Sulfur-containing amino acid metabolism US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Sulfur-containing amino acid metabolism. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Sulfur-containing amino acid metabolism US Medical PG Question 1: A 21-year-old man presents to the emergency department with acute back pain. The pain began a few hours prior to presentation and is located on the left lower back. The pain is described to be “shock-like,” 9/10 in pain severity, and radiates to the left groin. His temperature is 98.6°F (37°C), blood pressure is 120/75 mmHg, pulse is 101/min, and respirations are 18/min. The patient appears uncomfortable and is mildly diaphoretic. There is costovertebral angle tenderness and genitourinary exam is unremarkable. A non-contrast computerized tomography (CT) scan of the abdomen and pelvis demonstrates an opaque lesion affecting the left ureter with mild hydronephrosis. Straining of the urine with urine crystal analysis is demonstrated. Which of the following amino acids is most likely poorly reabsorbed by this patient’s kidney?
- A. Isoleucine
- B. Aspartic acid
- C. Phenylalanine
- D. Lysine (Correct Answer)
- E. Histidine
Sulfur-containing amino acid metabolism Explanation:
***Lysine***
- The patient's symptoms (acute, severe, radiating back pain, CVA tenderness, hydronephrosis, and opaque lesion on CT) are highly characteristic of a **kidney stone**.
- Given the patient's young age and the nature of the amino acid question, thinking of **cystinuria** is appropriate, where the basic amino acids **COLA** (cystine, ornithine, lysine, arginine) are poorly reabsorbed.
*Isoleucine*
- **Isoleucine** is a branched-chain amino acid, not one of the basic amino acids impacted by cystinuria.
- Its malabsorption is not associated with the formation of kidney stones.
*Aspartic acid*
- **Aspartic acid** is an acidic amino acid and is not involved in the transport defects seen in cystinuria.
- There is no direct link between aspartic acid malabsorption and kidney stone formation.
*Phenylalanine*
- **Phenylalanine** is an aromatic amino acid and its metabolism is associated with disorders like phenylketonuria, not kidney stones.
- It is not one of the amino acids whose renal reabsorption is impaired in cystinuria.
*Histidine*
- **Histidine** is an essential amino acid, but it is not one of the basic amino acids (COLA) whose transport is affected in cystinuria.
- Poor reabsorption of histidine is not typically associated with kidney stone formation.
Sulfur-containing amino acid metabolism US Medical PG Question 2: A 35-year-old woman comes to the physician because of a 1-day history of swelling and pain in the left leg. Two days ago, she returned from a business trip on a long-distance flight. She has alcohol use disorder. Physical examination shows a tender, swollen, and warm left calf. Serum studies show an increased homocysteine concentration and a methylmalonic acid concentration within the reference range. Further evaluation of this patient is most likely to show which of the following serum findings?
- A. Decreased cobalamin concentration
- B. Decreased protein C concentration
- C. Increased fibrinogen concentration
- D. Decreased folate concentration (Correct Answer)
- E. Increased pyridoxine concentration
Sulfur-containing amino acid metabolism Explanation: ***Decreased folate concentration***
- The patient's presentation with **pain and swelling in the left leg following a long flight** suggests a **deep vein thrombosis (DVT)**. Increased homocysteine levels are a risk factor for DVT.
