Glycogen structure and metabolism overview US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Glycogen structure and metabolism overview. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Glycogen structure and metabolism overview US Medical PG Question 1: A 4-month-old boy is brought to his pediatrician for a well-child visit. His parents have noticed that he has had poor growth compared to his older siblings. The boy was delivered vaginally after a normal pregnancy. His temperature is 98.8°F (37.1°C), blood pressure is 98/68 mmHg, pulse is 88/min, and respirations are 20/min. On exam, his abdomen appears protuberant, and the boy appears to have abnormally enlarged cheeks. A finger stick reveals that the patient’s fasting blood glucose is 50 mg/dL. On further laboratory testing, the patient is found to have elevated blood lactate levels, as well as no response to a glucagon stimulation test. What enzymatic defect is most likely present?
- A. Alpha-1,4-glucosidase
- B. Glycogen synthase
- C. Alpha-1,6-glucosidase
- D. Glucose-6-phosphatase (Correct Answer)
- E. Glycogen phosphorylase
Glycogen structure and metabolism overview Explanation: ***Glucose-6-phosphatase***
- The patient's symptoms, including **hypoglycemia**, **hepatomegaly** (implied by protuberant abdomen), **lactic acidosis** (elevated lactate), and lack of response to **glucagon stimulation**, are classic for **Type I glycogen storage disease (von Gierke disease)**, which is caused by a deficiency in **glucose-6-phosphatase**.
- This enzyme is crucial for the final step of both **glycogenolysis** and **gluconeogenesis**, and its deficiency prevents the liver from releasing glucose into the bloodstream, leading to severe hypoglycemia.
*Alpha-1,4-glucosidase*
- A deficiency in **alpha-1,4-glucosidase (acid maltase)** causes **Type II glycogen storage disease (Pompe disease)**, which primarily affects muscle (cardiac and skeletal).
- Symptoms include **cardiomyopathy**, **hypotonia**, and muscle weakness, and it does **not** typically present with hypoglycemia or lactic acidosis.
*Glycogen synthase*
- A deficiency in **glycogen synthase** would lead to an inability to synthesize glycogen, resulting in **hypoglycemia** but **low** (rather than high) glycogen levels.
- Patients typically experience fasting hypoglycemia, but **no hepatomegaly** or lactic acidosis would be expected.
*Alpha-1,6-glucosidase*
- A deficiency in **alpha-1,6-glucosidase (debranching enzyme)** causes **Type III glycogen storage disease (Cori disease)**.
- This condition presents with **hepatomegaly**, **hypoglycemia**, and sometimes muscle weakness, but patients typically **do respond to glucagon** and have less severe lactic acidosis compared to Type I.
*Glycogen phosphorylase*
- A deficiency in **glycogen phosphorylase (hepatic form, Type VI GSD or Hers disease)** primarily affects the liver's ability to break down glycogen.
- This typically causes **hepatomegaly** and **hypoglycemia**, but usually, the patients **respond to glucagon** because other pathways for glucose release (like gluconeogenesis) are intact.
Glycogen structure and metabolism overview US Medical PG Question 2: A 30-year-old woman presents to her physician for her annual checkup. She has diabetes mellitus, type 1 and takes insulin regularly. She reports no incidents of elevated or low blood sugar and that she is feeling energetic and ready to face the morning every day. Her vital signs and physical are normal. On the way home from her checkup she stops by the pharmacy and picks up her prescription of insulin. Later that night she takes a dose. What is the signaling mechanism associated with this medication?
- A. Increased concentration intracellular cAMP
- B. Increased permeability of the cell membrane to negatively charged molecules
- C. Activation of tyrosine kinase (Correct Answer)
- D. Rapid and direct upregulation of enzyme transcription
- E. Increased permeability of the cell membrane to positively charged molecules
Glycogen structure and metabolism overview Explanation: ***Activation of tyrosine kinase***
- **Insulin** primarily binds to the **insulin receptor**, which is a **receptor tyrosine kinase**.
