Glucogenic and ketogenic amino acids US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Glucogenic and ketogenic amino acids. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Glucogenic and ketogenic amino acids US Medical PG Question 1: Researchers are experimenting with hormone levels in mice in fasting and fed states. To test hormone levels in the fed state, the mice are given an oral glucose load and various hormones are measured in a blood sample. Researchers are most interested in the hormone whose blood levels track evenly with C-peptide levels. The hormone the researchers are most interested in is responsible for which of the following actions in the body?
- A. Protein catabolism
- B. Fatty acid breakdown
- C. Fatty acid synthesis (Correct Answer)
- D. Ketogenesis
- E. Lipolysis
Glucogenic and ketogenic amino acids Explanation: ***Fatty acid synthesis***
- The hormone whose blood levels track evenly with **C-peptide** levels after a glucose load is **insulin**.
- Insulin is a key anabolic hormone that promotes **fatty acid synthesis** from excess glucose in the fed state, particularly in the liver and adipose tissue.
*Protein catabolism*
- **Insulin** is an anabolic hormone that generally **inhibits protein catabolism** and promotes protein synthesis.
- Conditions like **glucagon excess** or **cortisol excess** promote protein catabolism, not insulin.
*Fatty acid breakdown*
- **Insulin inhibits fatty acid breakdown** (beta-oxidation) by suppressing hormone-sensitive lipase.
- **Glucagon** and **epinephrine** promote fatty acid breakdown, especially during fasting.
*Ketogenesis*
- **Insulin inhibits ketogenesis** by reducing the supply of fatty acids to the liver and inhibiting the enzymes involved in ketone body formation.
- **Glucagon** and **low insulin levels** (as in uncontrolled diabetes or prolonged fasting) promote ketogenesis.
*Lipolysis*
- **Insulin is a potent inhibitor of lipolysis** (breakdown of triglycerides into fatty acids and glycerol) in adipose tissue.
- **Glucagon**, **catecholamines**, and **growth hormone** stimulate lipolysis.
Glucogenic and ketogenic amino acids US Medical PG Question 2: A 4-day-old boy is brought to the physician by his mother because of vomiting, irritability, and poor feeding. Pregnancy and delivery were uncomplicated. Physical examination shows increased muscle tone in all extremities. He appears lethargic. His diapers emit a caramel-like odor. Urine studies are positive for ketone bodies. Supplementation of which of the following is most likely to improve this patient's condition?
- A. Tyrosine
- B. Cysteine
- C. Tetrahydrobiopterin
- D. Thiamine (Correct Answer)
- E. Leucine
Glucogenic and ketogenic amino acids Explanation: ***Thiamine***
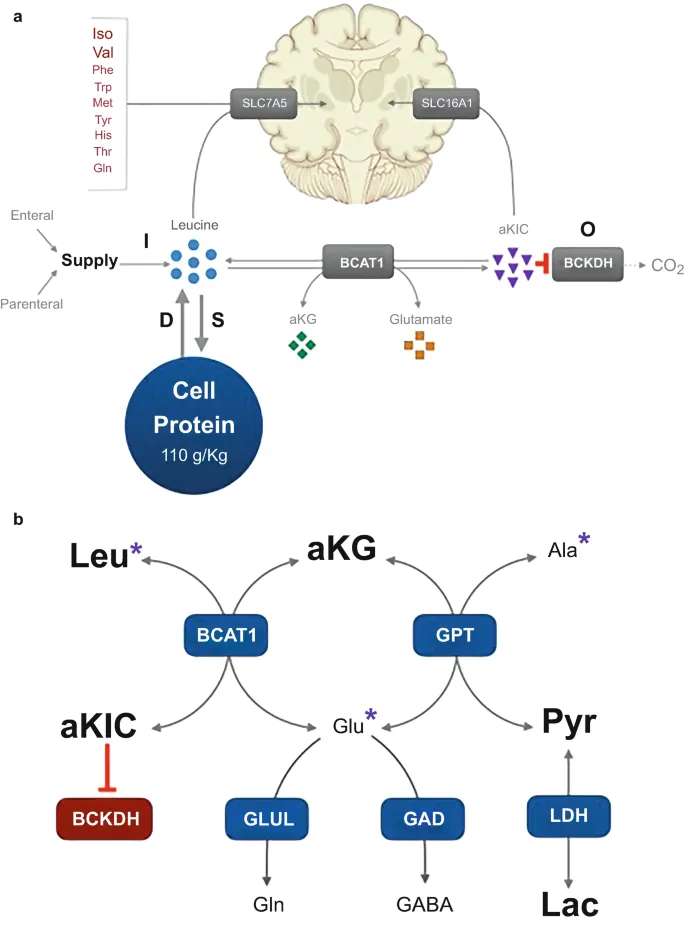
- This clinical scenario describes an infant with **vomiting, irritability, poor feeding, increased muscle tone, lethargy, and a caramel-like odor in the urine**, along with **ketone bodies in the urine**. These are classic signs of **Maple Syrup Urine Disease (MSUD)**.
