Genetics and inheritance of GSDs US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Genetics and inheritance of GSDs. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Genetics and inheritance of GSDs US Medical PG Question 1: A 15-year-old boy is sent from gym class with a chief complaint of severe muscle aches. In class today he was competing with his friends and therefore engaged in weightlifting for the first time. A few hours later he was extremely sore and found that his urine was red when he went to urinate. This concerned him and he was sent to the emergency department for evaluation.
Upon further questioning, you learn that since childhood he has always had muscle cramps with exercise. Physical exam was unremarkable. Upon testing, his creatine kinase level was elevated and his urinalysis was negative for blood and positive for myoglobin.
Thinking back to biochemistry you suspect that he may be suffering from a hereditary glycogen disorder. Given this suspicion, what would you expect to find upon examination of his cells?
- A. Normal glycogen structure (Correct Answer)
- B. Short outer glycogen chains
- C. Accumulation of glycogen in lysosomes forming dense granules
- D. Glycogen without normal branching pattern
- E. Absence of glycogen in muscles
Genetics and inheritance of GSDs Explanation: ***Normal glycogen structure***
- The patient's symptoms (exercise-induced muscle cramps, myoglobinuria, and elevated CK) are classic for **McArdle disease** (Glycogen Storage Disease Type V), caused by a deficiency in **muscle glycogen phosphorylase**.
- In McArdle disease, the enzyme responsible for breaking down glycogen (glycogen phosphorylase) is deficient, but the enzymes involved in synthesizing glycogen are normal. Therefore, the **structure of glycogen is normal**, but it accumulates in muscle cells because it cannot be catabolized.
*Short outer glycogen chains*
- **Short outer glycogen chains** are characteristic of **Cori disease** (Glycogen Storage Disease Type III), caused by a deficiency in **debranching enzyme**.
- This condition also presents with hypoglycemia and hepatomegaly, which are not described in the patient's presentation.
*Accumulation of glycogen in lysosomes forming dense granules*
- **Accumulation of glycogen in lysosomes** and the formation of **dense granules** is characteristic of **Pompe disease** (Glycogen Storage Disease Type II), caused by a deficiency in **lysosomal alpha-glucosidase (acid maltase)**.
- Pompe disease typically presents as a severe infantile form with cardiomegaly and hypotonia, or a later-onset form with proximal muscle weakness, which differs from the patient's primary complaint of exercise intolerance and myoglobinuria.
*Glycogen without normal branching pattern*
- **Glycogen without a normal branching pattern** (very long unbranched chains) is characteristic of **Andersen disease** (Glycogen Storage Disease Type IV), caused by a deficiency in **branching enzyme**.
- This condition typically leads to cirrhosis and liver failure in infancy, which is not consistent with the patient's presentation.
*Absence of glycogen in muscles*
- While McArdle disease involves an inability to break down muscle glycogen, it does not result in the **absence of glycogen** in muscles; rather, there is an **over-accumulation** of normal-structured glycogen because it cannot be utilized.
- The defect is in **glycogenolysis**, not glycogen synthesis, so glycogen is formed but not broken down.
Genetics and inheritance of GSDs US Medical PG Question 2: A 23-year-old woman and her husband come to a genetic counselor because she is concerned about the chance of having an inherited defect if they had a child. Family history reveals no significant family history in her husband; however, her sister had a son who has seizures, failure to thrive, and neurodegeneration. She does not remember the name of the disease but remembers that her nephew had sparse, brittle hair that kinked in odd directions. She does not think that any other members of her family including her sister's husband have had this disorder. If this couple had a son, what is the most likely chance that he would have the same disorder that affected the patient's nephew?
