutation**.
- It results in the substitution of one amino acid for another, rather than the creation of a **stop codon**.
GSD type V (McArdle disease) US Medical PG Question 6: A 13-year-old boy is brought to the physician by his parents, who are concerned about recurrent muscle cramps he experiences while playing soccer. The boy has always loved sports and has been playing in a soccer league for the past 3 years. He now complains of severe cramping pain in his legs after intense practice sessions. He has no significant medical history. His physical examination is unremarkable. A battery of laboratory tests is ordered and they are all normal. Imaging studies yield no abnormalities as well. Which of the following is most likely deficient in this patient?
- A. Carnitine palmitoyltransferase I
- B. Medium-chain acyl-coenzyme A dehydrogenase
- C. Carnitine palmitoyltransferase II
- D. Phosphofructokinase
- E. Myophosphorylase (Correct Answer)
GSD type V (McArdle disease) Explanation: ***Myophosphorylase***
- The patient's symptoms of **exercise-induced muscle cramps** and pain, specifically after intense activity, and normal lab findings, are classic for **McArdle disease** (glycogen storage disease type V).
- McArdle disease is caused by a deficiency in **myophosphorylase**, preventing the breakdown of glycogen for energy in muscles during exercise.
*Carnitine palmitoyltransferase I*
- Deficiency in CPT I primarily affects the liver and causes a hypoketotic hypoglycemia, not isolated exercise-induced muscle cramps.
- This enzyme is crucial for the transport of long-chain fatty acids into the mitochondria for beta-oxidation.
*Medium-chain acyl-coenzyme A dehydrogenase*
- MCAD deficiency is characterized by **hypoketotic hypoglycemia** and liver dysfunction, especially during fasting or illness, due to impaired fatty acid oxidation.
- It does not typically present with isolated exercise-induced muscle cramps in an otherwise healthy active adolescent.
*Carnitine palmitoyltransferase II*
- CPT II deficiency can cause **recurrent myoglobinuria** and acute muscle pain precipitated by prolonged exercise, fasting, or cold exposure, which might resemble the patient's symptoms.
- However, the presentation of "severe cramping pain in his legs after intense practice sessions" with normal lab tests points more directly to an issue with carbohydrate metabolism in muscle, making myophosphorylase deficiency a more likely primary diagnosis given the typical onset with intense, high-energy demand activities rather than prolonged exercise or fasting.
*Phosphofructokinase*
- PFK deficiency (Tarui disease) also presents with exercise intolerance, muscle pain, and cramps, and is a type of glycogen storage disease.
- It would typically result in **hemolytic anemia** and elevated bilirubin, which are not mentioned in this patient, and would also lead to an accumulation of glycolytic intermediates, which is not indicated by the normal lab results.
GSD type V (McArdle disease) US Medical PG Question 7: A 7-year-old boy is brought to his pediatrician by his mother who is worried about his clumsiness. She states that over the past 3 months she has noticed progressive weakness. He used to climb trees and run outside with his cousins, but now he says he gets “too tired.” She’s recently noticed him starting to “walk funny,” despite having “muscular legs.” Upon physical examination, the patient has calf muscle hypertrophy. He uses his arms to rise out of the chair. Labs are obtained that show an elevated creatine kinase. Genetic analysis detects a dystropin gene mutation. A muscle biopsy is performed that reveals reduced dystrophin. Which of the following is the most likely diagnosis?
- A. Fragile X syndrome
- B. Pompe disease
- C. Duchenne muscular dystrophy (Correct Answer)
- D. Spinal muscular atrophy
- E. Becker muscular dystrophy
GSD type V (McArdle disease) Explanation: ***Duchenne muscular dystrophy***
- This 7-year-old presents with classic features of **Duchenne muscular dystrophy (DMD)**: **progressive proximal muscle weakness**, **calf pseudohypertrophy**, **Gowers' sign** (using arms to rise from a chair), and **markedly elevated creatine kinase**.
- Genetic analysis confirms a **dystrophin gene mutation**, and muscle biopsy shows **reduced dystrophin**, consistent with DMD where dystrophin is absent or severely reduced (<3% of normal).