- MSUD is caused by a deficiency in the **branched-chain alpha-keto acid dehydrogenase complex (BCKDC)**, an enzyme that requires **thiamine** as a cofactor. In some cases, high-dose thiamine supplementation can improve enzyme activity and alleviate symptoms.
*Tyrosine*
- **Tyrosine** is an amino acid. Disorders of tyrosine metabolism, such as tyrosinemia, present with liver dysfunction, renal tubulopathy, and neurological crises, but typically do not involve a caramel-like odor or respond to thiamine.
- Tyrosine supplementation is not indicated for MSUD and would not improve the patient's condition.
*Cysteine*
- **Cysteine** is a sulfur-containing amino acid. Disorders involving cysteine metabolism, like homocystinuria, are characterized by ocular, skeletal, vascular, and neurological abnormalities.
- There is no direct role for cysteine supplementation in treating MSUD, and it would not address the underlying enzymatic defect.
*Tetrahydrobiopterin*
- **Tetrahydrobiopterin (BH4)** is a cofactor for several enzymes involved in amino acid metabolism, particularly in the synthesis of neurotransmitters and the metabolism of phenylalanine.
- BH4 deficiency causes phenylketonuria-like symptoms or other neurological issues, but not MSUD, and it would not address the BCKDC deficiency.
*Leucine*
- **Leucine** is one of the branched-chain amino acids (BCAAs) that accumulate in MSUD due to the defective BCKDC enzyme.
- Supplementing leucine would worsen the patient's condition by increasing the toxic BCAA levels, as the body cannot properly metabolize it.
Glucogenic and ketogenic amino acids US Medical PG Question 3: A 20-year-old male is brought by ambulance to the emergency room in extremis. He is minimally conscious, hypotensive, and tachypneic, and his breath gives off a "fruity" odor. An arterial blood gas and metabolic panel show anion gap metabolic acidosis. This patient is most likely deficient in which of the following metabolic actions?
- A. Glucagon production
- B. Cortisol secretion
- C. Formation of ketone bodies
- D. Glucose production
- E. Cellular uptake of glucose (Correct Answer)
Glucogenic and ketogenic amino acids Explanation: ***Cellular uptake of glucose***
- The patient's symptoms, including **fruity odor breath**, **anion gap metabolic acidosis**, and being found in extremis, are classic signs of **diabetic ketoacidosis (DKA)**.
- DKA results from a profound lack of **insulin**, which is essential for cells (especially muscle and adipose tissue) to take up glucose from the bloodstream, leading to hyperglycemia and a shift to fat metabolism.
*Glucagon production*
- **Glucagon** is a counter-regulatory hormone that *raises* blood glucose levels, and its production is often *increased* in DKA as the body attempts to provide fuel to cells in the absence of insulin's effect.