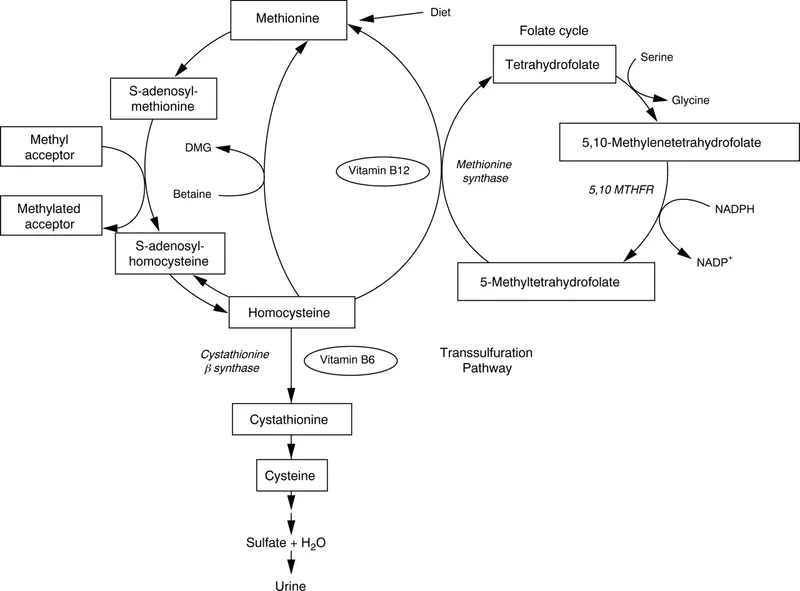
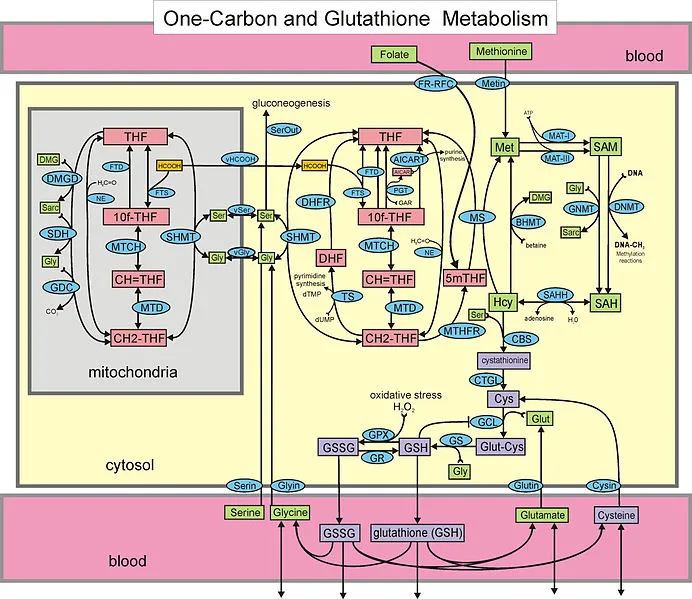
- Alcohol use disorder often leads to **malabsorption and poor nutritional intake**, profoundly affecting **folate metabolism** and leading to **folate deficiency**. This deficiency is a common cause of **hyperhomocysteinemia**, especially when methylmalonic acid levels are normal (ruling out B12 deficiency as the primary cause of hyperhomocysteinemia).
*Decreased cobalamin concentration*
- While alcohol use disorder can decrease **cobalamin (vitamin B12) concentration**, the **normal methylmalonic acid (MMA) concentration** in this patient makes a significant B12 deficiency unlikely to be the cause of the elevated homocysteine.
- Elevated MMA is a more specific indicator of **cobalamin deficiency**, as B12 is a cofactor for the enzyme that converts methylmalonyl-CoA to succinyl-CoA.
*Decreased protein C concentration*
- Decreased protein C concentration is a **thrombophilic condition** that increases the risk of DVT, but there is no direct evidence in the patient's history or lab results pointing specifically to this deficiency.
- While hereditary thrombophilias can contribute, a **primary nutritional deficiency** explains the constellation of findings better in this context.
*Increased fibrinogen concentration*
- **Fibrinogen** is an **acute-phase reactant** and would likely be elevated in the context of inflammation or thrombosis, but it is not directly linked to the patient's hyperhomocysteinemia due to alcohol use disorder.
- Elevated fibrinogen is a **consequence** of the thrombotic process, not typically a direct cause of the hyperhomocysteinemia in this scenario.
*Increased pyridoxine concentration*
- **Pyridoxine (vitamin B6) levels** are generally not increased in individuals with alcohol use disorder; in fact, chronic alcohol abuse can lead to **pyridoxine deficiency**.
- Pyridoxine is a cofactor in homocysteine metabolism, and deficiency can lead to elevated homocysteine, but an *increase* is not expected.
