GSD type II (Pompe disease) US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for GSD type II (Pompe disease). These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
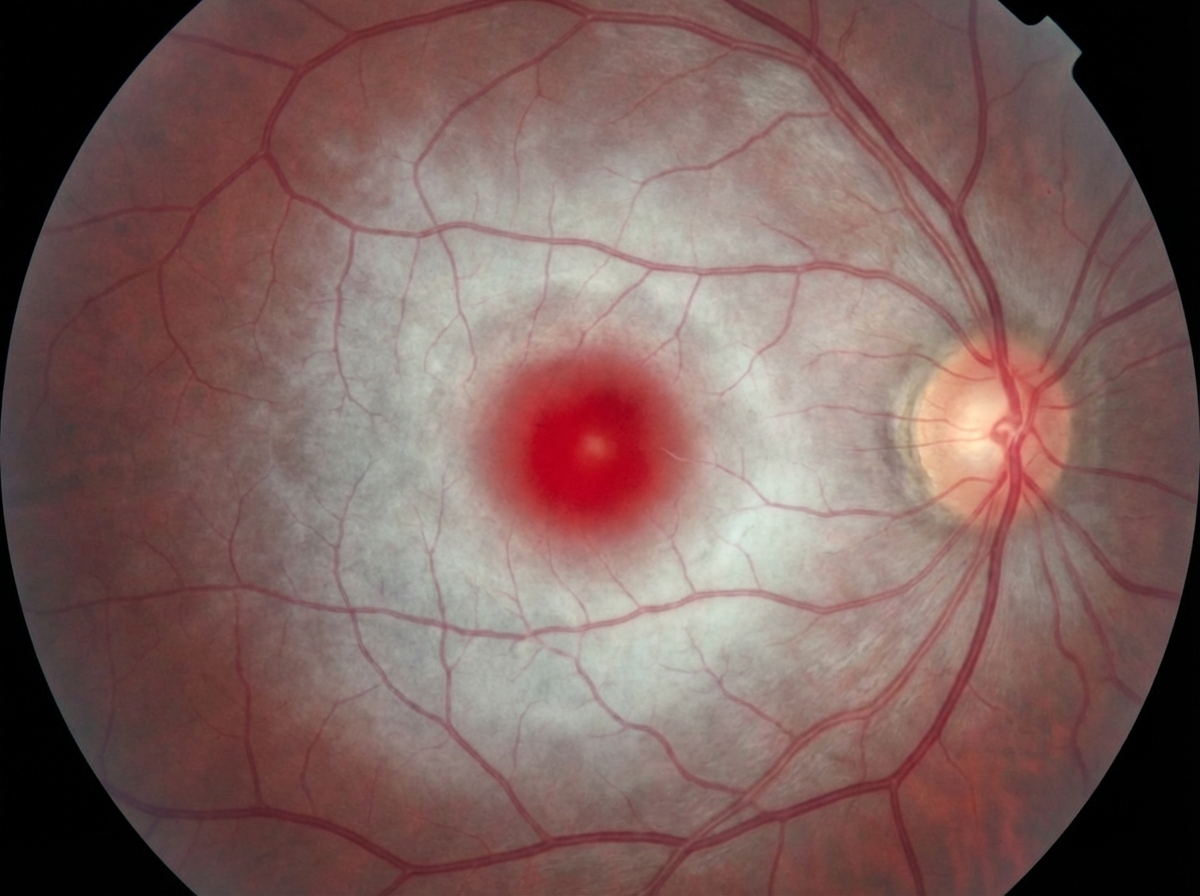
GSD type II (Pompe disease) US Medical PG Question 1: A 7-month-old boy is brought by his parents to the pediatrician’s office. His mother says the child has been weakening progressively and is not as active as he used to be when he was born. His condition seems to be getting worse, especially over the last month. He was born at 41 weeks through normal vaginal delivery. There were no complications observed during the prenatal period. He was progressing well over the 1st few months and achieving the appropriate milestones. On examination, his abdomen appears soft with no liver enlargement. The patient appears to be dehydrated and lethargic. The results of a fundoscopic examination are shown in the picture. A blood test for which of the following enzymes is the next best assay to evaluate this patient's health?
