Disorders of aromatic amino acids (PKU, alkaptonuria) US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Disorders of aromatic amino acids (PKU, alkaptonuria). These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Disorders of aromatic amino acids (PKU, alkaptonuria) US Medical PG Question 1: You are examining a 3-day-old newborn who was delivered vaginally without any complications. The newborn presents with vomiting, hyperventilation, lethargy, and seizures. Blood work demonstrates hyperammonemia, elevated glutamine levels, and decreased blood urea nitrogen. A CT scan demonstrates cerebral edema. Defects in which of the following enzymes would result in a clinical presentation similar to this infant?
- A. Carbamoyl phosphate synthetase I (Correct Answer)
- B. Homogentisate oxidase
- C. Cystathionine synthase
- D. Branched-chain ketoacid dehydrogenase
- E. Phenylalanine hydroxylase
Disorders of aromatic amino acids (PKU, alkaptonuria) Explanation: **Carbamoyl phosphate synthetase I**
- **Carbamoyl phosphate synthetase I (CPSI)** deficiency is a severe **urea cycle disorder** that typically presents in the neonatal period with **hyperammonemia**, **vomiting**, **lethargy**, **seizures**, and **hyperventilation**.
- The enzyme CPSI catalyzes the first step of the urea cycle, which is crucial for detoxifying ammonia, leading to **elevated glutamine** and **decreased blood urea nitrogen** when defective.
*Homogentisate oxidase*
- Deficiency in **homogentisate oxidase** causes **alkaptonuria**, a disorder of tyrosine metabolism.
- This condition is characterized by **dark urine** upon standing, **ochronosis** (bluish-black discoloration of cartilage and connective tissue later in life), and **arthropathy**, not hyperammonemia or acute neonatal crisis.
*Cystathionine synthase*
- A defect in **cystathionine synthase** leads to **homocystinuria**, an inherited disorder of methionine metabolism.
- Symptoms include **ectopia lentis**, **skeletal abnormalities**, **thromboembolic events**, and **developmental delay**, not acute neonatal hyperammonemic encephalopathy.
*Branched-chain ketoacid dehydrogenase*
- Deficiency in **branched-chain ketoacid dehydrogenase** causes **maple syrup urine disease (MSUD)**, a disorder of branched-chain amino acid metabolism.
- While it can present with vomiting, lethargy, and seizures in neonates, it is characterized by a distinctive **maple syrup odor** in urine and elevated branched-chain amino acids, not hyperammonemia and low BUN.
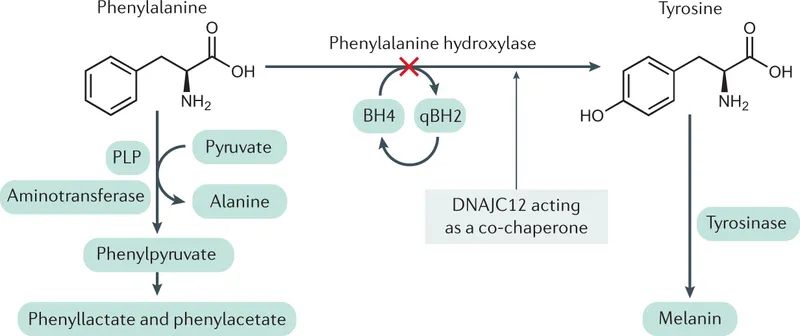
*Phenylalanine hydroxylase*
- A deficiency in **phenylalanine hydroxylase** causes **phenylketonuria (PKU)**, an amino acid metabolism disorder.
- PKU typically presents with intellectual disability, seizures, and a musty odor if untreated, but generally does not manifest as an acute neonatal crisis with hyperammonemia, as seen in urea cycle defects.