Sulfur-containing amino acid metabolism US Medical PG Question 3: A 48-year-old woman is brought to the emergency department by police because of confusion and agitation. Her medical record indicates that she has peptic ulcer disease that is treated with omeprazole. The patient's brother arrives shortly after. He reports that she drinks around 17 oz. of vodka daily. Neurological examination shows horizontal nystagmus. Her gait is wide-based with small steps. Her hemoglobin concentration is 9.1 g/dL. A peripheral blood smear shows hypersegmented neutrophils. Homocysteine levels are elevated. Methylmalonic acid levels are within normal limits. Which of the following is the most likely direct cause of this patient's anemia?
- A. Vitamin E deficiency
- B. Vitamin B1 deficiency
- C. Folate deficiency (Correct Answer)
- D. Vitamin B12 deficiency
- E. Alcohol toxicity
Sulfur-containing amino acid metabolism Explanation: ***Folate deficiency***
- The combination of **anemia**, **hypersegmented neutrophils**, elevated **homocysteine**, and *normal methylmalonic acid* levels strongly points to folate deficiency.
- **Alcoholism** is a significant risk factor for folate deficiency due to poor nutritional intake and impaired folate absorption and metabolism.
*Vitamin E deficiency*
- This deficiency typically causes **neurological dysfunction** and **hemolytic anemia**, but it does not lead to hypersegmented neutrophils or elevated homocysteine.
- It is often seen in conditions causing **fat malabsorption**, which is not explicitly indicated as the primary driver here.
*Vitamin B1 deficiency*
- **Thiamine (B1) deficiency** is associated with **Wernicke-Korsakoff syndrome**, characterized by confusion, nystagmus, and ataxia, which are present in this patient.
- Although alcohol abuse causes thiamine deficiency, it does not explain the **megaloblastic anemia** with hypersegmented neutrophils evident in the peripheral blood smear.
*Vitamin B12 deficiency*
- Vitamin B12 deficiency also causes **megaloblastic anemia** and elevated **homocysteine** levels, but it would also present with **elevated methylmalonic acid (MMA)** levels, which are explicitly stated as normal here.
- The patient's use of omeprazole (a proton pump inhibitor) can contribute to B12 deficiency over time by reducing gastric acid necessary for B12 release from food proteins, but the MMA levels rule it out as the *direct cause* of anemia in this specific instance.
*Alcohol toxicity*
- While chronic alcohol abuse can lead to **anemia** through various mechanisms, including **bone marrow suppression** or **gastrointestinal bleeding**, it does not directly explain the specific findings of **hypersegmented neutrophils** and the particular pattern of homocysteine and methylmalonic acid levels.
- Alcohol toxicity is an underlying cause for other deficiencies, but not the direct cause of this specific type of anemia.
Sulfur-containing amino acid metabolism US Medical PG Question 4: A 45-year-old woman presents with severe, acute-onset colicky abdominal pain and nausea. She also describes bone pain, constipation, headache, decreased vision, and menstrual irregularity. Past medical history is significant for surgical removal of an insulinoma one year ago. Two months ago, she was prescribed fluoxetine for depression but hasn’t found it very helpful. Family history is significant for a rare genetic syndrome. Non-contrast CT, CBC, CMP, and urinalysis are ordered in the diagnostic work-up. Urine sediment is significant for the findings shown in the picture. Which of the following will also be a likely significant finding in the diagnostic workup?