- A. 100%
- B. 12.5%
- C. 25% (Correct Answer)
- D. 50%
- E. Close to 0%
Genetics and inheritance of GSDs Explanation: ***25%***
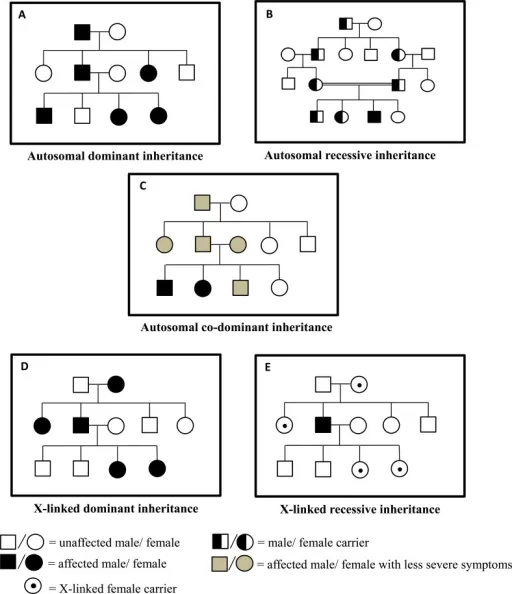
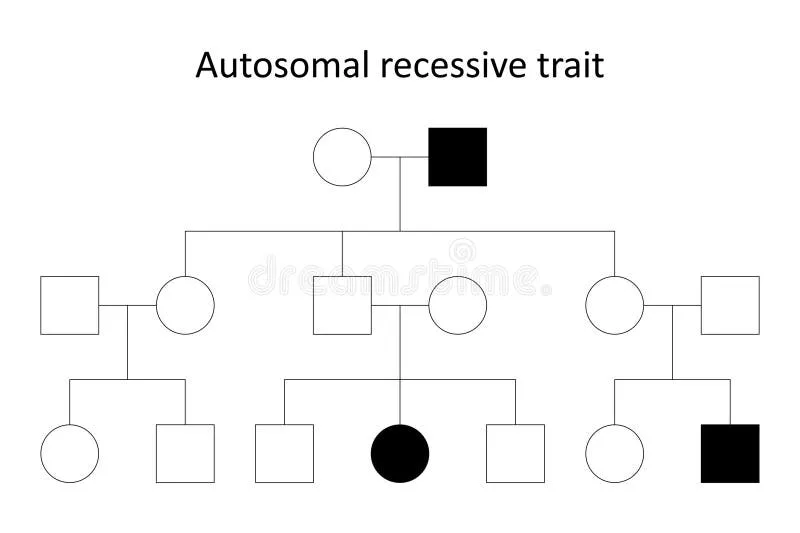
- The nephew's symptoms of **seizures, failure to thrive, neurodegeneration**, and **sparse, brittle, kinky hair** are highly indicative of **Menkes disease**, an **X-linked recessive** disorder.
- Since the patient's sister had an affected son, the sister is an **obligate carrier** of the mutation.
- The patient and her sister share the same parents, so their mother must be a carrier (or have the mutation).
- The patient herself has a **50% chance of being a carrier**.
- **If the patient is a carrier**, each son has a **50% chance** of being affected.
- **Overall probability**: 0.5 (chance patient is carrier) × 0.5 (chance son inherits mutation) = **0.25 = 25%**.
*Close to 0%*
- This would only be correct if the patient had no chance of being a carrier, which is not the case given her family history.
- Her sister's affected son confirms the mutation is present in the maternal lineage.
*100%*
- This would only occur if the patient were definitely a carrier AND all male offspring inherited the mutation, or if the disorder were autosomal dominant with complete penetrance.
- For **X-linked recessive** disorders, even carrier mothers only pass the mutation to 50% of sons on average.
*12.5%*
- This percentage might represent additional generational steps or compound probabilities not relevant to this direct parent-child scenario.
- The correct calculation for this scenario is 50% × 50% = 25%.
*50%*
- This would be correct if we knew with certainty that the patient is a carrier.
- However, since we only know her sister is a carrier, the patient has a 50% chance of being a carrier herself, making the overall risk 25%.
- This is a common error in genetic counseling calculations—forgetting to account for the uncertain carrier status of the at-risk individual.
Genetics and inheritance of GSDs US Medical PG Question 3: A 3-month-old girl is brought to the emergency department by her parents after she appeared to have a seizure at home. On presentation, she no longer has convulsions though she is still noted to be lethargic. She was born through uncomplicated vaginal delivery and was not noted to have any abnormalities at the time of birth. Since then, she has been noted by her pediatrician to be falling behind in height and weight compared to similarly aged infants. Physical exam reveals an enlarged liver, and laboratory tests reveal a glucose of 38 mg/dL. Advanced testing shows that a storage molecule present in the cells of this patient has abnormally short outer chains. Which of the following enzymes is most likely defective in this patient?