Disorders of aromatic amino acids (PKU, alkaptonuria) US Medical PG Question 2: A 6-month-old boy is brought to a pediatrician by his parents for his first visit after they adopt him from a European country. His parents are concerned about the boy’s short episodes of shaking of his arms and legs; they believe it might be epilepsy. They also note that the child is less responsive than other children of his age. The family is unable to provide any vaccination, birth, or family history. His pulse is 130/min, respiratory rate is 28/min, and blood pressure is 90/50 mm Hg. The boy has a light skin tone and emits a noticeable musty body odor. Which of the following should be supplemented in this patient’s diet?
- A. Isoleucine
- B. Leucine
- C. Tyrosine (Correct Answer)
- D. Phenylalanine
- E. Histidine
Disorders of aromatic amino acids (PKU, alkaptonuria) Explanation: ***Tyrosine***
- The patient's presentation with **seizures**, **developmental delay** (less responsive), **light skin tone**, and a **musty body odor** is highly suggestive of **phenylketonuria (PKU)**.
- In PKU, there is a deficiency in the enzyme **phenylalanine hydroxylase**, which converts **phenylalanine** to **tyrosine**. Therefore, **tyrosine** becomes an **essential amino acid** and must be supplemented in the diet.
*Isoleucine*
- **Isoleucine** is a **branched-chain amino acid** that is typically restricted, along with leucine and valine, in conditions like **maple syrup urine disease (MSUD)**, not PKU.
- Supplementation of isoleucine would be detrimental in MSUD and is not indicated for PKU.
*Leucine*
- Similar to isoleucine, **leucine** is a **branched-chain amino acid** whose metabolism is impaired in **MSUD**, not PKU.
- Supplementing leucine is not beneficial for PKU and would be harmful in MSUD.
*Phenylalanine*
- **Phenylalanine** is the amino acid that accumulates to toxic levels in **PKU** due to the enzyme deficiency.
- Therefore, phenylalanine must be **strictly restricted** in the patient's diet, not supplemented.
*Histidine*
- **Histidine** is an essential amino acid but is not directly involved in the metabolic pathway affected by PKU.
- There is no indication for histidine supplementation in the management of PKU.
Disorders of aromatic amino acids (PKU, alkaptonuria) US Medical PG Question 3: A 30-year-old African American G1P0 mother gives birth to a male infant at 33 weeks' gestation. The mother had no prenatal care and took no prenatal vitamins. The child’s postnatal period was complicated by neonatal sepsis due to group B Streptococcus. He required a two week stay in the neonatal intensive care unit to receive antibiotics, cardiopulmonary support, and intravenous nutrition. He eventually recovered and was discharged. At a normal follow-up visit to the pediatrician’s office one month later, the mother asks about the child’s skin color and hair color. On examination, the child has white hair and diffusely pale skin. The child’s irises appear translucent. Further questioning of the mother reveals that there is a distant family history of blindness. This child most likely has a defect in an enzyme involved in the metabolism of which of the following molecules?
- A. Leucine
- B. Homocysteine
- C. Phenylalanine
- D. Homogentisic acid
- E. DOPA (Correct Answer)
Disorders of aromatic amino acids (PKU, alkaptonuria) Explanation: ***DOPA***
- The symptoms of **white hair**, **pale skin**, and **translucent irises**, along with a family history of **blindness**, are classic signs of **oculocutaneous albinism**.
- **Oculocutaneous albinism** results from a defect in **tyrosinase**, an enzyme responsible for converting **DOPA** (3,4-dihydroxyphenylalanine) into **melanin**.
*Leucine*
- Defects in **leucine** metabolism are associated with **Maple Syrup Urine Disease**, characterized by sweet-smelling urine and neurological complications, not albinism.
- This condition involves impaired **branched-chain alpha-keto acid dehydrogenase** complex activity, leading to an accumulation of branched-chain amino acids.
*Homocysteine*
- Problems with **homocysteine** metabolism are seen in conditions like **homocystinuria**, which can cause developmental delay, skeletal abnormalities, and vascular issues, but not hypopigmentation.
- This is often due to deficiencies in **cystathionine beta-synthase** or other enzymes involved in folate and vitamin B12 metabolism.