- A. Decreased urine pH (Correct Answer)
- B. Hypokalemia and non-anion gap acidosis
- C. Diagnosis confirmed with cyanide-nitroprusside test
- D. Elevated hemoglobin on CBC with significantly low levels of EPO
- E. Imaging demonstrates staghorn calculi
Sulfur-containing amino acid metabolism Explanation: ***Decreased urine pH***
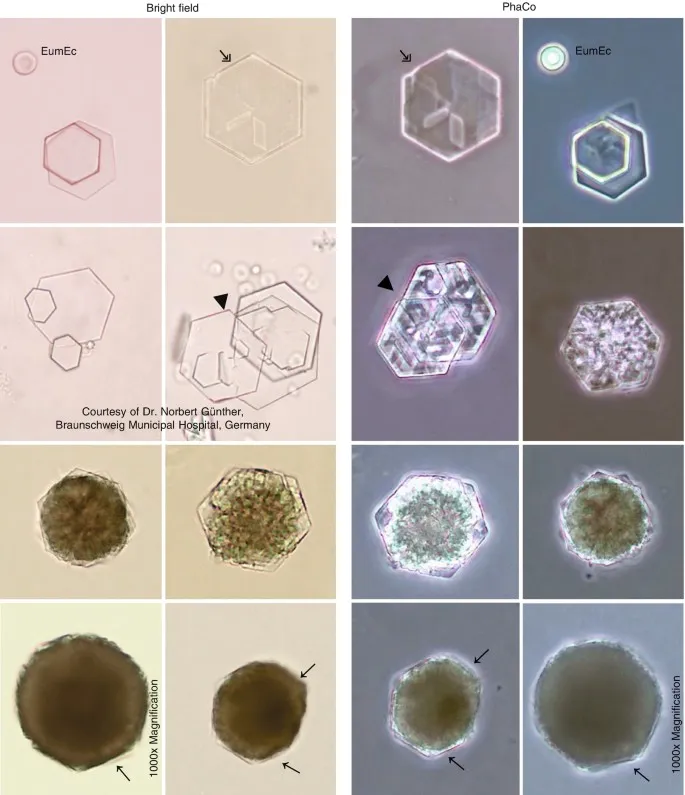
- The urine sediment shows **uric acid crystals** (rhomboid or rosette-shaped), which are pathognomonic for acidic urine.
- Uric acid stones form when **urine pH < 5.5**, as uric acid is insoluble in acidic conditions.
- This patient's complex presentation with history of insulinoma and family history of rare genetic syndrome suggests **MEN1 (Multiple Endocrine Neoplasia Type 1)**, which includes parathyroid adenomas, pancreatic tumors, and pituitary tumors.
- The symptoms of bone pain, abdominal pain, constipation, and neurological changes ("stones, bones, abdominal groans, psychiatric moans") suggest **hypercalcemia from primary hyperparathyroidism**.
- While calcium stones (not uric acid) are more common in hypercalcemia, the image specifically shows uric acid crystals, making decreased urine pH the most relevant finding in this diagnostic workup.
*Hypokalemia and non-anion gap acidosis*
- This constellation is characteristic of **Type 1 (distal) renal tubular acidosis**.
- While RTA can predispose to kidney stones (typically calcium phosphate in alkaline urine), it does not match the uric acid crystals shown in the image.
- The patient's symptoms are more consistent with hypercalcemia from MEN1 rather than RTA.
*Diagnosis confirmed with cyanide-nitroprusside test*
- The **cyanide-nitroprusside test** detects elevated cystine levels and is used to diagnose **cystinuria**.
- However, the image shows **uric acid crystals**, not hexagonal cystine crystals.
- This test would not be relevant to the current clinical picture.
*Elevated hemoglobin on CBC with significantly low levels of EPO*
- This suggests **polycythemia vera** or primary polycythemia, a myeloproliferative disorder.
- While some MEN syndromes can have associated findings, this is unrelated to the uric acid crystals and the primary presentation.
- There is no indication of polycythemia in this patient's presentation.
*Imaging demonstrates staghorn calculi*
- **Staghorn calculi** are typically **struvite stones** caused by urease-producing bacteria (e.g., *Proteus*) in **alkaline urine** with urinary tract infections.
- The image shows **uric acid crystals**, which form in acidic urine and typically produce small stones, not staghorn calculi.
- Staghorn calculi are inconsistent with the presented urine sediment findings.
Sulfur-containing amino acid metabolism US Medical PG Question 5: A 17-year-old girl is brought in by her mother due to rapid weight loss over the past month. The patient says she has been having episodes of diarrhea, which she attributes to laxatives she takes regularly to keep her weight down. She also says she has not had her period yet. The patient’s mother adds that the patient has been underperforming at school and acting very strangely at home. Her current BMI is 16.8 kg/m2. On physical examination, the skin on her limbs and around her neck is inflamed and erythematous. Her tongue is bright red and smooth. She states that over the last 2 weeks, she has been eating nothing but small portions of fruit. She is diagnosed with a vitamin deficiency. Which of the following statements is true about the vitamin most likely deficient in this patient?