- A. Acid alpha-glucosidase
- B. Hexosaminidase (Correct Answer)
- C. Sphingomyelinase
- D. Glucocerebrosidase
- E. Arylsulfatase A
GSD type II (Pompe disease) Explanation: ***Hexosaminidase***
- The symptoms and history suggest **Tay-Sachs disease**, characterized by progressive weakness and developmental delay, often linked to **deficiency in hexosaminidase A**.
- A fundoscopic exam typically reveals a **cherry-red spot**, consistent with this condition, making hexosaminidase testing essential for diagnosis.
- Tay-Sachs results from accumulation of **GM2 ganglioside** in neurons due to hexosaminidase A deficiency.
*Glucocerebrosidase*
- This enzyme is primarily associated with **Gaucher's disease**, which does not match the clinical features presented here.
- Symptoms of Gaucher's disease include **hepatosplenomegaly** and bone pain, not primarily weakness or lethargy in a young infant.
*Acid alpha-glucosidase*
- Generally tested for **Pompe disease**, which typically presents with **muscle weakness and hypertrophic cardiomyopathy**, not solely lethargy and failure to thrive.
- The clinical presentation in this case does not indicate glycogen storage disorder symptoms.
*Arylsulfatase A*
- This enzyme deficiency relates to **metachromatic leukodystrophy**, which often features neurological decline rather than isolated lethargy in infants.
- The specific symptoms and age do not align with the typical findings of this condition.
*Sphingomyelinase*
- Linked to **Niemann-Pick disease**, characterized by **hepatosplenomegaly** and neurological deterioration, absent in this scenario.
- The presentation of weakness does not match the classic signs expected with sphingomyelinase deficiency.
GSD type II (Pompe disease) US Medical PG Question 2: A 3-month-old girl is brought to the emergency department by her parents after she appeared to have a seizure at home. On presentation, she no longer has convulsions though she is still noted to be lethargic. She was born through uncomplicated vaginal delivery and was not noted to have any abnormalities at the time of birth. Since then, she has been noted by her pediatrician to be falling behind in height and weight compared to similarly aged infants. Physical exam reveals an enlarged liver, and laboratory tests reveal a glucose of 38 mg/dL. Advanced testing shows that a storage molecule present in the cells of this patient has abnormally short outer chains. Which of the following enzymes is most likely defective in this patient?
- A. Debranching enzyme (Correct Answer)
- B. Hepatic phosphorylase
- C. Glucose-6-phosphatase
- D. Muscle phosphorylase
- E. Branching enzyme
GSD type II (Pompe disease) Explanation: ***Debranching enzyme***
- The presence of **abnormally short outer chains** in a storage molecule, along with **hypoglycemia** and **hepatomegaly**, strongly suggests a defect in the **debranching enzyme** (Type III Glycogen Storage Disease or Cori/Forbes disease). This enzyme is responsible for breaking down the α-1,6 glycosidic bonds at the branch points of glycogen.
- Deficiency leads to the accumulation of glycogen with **short branches**, affecting both liver and muscle.
*Hepatic phosphorylase*
- A defect in **hepatic phosphorylase** (Type VI Glycogen Storage Disease or Hers' disease) leads to similar symptoms like **hepatomegaly** and **hypoglycemia**.
- However, the glycogen structure would be normal, not characterized by abnormally short outer chains.
*Glucose-6-phosphatase*
- A deficiency in **glucose-6-phosphatase** (Type I Glycogen Storage Disease or Von Gierke's disease) leads to severe **hypoglycemia**, **hepatomegaly**, and often **renal enlargement**.
- Glycogen structure in this condition is typically normal, with **increased hepatic glycogen stores**.