*Phenylalanine*
- A defect in **phenylalanine** metabolism, specifically **phenylalanine hydroxylase**, leads to **phenylketonuria (PKU)**, which causes intellectual disability, seizures, and a musty odor, but not the specific ocular and cutaneous features described for albinism.
- While PKU can cause milder hypopigmentation due to reduced tyrosine availability, the described translucent irises and severe white hair are more indicative of albinism.
*Homogentisic acid*
- A defect in **homogentisic acid** metabolism causes **alkaptonuria**, characterized by dark urine upon standing, blue-black discoloration of cartilage (ochronosis), and early-onset arthritis, which are not present in this case.
- This condition results from a deficiency of **homogentisate 1,2-dioxygenase**.
Disorders of aromatic amino acids (PKU, alkaptonuria) US Medical PG Question 4: A 3-month-old infant is brought to her pediatrician for a well-child visit. The infant was born to a 22-year-old mother via a spontaneous vaginal delivery at 38 weeks of gestation in her home. She moved to the United States approximately 3 weeks ago from a small village. She reports that her infant had 2 episodes of non-bloody and non-bilious vomiting. The infant's medical history includes eczema and 2 seizure episodes that resolved with benzodiazepines in the emergency department. Physical examination is notable for a musty body odor, eczema, and a fair skin complexion. Which of the following is the best next step in management?
- A. Dietary restriction (Correct Answer)
- B. Abdominal radiography
- C. Dermatology consult
- D. MRI of the brain
- E. Antiepileptic drug
Disorders of aromatic amino acids (PKU, alkaptonuria) Explanation: ***Dietary restriction***
- The infant's symptoms, including **eczema**, **seizures**, **fair skin**, and a distinctive "musty" odor, strongly suggest **phenylketonuria (PKU)**. PKU is an **autosomal recessive metabolic disorder** where the body cannot properly break down **phenylalanine**.
- The primary treatment for PKU is a **lifelong diet low in phenylalanine**. This involves restricting high-protein foods and using special medical formulas to provide adequate nutrition. Early and strict dietary management is crucial to prevent intellectual disability and other neurological complications.
*Abdominal radiography*
- While the infant experienced vomiting, the description of it being **non-bloody** and **non-bilious**, along with the absence of other gastrointestinal symptoms like distension, makes a significant abdominal pathology less likely than **metabolic derangement**.
- Abdominal radiography would be more appropriate for suspected **bowel obstruction** or perforation, for which there are no strong indications in this case.
*Dermatology consult*
- The presence of eczema is noted, but it is one of several symptoms pointing towards a **systemic metabolic disorder** rather than an isolated skin condition.
- Addressing the underlying metabolic cause (PKU) through dietary restriction will likely improve or resolve the eczema, making a consult for symptomatic treatment a secondary concern.
*MRI of the brain*
- The infant has experienced seizures, which often prompt neurological imaging. However, in the context of the other clinical findings (musty odor, fair skin, eczema), the seizures are highly suggestive of **metabolic encephalopathy** due to PKU.
- While an MRI might show changes related to chronic phenylalanine toxicity, the most urgent and effective intervention is to address the metabolic cause through **dietary restriction**.
*Antiepileptic drug*
- Starting an antiepileptic drug might control the seizures symptomatically, but it would **not address the underlying cause** of the seizures, which is the metabolic disturbance in PKU.
- **Untreated PKU** will lead to progressive neurological damage and intellectual disability even if seizures are controlled, highlighting the importance of root cause treatment.
Disorders of aromatic amino acids (PKU, alkaptonuria) US Medical PG Question 5: A 3-day-old female infant presents with poor feeding, lethargy, vomiting after feeding, and seizures. Labs revealed ketoacidosis and elevated hydroxypropionic acid levels. Upon administration of parenteral glucose and protein devoid of valine, isoleucine, methionine, and threonine, and carnitine, the infant began to recover. Which of the following enzymes is most likely deficient in this infant?