- A. Debranching enzyme (Correct Answer)
- B. Hepatic phosphorylase
- C. Glucose-6-phosphatase
- D. Muscle phosphorylase
- E. Branching enzyme
Genetics and inheritance of GSDs Explanation: ***Debranching enzyme***
- The presence of **abnormally short outer chains** in a storage molecule, along with **hypoglycemia** and **hepatomegaly**, strongly suggests a defect in the **debranching enzyme** (Type III Glycogen Storage Disease or Cori/Forbes disease). This enzyme is responsible for breaking down the α-1,6 glycosidic bonds at the branch points of glycogen.
- Deficiency leads to the accumulation of glycogen with **short branches**, affecting both liver and muscle.
*Hepatic phosphorylase*
- A defect in **hepatic phosphorylase** (Type VI Glycogen Storage Disease or Hers' disease) leads to similar symptoms like **hepatomegaly** and **hypoglycemia**.
- However, the glycogen structure would be normal, not characterized by abnormally short outer chains.
*Glucose-6-phosphatase*
- A deficiency in **glucose-6-phosphatase** (Type I Glycogen Storage Disease or Von Gierke's disease) leads to severe **hypoglycemia**, **hepatomegaly**, and often **renal enlargement**.
- Glycogen structure in this condition is typically normal, with **increased hepatic glycogen stores**.
*Muscle phosphorylase*
- A deficiency in **muscle phosphorylase** (Type V Glycogen Storage Disease or McArdle's disease) primarily affects skeletal muscle function, causing **muscle cramping**, pain, and **fatigue during exercise**.
- It does not typically present with severe **hypoglycemia** or **hepatomegaly** because the liver enzyme is unaffected.
*Branching enzyme*
- A defect in the **branching enzyme** (Type IV Glycogen Storage Disease or Andersen's disease) results in glycogen with **abnormally long unbranched chains** and fewer branch points.
- This typically leads to **cirrhosis** and liver failure, and while hypoglycemia can occur, the characteristic glycogen structure is the opposite of what is described in the patient.
Genetics and inheritance of GSDs US Medical PG Question 4: A deficiency in which of the following lysosomal enzymes is inherited in a pattern similar to a deficiency of iduronate sulfatase (Hunter syndrome)?
- A. Sphingomyelinase
- B. Glucocerebrosidase
- C. Galactocerebrosidase
- D. Alpha-L-iduronidase
- E. Alpha-galactosidase A (Correct Answer)
Genetics and inheritance of GSDs Explanation: ***Alpha-galactosidase A***
- A deficiency in **alpha-galactosidase A** causes **Fabry disease**, which, like Hunter syndrome (iduronate sulfatase deficiency), is inherited in an **X-linked recessive** pattern.
- Both conditions primarily affect males, with carrier females potentially exhibiting milder symptoms.
*Sphingomyelinase*
- A deficiency in sphingomyelinase leads to **Niemann-Pick disease types A and B**, which are inherited in an **autosomal recessive** pattern.
- This mode of inheritance differs from the X-linked pattern of Hunter syndrome.
*Glucocerebrosidase*
- A deficiency in glucocerebrosidase causes **Gaucher disease**, inherited in an **autosomal recessive** pattern.
- This is a common lysosomal storage disorder, but its inheritance pattern is distinct from X-linked disorders.
*Galactocerebrosidase*
- A deficiency in galactocerebrosidase causes **Krabbe disease (globoid cell leukodystrophy)**, which is inherited in an **autosomal recessive** pattern.
- Krabbe disease is a severe neurodegenerative disorder, but its genetic transmission is not X-linked.
*Alpha-L-iduronidase*
- A deficiency in **alpha-L-iduronidase** causes **Hurler syndrome (MPS I)**, which is inherited in an **autosomal recessive** pattern.
- While both Hunter and Hurler syndromes are mucopolysaccharidoses, their genetic inheritance patterns are different.