*Muscle phosphorylase*
- A deficiency in **muscle phosphorylase** (Type V Glycogen Storage Disease or McArdle's disease) primarily affects skeletal muscle function, causing **muscle cramping**, pain, and **fatigue during exercise**.
- It does not typically present with severe **hypoglycemia** or **hepatomegaly** because the liver enzyme is unaffected.
*Branching enzyme*
- A defect in the **branching enzyme** (Type IV Glycogen Storage Disease or Andersen's disease) results in glycogen with **abnormally long unbranched chains** and fewer branch points.
- This typically leads to **cirrhosis** and liver failure, and while hypoglycemia can occur, the characteristic glycogen structure is the opposite of what is described in the patient.
GSD type II (Pompe disease) US Medical PG Question 3: A 38-year-old woman presents to her primary care physician for evaluation of 3 months of increasing fatigue. She states that she feels normal in the morning, but that her fatigue gets worse throughout the day. Specifically, she says that her head drops when trying to perform overhead tasks. She also says that she experiences double vision when watching television or reading a book. On physical exam, there is right-sided ptosis after sustaining upward gaze for a 2 minutes. Which of the following treatments may be effective in treating this patient's diagnosis?
- A. Chemotherapy
- B. Vaccination
- C. Thymectomy (Correct Answer)
- D. Antitoxin
- E. Riluzole
GSD type II (Pompe disease) Explanation: ***Thymectomy***
- This patient's symptoms (fatigue worsening throughout the day, ptosis, diplopia, and head drop with overhead tasks) are classic for **myasthenia gravis (MG)**. Thymectomy is a definitive treatment option, especially for patients with a **thymoma** or generalized MG.
- Approximately 10-15% of MG patients have a thymoma, and many others have thymic hyperplasia. **Thymectomy** can lead to remission or improvement in a significant number of patients by reducing the production of abnormal antibodies.
*Chemotherapy*
- Chemotherapy is primarily used for treating cancers and is not a first-line treatment for autoimmune diseases like **myasthenia gravis**.
- While some immunosuppressants used in cancer may also be used in MG, chemotherapy, in its primary role, is not indicated for this condition.
*Vaccination*
- Vaccination is a preventive measure against infectious diseases and plays no role in the direct treatment of **myasthenia gravis**, which is an autoimmune disorder.
- While MG patients should receive recommended vaccinations, these do not treat the underlying disease.
*Antitoxin*
- Antitoxins are used to neutralize toxins produced by bacteria, such as in **botulism** or **tetanus**.
- Myasthenia gravis is an autoimmune disease involving antibodies against acetylcholine receptors, not a bacterial toxin.
*Riluzole*
- **Riluzole** is a medication approved for the treatment of **amyotrophic lateral sclerosis (ALS)**, a progressive neurodegenerative disease.
- It works by reducing glutamate-mediated excitotoxicity and has no role in the pathophysiology or treatment of **myasthenia gravis**.
GSD type II (Pompe disease) US Medical PG Question 4: A 7-year-old boy is brought to his pediatrician by his mother who is worried about his clumsiness. She states that over the past 3 months she has noticed progressive weakness. He used to climb trees and run outside with his cousins, but now he says he gets “too tired.” She’s recently noticed him starting to “walk funny,” despite having “muscular legs.” Upon physical examination, the patient has calf muscle hypertrophy. He uses his arms to rise out of the chair. Labs are obtained that show an elevated creatine kinase. Genetic analysis detects a dystropin gene mutation. A muscle biopsy is performed that reveals reduced dystrophin. Which of the following is the most likely diagnosis?
- A. Fragile X syndrome
- B. Pompe disease
- C. Duchenne muscular dystrophy (Correct Answer)
- D. Spinal muscular atrophy
- E. Becker muscular dystrophy
GSD type II (Pompe disease) Explanation: ***Duchenne muscular dystrophy***
- This 7-year-old presents with classic features of **Duchenne muscular dystrophy (DMD)**: **progressive proximal muscle weakness**, **calf pseudohypertrophy**, **Gowers' sign** (using arms to rise from a chair), and **markedly elevated creatine kinase**.