- A deficiency in glucagon production would more likely lead to **hypoglycemia**, not the profound hyperglycemia seen in DKA.
*Cortisol secretion*
- **Cortisol** is another counter-regulatory hormone that *increases* blood glucose, and its secretion is typically *elevated* in stress states like DKA.
- A deficiency in cortisol (e.g., in adrenal insufficiency) would present with different symptoms such as **hypoglycemia**, **hyponatremia**, and **hyperkalemia**, without the classic DKA picture.
*Formation of ketone bodies*
- The patient's **fruity odor breath** and **anion gap metabolic acidosis** are direct consequences of the *overproduction* of **ketone bodies**.
- This overproduction occurs when the body, lacking glucose for fuel due to insulin deficiency, switches to **fat metabolism**, leading to excessive formation of acetoacetate, beta-hydroxybutyrate, and acetone.
*Glucose production*
- **Glucose production** (gluconeogenesis and glycogenolysis) is typically *increased* in DKA as the liver tries to supply glucose to the body due to perceived cellular starvation (despite high blood glucose).
- A deficiency in glucose production, such as in certain glycogen storage diseases or severe liver failure, would lead to **hypoglycemia**, not the hyperglycemia characteristic of DKA.
Glucogenic and ketogenic amino acids US Medical PG Question 4: A 2-month-old boy is brought to his pediatrician’s office to be evaluated for new onset seizures and poor weight gain. The patient’s father says he is unable to track with his eyes and is unresponsive to verbal stimuli. The patient is hypotonic on physical exam. Further studies show elevated serum lactate levels and elevated levels of alanine and pyruvate. Family history reveals that several distant family members suffered from neurological diseases and died of unknown causes at a young age. Which of the following amino acids should be increased in this patient’s diet?
- A. Isoleucine
- B. Valine
- C. Arginine (Correct Answer)
- D. Leucine
- E. Methionine
Glucogenic and ketogenic amino acids Explanation: ***Arginine***
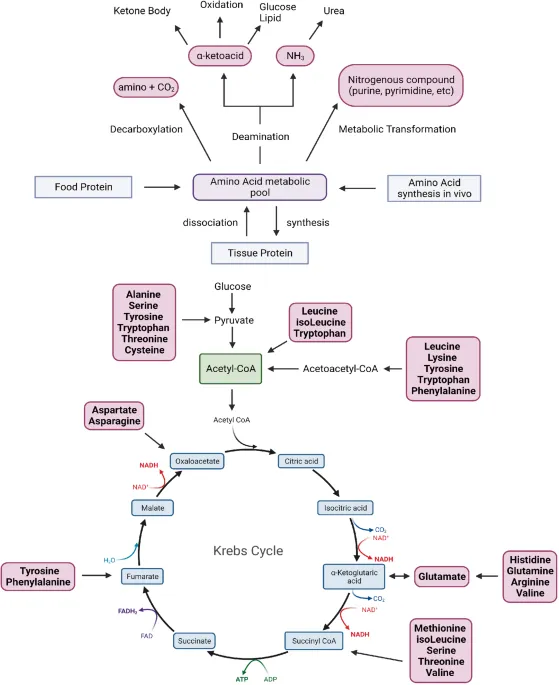
- The symptoms of **seizures, developmental delay, hypotonia, and elevated lactate/pyruvate** levels, along with a family history of early deaths, are highly suggestive of a **mitochondrial disorder**, specifically **pyruvate dehydrogenase complex (PDC) deficiency**.
- **Arginine** supplementation is used in certain **mitochondrial disorders** to enhance **nitric oxide (NO) production**, which improves **endothelial function and tissue perfusion**. While the primary treatment for PDC deficiency is a **ketogenic diet** and cofactor supplementation (thiamine, lipoic acid), among the amino acid options listed, arginine has supportive evidence in mitochondrial cytopathies.
- Arginine may help counteract **endothelial dysfunction** and improve oxygen delivery to tissues affected by mitochondrial impairment.