Genetics and inheritance of GSDs US Medical PG Question 5: A 12-year-old girl comes to the clinic with a grossly enlarged abdomen. She has a history of frequent episodes of weakness, sweating, and pallor that are eliminated by eating. Her development has been slow. She started to walk unassisted at 2 years and was not performing well at school. Physical examination reveals a blood pressure of 100/60 mm Hg, heart rate of 80/min, and temperature of 36.9°C (98.4℉). On physical examination, the liver is enlarged, firm, and palpable up to the pelvis. The spleen and kidney are not palpable. Laboratory investigation reveals low blood glucose and pH with high lactate, triglycerides, ketones, and free fatty acids. The liver biopsy revealed high glycogen content. Hepatic glycogen structure was normal. The enzyme assay performed on the biopsy tissue revealed very low glucose-6-phosphatase levels. What is the most likely diagnosis?
- A. Pompe's disease
- B. Cori's disease
- C. Hereditary hemochromatosis
- D. Von-Gierke's disease (Correct Answer)
- E. McArdle disease
Genetics and inheritance of GSDs Explanation: ***Von-Gierke's disease***
- The combination of **hepatomegaly**, **hypoglycemia** (causing weakness, sweating, pallor), **lactic acidosis**, **hyperlipidemia**, and elevated ketones points to a severe defect in glucose metabolism.
- **Very low glucose-6-phosphatase levels** on liver biopsy and normal hepatic glycogen structure are pathognomonic for Von-Gierke's disease (Glycogen Storage Disease Type I).
*Pompe's disease*
- This is a **lysosomal storage disease** affecting **alpha-1,4-glucosidase**, leading to glycogen accumulation in lysosomes.
- It primarily affects the **heart** and skeletal muscles and would not present with severe lactic acidosis and hyperlipidemia.
*Cori's disease*
- This is **Glycogen Storage Disease Type III**, caused by a deficiency in the **debranching enzyme** (amylo-alpha-1,6-glucosidase).
- While it can cause hepatomegaly and hypoglycemia, the hepatic glycogen structure would be abnormal due to incompletely debranched glycogen, and glucose-6-phosphatase levels would be normal.
*Hereditary hemochromatosis*
- This is an **iron overload disorder** leading to iron deposition in organs like the liver, heart, and pancreas.
- It would present with symptoms related to organ damage from iron accumulation, such as liver cirrhosis and diabetes, not the metabolic derangements seen here.
*McArdle disease*
- This is **Glycogen Storage Disease Type V**, due to a deficiency in **muscle glycogen phosphorylase**.
- It primarily causes exercise-induced muscle pain, cramping, and fatigue due to an inability to break down muscle glycogen for energy, not systemic metabolic disturbances or hepatomegaly.
Genetics and inheritance of GSDs US Medical PG Question 6: A 5-month-old boy presents with increasing weakness for the past 3 months. The patient’s mother says that the weakness is accompanied by dizziness, sweating, and vertigo early in the morning. Physical examination shows hepatomegaly. Laboratory findings show an increased amount of lactate, uric acid, and elevated triglyceride levels. Which of the following enzymes is most likely deficient in this patient?
- A. Hepatic glycogen phosphorylase
- B. Debranching enzyme
- C. Glucose-6-phosphatase (Correct Answer)
- D. Muscle glycogen phosphorylase
- E. Lysosomal α-1,4-glucosidase
Genetics and inheritance of GSDs Explanation: ***Glucose-6-phosphatase***
- The constellation of **hypoglycemia** (weakness, dizziness, sweating, vertigo, especially early morning), **hepatomegaly**, **lactic acidosis**, **hyperuricemia**, and **hypertriglyceridemia** are classic features of **Type I glycogen storage disease (von Gierke disease)**, which is caused by a deficiency of **glucose-6-phosphatase**.
- This enzyme is crucial for the final step of both **glycogenolysis** and **gluconeogenesis**, releasing free glucose into the bloodstream; its deficiency leads to an inability to maintain normal blood glucose levels during fasting and accumulation of glucose-6-phosphate, which shunts into other metabolic pathways.
*Hepatic glycogen phosphorylase*
- Deficiency in **hepatic glycogen phosphorylase** (Type VI glycogen storage disease, Hers disease) would cause **hepatomegaly** and **hypoglycemia**, but typically does not present with severe **lactic acidosis**, **hyperuricemia**, or **hypertriglyceridemia** to the same degree as von Gierke disease.