- Genetic analysis confirms a **dystrophin gene mutation**, and muscle biopsy shows **reduced dystrophin**, consistent with DMD where dystrophin is absent or severely reduced (<3% of normal).
- The **age of presentation (7 years)** is typical for DMD, as many boys are diagnosed between ages 3-7 when motor delays become apparent in school settings; the recent 3-month history of rapid decline is characteristic of DMD's progressive course.
- Boys with DMD typically lose ambulation by age 12 and require wheelchair assistance, distinguishing it from the milder Becker variant.
*Becker muscular dystrophy*
- While also caused by a **dystrophin gene mutation**, Becker muscular dystrophy (BMD) presents **later** (typically age 8-25) with a **much milder and slower progression**.
- In BMD, dystrophin is **reduced but functional** (3-20% or more of normal, often abnormal in size), not severely deficient as in this case.
- Patients with BMD remain ambulatory into their 20s-30s or beyond, which contrasts with this patient's relatively early onset and rapid 3-month decline.
- The clinical tempo and age of onset in this case are more consistent with Duchenne than Becker.
*Fragile X syndrome*
- This is a genetic disorder primarily characterized by **intellectual disability**, **developmental delays**, **autism spectrum features**, and distinct physical features (long face, large ears, macroorchidism).
- It does not present with **progressive muscle weakness**, **calf pseudohypertrophy**, **elevated CK**, or **dystrophin gene mutations**.
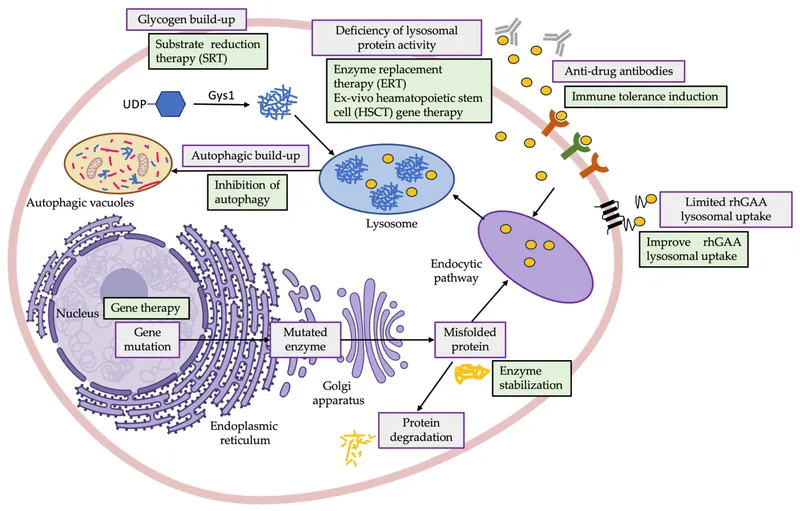
*Pompe disease*
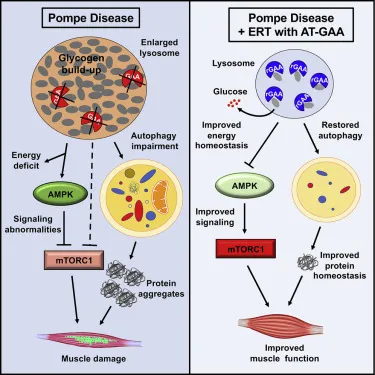
- This is a **lysosomal storage disorder** caused by deficiency of **acid alpha-glucosidase (GAA)**, leading to glycogen accumulation in lysosomes.
- While it can cause **muscle weakness** and elevated CK, infantile-onset Pompe presents with **cardiomyopathy** and **hypotonia** ("floppy infant"), and late-onset Pompe presents with limb-girdle weakness and respiratory failure.
- Pompe does **not involve dystrophin mutations** or **calf pseudohypertrophy**.
*Spinal muscular atrophy*
- This disorder results from **loss of motor neurons** in the spinal cord due to **SMN1 gene mutations**, causing muscle weakness and atrophy.