*Isoleucine*
- **Isoleucine** is a **branched-chain amino acid (BCAA)** that is catabolized to produce acetyl-CoA and succinyl-CoA for energy.
- In **PDC deficiency**, the problem is the conversion of **pyruvate to acetyl-CoA**, not BCAA metabolism. Increasing BCAAs is not a therapeutic strategy for this condition.
- Excessive BCAA intake could potentially worsen metabolic imbalances without addressing the underlying enzymatic defect.
*Valine*
- **Valine** is another **branched-chain amino acid (BCAA)** with no specific role in managing PDC deficiency.
- Like isoleucine, valine supplementation does not address the **pyruvate dehydrogenase complex defect** and is not part of standard dietary management.
- BCAAs require careful monitoring in metabolic disorders and are not indicated for mitochondrial disorders like PDC deficiency.
*Leucine*
- **Leucine** is a **branched-chain amino acid (BCAA)** and potent activator of mTOR signaling for protein synthesis.
- Direct leucine supplementation is **not indicated for PDC deficiency** and does not address the metabolic block at the pyruvate dehydrogenase step.
- In disorders like **maple syrup urine disease (MSUD)**, BCAAs including leucine must be **restricted**, not supplemented.
*Methionine*
- **Methionine** is a sulfur-containing amino acid important for **methylation reactions** through S-adenosylmethionine (SAM) synthesis.
- There is **no established role** for methionine supplementation in **pyruvate dehydrogenase complex deficiency** or mitochondrial disorders presenting with lactic acidosis.
- Methionine metabolism is not directly related to the pathophysiology of PDC deficiency.
Glucogenic and ketogenic amino acids US Medical PG Question 5: In a patient with maple syrup urine disease, all of the following amino acids should be restricted in diet except?
- A. Methionine (Correct Answer)
- B. Isoleucine
- C. Leucine
- D. Valine
Glucogenic and ketogenic amino acids Explanation: ***Methionine***
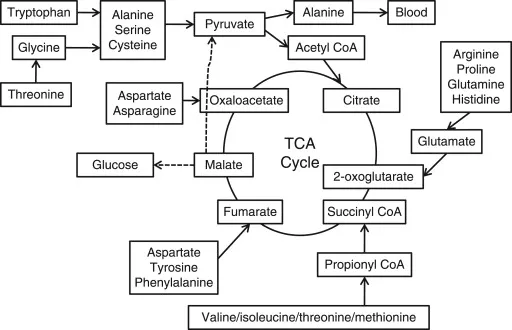
- **Maple syrup urine disease (MSUD)** is a disorder affecting the metabolism of **branched-chain amino acids (BCAAs)**: leucine, isoleucine, and valine.
- Therefore, methionine, which is not a BCAA, typically does not need to be restricted and is, in fact, an **essential amino acid** crucial for protein synthesis.
*Isoleucine*
- **Isoleucine** is a branched-chain amino acid (BCAA) whose metabolism is impaired in MSUD due to a deficiency in **branched-chain alpha-keto acid dehydrogenase complex**.
- Accumulation of isoleucine and its corresponding alpha-keto acid is toxic and must be **restricted in the diet**.
*Leucine*
- **Leucine** is another branched-chain amino acid (BCAA) that cannot be properly metabolized in MSUD.
- High levels of leucine and its metabolites are particularly **neurotoxic** and contribute to the characteristic neurological symptoms, necessitating strict dietary restriction.
*Valine*
- **Valine** is the third branched-chain amino acid (BCAA) whose breakdown is defective in MSUD.
- Dietary restriction of valine is essential to prevent its accumulation, which can lead to metabolic crises and **developmental delays**.
Glucogenic and ketogenic amino acids US Medical PG Question 6: A codon is an mRNA sequence consisting of 3 nucleotides that codes for an amino acid. Each position can be made up of any 4 nucleotides (A, U, G, C); therefore, there are a total of 64 (4 x 4 x 4) different codons that can be created but they only code for 20 amino acids. This is explained by the wobble phenomenon. One codon for leucine is CUU, which of the following can be another codon coding for leucine?