- A. Branched-chain ketoacid dehydrogenase
- B. Propionyl-CoA carboxylase (Correct Answer)
- C. Cystathionine synthase
- D. Phenylalanine hydroxylase
- E. Homogentisate oxidase
Disorders of aromatic amino acids (PKU, alkaptonuria) Explanation: ***Propionyl-CoA carboxylase***
- The presence of **ketoacidosis** and elevated **hydroxypropionic acid** levels is characteristic of propionic acidemia, which is caused by a deficiency in **propionyl-CoA carboxylase**.
- The therapeutic benefit from a diet restricted in **valine, methionine, threonine**, and **isoleucine** (precursors of propionyl-CoA) along with carnitine supplementation further supports this diagnosis.
*Branched-chain ketoacid dehydrogenase*
- A deficiency in this enzyme leads to **Maple Syrup Urine Disease**, characterized by elevated **branched-chain ketoacids** and associated with a distinctive sweet odor in urine.
- While it causes neurotoxicity and poor feeding, the specific finding of elevated **hydroxypropionic acid** points away from this diagnosis.
*Cystathionine synthase*
- Deficiency in **cystathionine synthase** causes **homocystinuria**, leading to elevated **homocysteine** levels.
- Symptoms include developmental delay, ectopia lentis, and skeletal abnormalities, but not typically elevated **hydroxypropionic acid** or severe neonatal ketoacidosis in this manner.
*Phenylalanine hydroxylase*
- This enzyme is deficient in **phenylketonuria (PKU)**, resulting in high levels of **phenylalanine** and its metabolites.
- PKU is typically associated with intellectual disability, seizures, and a musty odor, but not ketoacidosis or elevated **hydroxypropionic acid**.
*Homogentisate oxidase*
- A deficiency in this enzyme causes **alkaptonuria**, characterized by the accumulation of **homogentisic acid**.
- This condition is usually benign in infancy, primarily manifesting as dark urine upon standing and later developing into ochronosis and arthritis, without acute neonatal ketoacidosis or elevated **hydroxypropionic acid**.
Disorders of aromatic amino acids (PKU, alkaptonuria) US Medical PG Question 6: A 12-year-old boy comes to the physician for the evaluation of intermittent blood-tinged urine for several months. Four months ago, he had an episode of fever and sore throat that resolved without treatment after 5 days. During the past 2 years, he has also had recurrent episodes of swelling of his face and feet. 5 years ago, he was diagnosed with mild bilateral sensorineural hearing loss. His brother died of a progressive kidney disease at the age of 23. The patient appears pale. His temperature is 37°C (98.6°F), pulse is 70/min, and blood pressure is 145/85 mm Hg. Slit lamp examination shows a conical protrusion of both lenses. Laboratory studies show a hemoglobin concentration of 11 g/dL, urea nitrogen concentration of 40 mg/dL, and creatinine concentration of 2.4 mg/dL. Urinalysis shows:
Blood 2+
Protein 1+
RBC 5–7/hpf
RBC casts rare
Which of the following is the most likely underlying cause of this patient's symptoms?
- A. IgA deposits
- B. WT1 gene mutation
- C. Defective type IV collagen (Correct Answer)
- D. Autosomal-recessive kidney disease
- E. Type II hypersensitivity reaction
Disorders of aromatic amino acids (PKU, alkaptonuria) Explanation: ***Defective type IV collagen***
- This patient presents with a classic triad of symptoms: **progressive kidney disease** (elevated creatinine, blood-tinged urine, family history), **sensorineural hearing loss**, and **ocular abnormalities** (lenticonus on slit lamp exam). These findings are highly suggestive of **Alport syndrome**, which is caused by a defect in **type IV collagen**.
- The family history of a brother dying of progressive kidney disease at a young age further supports a genetic cause, and the intermittent blood-tinged urine after an upper respiratory infection can be a feature of Alport syndrome, often misinterpreted as IgA nephropathy early in its course.
*IgA deposits*
- **IgA nephropathy** can present with recurrent episodes of gross hematuria, often following an upper respiratory infection, similar to the initial presentation of this patient's blood-tinged urine.