- Upon insulin binding, the intrinsic tyrosine kinase activity of the receptor is activated, leading to **autophosphorylation** and phosphorylation of downstream signaling proteins like **IRS-1**.
*Increased concentration intracellular cAMP*
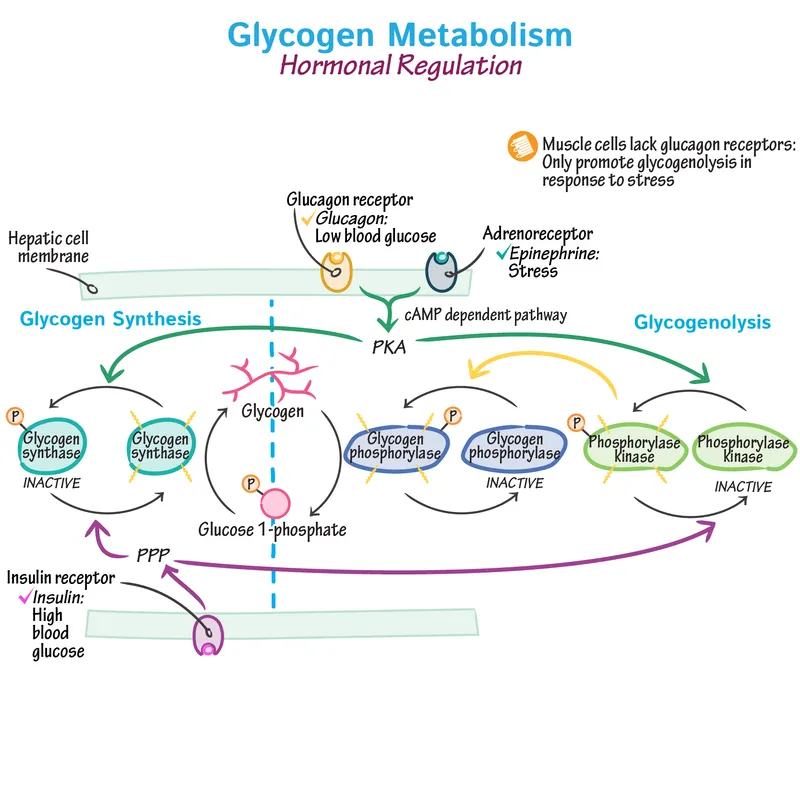
- This mechanism is characteristic of signaling pathways involving **G protein-coupled receptors** that activate adenylyl cyclase, such as those for **glucagon** or **catecholamines**.
- Insulin does not primarily signal through **cAMP** as a second messenger.
*Increased permeability of the cell membrane to negatively charged molecules*
- Changes in membrane permeability to negatively charged molecules are usually associated with **GABAergic** or **glycinergic neurotransmission**, leading to inhibitory postsynaptic potentials.
- This is not a primary mechanism for **insulin signaling**.
*Rapid and direct upregulation of enzyme transcription*
- While insulin does influence gene expression over longer periods, its immediate effects involve **protein phosphorylation** and translocation, not direct, rapid transcriptional changes at the moment of receptor binding.
- Steroid hormones typically mediate more direct transcriptional regulation.
*Increased permeability of the cell membrane to positively charged molecules*
- This mechanism is characteristic of **ligand-gated ion channels** that allow influx of ions like **Na+** or **Ca2+**, important in neuronal excitation or muscle contraction.
- Insulin signaling primarily involves **kinase cascades** and not direct changes in membrane permeability to positive ions.
Glycogen structure and metabolism overview US Medical PG Question 3: A scientist is trying to design a drug to modulate cellular metabolism in the treatment of obesity. Specifically, he is interested in understanding how fats are processed in adipocytes in response to different energy states. His target is a protein within these cells that catalyzes catabolism of an energy source. The products of this reaction are subsequently used in gluconeogenesis or β-oxidation. Which of the following is true of the most likely protein that is being studied by this scientist?