- A. CUA (Correct Answer)
- B. CCC
- C. UAA
- D. CCA
- E. AUG
Glucogenic and ketogenic amino acids Explanation: ***CUA***
- The **wobble hypothesis** allows for non-standard base pairing at the **third position** of the codon.
- Since CUU codes for leucine, a change in the third base to **A (CUA)** can often still code for the same amino acid due to degeneracy of the genetic code.
*CCC*
- This codon codes for **proline**, not leucine.
- A change in the **second letter** of the codon almost always results in a different amino acid.
*UAA*
- This is one of the **stop codons** (UAA, UAG, UGA), which signals the termination of translation.
- It does not code for any amino acid.
*CCA*
- This codon codes for **proline**, not leucine.
- Changing the first or second nucleotide typically results in a different amino acid.
*AUG*
- This codon codes for **methionine** and also serves as the **start codon** for protein synthesis.
- It does not code for leucine.
Glucogenic and ketogenic amino acids US Medical PG Question 7: A 50-year-old man presents to the office with the complaint of pain in his left great toe. The pain started 2 days ago and has been progressively getting worse to the point that it is difficult to walk even a few steps. He adds that his left big toe is swollen and hot to the touch. He has never had similar symptoms in the past. He normally drinks 2–3 cans of beer every night but recently binge drank 3 nights ago. Physical examination is notable for an overweight gentleman (BMI of 35) in moderate pain, with an erythematous, swollen, and exquisitely tender left great toe. Laboratory results reveal a uric acid level of 9 mg/dL. A complete blood count shows:
Hemoglobin % 12 gm/dL
Hematocrit 45%
Mean corpuscular volume (MCV) 90 fL
Platelets 160,000/mm3
Leukocytes 8,000/mm3
Segmented neutrophils 65%
Lymphocytes 25%
Eosinophils 3%
Monocytes 7%
RBCs 5.6 million/mm3
Synovial fluid analysis shows:
Cell count 55,000 cells/mm3 (80% neutrophils)
Crystals negatively birefringent crystals present
Culture pending
Gram stain no organisms seen
Which of the following is the mechanism of action of the drug that will most likely be used in the long-term management of this patient?
- A. Activates adenosine monophosphate (AMP) deaminase
- B. Inhibits renal clearance of uric acid
- C. Activates inosine monophosphate (IMP) dehydrogenase
- D. Inhibits xanthine oxidase (Correct Answer)
- E. Increases renal clearance of uric acid
Glucogenic and ketogenic amino acids Explanation: ***Inhibits xanthine oxidase***
- The patient's symptoms (acute, severe pain in the **great toe**, swelling, erythema, elevated **uric acid** 9 mg/dL, and presence of **negatively birefringent crystals** in synovial fluid) are classic for an acute **gout attack**.
- **Allopurinol** and **febuxostat** are long-term management drugs that work by inhibiting **xanthine oxidase**, an enzyme crucial for uric acid production, thereby reducing serum uric acid levels and preventing future attacks.
*Activates adenosine monophosphate (AMP) deaminase*
- This is not a mechanism of action for common long-term gout medications. AMP deaminase is involved in purine metabolism but is not a direct target for uric acid lowering.
- Manipulating AMP deaminase activity is not a recognized therapeutic approach for chronic gout management.
*Inhibits renal clearance of uric acid*
- This mechanism would *increase* serum uric acid levels, which is contraindicated in the long-term management of gout.
- Drugs that inhibit renal clearance of uric acid would exacerbate the condition, leading to more frequent and severe gout attacks.
*Activates inosine monophosphate (IMP) dehydrogenase*
- This is not a mechanism of action for long-term gout medications. IMP dehydrogenase is involved in de novo purine synthesis.