- The **age of presentation (7 years)** is typical for DMD, as many boys are diagnosed between ages 3-7 when motor delays become apparent in school settings; the recent 3-month history of rapid decline is characteristic of DMD's progressive course.
- Boys with DMD typically lose ambulation by age 12 and require wheelchair assistance, distinguishing it from the milder Becker variant.
*Becker muscular dystrophy*
- While also caused by a **dystrophin gene mutation**, Becker muscular dystrophy (BMD) presents **later** (typically age 8-25) with a **much milder and slower progression**.
- In BMD, dystrophin is **reduced but functional** (3-20% or more of normal, often abnormal in size), not severely deficient as in this case.
- Patients with BMD remain ambulatory into their 20s-30s or beyond, which contrasts with this patient's relatively early onset and rapid 3-month decline.
- The clinical tempo and age of onset in this case are more consistent with Duchenne than Becker.
*Fragile X syndrome*
- This is a genetic disorder primarily characterized by **intellectual disability**, **developmental delays**, **autism spectrum features**, and distinct physical features (long face, large ears, macroorchidism).
- It does not present with **progressive muscle weakness**, **calf pseudohypertrophy**, **elevated CK**, or **dystrophin gene mutations**.
*Pompe disease*
- This is a **lysosomal storage disorder** caused by deficiency of **acid alpha-glucosidase (GAA)**, leading to glycogen accumulation in lysosomes.
- While it can cause **muscle weakness** and elevated CK, infantile-onset Pompe presents with **cardiomyopathy** and **hypotonia** ("floppy infant"), and late-onset Pompe presents with limb-girdle weakness and respiratory failure.
- Pompe does **not involve dystrophin mutations** or **calf pseudohypertrophy**.
*Spinal muscular atrophy*
- This disorder results from **loss of motor neurons** in the spinal cord due to **SMN1 gene mutations**, causing muscle weakness and atrophy.
- SMA presents with **hypotonia**, **areflexia**, and **muscle atrophy** (not hypertrophy), with **fasciculations** of the tongue in some cases.
- It does **not involve dystrophin mutations**, **calf pseudohypertrophy**, or markedly elevated CK levels.
GSD type V (McArdle disease) US Medical PG Question 8: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
GSD type V (McArdle disease) Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
GSD type V (McArdle disease) US Medical PG Question 9: A 15-year-old boy comes to the physician because of severe muscle cramps and pain for 3 months. He first noticed these symptoms while attending tryouts for the high school football team. Since then, he becomes easily fatigued and has severe muscle pain and swelling after 10 minutes of playing. However, after a brief period of rest, the symptoms improve, and he is able to return to the game. Two days ago, he had an episode of reddish-brown urine after playing football. There is no family history of serious illness. He appears healthy. Vital signs are within normal limits. Physical and neurological examinations show no abnormalities. Serum creatine kinase concentration is 333 U/L. Urinalysis shows:
Blood 2+
Protein negative
Glucose negative
RBC negative
WBC 1–2/hpf
Which of the following is the most likely cause of this patient's symptoms?
- A. CTG repeat in the DMPK gene
- B. Myophosphorylase deficiency (Correct Answer)
- C. Dystrophin gene mutation
- D. Thyroid hormone deficiency
- E. Acid maltase deficiency
GSD type V (McArdle disease) Explanation: ***Myophosphorylase deficiency***
- This condition (also known as **McArdle disease**) presents with **exercise-induced muscle cramps, pain, and fatigue** immediately after initiating activity, with a "second wind" phenomenon where symptoms improve after resting.
- The elevated **creatine kinase** and **reddish-brown urine** (indicating **myoglobinuria** due to rhabdomyolysis) are classic findings after strenuous activity in this glycogen storage disorder.
*CTG repeat in the DMPK gene*
- This describes **myotonic dystrophy type 1**, which presents with **myotonia** (delayed muscle relaxation), muscle weakness, and often involves multiple organ systems.