- The primary defect is in breaking down glycogen, leading to its accumulation in the liver, but the products of glycolysis can still exit the liver via gluconeogenesis.
*Debranching enzyme*
- Deficiency in **debranching enzyme** (Type III glycogen storage disease, Cori or Forbes disease) causes **hepatomegaly** and **hypoglycemia**, but usually presents with milder symptoms and less severe **lactic acidosis**, **hyperuricemia**, and **hypertriglyceridemia**.
- Patients often present with symptoms similar to Type I, but muscle involvement is also common, and **glycogen structures with short outer branches** are characteristic.
*Muscle glycogen phosphorylase*
- Deficiency in **muscle glycogen phosphorylase** (Type V glycogen storage disease, McArdle disease) primarily affects **skeletal muscle**, leading to exercise intolerance, muscle pain, and myoglobinuria.
- It does not typically cause **hypoglycemia** or **hepatomegaly**, as the liver enzyme is functional, and the symptoms described are systemic rather than muscle-specific.
*Lysosomal α-1,4-glucosidase*
- Deficiency in **lysosomal α-1,4-glucosidase** (Type II glycogen storage disease, Pompe disease) primarily affects the **heart, muscle, and liver**, causing severe **cardiomyopathy**, hypotonia, and **hepatomegaly**.
- While it involves glycogen accumulation, it typically does not present with **hypoglycemia** (as cytoplasmic glycogen metabolism is intact), **lactic acidosis**, or the specific metabolic derangements seen in this patient.
Genetics and inheritance of GSDs US Medical PG Question 7: A newborn infant presents with severe weakness. He was born to a G1P1 mother at 40 weeks gestation with the pregnancy attended by a midwife. The mother's past medical history is unremarkable. She took a prenatal vitamin and folic acid throughout the pregnancy. Since birth, the child has had trouble breastfeeding despite proper counseling. He also has had poor muscle tone and a weak cry. His temperature is 99.5°F (37.5°C), blood pressure is 57/38 mmHg, pulse is 150/min, respirations are 37/min, and oxygen saturation is 96% on room air. Physical exam reveals poor muscle tone. The patient's sucking reflex is weak, and an enlarged tongue is noted. An ultrasound is performed, and is notable for hypertrophy of the myocardium. Which of the following is the most likely diagnosis?
- A. Acid maltase deficiency (Correct Answer)
- B. Familial hypertrophic cardiomyopathy
- C. Clostridium tetani infection
- D. Spinal muscular atrophy type I disease
- E. Clostridium botulinum infection
Genetics and inheritance of GSDs Explanation: ***Acid maltase deficiency***
- This condition is also known as **Pompe disease**. It is a **lysosomal storage disease** that presents in infancy with **cardiomegaly**, **macroglossia**, **hypotonia**, and **respiratory failure**, all of which are consistent with the patient's presentation.
- The deficiency in **acid alpha-glucosidase (acid maltase)** leads to glycogen accumulation in lysosomes, particularly in muscle cells, causing impaired muscle function, including the heart.
*Familial hypertrophic cardiomyopathy*
- While it causes **myocardial hypertrophy**, it typically does **not present with profound generalized hypotonia, macroglossia, or feeding difficulties** as the primary symptoms in infancy.
- This condition is usually due to **sarcomeric protein mutations** and lacks the widespread systemic muscle involvement seen in Pompe disease.
*Clostridium tetani infection*
- This infection causes **tetanus**, characterized by **severe muscle spasms, trismus (lockjaw), and opisthotonus**, rather than hypotonia and weakness.
- It would also typically involve a history of a **puncture wound or contaminated injury**, which is not mentioned.
*Spinal muscular atrophy type I disease*
- This is characterized by **severe hypotonia** and **muscle weakness** due to the degeneration of anterior horn cells.
- However, **cardiomegaly and macroglossia are not typical features** of spinal muscular atrophy.
*Clostridium botulinum infection*
- This infection causes **flaccid paralysis** and weakness, usually presenting with **constipation**, **weak cry**, and **difficulty feeding**, by preventing acetylcholine release at neuromuscular junctions.
- However, **cardiomyopathy and macroglossia are not characteristic** of botulism.