- A. It increases the GI absorption of iron
- B. It is derived from tyrosine
- C. Synthesis requires vitamin B2 and B6 (Correct Answer)
- D. Synthesis requires vitamin B1 and B6
- E. It is used to treat hypertension
Sulfur-containing amino acid metabolism Explanation: ***Synthesis requires vitamin B2 and B6***
- The patient's symptoms (diarrhea, dermatitis, dementia-like behavior, glossitis, and weight loss) are classic for **pellagra**, which is caused by a deficiency in **niacin (vitamin B3)**.
- The synthesis of **niacin** from **tryptophan** requires **pyridoxine (vitamin B6)** and **riboflavin (vitamin B2)** as cofactors.
*It increases the GI absorption of iron*
- **Vitamin C** (ascorbic acid) enhances the **gastrointestinal absorption of non-heme iron** by reducing ferric iron to its ferrous form.
- Niacin does not play a direct role in the absorption of iron.
*It is derived from tyrosine*
- **Tyrosine** is a precursor to several important compounds, including **catecholamines** (dopamine, norepinephrine, epinephrine) and **thyroid hormones**.
- **Niacin** is predominantly synthesized from the essential amino acid **tryptophan**.
*Synthesis requires vitamin B1 and B6*
- While **vitamin B6** is essential for niacin synthesis from tryptophan, **vitamin B1 (thiamine)** is not directly involved in this pathway.
- Thiamine's primary role is in carbohydrate metabolism.
*It is used to treat hypertension*
- While **niacin** can affect lipid profiles, it is **not commonly used as a primary treatment for hypertension**.
- **Niacin** is used, primarily in pharmacologic doses, to **lower LDL cholesterol** and **triglycerides** and **raise HDL cholesterol**, often in conjunction with other lipid-lowering agents.
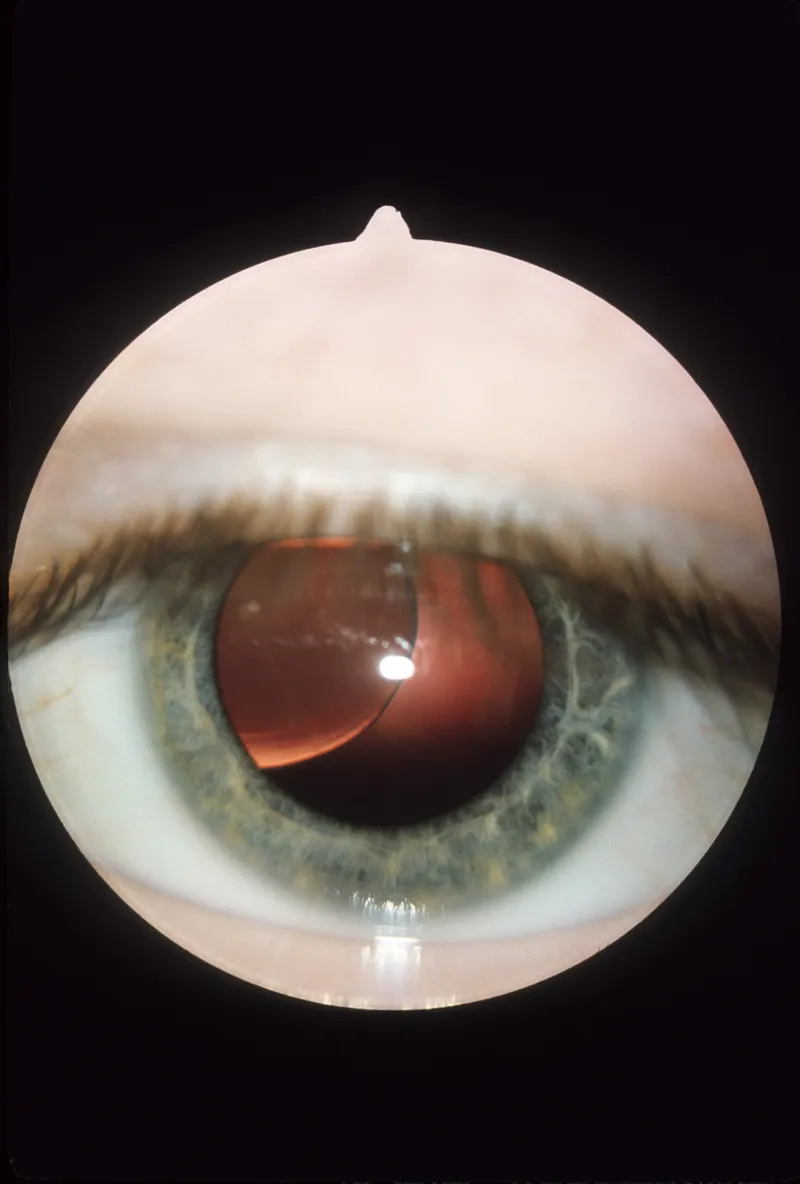
Sulfur-containing amino acid metabolism US Medical PG Question 6: A 4-year-old boy presents to the ophthalmologist for a down- and inward dislocation of the lens in his left eye. On physical exam, the boy has a marfanoid habitus and intellectual disability. Biochemical tests were performed to locate the exact defect in this boy. It was found that there was a significant deficiency in cystathionine beta-synthase activity with elevated homocysteine levels. Which of the following is the diagnosis?