- SMA presents with **hypotonia**, **areflexia**, and **muscle atrophy** (not hypertrophy), with **fasciculations** of the tongue in some cases.
- It does **not involve dystrophin mutations**, **calf pseudohypertrophy**, or markedly elevated CK levels.
GSD type II (Pompe disease) US Medical PG Question 5: A 5-month-old boy presents with increasing weakness for the past 3 months. The patient’s mother says that the weakness is accompanied by dizziness, sweating, and vertigo early in the morning. Physical examination shows hepatomegaly. Laboratory findings show an increased amount of lactate, uric acid, and elevated triglyceride levels. Which of the following enzymes is most likely deficient in this patient?
- A. Hepatic glycogen phosphorylase
- B. Debranching enzyme
- C. Glucose-6-phosphatase (Correct Answer)
- D. Muscle glycogen phosphorylase
- E. Lysosomal α-1,4-glucosidase
GSD type II (Pompe disease) Explanation: ***Glucose-6-phosphatase***
- The constellation of **hypoglycemia** (weakness, dizziness, sweating, vertigo, especially early morning), **hepatomegaly**, **lactic acidosis**, **hyperuricemia**, and **hypertriglyceridemia** are classic features of **Type I glycogen storage disease (von Gierke disease)**, which is caused by a deficiency of **glucose-6-phosphatase**.
- This enzyme is crucial for the final step of both **glycogenolysis** and **gluconeogenesis**, releasing free glucose into the bloodstream; its deficiency leads to an inability to maintain normal blood glucose levels during fasting and accumulation of glucose-6-phosphate, which shunts into other metabolic pathways.
*Hepatic glycogen phosphorylase*
- Deficiency in **hepatic glycogen phosphorylase** (Type VI glycogen storage disease, Hers disease) would cause **hepatomegaly** and **hypoglycemia**, but typically does not present with severe **lactic acidosis**, **hyperuricemia**, or **hypertriglyceridemia** to the same degree as von Gierke disease.
- The primary defect is in breaking down glycogen, leading to its accumulation in the liver, but the products of glycolysis can still exit the liver via gluconeogenesis.
*Debranching enzyme*
- Deficiency in **debranching enzyme** (Type III glycogen storage disease, Cori or Forbes disease) causes **hepatomegaly** and **hypoglycemia**, but usually presents with milder symptoms and less severe **lactic acidosis**, **hyperuricemia**, and **hypertriglyceridemia**.
- Patients often present with symptoms similar to Type I, but muscle involvement is also common, and **glycogen structures with short outer branches** are characteristic.
*Muscle glycogen phosphorylase*
- Deficiency in **muscle glycogen phosphorylase** (Type V glycogen storage disease, McArdle disease) primarily affects **skeletal muscle**, leading to exercise intolerance, muscle pain, and myoglobinuria.
- It does not typically cause **hypoglycemia** or **hepatomegaly**, as the liver enzyme is functional, and the symptoms described are systemic rather than muscle-specific.
*Lysosomal α-1,4-glucosidase*
- Deficiency in **lysosomal α-1,4-glucosidase** (Type II glycogen storage disease, Pompe disease) primarily affects the **heart, muscle, and liver**, causing severe **cardiomyopathy**, hypotonia, and **hepatomegaly**.
- While it involves glycogen accumulation, it typically does not present with **hypoglycemia** (as cytoplasmic glycogen metabolism is intact), **lactic acidosis**, or the specific metabolic derangements seen in this patient.
GSD type II (Pompe disease) US Medical PG Question 6: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
GSD type II (Pompe disease) Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
GSD type II (Pompe disease) US Medical PG Question 7: A 9-month-old girl is brought to the physician because of a 1-month history of poor feeding and irritability. She is at the 15th percentile for height and 5th percentile for weight. Examination shows hypotonia and wasting of skeletal muscles. Cardiopulmonary examination shows no abnormalities. There is hepatomegaly. Her serum glucose is 61 mg/dL, creatinine kinase is 100 U/L, and lactic acid is within the reference range. Urine ketone bodies are elevated. Which of the following enzymes is most likely deficient in this patient?