Genetics and inheritance of GSDs US Medical PG Question 8: A 15-year-old boy comes to the physician because of severe muscle cramps and pain for 3 months. He first noticed these symptoms while attending tryouts for the high school football team. Since then, he becomes easily fatigued and has severe muscle pain and swelling after 10 minutes of playing. However, after a brief period of rest, the symptoms improve, and he is able to return to the game. Two days ago, he had an episode of reddish-brown urine after playing football. There is no family history of serious illness. He appears healthy. Vital signs are within normal limits. Physical and neurological examinations show no abnormalities. Serum creatine kinase concentration is 333 U/L. Urinalysis shows:
Blood 2+
Protein negative
Glucose negative
RBC negative
WBC 1–2/hpf
Which of the following is the most likely cause of this patient's symptoms?
- A. CTG repeat in the DMPK gene
- B. Myophosphorylase deficiency (Correct Answer)
- C. Dystrophin gene mutation
- D. Thyroid hormone deficiency
- E. Acid maltase deficiency
Genetics and inheritance of GSDs Explanation: ***Myophosphorylase deficiency***
- This condition (also known as **McArdle disease**) presents with **exercise-induced muscle cramps, pain, and fatigue** immediately after initiating activity, with a "second wind" phenomenon where symptoms improve after resting.
- The elevated **creatine kinase** and **reddish-brown urine** (indicating **myoglobinuria** due to rhabdomyolysis) are classic findings after strenuous activity in this glycogen storage disorder.
*CTG repeat in the DMPK gene*
- This describes **myotonic dystrophy type 1**, which presents with **myotonia** (delayed muscle relaxation), muscle weakness, and often involves multiple organ systems.
- While it causes muscle weakness, it does not typically present with acute, exercise-induced pain, cramping, and rhabdomyolysis in this manner.
*Dystrophin gene mutation*
- This is characteristic of **Duchenne or Becker muscular dystrophy**, which are progressive muscle weakness disorders.
- They typically cause **progressive proximal muscle weakness** and atrophy, not acute, intermittent, exercise-induced pain and cramping with a "second wind" phenomenon.
*Thyroid hormone deficiency*
- **Hypothyroidism** can cause muscle cramps, weakness, and elevated creatine kinase, but these symptoms are usually chronic and progressive, not acutely exercise-induced with improvement after a short rest.
- It would also present with other systemic symptoms like fatigue, weight gain, and cold intolerance, which are not described.
*Acid maltase deficiency*
- Also known as **Pompe disease**, this is a glycogen storage disorder that primarily affects infants and can present in adults with **proximal muscle weakness**, respiratory insufficiency, and cardiac involvement.
- It does not typically present with acute, exercise-induced muscle cramps, pain, and rhabdomyolysis followed by a "second wind" phenomenon like McArdle disease.
Genetics and inheritance of GSDs US Medical PG Question 9: A 16-year-old boy comes to the physician because of muscle weakness and cramps for 5 months. He becomes easily fatigued and has severe muscle pain and swelling after 15 minutes of playing basketball with his friends. The symptoms improve after a brief period of rest. After playing, he sometimes also has episodes of reddish-brown urine. There is no family history of serious illness. Serum creatine kinase concentration is 950 U/L. Urinalysis shows:
Blood 2+
Protein negative
Glucose negative
RBC negative
WBC 1–2/hpf
Which of the following is the most likely underlying cause of this patient's symptoms?
- A. Medium-chain acyl-CoA dehydrogenase deficiency
- B. Myophosphorylase deficiency (Correct Answer)
- C. Low levels of triiodothyronine and thyroxine
- D. Acid maltase deficiency
- E. CTG repeat in the DMPK gene
Genetics and inheritance of GSDs Explanation: ***Myophosphorylase deficiency***
- This condition (McArdle disease) is an **autosomal recessive disorder** of glycogen metabolism characterized by a defect in **glycogenolysis**, specifically the breakdown of muscle glycogen. This leads to impaired energy production during exercise.
- The classic presentation includes **exercise-induced muscle pain, stiffness, cramps, fatigue**, and sometimes **myoglobinuria** (reddish-brown urine due to myoglobin release from damaged muscle), which is consistent with the patient's symptoms and elevated **creatine kinase**.