- Inhibitors of IMP dehydrogenase, like **mycophenolate mofetil**, are used in transplant medicine and autoimmune conditions, not for lowering uric acid.
*Increases renal clearance of uric acid*
- Drugs like **probenecid** act as **uricosurics** by increasing the renal excretion of uric acid. While this helps lower uric acid, it is specifically contraindicated in patients with **renal stones** or impaired renal function due to the risk of stone formation.
- **Uricosurics** are generally second-line agents for long-term management in patients who **under-excrete uric acid** and have good renal function.
Glucogenic and ketogenic amino acids US Medical PG Question 8: A group of researchers wish to develop a clinical trial assessing the efficacy of a specific medication on the urinary excretion of amphetamines in intoxicated patients. They recruit 50 patients for the treatment arm and 50 patients for the control arm of the study. Demographics are fairly balanced between the two groups. The primary end points include (1) time to recovery of mental status, (2) baseline heart rate, (3) urinary pH, and (4) specific gravity. Which medication should they use in order to achieve a statistically significant result positively favoring the intervention?
- A. Potassium citrate
- B. Ascorbic acid (Correct Answer)
- C. Tap water
- D. Sodium bicarbonate
- E. Aluminum hydroxide
Glucogenic and ketogenic amino acids Explanation: ***Ascorbic acid***
- Urinary excretion of **weak bases** like amphetamines is enhanced in an **acidic urine environment**. Ascorbic acid, or vitamin C, is an acidic substance that, when administered, can significantly **lower urinary pH**.
- By acidifying the urine, ascorbic acid promotes the **ionization of amphetamines** in the renal tubules, making them less lipid-soluble and decreasing their reabsorption, thereby **increasing their urinary excretion**.
*Potassium citrate*
- Potassium citrate is a **urinary alkalinizer**, meaning it would increase the pH of the urine.
- Increasing urinary pH would **decrease the excretion of acidic drugs** and **increase the reabsorption of basic drugs** like amphetamines, which is the opposite of the desired effect.
*Tap water*
- Administering tap water would primarily lead to **diuresis** (increased urine production) but would have a **negligible effect on urinary pH**.
- While increased urine volume can dilute the concentration of amphetamines, it does not significantly alter the **renal clearance rate based on pH**, which is crucial for weak bases.
*Sodium bicarbonate*
- Sodium bicarbonate is a potent **urinary alkalinizer**, used to increase the pH of the urine.
- Just like potassium citrate, a higher urinary pH would **inhibit the excretion of amphetamines** by promoting their non-ionized, lipid-soluble form and increasing their reabsorption.
*Aluminum hydroxide*
- Aluminum hydroxide is primarily an **antacid** and phosphate binder, used for conditions like GERD or hyperphosphatemia; it has **no significant direct effect on urinary pH or amphetamine excretion**.
- Its action is largely confined to the gastrointestinal tract, and it does not get absorbed in a way that would acidify the urine.
Glucogenic and ketogenic amino acids US Medical PG Question 9: A 35-year-old man comes to the physician because of worsening pain in his lower back, knees, and shoulders over the past few years. He used to be able to touch his fingers to his toes while standing; now he has difficulty touching his shins. He is wearing a shirt with dark brown stains around the armpits. Physical examination shows bluish-brown sclerae and thickening of the external ear. The range of motion of the affected joints is decreased. X-rays of the spine show calcification of multiple lumbar intervertebral discs. The patient's condition is most likely caused by impaired metabolism of which of the following?
- A. Ornithine
- B. Tyrosine (Correct Answer)
- C. Hypoxanthine
- D. Homocysteine
- E. Tryptophan
Glucogenic and ketogenic amino acids Explanation: ***Tyrosine***
- The constellation of symptoms, including dark discoloration of sweat (brown stains around armpits), bluish-brown sclerae, thickening of the ear cartilage (ochronosis), back and joint pain, and calcification of intervertebral discs, is classic for **alkaptonuria**.