- A. Glucose-6-phosphatase
- B. Muscle phosphorylase
- C. Acid alpha-glucosidase
- D. Glycogen debrancher (Correct Answer)
- E. Glucocerebrosidase
GSD type II (Pompe disease) Explanation: ***Glycogen debrancher***
- The patient's symptoms of **hepatomegaly**, **hypoglycemia**, **poor feeding**, **growth failure**, and **elevated urine ketones** in the presence of normal lactic acid suggest Type III glycogen storage disease (Cori disease), caused by a deficiency in **glycogen debrancher enzyme**.
- **Muscle wasting** and **hypotonia** are also consistent with Type III GSD, as the debranching enzyme is present in both liver and muscle.
*Glucose-6-phosphatase*
- Deficiency in **glucose-6-phosphatase** (Type I GSD, Von Gierke disease) also presents with **hepatomegaly** and **hypoglycemia**.
- However, Type I GSD is characterized by **lactic acidosis**, which is explicitly stated as normal in this patient, and **hyperlipidemia**, which is not mentioned.
*Muscle phosphorylase*
- Deficiency in **muscle phosphorylase** (Type V GSD, McArdle disease) primarily affects skeletal muscle, causing **exercise intolerance** and **muscle pain**.
- It does not typically present with **hypoglycemia**, **hepatomegaly**, or **growth failure** in infancy.
*Acid alpha-glucosidase*
- Deficiency in **acid alpha-glucosidase** (Type II GSD, Pompe disease) causes accumulation of glycogen in lysosomes, leading to severe **cardiomyopathy**, **hypotonia**, and **muscle weakness**.
- While hypotonia is present, the absence of **cardiomegaly** and significant **liver involvement** makes this diagnosis less likely.
*Glucocerebrosidase*
- Deficiency in **glucocerebrosidase** causes Gaucher disease, a lysosomal storage disorder, not a glycogen storage disorder.
- Symptoms include **hepatosplenomegaly**, **bone crises**, and neurological symptoms, but not **hypoglycemia** or isolated muscle wasting directly related to glycogen metabolism.
GSD type II (Pompe disease) US Medical PG Question 8: A newborn infant presents with severe weakness. He was born to a G1P1 mother at 40 weeks gestation with the pregnancy attended by a midwife. The mother's past medical history is unremarkable. She took a prenatal vitamin and folic acid throughout the pregnancy. Since birth, the child has had trouble breastfeeding despite proper counseling. He also has had poor muscle tone and a weak cry. His temperature is 99.5°F (37.5°C), blood pressure is 57/38 mmHg, pulse is 150/min, respirations are 37/min, and oxygen saturation is 96% on room air. Physical exam reveals poor muscle tone. The patient's sucking reflex is weak, and an enlarged tongue is noted. An ultrasound is performed, and is notable for hypertrophy of the myocardium. Which of the following is the most likely diagnosis?