- A. Marfan syndrome
- B. Homocystinuria (Correct Answer)
- C. Alkaptonuria
- D. Phenylketonuria
- E. Maple syrup urine disease
Sulfur-containing amino acid metabolism Explanation: ***Homocystinuria***
- The combination of **ectopia lentis** (lens dislocation), **marfanoid habitus**, and **intellectual disability** is characteristic of homocystinuria.
- The **deficiency in cystathionine beta-synthase** leading to **elevated homocysteine levels** is the biochemical hallmark of this disorder.
*Marfan syndrome*
- While it presents with **marfanoid habitus** and **ectopia lentis**, the lens dislocation is typically **upward and outward**, unlike the down- and inward dislocation seen here.
- Marfan syndrome is caused by a defect in **fibrillin-1**, and biochemical tests would not show elevated homocysteine.
*Alkaptonuria*
- This disorder is characterized by **dark urine** upon standing, **ochronosis** (darkening of cartilage and connective tissue), and **arthropathy**.
- It results from a deficiency in **homogentisate oxidase** and does not present with lens dislocation or intellectual disability.
*Phenylketonuria*
- PKU is caused by a deficiency in **phenylalanine hydroxylase**, leading to an accumulation of phenylalanine.
- It primarily causes **severe intellectual disability**, seizures, and a musty odor, but not ectopia lentis or marfanoid habitus.
*Maple syrup urine disease*
- This is a metabolic disorder affecting the metabolism of **branched-chain amino acids** (leucine, isoleucine, valine).
- It presents with a characteristic **maple syrup odor** in urine, poor feeding, lethargy, and developmental delay, but not the specific features seen in this case.
Sulfur-containing amino acid metabolism US Medical PG Question 7: A 38-year-old, working, first-time mother brings her 9-month-old male infant to the pediatrician for "wounds that simply won't heal" and bleeding gums. She exclaims, "I have been extra careful with him making sure to not let him get dirty, I boil his baby formula for 15 minutes each morning before I leave for work to give to the caregiver, and he has gotten all of his vaccinations." This infant is deficient in a molecule that is also an essential co-factor for which of the following reactions?
- A. Conversion of homocysteine to methionine
- B. Conversion of alpha ketoglutarate to succinyl-CoA
- C. Conversion of dopamine to norepinephrine (Correct Answer)
- D. Conversion of pyruvate to acetyl-CoA
- E. Conversion of pyruvate to oxaloacetate
Sulfur-containing amino acid metabolism Explanation: ***Conversion of dopamine to norepinephrine***
- The infant's symptoms of "wounds that simply won't heal" and **bleeding gums** are classic signs of **scurvy**, caused by a deficiency in **vitamin C (ascorbic acid)**.
- **Vitamin C** is an essential cofactor for **dopamine beta-hydroxylase**, the enzyme responsible for converting **dopamine to norepinephrine**.
*Conversion of homocysteine to methionine*
- This reaction is catalyzed by **methionine synthase**, which requires **vitamin B12** (cobalamin) and **folate (vitamin B9)** as cofactors.