- A. It is stimulated by epinephrine (Correct Answer)
- B. It is inhibited by glucagon
- C. It is inhibited by acetylcholine
- D. It is inhibited by cortisol
- E. It is stimulated by insulin
Glycogen structure and metabolism overview Explanation: ***It is stimulated by epinephrine***
- The protein described is likely **hormone-sensitive lipase (HSL)**, which catabolizes **triglycerides** in adipocytes to **glycerol** and **fatty acids**.
- **Epinephrine** (and norepinephrine) stimulates HSL activity via a **cAMP-dependent protein kinase A (PKA)** pathway, leading to increased fatty acid release for energy.
*It is inhibited by glucagon*
- **Glucagon primarily acts on the liver** to promote gluconeogenesis and glycogenolysis, but it does **not directly inhibit HSL** in adipocytes.
- While glucagon has a lipolytic effect, it doesn't inhibit the enzyme that releases fatty acids.
*It is inhibited by acetylcholine*
- **Acetylcholine** is a neurotransmitter involved in the **parasympathetic nervous system**, which generally promotes energy storage.
- It does **not directly inhibit HSL**; its effects on lipid metabolism are indirect and typically involve other pathways.
*It is inhibited by cortisol*
- **Cortisol**, a glucocorticoid, generally **promotes lipolysis** (breakdown of fats) in certain contexts, particularly during stress to provide energy substrates.
- Therefore, it would **not inhibit HSL**; rather, it often enhances its activity or provides a permissive effect for other lipolytic hormones.
*It is stimulated by insulin*
- **Insulin** is an **anabolic hormone** that promotes energy storage, including **lipogenesis** (fat synthesis) and inhibits lipolysis.
- Insulin **inhibits HSL activity** by activating phosphodiesterase, which reduces cAMP levels, thus deactivating PKA and preventing HSL phosphorylation.
Glycogen structure and metabolism overview US Medical PG Question 4: An experimental compound added to a protein disrupts both alpha helices as well as beta-pleated sheets. Which of the following has the experimental compound affected?
- A. Ionic bonds between amino acids
- B. Hydrogen bonds between amino acids (Correct Answer)
- C. Covalent peptide bonds between amino acids
- D. Disulfide bonds between amino acids
- E. The primary structure of the protein
Glycogen structure and metabolism overview Explanation: ***Hydrogen bonds between amino acids***
- Both **alpha helices** and **beta-pleated sheets** are formed and stabilized by **hydrogen bonds** between the backbone atoms (carbonyl oxygen and amide hydrogen) of different amino acids.
- Disrupting these specific bonds would destabilize and unravel these **secondary protein structures**.
*Ionic bonds between amino acids*
- **Ionic bonds** are electrostatic interactions between charged R-groups of amino acids and primarily contribute to **tertiary** and **quaternary protein structures**.
- While important for overall protein folding, they are not the primary stabilizing force for **alpha helices** and **beta-pleated sheets**.
*Covalent peptide bonds between amino acids*
- **Peptide bonds** are the **covalent links** that form the **primary structure** (amino acid sequence) of a protein.
- Disrupting these would lead to the protein breaking down into smaller peptides or individual amino acids, which is a much more severe disruption than just affecting secondary structures.
*Disulfide bonds between amino acids*
- **Disulfide bonds** are **covalent bonds** formed between the sulfur atoms of two **cysteine residues**.
- These bonds contribute significantly to the stability of **tertiary protein structure** and sometimes **quaternary structure**, but not directly to the formation of alpha helices or beta-pleated sheets.
*The primary structure of the protein*
- The **primary structure** is the unique linear sequence of amino acids linked by **peptide bonds**.
- Disruption of **alpha helices** and **beta-pleated sheets** indicates an effect on the **secondary structure**, not the primary sequence itself.
Glycogen structure and metabolism overview US Medical PG Question 5: An investigator is studying a hereditary defect in the mitochondrial enzyme succinyl-CoA synthetase. In addition to succinate, the reaction catalyzed by this enzyme produces a molecule that is utilized as an energy source for protein translation. This molecule is also required for which of the following conversion reactions?