- While it causes muscle weakness, it does not typically present with acute, exercise-induced pain, cramping, and rhabdomyolysis in this manner.
*Dystrophin gene mutation*
- This is characteristic of **Duchenne or Becker muscular dystrophy**, which are progressive muscle weakness disorders.
- They typically cause **progressive proximal muscle weakness** and atrophy, not acute, intermittent, exercise-induced pain and cramping with a "second wind" phenomenon.
*Thyroid hormone deficiency*
- **Hypothyroidism** can cause muscle cramps, weakness, and elevated creatine kinase, but these symptoms are usually chronic and progressive, not acutely exercise-induced with improvement after a short rest.
- It would also present with other systemic symptoms like fatigue, weight gain, and cold intolerance, which are not described.
*Acid maltase deficiency*
- Also known as **Pompe disease**, this is a glycogen storage disorder that primarily affects infants and can present in adults with **proximal muscle weakness**, respiratory insufficiency, and cardiac involvement.
- It does not typically present with acute, exercise-induced muscle cramps, pain, and rhabdomyolysis followed by a "second wind" phenomenon like McArdle disease.
GSD type V (McArdle disease) US Medical PG Question 10: A 16-year-old boy comes to the physician because of muscle weakness and cramps for 5 months. He becomes easily fatigued and has severe muscle pain and swelling after 15 minutes of playing basketball with his friends. The symptoms improve after a brief period of rest. After playing, he sometimes also has episodes of reddish-brown urine. There is no family history of serious illness. Serum creatine kinase concentration is 950 U/L. Urinalysis shows:
Blood 2+
Protein negative
Glucose negative
RBC negative
WBC 1–2/hpf
Which of the following is the most likely underlying cause of this patient's symptoms?
- A. Medium-chain acyl-CoA dehydrogenase deficiency
- B. Myophosphorylase deficiency (Correct Answer)
- C. Low levels of triiodothyronine and thyroxine
- D. Acid maltase deficiency
- E. CTG repeat in the DMPK gene
GSD type V (McArdle disease) Explanation: ***Myophosphorylase deficiency***
- This condition (McArdle disease) is an **autosomal recessive disorder** of glycogen metabolism characterized by a defect in **glycogenolysis**, specifically the breakdown of muscle glycogen. This leads to impaired energy production during exercise.
- The classic presentation includes **exercise-induced muscle pain, stiffness, cramps, fatigue**, and sometimes **myoglobinuria** (reddish-brown urine due to myoglobin release from damaged muscle), which is consistent with the patient's symptoms and elevated **creatine kinase**.
*Medium-chain acyl-CoA dehydrogenase deficiency*
- This is a disorder of **fatty acid oxidation** that primarily affects the liver, leading to episodes of **hypoketotic hypoglycemia** during fasting or illness.
- It does not typically present with isolated exercise-induced muscle pain and myoglobinuria.
*Low levels of triiodothyronine and thyroxine*
- **Hypothyroidism** can cause generalized muscle weakness, fatigue, and muscle cramps, but it is usually associated with other systemic symptoms like weight gain, cold intolerance, and constipation.
- While it can cause elevated CK, it generally does not present with acute, exercise-induced muscle pain and myoglobinuria in the manner described.
*Acid maltase deficiency*
- This (Pompe disease) is a lysosomal storage disorder affecting glycogen metabolism, but it results from a deficiency of **acid alpha-glucosidase (acid maltase)**.
- The infantile form presents with severe hypotonia and cardiomyopathy, while the juvenile and adult forms typically cause **proximal muscle weakness** and respiratory insufficiency, rather than exercise-induced muscle pain and myoglobinuria.
*CTG repeat in the DMPK gene*
- This genetic defect is associated with **myotonic dystrophy type 1 (Steinert disease)**, an autosomal dominant disorder.
- Key features include **myotonia** (delayed relaxation of muscles), muscle weakness, cataracts, and cardiac conduction abnormalities, which are distinct from the patient's presentation of exercise-induced cramps and myoglobinuria without myotonia.
More GSD type V (McArdle disease) US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.