- A. Acid maltase deficiency (Correct Answer)
- B. Familial hypertrophic cardiomyopathy
- C. Clostridium tetani infection
- D. Spinal muscular atrophy type I disease
- E. Clostridium botulinum infection
GSD type II (Pompe disease) Explanation: ***Acid maltase deficiency***
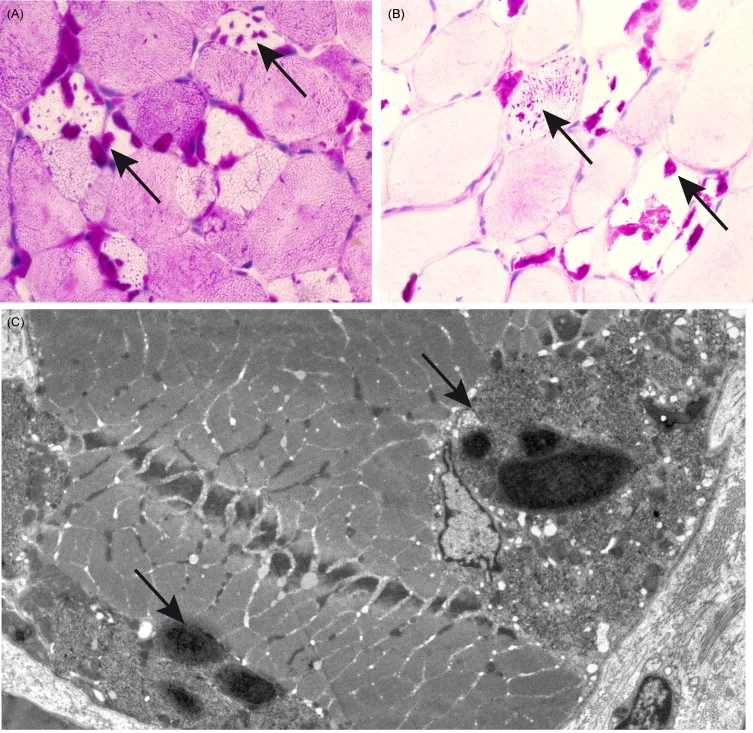
- This condition is also known as **Pompe disease**. It is a **lysosomal storage disease** that presents in infancy with **cardiomegaly**, **macroglossia**, **hypotonia**, and **respiratory failure**, all of which are consistent with the patient's presentation.
- The deficiency in **acid alpha-glucosidase (acid maltase)** leads to glycogen accumulation in lysosomes, particularly in muscle cells, causing impaired muscle function, including the heart.
*Familial hypertrophic cardiomyopathy*
- While it causes **myocardial hypertrophy**, it typically does **not present with profound generalized hypotonia, macroglossia, or feeding difficulties** as the primary symptoms in infancy.
- This condition is usually due to **sarcomeric protein mutations** and lacks the widespread systemic muscle involvement seen in Pompe disease.
*Clostridium tetani infection*
- This infection causes **tetanus**, characterized by **severe muscle spasms, trismus (lockjaw), and opisthotonus**, rather than hypotonia and weakness.
- It would also typically involve a history of a **puncture wound or contaminated injury**, which is not mentioned.
*Spinal muscular atrophy type I disease*
- This is characterized by **severe hypotonia** and **muscle weakness** due to the degeneration of anterior horn cells.
- However, **cardiomegaly and macroglossia are not typical features** of spinal muscular atrophy.
*Clostridium botulinum infection*
- This infection causes **flaccid paralysis** and weakness, usually presenting with **constipation**, **weak cry**, and **difficulty feeding**, by preventing acetylcholine release at neuromuscular junctions.
- However, **cardiomyopathy and macroglossia are not characteristic** of botulism.
GSD type II (Pompe disease) US Medical PG Question 9: A 1-year-old male with a history of recurrent pseudomonal respiratory infections and steatorrhea presents to the pediatrician for a sweat test. The results demonstrate a chloride concentration of 70 mEq/L (nl < 40 mEq/L). Which of the following defects has a similar AUTOSOMAL RECESSIVE mode of inheritance as the disorder experienced by this patient?
- A. Abnormal production of type IV collagen
- B. Trinucleotide repeat expansion of CAG on chromosome 4
- C. Mutated gene for mitochondrial-tRNA-Lys
- D. Accumulation of glycogen in the lysosome (Correct Answer)
- E. Inability to convert carbamoyl phosphate and ornithine into citrulline
GSD type II (Pompe disease) Explanation: ***Accumulation of glycogen in the lysosome***
- The patient's symptoms (recurrent **pseudomonal respiratory infections**, **steatorrhea**, and elevated sweat chloride) are classic for **cystic fibrosis (CF)**, an **autosomal recessive** disorder.
- Accumulation of glycogen in the lysosome describes **Pompe disease (Type II Glycogen Storage Disease)**, which is also an **autosomal recessive** disorder, making this the correct answer.