- However, IgA nephropathy typically does not involve **sensorineural hearing loss** or **ocular abnormalities** like lenticonus.
*WT1 gene mutation*
- A **WT1 gene mutation** is associated with **Denys-Drash syndrome** and **Frasier syndrome**, which involve nephropathy and, in some cases, gonadal abnormalities or ambiguous genitalia.
- While these can cause kidney disease, they do not typically present with the characteristic ocular findings (lenticonus) or sensorineural hearing loss seen in this patient.
*Autosomal-recessive kidney disease*
- While Alport syndrome can have autosomal recessive inheritance (10-15% of cases), this option is too broad and does not specify the underlying **molecular defect** (type IV collagen).
- The family history pattern here (affected brother, male proband) is more consistent with **X-linked Alport syndrome** (85% of cases), and this non-specific option does not pinpoint the actual pathogenic mechanism that links all the patient's symptoms.
*Type II hypersensitivity reaction*
- A **type II hypersensitivity reaction** involves antibody-mediated cellular destruction or dysfunction, such as in Goodpasture syndrome, where antibodies attack the glomerular basement membrane.
- This mechanism does not explain the long-standing, progressive nature of kidney disease combined with sensorineural hearing loss and ocular defects. Instead, these are characteristic of an underlying structural protein defect.
Disorders of aromatic amino acids (PKU, alkaptonuria) US Medical PG Question 7: A 2-week-old boy presents to the emergency department because of unusual irritability and lethargy. The patient is admitted to the pediatric intensive care unit and minutes later develops metabolic encephalopathy. This progressed to a coma, followed by death before any laboratory tests are completed. The infant was born at home via vaginal delivery at 39 weeks' of gestation. His mother says that the symptoms started since the infant was 4-days-old, but since he only seemed ‘tired’, she decided not to seek medical attention. Further testing during autopsy shows hyperammonemia, low citrulline, and increased orotic acid. Which of the following enzymes is most likely deficient in this patient?
- A. Branched-chain alpha-ketoacid dehydrogenase
- B. Propionyl-CoA carboxylase
- C. Homogentisic acid dioxygenase
- D. Ornithine transcarbamylase (Correct Answer)
- E. Cystathionine beta-synthase
Disorders of aromatic amino acids (PKU, alkaptonuria) Explanation: **Ornithine transcarbamylase**
- **Hyperammonemia**, **low citrulline**, and **increased orotic acid** are classic findings in **Ornithine Transcarbamylase (OTC) deficiency**. OTC is an X-linked urea cycle disorder.
- The rapid progression to **metabolic encephalopathy** and death in a neonate with these laboratory findings is highly characteristic of severe OTC deficiency, often presenting in the first few days of life.
*Branched-chain alpha-ketoacid dehydrogenase*
- Deficiency of this enzyme causes **Maple Syrup Urine Disease**, characterized by elevated **branched-chain amino acids** and their corresponding ketoacids in blood and urine.
- While it can cause neurological symptoms, it does not typically present with the specific constellation of **hyperammonemia**, low citrulline, and high orotic acid.
*Propionyl-CoA carboxylase*
- Deficiency of this enzyme leads to **Propionic acidemia**, a type of organic acidemia, characterized by **propionic acid accumulation** and often **metabolic acidosis**, ketosis, and hyperammonemia.
- However, it would not typically cause **low citrulline** or isolated **elevated orotic acid** as seen in urea cycle disorders.
*Homogentisic acid dioxygenase*
- Deficiency of this enzyme causes **Alkaptonuria**, an inborn error of metabolism characterized by the accumulation of **homogentisic acid**.
- This condition is usually benign in infancy, with symptoms appearing later in life such as **dark urine** on standing and **ochronosis** (darkening of cartilage). It does not present with acute hyperammonemia or metabolic encephalopathy.
*Cystathionine beta-synthase*
- Deficiency of this enzyme causes **homocystinuria**, an inborn error of methionine metabolism, leading to elevated **homocysteine** and methionine.