- A. Oxaloacetate to phosphoenolpyruvate (Correct Answer)
- B. Pyruvate to acetyl-CoA
- C. Acetaldehyde to acetate
- D. Glucose-6-phosphate to 6-phosphogluconolactone
- E. Fructose-6-phosphate to fructose-1,6-bisphosphate
Glycogen structure and metabolism overview Explanation: ***Oxaloacetate to phosphoenolpyruvate***
- The reaction catalyzed by **succinyl-CoA synthetase** (also known as succinate thiokinase) produces **GTP** (guanosine triphosphate) from GDP and Pi, in addition to succinate.
- **GTP** is required for the conversion of **oxaloacetate** to **phosphoenolpyruvate** in gluconeogenesis, catalyzed by **PEP carboxykinase**.
*Pyruvate to acetyl-CoA*
- This reaction is catalyzed by the **pyruvate dehydrogenase complex** and produces NADH, not GTP.
- It is an irreversible step linking glycolysis to the citric acid cycle.
*Acetaldehyde to acetate*
- This reaction is catalyzed by **aldehyde dehydrogenase** and uses **NAD+** as a cofactor, producing NADH.
- It is involved in alcohol metabolism.
*Glucose-6-phosphate to 6-phosphogluconolactone*
- This is the first committed step of the **pentose phosphate pathway**, catalyzed by **glucose-6-phosphate dehydrogenase**.
- It uses **NADP+** as a cofactor, producing NADPH.
*Fructose-6-phosphate to fructose-1,6-bisphosphate*
- This reaction is a key regulatory step in **glycolysis**, catalyzed by **phosphofructokinase-1 (PFK-1)**.
- It consumes **ATP**, rather than producing GTP or utilizing it as a cofactor in the context of this question.
Glycogen structure and metabolism overview US Medical PG Question 6: The balance between glycolysis and gluconeogenesis is regulated at several steps, and accumulation of one or more products/chemicals can either promote or inhibit one or more enzymes in either pathway. Which of the following molecules if increased in concentration can promote gluconeogenesis?
- A. ADP
- B. Acetyl-CoA (Correct Answer)
- C. AMP
- D. Fructose-2,6-bisphosphate
- E. Insulin
Glycogen structure and metabolism overview Explanation: ***Acetyl-CoA***
- **Acetyl-CoA** promotes gluconeogenesis by activating **pyruvate carboxylase**, the enzyme that converts pyruvate to oxaloacetate, effectively pushing the pathway forward.
- High levels of **Acetyl-CoA** generally signal a state of abundant energy from fatty acid oxidation, indicating that glucose is not immediately needed for energy and can be synthesized for storage or use elsewhere.
*ADP*
- **ADP** is a key indicator of low cellular energy and **stimulates** glycolysis while **inhibiting** gluconeogenesis to produce ATP.
- Its presence signals a need for energy synthesis rather than glucose production.
*AMP*
- **AMP** also signals low energy status and is a powerful **allosteric activator** of **phosphofructokinase-1 (PFK-1)**, the rate-limiting enzyme in glycolysis.
- Activates **AMP-activated protein kinase (AMPK)**, which promotes catabolic processes like glycolysis and inhibits anabolic processes like gluconeogenesis.
*Fructose-2,6-bisphosphate*
- **Fructose-2,6-bisphosphate** is a potent **allosteric activator** of **PFK-1** in glycolysis and a strong **inhibitor** of **fructose-1,6-bisphosphatase** in gluconeogenesis.
- Its levels increase in response to insulin, promoting glucose utilization and inhibiting glucose production.
*Insulin*
- **Insulin** is a hormone that **promotes glucose uptake** and utilization by tissues and **inhibits gluconeogenesis**.
- It achieves this by activating enzymes involved in glycolysis and glycogen synthesis while inhibiting key enzymes in gluconeogenesis, such as **fructose-1,6-bisphosphatase**.