*Abnormal production of type IV collagen*
- This defect is characteristic of **Alport syndrome**, which is predominantly **X-linked dominant** (~80-85% of cases), though autosomal recessive forms exist.
- The question context and typical board exam framing classify this as X-linked, not autosomal recessive.
- Alport syndrome primarily affects the kidneys, ears, and eyes, and does not present with recurrent pseudomonal infections or steatorrhea.
*Trinucleotide repeat expansion of CAG on chromosome 4*
- This genetic defect is responsible for **Huntington's disease**, which is an **autosomal dominant** neurodegenerative disorder.
- Huntington's disease presents with chorea, cognitive decline, and psychiatric symptoms, which are distinct from CF.
*Mutated gene for mitochondrial-tRNA-Lys*
- A mutated gene for mitochondrial-tRNA-Lys is associated with **MELAS syndrome (Mitochondrial Encephalomyopathy, Lactic Acidosis, and Stroke-like episodes)**, which is inherited through **maternal (mitochondrial)** inheritance.
- This mode of inheritance is distinct from the autosomal recessive pattern seen in cystic fibrosis.
*Inability to convert carbamoyl phosphate and ornithine into citrulline*
- This describes a defect in **ornithine transcarbamylase (OTC) deficiency**, an **X-linked recessive** disorder, not autosomal recessive.
- OTC deficiency leads to hyperammonemia and metabolic disturbances, without the pulmonary and gastrointestinal symptoms typical of cystic fibrosis.
GSD type II (Pompe disease) US Medical PG Question 10: An 8-month-old infant is brought in with poor feeding, lethargy, hypotonia, and hepatomegaly. Labs reveal hypoglycemia and metabolic acidosis. Which condition is most likely?
- A. Hereditary fructose intolerance
- B. Galactosemia
- C. Pompe disease
- D. Von Gierke disease (Correct Answer)
- E. Medium-chain acyl-CoA dehydrogenase (MCAD) deficiency
GSD type II (Pompe disease) Explanation: ***Von Gierke disease***
- **Type I glycogen storage disease** (GSD I) typically presents in infancy with **hypoglycemia** (due to impaired glucose release from glycogen), **hepatomegaly** (due to glycogen accumulation), and **lactic acidosis**.
- Other common findings include **hyperlipidemia** and **hyperuricemia**, while **hypotonia** and **poor feeding** are generalized symptoms stemming from metabolic derangements.
*Hereditary fructose intolerance*
- This condition presents when **fructose** is introduced into the diet, typically after 4-6 months of age, with symptoms like **nausea, vomiting, abdominal pain**, and **hepatomegaly**.
- While it can cause **hypoglycemia** and **metabolic acidosis**, the profound **hypotonia** and general metabolic collapse described in an 8-month-old on a typical diet makes GSD I more likely initially.
*Galactosemia*
- Symptoms usually appear within days or weeks of birth upon the initiation of **milk feeding**, including **vomiting, lethargy, poor feeding, jaundice, hepatomegaly**, and **cataracts**.
- While it causes **hypoglycemia** and can lead to acidosis and hypotonia, the age of presentation and lack of specific mention of jaundice or cataracts makes it a less precise fit.
*Pompe disease*
- Also known as **glycogen storage disease type II**, it is characterized by the accumulation of glycogen in **lysosomes**, primarily affecting muscles.
- The infantile form presents with severe **cardiomyopathy**, **muscle weakness**, and **hypotonia**, but **hypoglycemia** and **hepatomegaly** are not its primary or most prominent features.
*Medium-chain acyl-CoA dehydrogenase (MCAD) deficiency*
- A **fatty acid oxidation disorder** that presents with episodic **hypoglycemia** (particularly during fasting or illness), **lethargy**, and **hepatomegaly**.
- Key distinguishing features include **hypoketotic hypoglycemia** and elevated **dicarboxylic acids** on urine organic acids, but the **lactic acidosis** and overall metabolic profile are more consistent with GSD I.
More GSD type II (Pompe disease) US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.