- Deficiency in these vitamins would lead to **megaloblastic anemia** and neurological symptoms, not delayed wound healing and bleeding gums.
*Conversion of alpha ketoglutarate to succinyl-CoA*
- This step in the **Krebs cycle** is catalyzed by **alpha-ketoglutarate dehydrogenase**, which requires **thiamine (vitamin B1)**, **lipoic acid**, **Mg2+**, **NAD+**, and **FAD** as cofactors.
- Thiamine deficiency can cause **beriberi** or **Wernicke-Korsakoff syndrome**, not scurvy symptoms.
*Conversion of pyruvate to acetyl-CoA*
- This reaction is catalyzed by the **pyruvate dehydrogenase complex**, which requires **thiamine (vitamin B1)**, **lipoic acid**, **coenzyme A**, **FAD**, and **NAD+** as cofactors.
- A deficiency in any of these, particularly thiamine, leads to impaired carbohydrate metabolism and lactic acidosis.
*Conversion of pyruvate to oxaloacetate*
- This reaction is catalyzed by **pyruvate carboxylase**, which requires **biotin (vitamin B7)** as a cofactor and is essential for **gluconeogenesis**.
- Biotin deficiency is rare and can present with dermatitis, hair loss, and neurological symptoms, not the classic signs of scurvy.
Sulfur-containing amino acid metabolism US Medical PG Question 8: A 9-month-old infant presents to your office for a check-up. Exam reveals developmental delay, microcephaly, and a mousy odor to his breath. You should be concerned that the infant may have which of the following?
- A. Excess tetrahydrobiopterin cofactor
- B. Deficit of porphobilinogen deaminase activity
- C. Deficit of tyrosine hydroxylase activity
- D. Excess phenylalanine hydroxylase activity
- E. Deficit of phenylalanine hydroxylase activity (Correct Answer)
Sulfur-containing amino acid metabolism Explanation: ***Deficit of phenylalanine hydroxylase activity***
- The combination of **developmental delay**, **microcephaly**, and a **mousy odor** is characteristic of **phenylketonuria (PKU)**.
- PKU is caused by a deficient **phenylalanine hydroxylase** enzyme, leading to a buildup of phenylalanine and its metabolites, which are toxic to the developing brain.
*Excess tetrahydrobiopterin cofactor*
- This condition (**BH4 excess**) is rare and does not typically present with the classic signs of PKU; rather, it often involves neurological symptoms due to other metabolic imbalances.
- An excess of the BH4 cofactor would theoretically enhance rather than inhibit phenylalanine hydroxylase activity, if the enzyme itself were functional.
*Deficit of porphobilinogen deaminase activity*
- A deficit in **porphobilinogen deaminase** is associated with **Acute Intermittent Porphyria (AIP)**, which presents with acute neurovisceral attacks.
- Symptoms of AIP include severe abdominal pain, psychiatric disturbances, and neurological deficits, but not developmental delay or a mousy odor.
*Deficit of tyrosine hydroxylase activity*
- A deficiency in **tyrosine hydroxylase** affects the synthesis of **dopamine** and other catecholamines, leading to neurological disorders, including **dystonia** and **Parkinsonian symptoms**.
- While it can cause developmental delay, it does not typically present with a mousy odor or microcephaly, and its primary symptoms relate to motor control.
*Excess phenylalanine hydroxylase activity*
- An **excess** of phenylalanine hydroxylase activity would lead to increased breakdown of phenylalanine, preventing its buildup.
- This would not cause the symptoms described; instead, it would likely result in lower-than-normal phenylalanine levels, which is generally not problematic.
Sulfur-containing amino acid metabolism US Medical PG Question 9: An 8-day-old boy is brought to the physician by his mother because of vomiting and poor feeding. The pregnancy was uncomplicated, and he was born at full term. He appears pale and lethargic. Physical examination shows diffusely increased muscle tone. His urine is noted to have a sweet odor. This patient's symptoms are most likely caused by the accumulation of which of the following?