Glycogen structure and metabolism overview US Medical PG Question 7: A 5-month-old boy presents with increasing weakness for the past 3 months. The patient’s mother says that the weakness is accompanied by dizziness, sweating, and vertigo early in the morning. Physical examination shows hepatomegaly. Laboratory findings show an increased amount of lactate, uric acid, and elevated triglyceride levels. Which of the following enzymes is most likely deficient in this patient?
- A. Hepatic glycogen phosphorylase
- B. Debranching enzyme
- C. Glucose-6-phosphatase (Correct Answer)
- D. Muscle glycogen phosphorylase
- E. Lysosomal α-1,4-glucosidase
Glycogen structure and metabolism overview Explanation: ***Glucose-6-phosphatase***
- The constellation of **hypoglycemia** (weakness, dizziness, sweating, vertigo, especially early morning), **hepatomegaly**, **lactic acidosis**, **hyperuricemia**, and **hypertriglyceridemia** are classic features of **Type I glycogen storage disease (von Gierke disease)**, which is caused by a deficiency of **glucose-6-phosphatase**.
- This enzyme is crucial for the final step of both **glycogenolysis** and **gluconeogenesis**, releasing free glucose into the bloodstream; its deficiency leads to an inability to maintain normal blood glucose levels during fasting and accumulation of glucose-6-phosphate, which shunts into other metabolic pathways.
*Hepatic glycogen phosphorylase*
- Deficiency in **hepatic glycogen phosphorylase** (Type VI glycogen storage disease, Hers disease) would cause **hepatomegaly** and **hypoglycemia**, but typically does not present with severe **lactic acidosis**, **hyperuricemia**, or **hypertriglyceridemia** to the same degree as von Gierke disease.
- The primary defect is in breaking down glycogen, leading to its accumulation in the liver, but the products of glycolysis can still exit the liver via gluconeogenesis.
*Debranching enzyme*
- Deficiency in **debranching enzyme** (Type III glycogen storage disease, Cori or Forbes disease) causes **hepatomegaly** and **hypoglycemia**, but usually presents with milder symptoms and less severe **lactic acidosis**, **hyperuricemia**, and **hypertriglyceridemia**.
- Patients often present with symptoms similar to Type I, but muscle involvement is also common, and **glycogen structures with short outer branches** are characteristic.
*Muscle glycogen phosphorylase*
- Deficiency in **muscle glycogen phosphorylase** (Type V glycogen storage disease, McArdle disease) primarily affects **skeletal muscle**, leading to exercise intolerance, muscle pain, and myoglobinuria.
- It does not typically cause **hypoglycemia** or **hepatomegaly**, as the liver enzyme is functional, and the symptoms described are systemic rather than muscle-specific.
*Lysosomal α-1,4-glucosidase*
- Deficiency in **lysosomal α-1,4-glucosidase** (Type II glycogen storage disease, Pompe disease) primarily affects the **heart, muscle, and liver**, causing severe **cardiomyopathy**, hypotonia, and **hepatomegaly**.
- While it involves glycogen accumulation, it typically does not present with **hypoglycemia** (as cytoplasmic glycogen metabolism is intact), **lactic acidosis**, or the specific metabolic derangements seen in this patient.
Glycogen structure and metabolism overview US Medical PG Question 8: A 24-year-old man comes to the physician because of chronic fatigue and generalized weakness after exertion. His legs feel stiff after walking long distances and he has leg cramps after climbing stairs. His symptoms are always relieved by rest. Urine dipstick shows 3+ blood and urinalysis is negative for RBCs. Baseline venous lactate and serum ammonia levels are collected, after which a blood pressure cuff is attached to the upper right arm. The patient is asked to continuously pump his right arm with the cuff inflated and additional venous samples are collected at 2-minute intervals. Analysis of the venous blood samples shows that, over time, serum ammonia levels increase and venous lactate levels remain stable. A biopsy of the right gastrocnemius muscle will most likely show which of the following?