- **Alkaptonuria** is an autosomal recessive disorder caused by a deficiency of homogentisate 1,2-dioxygenase, an enzyme involved in the metabolism of **tyrosine**. This leads to the accumulation of **homogentisic acid**.
*Ornithine*
- Impaired metabolism of ornithine is associated with disorders of the **urea cycle**, such as **ornithine transcarbamylase deficiency**.
- These conditions primarily lead to **hyperammonemia** and neurological symptoms, not the musculoskeletal or ochronotic features described.
*Hypoxanthine*
- Hypoxanthine is a purine derivative whose metabolism is relevant in disorders like **gout** (due to overproduction or underexcretion of uric acid, a metabolite of hypoxanthine) and **Lesch-Nyhan syndrome**.
- These conditions do not present with the characteristic features of ochronosis or multijoint calcification seen in this patient.
*Homocysteine*
- Impaired metabolism of homocysteine is characteristic of disorders like **homocystinuria**, which can be caused by deficiencies in enzymes such as **cystathionine beta-synthase**.
- Homocystinuria typically presents with lens dislocation, Marfanoid habitus, developmental delay, and thromboembolic events, not ochronosis or joint calcification.
*Tryptophan*
- Impaired metabolism of tryptophan can be seen in conditions such as **Hartnup disease** (a defect in amino acid transport) or in deficiencies affecting **niacin synthesis**.
- These conditions typically manifest with symptoms like pellagra-like dermatosis, cerebellar ataxia, and neuropsychiatric disturbances, which are not consistent with the patient's presentation.
Glucogenic and ketogenic amino acids US Medical PG Question 10: An investigator is studying nutritional deficiencies in humans. A group of healthy volunteers are started on a diet deficient in pantothenic acid. After 4 weeks, several of the volunteers develop irritability, abdominal cramps, and burning paresthesias of their feet. These symptoms are fully reversed after reintroduction of pantothenic acid to their diet. The function of which of the following enzymes was most likely impaired in the volunteers during the study?
- A. Gamma-glutamyl carboxylase
- B. Alpha-ketoglutarate dehydrogenase (Correct Answer)
- C. Dopamine beta-hydroxylase
- D. Methionine synthase
- E. Glutathione reductase
Glucogenic and ketogenic amino acids Explanation: ***Alpha-ketoglutarate dehydrogenase***
- **Pantothenic acid** (vitamin B5) is a precursor of **coenzyme A (CoA)**, which is essential for the function of alpha-ketoglutarate dehydrogenase in the **Krebs cycle**.
- Impairment of this enzyme, critical for energy production, can lead to widespread metabolic dysfunction, manifesting as neurological and gastrointestinal symptoms like **irritability, abdominal cramps**, and **burning paresthesias**, which are classic signs of pantothenic acid deficiency.
*Gamma-glutamyl carboxylase*
- This enzyme is involved in the post-translational modification of several proteins, including **clotting factors**, and requires **vitamin K** as a cofactor.
- Its deficiency leads to bleeding disorders, not the neurological and GI symptoms described.
*Dopamine beta-hydroxylase*
- This enzyme converts **dopamine to norepinephrine** and requires vitamin C and copper.
- Its impairment can affect neurotransmitter synthesis but is not directly linked to pantothenic acid deficiency.
*Methionine synthase*
- This enzyme is crucial for the metabolism of **homocysteine** and requires **vitamin B12** and **folate** as cofactors.
- Its deficiency is associated with megaloblastic anemia and neurological symptoms, but not the specific presentation seen with pantothenic acid deficiency.
*Glutathione reductase*
- This enzyme is essential for maintaining the reduced state of **glutathione**, an antioxidant, and requires **riboflavin** (vitamin B2) in its coenzyme form, FAD.
- Dysfunction typically leads to oxidative stress, hemolytic anemia, and other symptoms different from those described.
More Glucogenic and ketogenic amino acids US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.