- A. Phenylalanine
- B. Homogentisic acid
- C. Isoleucine (Correct Answer)
- D. Homocysteine
- E. Phytanic acid
Sulfur-containing amino acid metabolism Explanation: ***Isoleucine***
- The combination of **vomiting**, poor feeding, lethargy, **increased muscle tone**, and a **sweet-smelling urine** (often described as maple syrup odor) in a neonate strongly points to **Maple Syrup Urine Disease (MSUD)**.
- MSUD is caused by a defect in the **branched-chain alpha-keto acid dehydrogenase complex**, leading to the accumulation of branched-chain amino acids (leucine, isoleucine, and valine) and their corresponding alpha-keto acids.
*Phenylalanine*
- Accumulation of **phenylalanine** is characteristic of **Phenylketonuria (PKU)**, which typically presents with intellectual disability, seizures, and an eczematous rash if untreated, but not a maple syrup odor in urine or acute neonatal crisis.
- The urine odor in PKU is often described as **mousy** or musty, distinctly different from a sweet or maple syrup odor.
*Homogentisic acid*
- Accumulation of **homogentisic acid** is seen in **Alkaptonuria**, an inborn error of metabolism that primarily causes dark urine upon standing (due to oxidation of homogentisic acid), ochronosis (blue-black pigmentation of cartilage and connective tissue later in life), and arthritis.
- It does not present with acute neonatal symptoms such as vomiting, lethargy, or a sweet urine odor.
*Homocysteine*
- Elevated levels of **homocysteine** are found in **Homocystinuria**, which can lead to intellectual disability, developmental delay, dislocation of the ocular lens (ectopia lentis), Marfanoid habitus, and thromboembolic events.
- It does not typically present in the neonatal period with a sweet urine odor or acute neurological symptoms like increased muscle tone.
*Phytanic acid*
- Accumulation of **phytanic acid** is characteristic of **Refsum disease**, a rare peroxisomal disorder that causes progressive neurological symptoms such as retinitis pigmentosa, peripheral neuropathy, ataxia, and deafness in childhood or adulthood.
- It does not present in the neonatal period with the described acute symptoms or unique urine odor.
Sulfur-containing amino acid metabolism US Medical PG Question 10: A 5 year old child was brought to the physician with a history of black urine. There is no history of fever or any other complaints. There is no growth retardation and all the developmental milestones are normal. The child is suspected to have an enzyme defect for metabolism of an aromatic amino acid. What is the enzyme deficient
- A. Homogentisate dehydrogenase
- B. Homogentistae oxidase (Correct Answer)
- C. Tyrosine Transaminase
- D. Tryptophan Hydroxylase
- E. Phenylalanine Hydroxylase
Sulfur-containing amino acid metabolism Explanation: ***Homogentistae oxidase***
- The presentation of a child with **black urine** (alkaptonuria) in the absence of other symptoms is characteristic of a deficiency in **homogentisate oxidase**.
- This enzyme is crucial in the catabolism of **tyrosine**, and its deficiency leads to the accumulation of **homogentisic acid**, which oxidizes upon exposure to air, turning urine black.
*Homogentisate dehydrogenase*
- This enzyme is not a recognized component of the **tyrosine degradation pathway** in humans.
- The correct enzyme involved in the breakdown of **homogentisate** is an oxidase, not a dehydrogenase, in this context.
*Tyrosine Transaminase*
- A deficiency in **tyrosine transaminase** (tyrosinemia type II) would lead to elevated tyrosine levels and typically presents with symptoms affecting the eyes, skin, and intellectual disability, not primarily black urine.
- This condition is characterized by **ocular findings** (corneal ulcers), **skin lesions**, and **neurological symptoms**.
*Tryptophan Hydroxylase*
- This enzyme is involved in the synthesis of **serotonin** and **melatonin** from tryptophan, a different amino acid pathway.
- A deficiency or abnormality in **tryptophan hydroxylase** would not cause black urine but could lead to neurological or mood disorders.
*Phenylalanine Hydroxylase*
- A deficiency in **phenylalanine hydroxylase** causes **phenylketonuria (PKU)**, which affects phenylalanine metabolism, not tyrosine metabolism directly.
- PKU typically presents with **intellectual disability**, **musty odor**, **fair skin**, and **seizures** if untreated, not black urine.
More Sulfur-containing amino acid metabolism US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.