- A. Intrafascicular CD8+ lymphocytic infiltration
- B. Endomysial fibrosis with absent dystrophin
- C. Intermyofibrillar proliferation of mitochondria
- D. Perivascular CD4+ lymphocytic infiltrate
- E. Subsarcolemmal periodic acid–Schiff-positive deposits (Correct Answer)
Glycogen structure and metabolism overview Explanation: ***Subsarcolemmal acid–Schiff-positive deposits***
- The patient's symptoms (chronic fatigue, generalized weakness, leg stiffness, and cramps after exertion, relieved by rest) combined with the **ischemic forearm test** results (increased ammonia, stable lactate) are highly suggestive of **McArdle disease** (glycogen storage disease type V).
- McArdle disease is caused by a deficiency in **myophosphorylase**, leading to an inability to break down glycogen in muscles. Muscle biopsy in McArdle disease typically reveals **subsarcolemmal accumulation of glycogen**, which stains positive with periodic acid–Schiff (PAS) reagent.
*Intrafascicular CD8+ lymphocytic infiltration*
- This finding is characteristic of **polymyositis**, an inflammatory myopathy.
- Polymyositis would typically present with **progressive proximal muscle weakness** and elevated muscle enzymes, rather than activity-induced cramps and fatigue, and the ischemic forearm test would not show stable lactate.
*Endomysial fibrosis with absent dystrophin*
- This is a hallmark of **Duchenne muscular dystrophy**, a genetic disorder.
- Duchenne muscular dystrophy presents in early childhood with **progressive muscle degeneration**, Gower's sign, and significantly elevated creatine kinase, which is different from the described symptoms.
*Intermyofibrillar proliferation of mitochondria*
- This is characteristic of **mitochondrial myopathies**, such as ragged red fibers, often seen with specific stains like Gomori trichrome.
- While mitochondrial myopathies can cause exercise intolerance, the specific ischemic forearm test results (normal lactate response) do not align with a primary defect in aerobic respiration.
*Perivascular CD4+ lymphocytic infiltrate*
- This histological finding is typically associated with **dermatomyositis**, another inflammatory myopathy linked to specific skin lesions and muscle weakness.
- Dermatomyositis shares some features with polymyositis but has distinct perivascular inflammation and usually presents with pathognomonic skin rashes, which are absent in this case.
Glycogen structure and metabolism overview US Medical PG Question 9: A 16-year-old boy comes to the physician because of muscle weakness and cramps for 5 months. He becomes easily fatigued and has severe muscle pain and swelling after 15 minutes of playing basketball with his friends. The symptoms improve after a brief period of rest. After playing, he sometimes also has episodes of reddish-brown urine. There is no family history of serious illness. Serum creatine kinase concentration is 950 U/L. Urinalysis shows:
Blood 2+
Protein negative
Glucose negative
RBC negative
WBC 1–2/hpf
Which of the following is the most likely underlying cause of this patient's symptoms?
- A. Medium-chain acyl-CoA dehydrogenase deficiency
- B. Myophosphorylase deficiency (Correct Answer)
- C. Low levels of triiodothyronine and thyroxine
- D. Acid maltase deficiency
- E. CTG repeat in the DMPK gene
Glycogen structure and metabolism overview Explanation: ***Myophosphorylase deficiency***
- This condition (McArdle disease) is an **autosomal recessive disorder** of glycogen metabolism characterized by a defect in **glycogenolysis**, specifically the breakdown of muscle glycogen. This leads to impaired energy production during exercise.
- The classic presentation includes **exercise-induced muscle pain, stiffness, cramps, fatigue**, and sometimes **myoglobinuria** (reddish-brown urine due to myoglobin release from damaged muscle), which is consistent with the patient's symptoms and elevated **creatine kinase**.
*Medium-chain acyl-CoA dehydrogenase deficiency*
- This is a disorder of **fatty acid oxidation** that primarily affects the liver, leading to episodes of **hypoketotic hypoglycemia** during fasting or illness.
- It does not typically present with isolated exercise-induced muscle pain and myoglobinuria.