*Medium-chain acyl-CoA dehydrogenase deficiency*
- This is a disorder of **fatty acid oxidation** that primarily affects the liver, leading to episodes of **hypoketotic hypoglycemia** during fasting or illness.
- It does not typically present with isolated exercise-induced muscle pain and myoglobinuria.
*Low levels of triiodothyronine and thyroxine*
- **Hypothyroidism** can cause generalized muscle weakness, fatigue, and muscle cramps, but it is usually associated with other systemic symptoms like weight gain, cold intolerance, and constipation.
- While it can cause elevated CK, it generally does not present with acute, exercise-induced muscle pain and myoglobinuria in the manner described.
*Acid maltase deficiency*
- This (Pompe disease) is a lysosomal storage disorder affecting glycogen metabolism, but it results from a deficiency of **acid alpha-glucosidase (acid maltase)**.
- The infantile form presents with severe hypotonia and cardiomyopathy, while the juvenile and adult forms typically cause **proximal muscle weakness** and respiratory insufficiency, rather than exercise-induced muscle pain and myoglobinuria.
*CTG repeat in the DMPK gene*
- This genetic defect is associated with **myotonic dystrophy type 1 (Steinert disease)**, an autosomal dominant disorder.
- Key features include **myotonia** (delayed relaxation of muscles), muscle weakness, cataracts, and cardiac conduction abnormalities, which are distinct from the patient's presentation of exercise-induced cramps and myoglobinuria without myotonia.
Genetics and inheritance of GSDs US Medical PG Question 10: A 1-year-old male with a history of recurrent pseudomonal respiratory infections and steatorrhea presents to the pediatrician for a sweat test. The results demonstrate a chloride concentration of 70 mEq/L (nl < 40 mEq/L). Which of the following defects has a similar AUTOSOMAL RECESSIVE mode of inheritance as the disorder experienced by this patient?
- A. Abnormal production of type IV collagen
- B. Trinucleotide repeat expansion of CAG on chromosome 4
- C. Mutated gene for mitochondrial-tRNA-Lys
- D. Accumulation of glycogen in the lysosome (Correct Answer)
- E. Inability to convert carbamoyl phosphate and ornithine into citrulline
Genetics and inheritance of GSDs Explanation: ***Accumulation of glycogen in the lysosome***
- The patient's symptoms (recurrent **pseudomonal respiratory infections**, **steatorrhea**, and elevated sweat chloride) are classic for **cystic fibrosis (CF)**, an **autosomal recessive** disorder.
- Accumulation of glycogen in the lysosome describes **Pompe disease (Type II Glycogen Storage Disease)**, which is also an **autosomal recessive** disorder, making this the correct answer.
*Abnormal production of type IV collagen*
- This defect is characteristic of **Alport syndrome**, which is predominantly **X-linked dominant** (~80-85% of cases), though autosomal recessive forms exist.
- The question context and typical board exam framing classify this as X-linked, not autosomal recessive.
- Alport syndrome primarily affects the kidneys, ears, and eyes, and does not present with recurrent pseudomonal infections or steatorrhea.
*Trinucleotide repeat expansion of CAG on chromosome 4*
- This genetic defect is responsible for **Huntington's disease**, which is an **autosomal dominant** neurodegenerative disorder.
- Huntington's disease presents with chorea, cognitive decline, and psychiatric symptoms, which are distinct from CF.
*Mutated gene for mitochondrial-tRNA-Lys*
- A mutated gene for mitochondrial-tRNA-Lys is associated with **MELAS syndrome (Mitochondrial Encephalomyopathy, Lactic Acidosis, and Stroke-like episodes)**, which is inherited through **maternal (mitochondrial)** inheritance.
- This mode of inheritance is distinct from the autosomal recessive pattern seen in cystic fibrosis.
*Inability to convert carbamoyl phosphate and ornithine into citrulline*
- This describes a defect in **ornithine transcarbamylase (OTC) deficiency**, an **X-linked recessive** disorder, not autosomal recessive.
- OTC deficiency leads to hyperammonemia and metabolic disturbances, without the pulmonary and gastrointestinal symptoms typical of cystic fibrosis.
More Genetics and inheritance of GSDs US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.