- Clinical features include **ectopia lentis**, skeletal abnormalities, and intellectual disability, but not usually acute neonatal hyperammonemia or the specific findings of low citrulline and high orotic acid.
Disorders of aromatic amino acids (PKU, alkaptonuria) US Medical PG Question 8: A 5 year old child was brought to the physician with a history of black urine. There is no history of fever or any other complaints. There is no growth retardation and all the developmental milestones are normal. The child is suspected to have an enzyme defect for metabolism of an aromatic amino acid. What is the enzyme deficient
- A. Homogentisate dehydrogenase
- B. Homogentistae oxidase (Correct Answer)
- C. Tyrosine Transaminase
- D. Tryptophan Hydroxylase
- E. Phenylalanine Hydroxylase
Disorders of aromatic amino acids (PKU, alkaptonuria) Explanation: ***Homogentistae oxidase***
- The presentation of a child with **black urine** (alkaptonuria) in the absence of other symptoms is characteristic of a deficiency in **homogentisate oxidase**.
- This enzyme is crucial in the catabolism of **tyrosine**, and its deficiency leads to the accumulation of **homogentisic acid**, which oxidizes upon exposure to air, turning urine black.
*Homogentisate dehydrogenase*
- This enzyme is not a recognized component of the **tyrosine degradation pathway** in humans.
- The correct enzyme involved in the breakdown of **homogentisate** is an oxidase, not a dehydrogenase, in this context.
*Tyrosine Transaminase*
- A deficiency in **tyrosine transaminase** (tyrosinemia type II) would lead to elevated tyrosine levels and typically presents with symptoms affecting the eyes, skin, and intellectual disability, not primarily black urine.
- This condition is characterized by **ocular findings** (corneal ulcers), **skin lesions**, and **neurological symptoms**.
*Tryptophan Hydroxylase*
- This enzyme is involved in the synthesis of **serotonin** and **melatonin** from tryptophan, a different amino acid pathway.
- A deficiency or abnormality in **tryptophan hydroxylase** would not cause black urine but could lead to neurological or mood disorders.
*Phenylalanine Hydroxylase*
- A deficiency in **phenylalanine hydroxylase** causes **phenylketonuria (PKU)**, which affects phenylalanine metabolism, not tyrosine metabolism directly.
- PKU typically presents with **intellectual disability**, **musty odor**, **fair skin**, and **seizures** if untreated, not black urine.
Disorders of aromatic amino acids (PKU, alkaptonuria) US Medical PG Question 9: A 21-year-old man presents to the emergency department with acute back pain. The pain began a few hours prior to presentation and is located on the left lower back. The pain is described to be “shock-like,” 9/10 in pain severity, and radiates to the left groin. His temperature is 98.6°F (37°C), blood pressure is 120/75 mmHg, pulse is 101/min, and respirations are 18/min. The patient appears uncomfortable and is mildly diaphoretic. There is costovertebral angle tenderness and genitourinary exam is unremarkable. A non-contrast computerized tomography (CT) scan of the abdomen and pelvis demonstrates an opaque lesion affecting the left ureter with mild hydronephrosis. Straining of the urine with urine crystal analysis is demonstrated. Which of the following amino acids is most likely poorly reabsorbed by this patient’s kidney?
- A. Isoleucine
- B. Aspartic acid
- C. Phenylalanine
- D. Lysine (Correct Answer)
- E. Histidine
Disorders of aromatic amino acids (PKU, alkaptonuria) Explanation:
***Lysine***
- The patient's symptoms (acute, severe, radiating back pain, CVA tenderness, hydronephrosis, and opaque lesion on CT) are highly characteristic of a **kidney stone**.
- Given the patient's young age and the nature of the amino acid question, thinking of **cystinuria** is appropriate, where the basic amino acids **COLA** (cystine, ornithine, lysine, arginine) are poorly reabsorbed.
*Isoleucine*
- **Isoleucine** is a branched-chain amino acid, not one of the basic amino acids impacted by cystinuria.
- Its malabsorption is not associated with the formation of kidney stones.