*Low levels of triiodothyronine and thyroxine*
- **Hypothyroidism** can cause generalized muscle weakness, fatigue, and muscle cramps, but it is usually associated with other systemic symptoms like weight gain, cold intolerance, and constipation.
- While it can cause elevated CK, it generally does not present with acute, exercise-induced muscle pain and myoglobinuria in the manner described.
*Acid maltase deficiency*
- This (Pompe disease) is a lysosomal storage disorder affecting glycogen metabolism, but it results from a deficiency of **acid alpha-glucosidase (acid maltase)**.
- The infantile form presents with severe hypotonia and cardiomyopathy, while the juvenile and adult forms typically cause **proximal muscle weakness** and respiratory insufficiency, rather than exercise-induced muscle pain and myoglobinuria.
*CTG repeat in the DMPK gene*
- This genetic defect is associated with **myotonic dystrophy type 1 (Steinert disease)**, an autosomal dominant disorder.
- Key features include **myotonia** (delayed relaxation of muscles), muscle weakness, cataracts, and cardiac conduction abnormalities, which are distinct from the patient's presentation of exercise-induced cramps and myoglobinuria without myotonia.
Glycogen structure and metabolism overview US Medical PG Question 10: A 15-year-old boy comes to the physician because of severe muscle cramps and pain for 3 months. He first noticed these symptoms while attending tryouts for the high school football team. Since then, he becomes easily fatigued and has severe muscle pain and swelling after 10 minutes of playing. However, after a brief period of rest, the symptoms improve, and he is able to return to the game. Two days ago, he had an episode of reddish-brown urine after playing football. There is no family history of serious illness. He appears healthy. Vital signs are within normal limits. Physical and neurological examinations show no abnormalities. Serum creatine kinase concentration is 333 U/L. Urinalysis shows:
Blood 2+
Protein negative
Glucose negative
RBC negative
WBC 1–2/hpf
Which of the following is the most likely cause of this patient's symptoms?
- A. CTG repeat in the DMPK gene
- B. Myophosphorylase deficiency (Correct Answer)
- C. Dystrophin gene mutation
- D. Thyroid hormone deficiency
- E. Acid maltase deficiency
Glycogen structure and metabolism overview Explanation: ***Myophosphorylase deficiency***
- This condition (also known as **McArdle disease**) presents with **exercise-induced muscle cramps, pain, and fatigue** immediately after initiating activity, with a "second wind" phenomenon where symptoms improve after resting.
- The elevated **creatine kinase** and **reddish-brown urine** (indicating **myoglobinuria** due to rhabdomyolysis) are classic findings after strenuous activity in this glycogen storage disorder.
*CTG repeat in the DMPK gene*
- This describes **myotonic dystrophy type 1**, which presents with **myotonia** (delayed muscle relaxation), muscle weakness, and often involves multiple organ systems.
- While it causes muscle weakness, it does not typically present with acute, exercise-induced pain, cramping, and rhabdomyolysis in this manner.
*Dystrophin gene mutation*
- This is characteristic of **Duchenne or Becker muscular dystrophy**, which are progressive muscle weakness disorders.
- They typically cause **progressive proximal muscle weakness** and atrophy, not acute, intermittent, exercise-induced pain and cramping with a "second wind" phenomenon.
*Thyroid hormone deficiency*
- **Hypothyroidism** can cause muscle cramps, weakness, and elevated creatine kinase, but these symptoms are usually chronic and progressive, not acutely exercise-induced with improvement after a short rest.
- It would also present with other systemic symptoms like fatigue, weight gain, and cold intolerance, which are not described.
*Acid maltase deficiency*
- Also known as **Pompe disease**, this is a glycogen storage disorder that primarily affects infants and can present in adults with **proximal muscle weakness**, respiratory insufficiency, and cardiac involvement.
- It does not typically present with acute, exercise-induced muscle cramps, pain, and rhabdomyolysis followed by a "second wind" phenomenon like McArdle disease.
More Glycogen structure and metabolism overview US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.