*Aspartic acid*
- **Aspartic acid** is an acidic amino acid and is not involved in the transport defects seen in cystinuria.
- There is no direct link between aspartic acid malabsorption and kidney stone formation.
*Phenylalanine*
- **Phenylalanine** is an aromatic amino acid and its metabolism is associated with disorders like phenylketonuria, not kidney stones.
- It is not one of the amino acids whose renal reabsorption is impaired in cystinuria.
*Histidine*
- **Histidine** is an essential amino acid, but it is not one of the basic amino acids (COLA) whose transport is affected in cystinuria.
- Poor reabsorption of histidine is not typically associated with kidney stone formation.
Disorders of aromatic amino acids (PKU, alkaptonuria) US Medical PG Question 10: A 63-year-old man presents to his primary care provider with colicky pain radiating to his left groin. The pain has been intermittent for several days. He has also been experiencing occasional burning pain in his hands and feet and frequent headaches. His past medical history is significant for an NSTEMI last year. He is currently taking atorvastatin and low dose aspirin. Today his temperature is 36.8°C (98.2°F), the heart rate is 103/min, the respiratory rate is 15/min, the blood pressure 135/85 mm Hg, and the oxygen saturation is 100% on room air. On physical exam, he appears gaunt and anxious. His heart is tachycardia with a regular rhythm and his lungs are clear to auscultation bilaterally. On abdominal exam he has hepatomegaly. A thorough blood analysis reveals a hemoglobin of 22 mg/dL and a significantly reduced EPO. Renal function and serum electrolytes are within normal limits. A urinalysis is positive for blood. A non-contrast CT shows a large kidney stone obstructing the left ureter. The patient’s pain is managed with acetaminophen and the stone passes with adequate hydration. It is sent to pathology for analysis. Additionally, a bone marrow biopsy is performed which reveals trilineage hematopoiesis and hypercellularity with a JAK2 mutation. Which medication would help prevent future episodes of nephrolithiasis?
- A. Hydroxyurea
- B. Probenecid
- C. Thiazide
- D. Antihistamines
- E. Allopurinol (Correct Answer)
Disorders of aromatic amino acids (PKU, alkaptonuria) Explanation: ***Allopurinol***
- The patient's presentation, including **hypercellularity** with a **JAK2 mutation**, extremely high hemoglobin (22 mg/dL), and hepatomegaly, is consistent with **polycythemia vera**. This condition leads to increased cell turnover and elevated uric acid levels, predisposing to **uric acid nephrolithiasis**.
- **Allopurinol** inhibits xanthine oxidase, reducing the production of uric acid and preventing the formation of uric acid stones, which is crucial in patients with myeloproliferative disorders like polycythemia vera.
*Hydroxyurea*
- **Hydroxyurea** is a cytoreductive agent used in polycythemia vera to lower blood cell counts, thereby reducing the risk of thrombotic events and controlling symptoms.
- While it manages the underlying myeloproliferative disorder, it does not directly prevent **uric acid stone formation** and can sometimes increase uric acid levels during initial cytoreduction due to rapid cell lysis.
*Probenecid*
- **Probenecid** is a uricosuric agent that increases the excretion of uric acid in the urine.
- It is used in patients with **gout** or hyperuricemia who are underexcretors of uric acid, but it can paradoxically increase the risk of uric acid nephrolithiasis due to higher urinary uric acid concentrations.
*Thiazide*
- **Thiazide diuretics** reduce urinary calcium excretion and are primarily used to prevent **calcium-containing kidney stones**, such as calcium oxalate or calcium phosphate stones.
- They are not indicated for the prevention of **uric acid stones**, which are the likely type in this patient given his polycythemia vera.
*Antihistamines*
- **Antihistamines** block histamine receptors and are primarily used to treat allergic reactions, insomnia, or nausea.
- They have no role in the prevention or treatment of **nephrolithiasis** or conditions like polycythemia vera.
More Disorders of aromatic amino acids (PKU, alkaptonuria) US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.